Abstract
Hepatocellular carcinoma (HCC) is the world’s fifth most common cancer and second leading cause of cancer-related death in Taiwan. Over 600,000 HCC patients die each year worldwide despite recent advances in surgical techniques and medical treatments. Epigenetic regulations including DNA methylation and histone modification control gene expressions and play important roles during tumorigenesis. This study evaluates association between histone-modifying genes and prognosis of HCC to ferret out new diagnostic markers. We collected 50 paired HCC and adjacent non-cancerous tissues from Taiwanese patients for survey by RT-qPCR and tissue microarray-based immunohistochemistry (TMA-based IHC) staining. RT-qPCR data showed four of twenty-four genes over eightfold up-regulated in tumor tissues: e.g., histone phosphorylation gene-ARK2, methylation genes-G9a, SUV39H2, and EZH2 (n = 50, all p < 0.0001). Results of TMA-based IHC staining showed proteins of ARK2, EZH2, G9a, and SUV39H2 also overexpressed in tumor tissues. Staining intensity of SUV39H2 correlated with HCV infection (p = 0.025). We further restricted the analysis only in tumor tissues, we found EZH2 staining intensity associated with tumor stage (p = 0.016) and survival (p = 0.007); SUV39H2 intensity associated with tumor stage (p = 0.044). Our findings indicate overexpression of histone-modifying genes EZH2 and SUV39H2 associated with prognosis of HCC cases. EZH2 expression can serve as a novel prognostic biomarker during HCC progression among Taiwanese.
Keywords: Hepatocellular carcinoma, histone acetylation, histone methylation, histone phosphorylation, histone modification
Introduction
Hepatocellular carcinoma (HCC; also called liver cancer) is a highly lethal cancer (third most common cause of cancer mortality worldwide) with rising incidence; approximately 750,000 new cases reported each year around the globe and overall 5-year survival rate is only 0-14% [1,2]. In addition, the Cancer Registry Annual Report in Taiwan of 2012 ranked HCC as second most common cancer-related death in Taiwanese. This illustrates the urgency to expose cellular mechanisms involved in this aggressive cancer to develop more effective treatments and better prognosis. Chief risk factors include chronic viral hepatitis of B- or C-virus infection (HBV or HCV), alcohol abuse, nonalcoholic steatohepatitis, aflatoxin B1 exposure, and liver cirrhosis [3,4]. Currently, HCCs are diagnosed by the invasive (biopsy) and non-invasive (images and tumor markers) methods [5]. The former include imaging diagnosis such as computed tomography (CT), magnetic resonance imaging (MRI), and tumor markers like α-fetaprotein and glypican-3 [5]. Yet detailed molecular mechanisms of hepatocarcinogenesis are not fully understood; molecular factors capable of predicting clinical outcome and acting as potential therapeutic targets remain limited.
Human genome is highly compacted by nucleoprotein complexes called chromatin, whose basic unit is a nucleosome; DNA is tightly packed in nuclei with the help of proteins called linker (H1) and packing (H2A, H2B, H3, and H4) histones [6]. The term “epigenetics” means changes in gene expression and cellular phenotype without affecting DNA sequence [7]. Epigenetic mechanisms can be considered as an interface between the genome and risk factors of lifestyle and the environment [8]. Histone modification is one of the epigenetic mechanism belonging to post-translational modification of N-terminal tails of histone proteins by acetylation, methylation, phosphorylation, ubiquitylation, sumoylation, ADP ribosylation, biotinylation, and potentially other modifications; these appear to work together with other epigenetic mechanisms in establishing and maintaining gene activity states, thus regulating a gamut of cellular processes [9]. So that several families of enzymes catalyze post-translational modifications of histones, including acetyltransferases and deacetylases, methyltransferases and demethylases, etc. play key roles in histone modification [10]. Recent studies prove the importance of histone-modifying enzymes and chromatin remodeling complexes in regulating chromatin activities of transcription, replication, and DNA repair. Histone modification plays essential roles in generating the dynamic state of chromatin [6]. Alternations in the function of histone-modifying molecules and protein complexes are found to disrupt the pattern and levels of histone marks and consequently deregulate the control of chromatin-based processes leads to development of many cancers [11].
Hepatocarcinogenesis is viewed as a complex and multi-step process entailing epigenetic and genetic events [12]. Recent reports show histone-modifying genes associate with HCC prognosis. Besides histone acetylation-related proteins, epigenetic aberrations which caused by histone phosphorylation (like ARK2 and MSK1) and lysine or arginine methylation (like G9a, EZH2, SUV39H1, and SUV39H2) demonstrably associate with progression of many tumors [13-15]. For example, histone phosphorylation enzymes-Aurora kinases (subfamily of serine/threonine mitotic kinases) are primary molecules for maintaining accurate cell cycling and genomic stability [16]. In HCC, ARK1 (Aurora-A kinase; centrosome-associated serine/threonine kinase) is overexpressed frequently in HCC patients, and correlated with high grade and high stage [17]. ARK2 (Aurora-B kinase, which phosphorylates histone H3 at serine 10) is a chromosomal passenger protein and that is essential for chromosome segregation and cytokinesis; mRNA level of ARK2 is an independent molecular marker predicting tumor invasion of HCCs [18]. Likewise, Aurora kinase inhibitors are potential therapeutic agents for HCC treatment [18,19]. G9a, a histone methyltransferase for lysine 9 of histone 3 (H3K9), is also a major player in gene silencing and essential for early embryogenesis to regulate developmental gene expression [20,21]. EZH2 (a histone methyltransferase for lysine 27 of histone 3) belongs to the polycomb genes crucial for transcriptional regulation via nucleosome modification, chromatin remodeling, and interaction with other transcription factors [22]. Positive EZH2 expression as a diagnostic biomarker detects aggressive phenotype or a phenotype with poor prognosis in patients of China population [23]. SUV39H1 was the first SET domain-containing histone lysine methyltransferase (HKMT) discovered in 2000; SUV39H1 and SUV39H2 knockout mice have shown genomic instability [24]. The mRNA level of SUV39H1 has been shown no different in 23 paired HCC and non-cancerous liver tissues from Japanese population [25]. On the other hand, SUV39H1 mRNA level shows up-regulated in 38 HCC patients from Hong Kong [26].
The present report examines expressions of histone-modifying genes in 50 HCC patients to derive a relationship between gene expressions and clinicopathological parameters in these Taiwanese patients. Here, we assessed mRNA expression of 24 histone-modifying genes further studied protein expressions in HCC and corresponding non-cancerous liver tissues by RT-qPCR and immunohistochemistry staining. Once we better understand the clinical relevance of those histone-modifying genes in HCCs among the Taiwanese population, clinicians can offer effective cancer treatments, biomarkers for early detection, better prognosis, and novel therapeutic targets. Identifying molecular markers related to hepatocarcinogenesis would benefit patients and serve as potential therapeutic target for novel HCC drug treatments.
Materials and methods
Patients and clinical methods
This study was approved by the Institutional Review Board of the China Medical University Hospital (CMUH103-REC1-033). Fifty Taiwanese patients diagnosed with HCC at Changhua Christian Hospital (Changhua, Taiwan) during 2002-2006 enrolled. All underwent surgery with or without radiotherapy and/or chemotherapy. Their 50 paired HCC tissues and corresponding adjacent non-cancerous liver tissues were stored at -80°C until RNA extraction and IHC staining, their medical records reviewed. All tumors were classified according to the 7th edition of TNM Staging Manual of American Joint Committee on Cancer [27].
RNA extraction, reverse-transcription, and real-time quantitative polymerase chain reaction (RT-qPCR)
Total RNA was extracted from tissues according to instructions of the High Pure RNA Isolation Kit (Roche Applied Science; Mannheim, Germany). Single-strand cDNA was synthesized by high-capacity cDNA reverse transcription kit (Applied Biosystems, Foster City, CA). The RT-qPCR was performed to analyze mRNA expression in 4 groups: {1} histone acetylation genes- such as ADA (adenosine deaminase), ATF2 (activating transcription factor 2), CREBBP (CREB binding protein), ESA1 (histone acetyltransferase ESA1), GCN5 (general control of amino-acid synthesis 5-like 2, yeast), HAT1 (histone acetyltransferase 1), MOF (lysine acetyltransferase 8), p300/CBP (E1A binding protein P300), PCAF (TAF6-like RNA polymerase II, P300/CBP-associated factor), and SRC1; {2} histone lysine methylation genes such as MLL/TRX (myeloid/lymphoid or mixed-lineage leukemia/trithorax homolog, drosophila), SET1 (SET domain containing 1A), SET7 (SET domain containing 7), G9a (euchromatic histone-lysine N-methyltransferase 2), SETDB1 (SET domain, bifurcated 1), SUV39H1 (suppressor of variegation 3-9 homolog 1, drosophila), SUV39H2 (suppressor of variegation 3-9 homolog 2, drosophila), EZH2 (enhancer of zeste homolog 2, drosophila), DOT1 (disruptor of telomeric silencing-1), and SET8 (SET domain containing lysine methyltransferase 8); {3} histone arginine methylation genes such as CARM1 (coactivator-associated arginine methyltransferase 1) and PRMT1 (protein arginine methyltransferase 1); {4} histone serine/threonine phosphorylation genes such as ARK2 (aurora kinase B) and MSK1 (ribosomal protein S6 kinase, 90 kDa, polypeptide 5). We used GAPDH (glyceraldehyde-3-phosphate dehydrogenase) as the RT-qPCR internal control. Table 1 shows primer and probe sequences for each RT-qPCR reaction. The thermal cycling conditions: 95°C for 10 min, followed by 40 cycles of 95°C for 10 s, 60°C for 30 s, and 72°C for 10 s. Expression levels of mRNA were first normalized to mRNA of GAPDH and then expressed as folds of normal by 2-ΔΔCt method according to Liu et al [28].
Table 1.
Primer and probe sequences of RT-qPCR assays
| Gene | Forward primer | Reverse primer | Probe |
|---|---|---|---|
| ADA | ccttcgacaagcccaaagta | gcccctctgctgtgttagc | ctcctgcc |
| ARK2 | attgctgacttcggctggt | gtccagggtgccacacat | cttcctcc |
| ATF2 | cgaccgcagtcattacaaca | gtggagttgtgtgagctgga | tgtggctg |
| CARM1 | cacaccgacttcaaggacaa | aaaaacgacaggatcccaga | tggctgtg |
| CBP/CREBBP | gagatccagggcgagaatg | aactgatcctttgaaattgtcgt | ctggggct |
| DOT1 | ccccactcacctcagacg | ttgcaatttttctctcaattgc | cccagcag |
| ESA1 | aaggagctcatcgctacagtg | caagaggacctgcttcacct | gctggatc |
| EZH2 | tgcacatcctgacttctgtga | tcatctcccatataaggaatgttatg | ggaggtgg |
| G9a | gggaccttcatctgcgagta | tctcacatcagcctcagcat | gggagctg |
| GAPDH | agccacatcgctcagacac | gcccaatacgaccaaatcc | cttcagcc |
| Gcn5 | ccgaccagctctacacaacc | aggcactggggtgagactt | gggagctg |
| HAT1 | tctaaagttgatgagaactttgactgt | ttgtctaattttgccctcaaca | ctgcctct |
| MLL/TRX | gcgccaagctctttgcta | catcatcatcataacatttgtcacag | cttctgcc |
| MOF | gaagttcctcatcgctttcag | tcagacagcggcttctcc | ctccagct |
| MSK1 | tggtgctgacagattttggt | caaaaggaatatgctctttcagtttc | cctggcgc |
| P300 | gcagcctgcaactccact | gaggatttgatacctgtccttca | cctggagc |
| PCAF | cagagaccctgaccagcttt | gcgctttgatggctcttc | acctgctg |
| PRMT1 | ggagaattttgtagccaccttg | cctggccacaggacactt | ctccagcc |
| SET1 | cactgggtccatcacacaat | ctgagcctgtctggtgctc | ctggggcc |
| SETDB1 | tgaaaaagagcccttgaagc | ccaggaagggaagacatgc | tcctctcc |
| SET7 | atggatagcgacgacgaga | taatccgtcatcgtccaggt | tggaggag |
| SET8 | ggatttctaccctgtccgaag | ttcaatcaattcatctattcttttcc | cctggagc |
| SRC1 | tctcaaaacagaagcagatgga | gacgtcagcaaacacctgaa | acctgctg |
| SUV39H1 | tcatggagtacgtgggagaga | cctgacggtcgtagatctgg | ctctgcct |
| SUV39H2 | gcattgttttccacaagaacc | tgggctgtggtcaatagaatc | ctccagca |
Tissue microarray-based immunohistochemistry (TMA-based IHC) staining analysis and antibodies
TMA-based IHC staining for ARK2, EZH2, G9a, and SUV39H2 proteins was performed as follows. Primary antibodies for the study were ARK2 (Santa Cruz; sc-14327), EZH2 (Invitrogen; 49-1043), G9a (Santa Cruz; sc-22877), and SUV39H2 (Abgent; AP1281a). Briefly, the 5-μm paraffin-embedded sections (5 × 8 = 40 cores/slide tissue array; each slide has 20 paired of normal and tumor tissues from HCC patients) were deparaffinized, retrieved with heat in 10 mM citrate buffer (pH 6.0) at 121°C for 10 min, then treated with 3% hydrogen peroxide to remove endogenous peroxidase activity. Primary antibodies were used as suggested by manufacturers and were used at dilution of 1:50 after optimization. Tissue sections treated with secondary antibodies and with biotin-streptavidin complex for 30 min each at 37°C. Diaminobenzidine served as chromogene for immunoperoxidase reaction, slides counterstained with hematoxylin and examined for intensity by the pathologist in a blind manner. More than 50% of cells displayed positive staining and intensity scores of moderate and strong, was considered to be protein overexpression in this study. Tissue specimens were broadly distributed by immunohistochemical staining category (0, 1+, 2+, or 3+) according to the guidelines based on Hofmann et al. [29].
Statistical analysis
Statistical analyses were performed using SPSS v17 (SPSS Inc., Working, UK). Paired t-test was used for analysis RT-qPCR assays. Correction between protein expression and clinicopathological features of 50 HCC patients were drawn by Pearson’s Chi-squared test, P-values < 0.05 considered statistically significant.
Results
Four mRNAs of histone-modifying genes more than eightfold overexpressed in HCC tissues
To rate mRNA expression of histone-modifying genes in HCC, we performed RT-qPCR analysis on total RNA extracted, classifying 24 histone-modifying genes as {1} acetylation of lysine, {2} methylation of lysine, {3} methylation of arginine, or {4} phosphorylation of serine/threonine. Table 2 shows an overview of these histone-modifying genes. RT-qPCR results show all 24 genes significantly up-regulated in HCC tissues (tumors) from 50 patients as compared to adjacent non-cancerous tissues (normal) (P < 0.05; Figure 1A). Since all these genes showed statistically significant increase in tumors, we set eightfold up-regulation as threshold of mRNA overexpression. We found G9a (↑8.85 folds; methylation of lysine), SUV39H2 (↑9.78 folds; methylation of lysine), EZH2 (↑8.52 folds; methylation of lysine), and ARK2 (↑15.53 folds; phosphorylation of serine/threonine) were more than eightfold overexpressed in tumor (P < 0.0001; n = 50; Figure 1B). Figure 1B shows gene expression patterns in 50 paired tissues.
Table 2.
Overview of different classes of histone-modifying genes in this study
| Histone modifications | Residues modified | Genes-included in this study | Functions regulated |
|---|---|---|---|
| Acetylation of lysine | Lysine | ADA, ATF2, CREBBP, ESA1, GCN5, HAT1, MOF, p300/CBP, PCAF, SRC1 | Transcription; repair; replication; condensation |
|
| |||
| Methylation of lysine | Histone H3 Lysine 4 | MLL/TRX, SET1, SET7 | Transcription; repair |
| Histone H3 Lysine 9 | G9a, SETDB1, SUV39H1, SUV39H2 | ||
| Histone H3 Lysine 27 | EZH2 | ||
| Histone H3 Lysine 79 | DOT1 | ||
| Histone H4 Lysine 20 | SET8 | ||
|
| |||
| Methylation of arginine | Histone H3 on Arginine 17 | CARM1 | Transcription |
| Histone H4 on Arginine 3 | PRMT1 | ||
|
| |||
| Phosphorylation of serine/threonine | Histone H3 on Serine 10 | ARK2, MSK1 | Transcription; repair; condensation |
Figure 1.
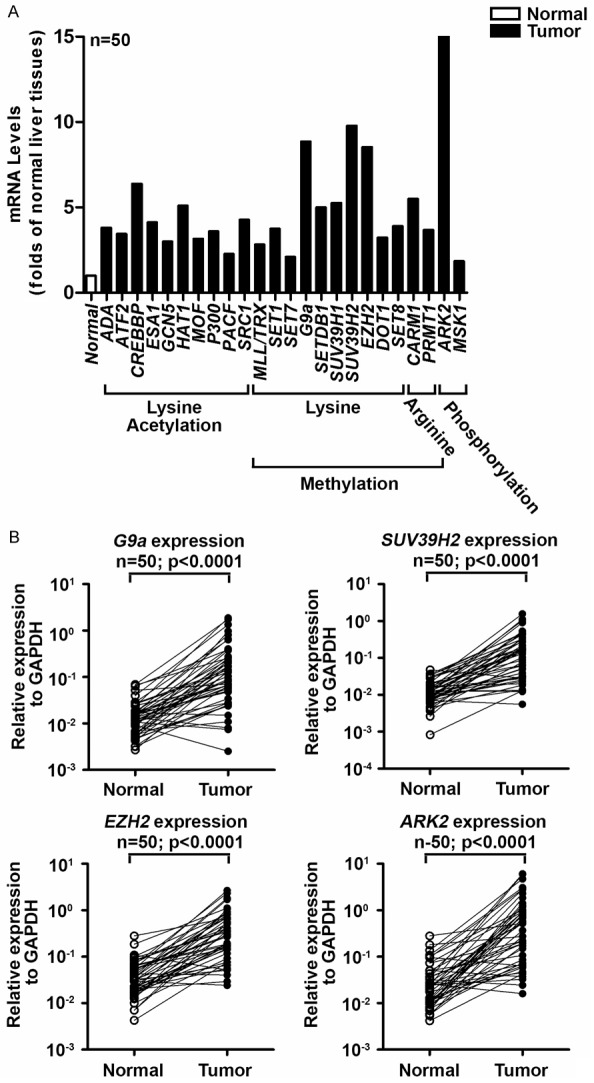
Enhanced mRNA expression levels of 24 histone-modifying genes in tumorous liver tissues of 50 HCC patients. Twenty-four histone-modifying genes including acetylation of lysine, methylation of lysine, methylation of arginine, and phosphorylation of serine/threonine were selected for RT-qPCR study. A: RT-qPCR shows all 24 genes significantly up-regulated in tumorous versus non-tumorous tissues of liver in 50 HCC patients (P < 0.05 in all 24 genes). B: G9a, SUV39H2, EZH2, and ARK2 were more than eightfold up-regulated in timorous tissues of fifty HCC patients. Gene expression is presented as relative expression to GAPDH for each paired liver tissues.
Increase protein expressions of ARK2, EZH2, G9a, and SUV39H2 in tumors
Since mRNAs of ARK2, EZH2, G9a, and SUV39H2 were more than eightfold overexpressed in tumor tissues of 50 HCC patients. We then studied protein expressions of ARK2, EZH2, G9a and SUV39H2 in 50 HCC patients by IHC staining on tissue microarray. Figure 2 shows the typical staining patterns of ARK2, EZH2, G9a, and SUV39H2 in respective normal and tumor tissues from HCC patients. We found that protein levels of ARK2, EZH2, G9a, and SUV39H2 were increase only in tumor but not normal tissues. These results concur with our mRNA expression data.
Figure 2.
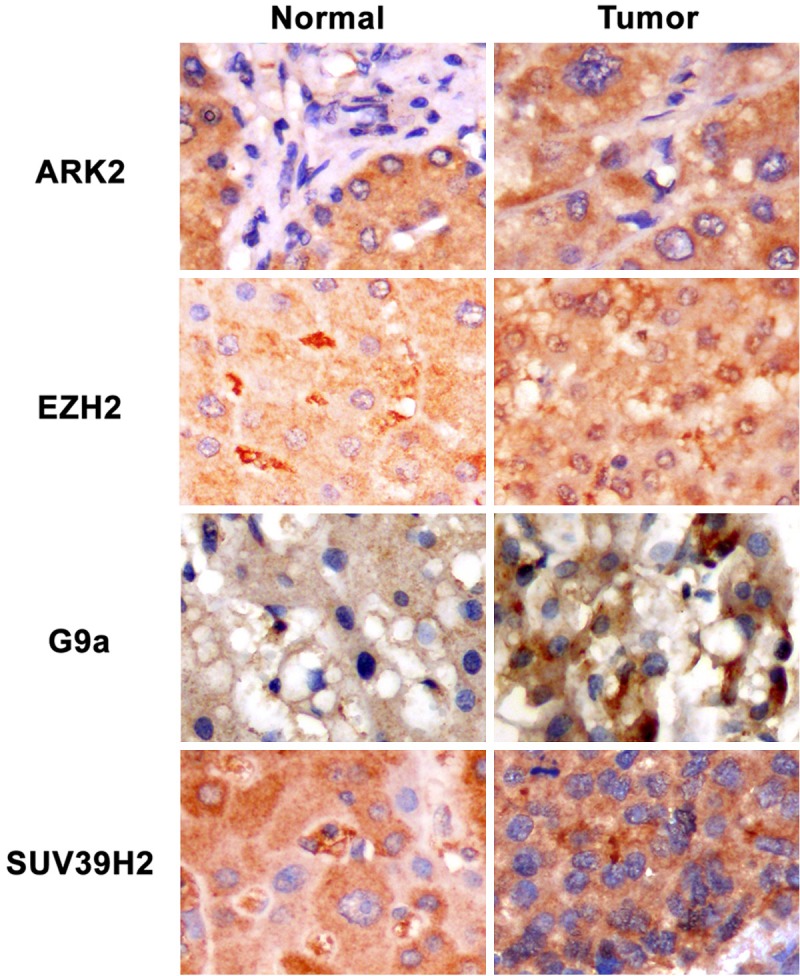
Tissue microarray-based immunohistochemical staining patterns of four histone-modifying proteins. Immunohistochemical staining results of ARK2, EZH2, G9a, and SUV39H2 in tissues from hepatocellular carcinoma (HCC) patients. Original magnification, ×400.
Association of ARK2, EZH2, G9a, and SUV39H2 protein levels with clinicopathological parameters
Table 3 shows relationship between protein intensity of ARK2 or EZH2 and clinicopathological parameters of 50 HCC patients. ARK2 and EZH2 intensity in normal and tumor liver tissues were not significant associated with any clinicopathological parameters: i.e., tumor size, grade, stage, survival, HBV infection, HCV infection, virus infection, and cirrhosis. We then restricted the analysis to ARK2 and EZH2 intensity in tumor tissues and found EZH2 but not ARK2 intensity in tumor tissues associated with survival (P = 0.015; Table 4). Table 5 shows the relationships between G9a and SUV39H2 intensity and clinicopathological parameters in 50 HCC patients; SUV39H2 intensity was associated with HCV infection (P = 0.025); G9 intensity was not linked with any clinicopathological parameters: e.g., tumor size, grade, stage, survival, virus infection, and cirrhosis. If we further restricted the analysis to G9a and SUV39H2 intensity in tumors, we found SUV39H2 but not G9a intensity associated with tumor stage (P = 0.044; Table 6).
Table 3.
Correction of ARK2 and EZH2 protein intensity with clinicopathological parameters in 50 Taiwanese patients with HCC
| Characteristics | ARK2 | EZH2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Tumor ≥ Normal | Tumor < Normal | Total | P-value | Tumor ≥ Normal | Tumor < Normal | Total | p-value | ||
| Tumor Size | ≤ 2 cm | 1 | 5 | 6 | 1.000 | 0 | 6 | 6 | 1.000 |
| > 2 cm | 4 | 28 | 32 | 1 | 30 | 31 | |||
| Grade | Well | 0 | 4 | 4 | 0.309 | 0 | 3 | 3 | 0.827 |
| Moderate | 5 | 22 | 27 | 1 | 26 | 27 | |||
| Poor | 0 | 7 | 7 | 0 | 7 | 7 | |||
| Stage | I, II | 4 | 17 | 21 | 0.349 | 1 | 20 | 21 | 0.474 |
| III, IV | 1 | 17 | 18 | 1 | 17 | 18 | |||
| Survival | ≤ 2 years | 1 | 16 | 17 | 0.363 | 1 | 16 | 17 | 0.447 |
| > 2 years | 4 | 18 | 22 | 0 | 21 | 21 | |||
| HBV infection | No | 2 | 10 | 12 | 0.594 | 0 | 12 | 12 | 0.647 |
| Yes | 2 | 21 | 23 | 1 | 21 | 22 | |||
| HCV infection | No | 1 | 19 | 20 | 0.303 | 0 | 19 | 19 | 0.458 |
| Yes | 3 | 13 | 16 | 1 | 15 | 16 | |||
| Virus infection | No | 0 | 2 | 2 | 1.000 | 0 | 2 | 2 | 1.000 |
| Yes | 4 | 31 | 35 | 1 | 33 | 34 | |||
| Cirrhosis | No | 1 | 15 | 16 | 0.618 | 1 | 15 | 16 | 0.444 |
| Yes | 3 | 18 | 21 | 0 | 20 | 20 | |||
Table 4.
Correction of ARK2 and EZH2 protein intensity in tumor tissues with clinicopathological parameters in 50 Taiwanese patients with HCC
| Characteristics | ARK2 in tumor | EZH2 in tumor | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| ≤ 1+ | ≥ 2+ | Total | P-value | ≤ 1+ | ≥ 2+ | Total | P-value | ||
| Tumor Size | ≤ 2 cm | 2 | 4 | 6 | 1.000 | 2 | 4 | 6 | 0.668 |
| > 2 cm | 11 | 24 | 35 | 17 | 18 | 35 | |||
| Stage | I | 3 | 4 | 7 | 0.780 | 3 | 4 | 7 | 0.344 |
| II | 3 | 11 | 14 | 4 | 10 | 14 | |||
| III | 4 | 9 | 13 | 8 | 5 | 13 | |||
| IV | 3 | 6 | 9 | 5 | 4 | 9 | |||
| Grade | Well | 2 | 2 | 4 | 0.578 | 1 | 3 | 4 | 0.635 |
| Moderate | 8 | 22 | 30 | 15 | 15 | 30 | |||
| Poor | 3 | 5 | 8 | 4 | 4 | 8 | |||
| Survival | ≤ 2 years | 7 | 14 | 21 | 0.747 | 14 | 7 | 21 | 0.015* |
| > 2 years | 6 | 16 | 22 | 6 | 16 | 22 | |||
p < 0.05.
Table 5.
Correction of G9a and SUV39H2 protein intensity with clinicopathological parameters in 50 Taiwanese patients with HCC
| Characteristics | G9a | SUV39H2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Tumor ≥ Normal | Tumor < Normal | Total | P-value | Tumor ≥ Normal | Tumor < Normal | Total | P-value | ||
| Tumor Size | ≤ 2 cm | 2 | 4 | 6 | 1.000 | 2 | 4 | 6 | 1.000 |
| > 2 cm | 10 | 20 | 30 | 8 | 20 | 28 | |||
| Grade | Well | 1 | 2 | 3 | 0.108 | 1 | 3 | 4 | 0.710 |
| Moderate | 11 | 15 | 26 | 8 | 16 | 24 | |||
| Poor | 0 | 7 | 7 | 1 | 5 | 6 | |||
| Stage | I, II | 7 | 12 | 19 | 0.728 | 7 | 12 | 19 | 0.285 |
| III, IV | 5 | 13 | 18 | 3 | 13 | 16 | |||
| Survival | ≤ 2 years | 5 | 12 | 17 | 1.000 | 4 | 11 | 15 | 1.000 |
| > 2 years | 7 | 13 | 20 | 6 | 14 | 20 | |||
| HBV infection | No | 5 | 6 | 11 | 0.434 | 5 | 7 | 12 | 0.24 |
| Yes | 6 | 17 | 23 | 4 | 16 | 20 | |||
| HCV infection | No | 5 | 16 | 21 | 0.153 | 2 | 17 | 19 | 0.025* |
| Yes | 7 | 7 | 14 | 7 | 8 | 15 | |||
| Virus infection | No | 0 | 2 | 2 | 0.536 | 0 | 2 | 2 | 1.000 |
| Yes | 12 | 21 | 33 | 9 | 22 | 31 | |||
| Cirrhosis | No | 4 | 11 | 15 | 0.721 | 3 | 12 | 15 | 0.451 |
| Yes | 7 | 13 | 20 | 7 | 12 | 19 | |||
p < 0.05.
Table 6.
Correction of G9a and SUV39H2 proteins expression levels in tumor tissues with clinicopathological parameters in 50 Taiwanese patients with HCC
| Characteristics | G9a in tumor | SUV39H2 in tumor | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| ≤ 1+ | ≥ 2+ | Total | P-value | No | Yes | Total | P-value | ||
| Tumor Size | ≤ 2 cm | 1 | 5 | 6 | 1.000 | 2 | 4 | 6 | 0.206 |
| > 2 cm | 6 | 29 | 35 | 4 | 31 | 35 | |||
| Stage | I | 2 | 5 | 7 | 0.143 | 3 | 4 | 7 | 0.044* |
| II | 0 | 14 | 14 | 0 | 14 | 14 | |||
| III | 2 | 11 | 13 | 1 | 12 | 13 | |||
| IV | 3 | 6 | 9 | 2 | 7 | 9 | |||
| Grade | Well | 0 | 4 | 4 | 0.170 | 0 | 4 | 4 | 0.098 |
| Moderate | 4 | 26 | 30 | 3 | 27 | 30 | |||
| Poor | 3 | 5 | 8 | 3 | 5 | 8 | |||
| Survival | ≤ 2 years | 5 | 16 | 21 | 0.240 | 3 | 18 | 21 | 1.000 |
| > 2 years | 2 | 20 | 22 | 3 | 19 | 22 | |||
p < 0.05.
Discussion
In 2012, HCC ranked as second leading cause of cancer-related deaths in Taiwan (Department of Health, Executive Yuan). The hepatitis B vaccination program launched in 1984 has successfully reduced HCC incidence in children, yet incidence and mortality in the general Taiwanese population remain high (overall 5-year survival rate was 15% during 1987-1992) and lack diagnostic markers for early detection [30-32]. Histones originally believed to function as a scaffold for DNA packing, have now emerged in posttranslational modifications that regulated chromatin condensation and DNA accessibility. Histone modifications affect chromatin structure further gene expression, and play a vital role in establishment of gene silencing during tumorigenesis [33]. N-terminal tails of histone proteins are subject to a wide range of covalent modification at many sites. Over 60 residues on histones are modified; the most studied are acetylation and methylation of specific lysine residues on histone H3 and H4 [34]. Kondo et al. showed that multiple epigenetic silencing mechanisms inappropriately active in HCC cells and mRNAs of histone methyltransferases-EZH2 and G9a (but not SUV39H1) higher in malignant liver tissues of 23 HCC patients of Japan [25]. Suggesting histone methylations contribute to gene silencing in HCC. In this report, we have studied four groups of histone modifying genes including lysine acetylation, lysine methylation, arginine methylation, serine/threonine phosphorylation. This is the first report discussing expressions of 24 histone-modifying genes in hepatocarcinogenesis.
To assess histone-modifying genes from mRNA to protein levels, both mRNAs and proteins were measured in tissue pairs by RT-qPCR and tissue microarray-based immunohistochemistry (TMA-based IHC) staining. Since RT-qPCR accurately monitors mRNA expressions and immunohistochemistry staining allowed us to generate staining profiles for various antibodies specific to the same fixation and staining procedures for 40 cores normal and tumor tissues from HCC patients on the same slide. Although immunohistochemistry staining is essential for diagnostic pathology, it exhibits inconsistency of quality assurance in data interpretation. Despite widespread use of immunohistochemistry, significant problems remain with regard to variability in tissue fixation, processing, staining methodologies and reagents, and interpretation of staining results persists between different slides [35]. Combining RT-qPCR and immunohistochemistry staining in this study, we monitor histone-modifying gene’s mRNA expression and its’ coding protein level to glean more information to interpret our data.
Besides the well-known alteration of histone acetylation patterns, cancer cells also display widespread changes in histone phosphorylation and methylation patterns [24,36-39]. We selected genes that showed more than eightfold overexpression in tumor tissues for further immunohistochemistry staining: histone phosphorylation protein (ARK2) and methylation proteins (G9a, EZH2 and SUV39H2). We previously showed that overexpression of histone methylation- and phosphorylation-related proteins-ARK2, G9a, EZH2 (but not SUV39H2) associated with prognosis of oral squamous cell carcinoma in 215 male of Taiwan [40]. ARK2 may serve as both an effective prognostic factor and a biomarker for predicting various clinical outcomes of oral cancer [40]. In the present report, our data shows all mRNAs of 24 histone-modifying genes increasing in tumor tissues, suggesting that histone modification (includes acetylation of lysine, methylation of lysine, methylation of arginine, and phosphorylation of serine/threonine) plays a lead role in HCC carcinogenesis. Within these 24 genes, mRNAs of G9a, SUV39H2, EZH2, and ARK2 were more than eightfold overexpressed in tumor tissues. In spite of mRNAs expression, we found proteins of ARK2, EZH2, G9a, and SUV39H2 consistently up-regulated in tumors of 50 HCC patients.
ARK2 (a kinase for H3S10) overexpression proves associated with stages of malignant progression in thyroid carcinomas and with poor prognosis in endometrial carcinomas [13,41]. Lin et al. showed that ARK2 mRNA frequent overexpressed in 160 Taiwanese HCC cases, which can be used as an important molecular marker of early recurrence and poor prognosis [18]. In addition, they suggest that ARK2 selected inhibitors-AZD1152-HQPA and VE-465 had anticancer effects in HCC cells [18,19]. Sorafenib (Nexavar®) is an orally active multikinase inhibitor approved in Europe for treatment of HCC, showing greater survival duration in combination therapy with doxorubicin in advanced HCC [42]. We found mRNA and protein of ARK2 were both overexpressed in 50 HCCs, yet staining intensity of ARK2 not correlated with any clinicopathologic characteristics. Possible reasons of this variation may be differences in selected antibody, sample size, genetic background, and/or risk factors between selected populations.
The polycomb group protein-EZH2 functions as a histone methyltransferase for H3K27 (histone H3 lysine 27) as catalytic subunit of polycomb repressive complex 2 (PRC2) and mediates transcription silencing [43]. Increased expression of EZH2 is frequently detected in HCC tissues and it is associated with the aggressiveness and/or poor prognosis [44-46]. Knockdown of EZH2 expression in HCC cells could reverse tumorigenicity in mice, which suggests that EZH2 inhibition has therapeutic value in HCC [47]. In addition, EZH2 expression, as examined by IHC, has been correlated with aggressiveness and poor prognosis of HCC in the China population, indicating EZH2 as a diagnostic biomarker for HCC [23]. Our results prove EZH2 intensity of tumor tissues also associated with survival in the 50 HCC patients, such that EZH2 might serve as an efficient prognostic biomarker.
Histone H3K9 di-methylation (H3K9me2) and tri-methylation (H3K9me3) can be mediated by histone methyltransferase (HMT)-G9a and SUV39H1, respectively. G9a promotes lung cancer cell invasion and may play an early role in metastasis cascade [48]. Nuclear intensity of G9a protein correlates with reduced overall survival and disease-free interval in lung cancer [48]. Kondo et al. showed mRNA expressions of EZH2 and G9a but not SUV39H1 were higher in cancerous tissues of 23 HCC patients in Japan [25]. We found both mRNA and protein expressions of ARK2, EZH2, G9a, and SUV39H2 in tumor tissues significantly enhanced, suggesting these histone methylation- and phosphorylation-related genes involves in hepatocarcinogenesis. But G9a protein intensity from immunohistochemistry staining shows no link with clinicopathological parameters in 50 HCC cases. On the other hand, SUV39H2 intensity correlated with HCV infection and tumor stage (the intensity in tumor tissues). Ours is the first report to link SUV39H2 expression with HCV infection and tumor stage in HCC cases.
This article focuses on markers of histone methylation and phosphorylation proteins: ARK2, G9a, EZH2, and SUV39H2. Findings suggest EZH2 and SUV39H2 as highly correlated with survival and tumor stage, respectively, and may yield important biomarkers that predict patient survival and prognosis in HCC patients of Taiwan.
Acknowledgements
This work was supported by the grant from CMU Hospital (DMR-103-047).
Disclosure of conflict of interest
None.
References
- 1.Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212–236. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 3.Maluccio M, Covey A. Recent progress in understanding, diagnosing, and treating hepatocellular carcinoma. CA Cancer J Clin. 2012;62:394–399. doi: 10.3322/caac.21161. [DOI] [PubMed] [Google Scholar]
- 4.El-Serag HB. Hepatocellular carcinoma: an epidemiologic view. J Clin Gastroenterol. 2002;35:S72–78. doi: 10.1097/00004836-200211002-00002. [DOI] [PubMed] [Google Scholar]
- 5.Song do S, Bae SH. Changes of guidelines diagnosing hepatocellular carcinoma during the last ten-year period. Clin Mol Hepatol. 2012;18:258–267. doi: 10.3350/cmh.2012.18.3.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kornberg RD, Lorch Y. Twenty-five years of the nucleosome, fundamental particle of the eukaryote chromosome. Cell. 1999;98:285–294. doi: 10.1016/s0092-8674(00)81958-3. [DOI] [PubMed] [Google Scholar]
- 7.Bird A. Perceptions of epigenetics. Nature. 2007;447:396–398. doi: 10.1038/nature05913. [DOI] [PubMed] [Google Scholar]
- 8.Herceg Z, Paliwal A. Epigenetic mechanisms in hepatocellular carcinoma: how environmental factors influence the epigenome. Mutat Res. 2011;727:55–61. doi: 10.1016/j.mrrev.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 9.Dawson MA, Kouzarides T. Cancer epigenetics: from mechanism to therapy. Cell. 2012;150:12–27. doi: 10.1016/j.cell.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 10.Arrowsmith CH, Bountra C, Fish PV, Lee K, Schapira M. Epigenetic protein families: a new frontier for drug discovery. Nat Rev Drug Discov. 2012;11:384–400. doi: 10.1038/nrd3674. [DOI] [PubMed] [Google Scholar]
- 11.Jones PA, Baylin SB. The epigenomics of cancer. Cell. 2007;128:683–692. doi: 10.1016/j.cell.2007.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feinberg AP. Phenotypic plasticity and the epigenetics of human disease. Nature. 2007;447:433–440. doi: 10.1038/nature05919. [DOI] [PubMed] [Google Scholar]
- 13.Sorrentino R, Libertini S, Pallante PL, Troncone G, Palombini L, Bavetsias V, Spalletti-Cernia D, Laccetti P, Linardopoulos S, Chieffi P, Fusco A, Portella G. Aurora B overexpression associates with the thyroid carcinoma undifferentiated phenotype and is required for thyroid carcinoma cell proliferation. J Clin Endocrinol Metab. 2005;90:928–935. doi: 10.1210/jc.2004-1518. [DOI] [PubMed] [Google Scholar]
- 14.Taby R, Issa JP. Cancer epigenetics. CA Cancer J Clin. 2010;60:376–392. doi: 10.3322/caac.20085. [DOI] [PubMed] [Google Scholar]
- 15.Sharma S, Kelly TK, Jones PA. Epigenetics in cancer. Carcinogenesis. 2010;31:27–36. doi: 10.1093/carcin/bgp220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keen N, Taylor S. Aurora-kinase inhibitors as anticancer agents. Nat Rev Cancer. 2004;4:927–936. doi: 10.1038/nrc1502. [DOI] [PubMed] [Google Scholar]
- 17.Jeng YM, Peng SY, Lin CY, Hsu HC. Overexpression and amplification of Aurora-A in hepatocellular carcinoma. Clin Cancer Res. 2004;10:2065–2071. doi: 10.1158/1078-0432.ccr-1057-03. [DOI] [PubMed] [Google Scholar]
- 18.Lin ZZ, Jeng YM, Hu FC, Pan HW, Tsao HW, Lai PL, Lee PH, Cheng AL, Hsu HC. Significance of Aurora B overexpression in hepatocellular carcinoma. Aurora B Overexpression in HCC. BMC Cancer. 2010;10:461. doi: 10.1186/1471-2407-10-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin ZZ, Hsu HC, Hsu CH, Yeh PY, Huang CY, Huang YF, Chen TJ, Kuo SH, Hsu C, Hu FC, Jeng YM, Chung Y, Cheng AL. The Aurora kinase inhibitor VE-465 has anticancer effects in pre-clinical studies of human hepatocellular carcinoma. J Hepatol. 2009;50:518–527. doi: 10.1016/j.jhep.2008.10.022. [DOI] [PubMed] [Google Scholar]
- 20.Rice JC, Briggs SD, Ueberheide B, Barber CM, Shabanowitz J, Hunt DF, Shinkai Y, Allis CD. Histone methyltransferases direct different degrees of methylation to define distinct chromatin domains. Mol Cell. 2003;12:1591–1598. doi: 10.1016/s1097-2765(03)00479-9. [DOI] [PubMed] [Google Scholar]
- 21.Tachibana M, Sugimoto K, Nozaki M, Ueda J, Ohta T, Ohki M, Fukuda M, Takeda N, Niida H, Kato H, Shinkai Y. G9a histone methyltransferase plays a dominant role in euchromatic histone H3 lysine 9 methylation and is essential for early embryogenesis. Genes Dev. 2002;16:1779–1791. doi: 10.1101/gad.989402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simon JA, Tamkun JW. Programming off and on states in chromatin: mechanisms of Polycomb and trithorax group complexes. Curr Opin Genet Dev. 2002;12:210–218. doi: 10.1016/s0959-437x(02)00288-5. [DOI] [PubMed] [Google Scholar]
- 23.Cai MY, Tong ZT, Zheng F, Liao YJ, Wang Y, Rao HL, Chen YC, Wu QL, Liu YH, Guan XY, Lin MC, Zeng YX, Kung HF, Xie D. EZH2 protein: a promising immunomarker for the detection of hepatocellular carcinomas in liver needle biopsies. Gut. 2011;60:967–976. doi: 10.1136/gut.2010.231993. [DOI] [PubMed] [Google Scholar]
- 24.Peters AH, O’Carroll D, Scherthan H, Mechtler K, Sauer S, Schofer C, Weipoltshammer K, Pagani M, Lachner M, Kohlmaier A, Opravil S, Doyle M, Sibilia M, Jenuwein T. Loss of the Suv39h histone methyltransferases impairs mammalian heterochromatin and genome stability. Cell. 2001;107:323–337. doi: 10.1016/s0092-8674(01)00542-6. [DOI] [PubMed] [Google Scholar]
- 25.Kondo Y, Shen L, Suzuki S, Kurokawa T, Masuko K, Tanaka Y, Kato H, Mizuno Y, Yokoe M, Sugauchi F, Hirashima N, Orito E, Osada H, Ueda R, Guo Y, Chen X, Issa JP, Sekido Y. Alterations of DNA methylation and histone modifications contribute to gene silencing in hepatocellular carcinomas. Hepatol Res. 2007;37:974–983. doi: 10.1111/j.1872-034X.2007.00141.x. [DOI] [PubMed] [Google Scholar]
- 26.Fan DN, Tsang FH, Tam AH, Au SL, Wong CC, Wei L, Lee JM, He X, Ng IO, Wong CM. Histone lysine methyltransferase, suppressor of variegation 3-9 homolog 1, promotes hepatocellular carcinoma progression and is negatively regulated by microRNA-125b. Hepatology. 2013;57:637–647. doi: 10.1002/hep.26083. [DOI] [PubMed] [Google Scholar]
- 27.Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17:1471–1474. doi: 10.1245/s10434-010-0985-4. [DOI] [PubMed] [Google Scholar]
- 28.Liu TC, Lin SF, Chang JG, Yang MY, Hung SY, Chang CS. Epigenetic alteration of the SOCS1 gene in chronic myeloid leukaemia. Br J Haematol. 2003;123:654–661. doi: 10.1046/j.1365-2141.2003.04660.x. [DOI] [PubMed] [Google Scholar]
- 29.Hofmann M, Stoss O, Shi D, Buttner R, van de Vijver M, Kim W, Ochiai A, Ruschoff J, Henkel T. Assessment of a HER2 scoring system for gastric cancer: results from a validation study. Histopathology. 2008;52:797–805. doi: 10.1111/j.1365-2559.2008.03028.x. [DOI] [PubMed] [Google Scholar]
- 30.Lee CL, Ko YC, Choong CS. Survival rate for liver cancer in Taiwan. Zhonghua Yi Xue Za Zhi (Taipei) 2000;63:16–20. [PubMed] [Google Scholar]
- 31.Shyu HJ, Lung CC, Ho CC, Sun YH, Ko PC, Huang JY, Pan CC, Chiang YC, Chen SC, Liaw YP. Geographic patterns of hepatocellular carcinoma mortality with exposure to iron in groundwater in Taiwanese population: an ecological study. BMC Public Health. 2013;13:352. doi: 10.1186/1471-2458-13-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang MH, Chen CJ, Lai MS, Hsu HM, Wu TC, Kong MS, Liang DC, Shau WY, Chen DS. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. Taiwan Childhood Hepatoma Study Group. N Engl J Med. 1997;336:1855–1859. doi: 10.1056/NEJM199706263362602. [DOI] [PubMed] [Google Scholar]
- 33.Jones PA, Baylin SB. The fundamental role of epigenetic events in cancer. Nat Rev Genet. 2002;3:415–428. doi: 10.1038/nrg816. [DOI] [PubMed] [Google Scholar]
- 34.Kouzarides T. Chromatin modifications and their function. Cell. 2007;128:693–705. doi: 10.1016/j.cell.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 35.Hsu FD, Nielsen TO, Alkushi A, Dupuis B, Huntsman D, Liu CL, van de Rijn M, Gilks CB. Tissue microarrays are an effective quality assurance tool for diagnostic immunohistochemistry. Mod Pathol. 2002;15:1374–1380. doi: 10.1097/01.MP.0000039571.02827.CE. [DOI] [PubMed] [Google Scholar]
- 36.Nguyen CT, Weisenberger DJ, Velicescu M, Gonzales FA, Lin JC, Liang G, Jones PA. Histone H3-lysine 9 methylation is associated with aberrant gene silencing in cancer cells and is rapidly reversed by 5-aza-2’-deoxycytidine. Cancer Res. 2002;62:6456–6461. [PubMed] [Google Scholar]
- 37.Kondo Y, Shen L, Ahmed S, Boumber Y, Sekido Y, Haddad BR, Issa JP. Downregulation of histone H3 lysine 9 methyltransferase G9a induces centrosome disruption and chromosome instability in cancer cells. PLoS One. 2008;3:e2037. doi: 10.1371/journal.pone.0002037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Valk-Lingbeek ME, Bruggeman SW, van Lohuizen M. Stem cells and cancer; the polycomb connection. Cell. 2004;118:409–418. doi: 10.1016/j.cell.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 39.Kondo Y, Shen L, Cheng AS, Ahmed S, Boumber Y, Charo C, Yamochi T, Urano T, Furukawa K, Kwabi-Addo B, Gold DL, Sekido Y, Huang TH, Issa JP. Gene silencing in cancer by histone H3 lysine 27 trimethylation independent of promoter DNA methylation. Nat Genet. 2008;40:741–750. doi: 10.1038/ng.159. [DOI] [PubMed] [Google Scholar]
- 40.Chen JH, Yeh KT, Yang YM, Chang JG, Lee HE, Hung SY. High expressions of histone methylation- and phosphorylation-related proteins are associated with prognosis of oral squamous cell carcinoma in male population of Taiwan. Med Oncol. 2013;30:513. doi: 10.1007/s12032-013-0513-z. [DOI] [PubMed] [Google Scholar]
- 41.Kurai M, Shiozawa T, Shih HC, Miyamoto T, Feng YZ, Kashima H, Suzuki A, Konishi I. Expression of Aurora kinases A and B in normal, hyperplastic, and malignant human endometrium: Aurora B as a predictor for poor prognosis in endometrial carcinoma. Hum Pathol. 2005;36:1281–1288. doi: 10.1016/j.humpath.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 42.Keating GM, Santoro A. Sorafenib: a review of its use in advanced hepatocellular carcinoma. Drugs. 2009;69:223–240. doi: 10.2165/00003495-200969020-00006. [DOI] [PubMed] [Google Scholar]
- 43.Cao R, Wang L, Wang H, Xia L, Erdjument-Bromage H, Tempst P, Jones RS, Zhang Y. Role of histone H3 lysine 27 methylation in Polycomb-group silencing. Science. 2002;298:1039–1043. doi: 10.1126/science.1076997. [DOI] [PubMed] [Google Scholar]
- 44.Sudo T, Utsunomiya T, Mimori K, Nagahara H, Ogawa K, Inoue H, Wakiyama S, Fujita H, Shirouzu K, Mori M. Clinicopathological significance of EZH2 mRNA expression in patients with hepatocellular carcinoma. Br J Cancer. 2005;92:1754–1758. doi: 10.1038/sj.bjc.6602531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sasaki M, Ikeda H, Itatsu K, Yamaguchi J, Sawada S, Minato H, Ohta T, Nakanuma Y. The overexpression of polycomb group proteins Bmi1 and EZH2 is associated with the progression and aggressive biological behavior of hepatocellular carcinoma. Lab Invest. 2008;88:873–882. doi: 10.1038/labinvest.2008.52. [DOI] [PubMed] [Google Scholar]
- 46.Yonemitsu Y, Imazeki F, Chiba T, Fukai K, Nagai Y, Miyagi S, Arai M, Aoki R, Miyazaki M, Nakatani Y, Iwama A, Yokosuka O. Distinct expression of polycomb group proteins EZH2 and BMI1 in hepatocellular carcinoma. Hum Pathol. 2009;40:1304–1311. doi: 10.1016/j.humpath.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 47.Chen Y, Lin MC, Yao H, Wang H, Zhang AQ, Yu J, Hui CK, Lau GK, He ML, Sung J, Kung HF. Lentivirus-mediated RNA interference targeting enhancer of zeste homolog 2 inhibits hepatocellular carcinoma growth through down-regulation of stathmin. Hepatology. 2007;46:200–208. doi: 10.1002/hep.21668. [DOI] [PubMed] [Google Scholar]
- 48.Chen MW, Hua KT, Kao HJ, Chi CC, Wei LH, Johansson G, Shiah SG, Chen PS, Jeng YM, Cheng TY, Lai TC, Chang JS, Jan YH, Chien MH, Yang CJ, Huang MS, Hsiao M, Kuo ML. H3K9 histone methyltransferase G9a promotes lung cancer invasion and metastasis by silencing the cell adhesion molecule Ep-CAM. Cancer Res. 2010;70:7830–7840. doi: 10.1158/0008-5472.CAN-10-0833. [DOI] [PubMed] [Google Scholar]


