ABSTRACT
BACKGROUND
While the potential of patient-centered medical homes (PCMH) is promising, little is known empirically about the frontline challenges that primary care (PC) leaders face before making the decision to implement PCMH, let alone in making it a reality.
OBJECTIVE
Prior to the design and implementation of the Veterans Health Administration’s (VA) national PCMH model—Patient Aligned Care Teams (PACT)—we identified the top challenges faced by PC directors and examined the organizational and area level factors that influenced those challenges.
DESIGN AND PARTICIPANTS
A national cross-sectional key informant organizational survey was fielded to the census of PC directors at VA medical centers and large community-based outpatient clinics (final sample n = 229 sites).
MAIN MEASURES
PC directors were asked to rate the degree to which they faced 48 management challenges in eight PCMH-related domains (access, preventive care, chronic diseases requiring care in PC, challenging medical conditions, mental health/substance abuse, special populations, PC coordination of care, and clinical informatics). Responses were dichotomized as moderately-to-extremely challenging versus somewhat-slightly-not at all challenging. Items were rank ordered; chi square or regression techniques were used to examine variations in facility size, type, urban/rural location, and region.
KEY RESULTS
On average, VA PC directors reported 16 moderate-to-extreme challenges, and the top 20 challenges spanned all eight PCMH domains. Four of the top 20 challenges, including the top two challenges, were from the clinical informatics domain. Management of chronic non-malignant pain requiring opiate therapy was the third most reported challenge nationwide. Significant organizational and area level variations in reported challenges were found especially for care coordination.
CONCLUSIONS
Better understanding of PC challenges ahead of PCMH implementation provides important context for strategic planning and redesign efforts. As a national healthcare system, the VA provides a unique opportunity to examine organizational and area determinants relevant to other PCMH models.
KEY WORDS: primary care, patient-centered medical home, Veterans, VA healthcare system, health care management
INTRODUCTION
American primary care (PC) delivery is at a crossroads. An ever-increasing proportion of medical trainees are moving into specialty care, while current PC providers are leaving practice at an increased rate in the face of dwindling reimbursements.1,2 Experts point to a "perfect storm" of increased work with decreased rewards, and predict the impending "collapse of primary care" in the absence of real solutions.1,3 Patient-centered medical homes (PCMH) represent an updated PC model that recognizes and rewards, through appropriate payment, the diverse but necessary activities of establishing a PC base for a population of patients.4,5 Most major medical societies and healthcare funders have endorsed some version of the PCMH concept, while an array of demonstration projects are underway in public and private health care settings.6 The ability of the Affordable Care Act (ACA) to improve U.S. health care delivery while reducing costs will likely rely in large part on the success of care models like the medical home as a response to the threats to PC delivery as the hub of an effective national health care system. For better or worse, already over-stretched PC physicians are the heart of these changes.7
While the promise and potential of PCMH is great, little is known empirically about the frontline challenges that PC leaders face before making the decision to implement PCMH. Early evidence from PCMH demonstrations suggests that implementation is challenging at best, requiring much more than payment reform and a menu of discrete changes to be successful.8–10 In fact, the complexity underlying achievement of medical homes may be out of reach of many PC practices,11 especially those without electronic health records, data systems, access to care managers, structured practice facilitation, and other key elements.12–15 Findings from widely publicized medical home efforts, such as those at Geisinger, Intermountain and Group Health, suggest early provider burnout and significant challenges in operationalizing the tenets of PCMH in diverse settings, yet have nonetheless managed to accomplish important process and outcome changes.16 What is missing from the literature is what these PC challenges look like ahead of PCMH implementation. What are the top challenges that PC leaders face heading into PCMH? What organizational or area factors influence the challenges they face? And what are their implications for PCMH implementation?
We address these questions in the Veterans Health Administration (VA), the largest integrated healthcare delivery system in the U.S., with hospital-based and freestanding PC clinics spanning all 50 U.S. states and several territories. Prior to the design and implementation of VA’s national PCMH model—Patient Aligned Care Teams (or PACTs)—VA PC leadership partnered with health services researchers to design and field a survey among the PC directors at all VA medical centers (VAMCs) and large community-based outpatient clinics (CBOCs) to gauge the challenges that frontline PC leaders were facing in delivering PC to our nation’s Veterans ahead of PACT implementation.
METHODS
Design and Participants
This project was designed as a national cross-sectional key informant organizational survey, the National VA Primary Care Survey (2008–2009), to the census of PC directors at VAMCs and CBOCs that served 4,000 or more outpatients and delivered 20,000 or more PC visits in the previous year (N = 248 geographically distinct sites).
Survey Design and Measures
Survey content was driven by operational issues identified by national VA PC leadership, anticipating PC management challenges to better design policy and practice improvement initiatives. The team conducted interviews with PC leaders and used items from prior organizational survey instruments.17–19 The survey was piloted and cognitive interviews with regional PC leaders, network leaders, and frontline practice PC directors were conducted to review content and improve construct validity. Surveys were fielded using email contacts to PC directors with embedded links to the resulting web-based survey instrument. A two-week turnaround was requested, with email reminders and telephone follow-up as needed.20
We asked PC directors to rate the degree to which they faced each of 48 management challenges in the following domains (shown in Table 1): access (four items), preventive care (seven items), chronic diseases requiring care in PC (eight items), challenging medical conditions (three items), mental health (MH)/substance abuse (four items), special populations (four items), PC coordination of care (six items), and clinical informatics (12 items). Response options were a five-point ordinal scale of not at all challenging, slightly challenging, somewhat challenging, moderately challenging, to extremely challenging. We dichotomized responses as moderately-to-extremely challenging (1) versus somewhat-slightly-not at all challenging (0). We also created a count variable, with high values representing PC practices with more challenges.
Table 1.
Percent of Primary Care (PC) Directors Reporting Each as Moderately-to-Extremely Challenging by Site-Level Characteristics (n = 229)
| Challenge to primary care practice: | Total | Facility Type | Facility Size in Thousands | Region | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample n = 229 | VAMC n = 133 | CBOC n = 96 | p† | LT 10 n = 43 | 10–20 n = 61 | 20–30 n = 39 | 30+ n = 86 | p‡ | NE n = 37 | MW n = 57 | S n = 88 | W n = 47 | p‡ | Urban n = 92 | Rural n = 137 | p† | |
| Access: Availability of | |||||||||||||||||
| New patient appointments | 25 % | 23 % | 27 % | 28 % | 21 % | 26 % | 26 % | 19 % | 26 % | 24 % | 30 % | 23 % | 26 % | ||||
| Established patient: return appt | 17 % | 17 % | 17 % | 16 % | 16 % | 13 % | 20 % | 8 % | 14 % | 19 % | 23 % | 13 % | 20 % | ||||
| Established patient: new problem | 24 % | 26 % | 22 % | 14 % | 25 % | 26 % | 28 % | 19 % | 21 % | 26 % | 28 % | 16 % | 29 % | * | |||
| Access to PC team via telephone | 47 % | 51 % | 41 % | 37 % | 43 % | 46 % | 55 % | 51 % | 37 % | 50 % | 49 % | 49 % | 45 % | ||||
| Preventive Care: | |||||||||||||||||
| Colorectal cancer screening | 28 % | 31 % | 24 % | 16 % | 31 % | 23 % | 34 % | * | 27 % | 28 % | 27 % | 30 % | 24 % | 31 % | |||
| Influenza immunizations | 10 % | 11 % | 7 % | 7 % | 8 % | 10 % | 12 % | 5 % | 7 % | 14 % | 9 % | 5 % | 12 % | ||||
| Pneumococcal immunizations | 7 % | 8 % | 6 % | 7 % | 7 % | 13 % | 5 % | 11 % | 5 % | 8 % | 4 % | 5 % | 8 % | ||||
| Tobacco use screening | 7 % | 7 % | 7 % | 7 % | 3 % | 15 % | 6 % | 5 % | 7 % | 7 % | 9 % | 4 % | 9 % | ||||
| Lipid screening | 10 % | 8 % | 13 % | 9 % | 11 % | 10 % | 9 % | 14 % | 5 % | 13 % | 9 % | 11 % | 9 % | ||||
| Breast cancer screening (i.e., mammography) | 18 % | 19 % | 17 % | 19 % | 21 % | 18 % | 15 % | 35 % | 9 % | 13 % | 26 % | * | 20 % | 17 % | |||
| Cervical cancer screening (i.e., paps) | 15 % | 16 % | 15 % | 19 % | 18 % | 13 % | 13 % | 19 % | 12 % | 11 % | 23 % | 13 % | 17 % | ||||
| Chronic Disease Care Requiring Care in PC: | |||||||||||||||||
| Hypertension | 25 % | 25 % | 25 % | 21 % | 26 % | 33 % | 22 % | 27 % | 18 % | 22 % | 38 % | * | 21 % | 28 % | |||
| Diabetes | 38 % | 41 % | 33 % | 28 % | 43 % | 33 % | 41 % | 43 % | 28 % | 38 % | 45 % | 41 % | 35 % | ||||
| Elevated cholesterol | 30 % | 36 % | 22 % | * | 14 % | 34 % | 38 % | 31 % | * | 41 % | 23 % | 30 % | 32 % | 27 % | 32 % | ||
| Coronary artery disease | 10 % | 9 % | 10 % | 7 % | 10 % | 13 % | 9 % | 19 % | 4 % | 11 % | 6 % | 9 % | 10 % | ||||
| Chronic obstructive pulmonary disease | 5 % | 5 % | 5 % | 5 % | 8 % | 3 % | 5 % | 5 % | 2 % | 7 % | 6 % | 1 % | 8 % | * | |||
| Degenerative joint disease | 10 % | 8 % | 13 % | 7 % | 11 % | 8 % | 10 % | 5 % | 2 % | 11 % | 19 % | * | 9 % | 10 % | |||
| Chronic kidney disease | 15 % | 15 % | 16 % | 14 % | 16 % | 23 % | 12 % | 22 % | 9 % | 16 % | 17 % | 13 % | 17 % | ||||
| Peripheral vascular disease | 14 % | 15 % | 14 % | 7 % | 25 % | 21 % | 8 % | * | 19 % | 5 % | 15 % | 21 % | * | 8 % | 19 % | * | |
| Challenging Medical Conditions: | |||||||||||||||||
| Chronic non-malignant pain w/opiate therapy | 71 % | 75 % | 65 % | 51 % | 70 % | 74 % | 79 % | ** | 70 % | 60 % | 75 % | 77 % | 67 % | 73 % | |||
| Dementia | 24 % | 23 % | 24 % | 23 % | 26 % | 26 % | 21 % | 32 % | 14 % | 22 % | 32 % | * | 25 % | 23 % | |||
| Human Immunodeficiency Virus | 14 % | 13 % | 17 % | 9 % | 28 % | 13 % | 8 % | * | 3 % | 12 % | 17 % | 21 % | 8 % | 19 % | * | ||
| Mental Health/Substance Abuse: | |||||||||||||||||
| Depression | 11 % | 11 % | 11 % | 5 % | 12 % | 18 % | 10 % | 6 % | 9 % | 10 % | 17 % | 8 % | 13 % | ||||
| Posttraumatic stress disorder | 19 % | 16 % | 24 % | 28 % | 21 % | 25 % | 12 % | * | 14 % | 14 % | 18 % | 33 % | * | 13 % | 23 % | ||
| Substance abuse | 51 % | 52 % | 51 % | 43 % | 57 % | 50 % | 52 % | 54 % | 44 % | 45 % | 69 % | * | 53 % | 50 % | |||
| Anxiety disorders | 10 % | 10 % | 9 % | 5 % | 11 % | 13 % | 10 % | 9 % | 10 % | 8 % | 13 % | 7 % | 11 % | ||||
| Special Populations: | |||||||||||||||||
| Frail elderly | 28 % | 30 % | 25 % | 30 % | 30 % | 28 % | 26 % | 41 % | 19 % | 25 % | 34 % | 28 % | 28 % | ||||
| Women | 15 % | 15 % | 16 % | 19 % | 20 % | 10 % | 13 % | 22 % | 14 % | 15 % | 13 % | 10 % | 19 % | ||||
| OEF/OIF Veterans | 23 % | 26 % | 20 % | 19 % | 31 % | 18 % | 22 % | 30 % | 18 % | 18 % | 34 % | * | 21 % | 25 % | |||
| Seriously mentally ill | 52 % | 53 % | 51 % | 53 % | 54 % | 51 % | 50 % | 46 % | 51 % | 44 % | 72 % | ** | 55 % | 50 % | |||
| PC Coordination of Care with: | |||||||||||||||||
| Medical specialty outpatient care | 31 % | 28 % | 35 % | 28 % | 54 % | 26 % | 19 % | ** | 30 % | 26 % | 32 % | 36 % | 18 % | 39 % | ** | ||
| Surgical specialty outpatient care | 36 % | 32 % | 41 % | 28 % | 61 % | 36 % | 22 % | ** | 35 % | 26 % | 38 % | 45 % | 23 % | 45 % | ** | ||
| Mental health outpatient specialty care | 18 % | 13 % | 25 % | * | 26 % | 21 % | 18 % | 12 % | * | 11 % | 7 % | 22 % | 30 % | ** | 11 % | 23 % | * |
| Emergency Department | 21 % | 16 % | 28 % | * | 26 % | 28 % | 21 % | 14 % | 22 % | 16 % | 22 % | 26 % | 15 % | 25 % | |||
| Inpatient care | 17 % | 9 % | 29 % | *** | 26 % | 25 % | 13 % | 10 % | * | 19 % | 11 % | 16 % | 28 % | * | 17 % | 18 % | |
| VA and non-VA providers | 56 % | 60 % | 50 % | 51 % | 48 % | 67 % | 60 % | 73 % | 39 % | 56 % | 66 % | ** | 55 % | 57 % | |||
| Clinical Informatics: | |||||||||||||||||
| Volume of CPRS alerts | 75 % | 80 % | 69 % | 67 % | 79 % | 74 % | 77 % | 78 % | 65 % | 77 % | 81 % | 70 % | 79 % | ||||
| Volume of clinical reminders | 80 % | 82 % | 77 % | 77 % | 82 % | 85 % | 78 % | 81 % | 72 % | 80 % | 89 % | * | 76 % | 82 % | |||
| Time and effort to input notes | 60 % | 58 % | 63 % | 49 % | 66 % | 67 % | 58 % | 62 % | 54 % | 63 % | 60 % | 54 % | 64 % | ||||
| Clinical informatics support | 43 % | 42 % | 44 % | 40 % | 51 % | 49 % | 36 % | 54 % | 37 % | 38 % | 51 % | 41 % | 44 % | ||||
| Availability of consultant reports | 18 % | 18 % | 19 % | 19 % | 26 % | 23 % | 10 % | 14 % | 16 % | 23 % | 17 % | 11 % | 23 % | * | |||
| Availability of VA inpatient information | 5 % | 5 % | 6 % | 5 % | 3 % | 13 % | 3 % | 11 % | 4 % | 3 % | 6 % | 7 % | 4 % | ||||
| Availability of VA ER information | 5 % | 4 % | 7 % | 5 % | 5 % | 8 % | 5 % | 5 % | 5 % | 6 % | 4 % | 3 % | 7 % | ||||
| Availability of laboratory test results | 3 % | 5 % | 0 % | * | 0 % | 3 % | 5 % | 2 % | 8 % | 2 % | 1 % | 2 % | 1 % | 4 % | |||
| Availability of diagnostic imaging reports | 3 % | 5 % | 2 % | 2 % | 2 % | 5 % | 5 % | 0 % | 4 % | 5 % | 4 % | 4 % | 3 % | ||||
| Processing & transmission time for CPRS data | 10 % | 9 % | 10 % | 12 % | 10 % | 15 % | 6 % | 3 % | 18 % | 7 % | 11 % | 5 % | 12 % | ||||
| Availability of historic pharmacy data | 10 % | 14 % | 3 % | ** | 5 % | 8 % | 15 % | 10 % | 19 % | 12 % | 7 % | 4 % | * | 8 % | 11 % | ||
| Availability of data from other VAs | 16 % | 17 % | 15 % | 14 % | 13 % | 18 % | 17 % | 24 % | 9 % | 14 % | 21 % | 16 % | 15 % | ||||
OEF/OIF Operation Enduring Freedom/Operation Iraqi Freedom; CPRS Computerized Patient Record System; ER Emergency Room
†Chi Square for Facility Type and Urban/Rural
‡Logistic regression for Facility Size and Region
*p < 0.05, **p < 0.01, ***p < 0.001
We obtained organizational characteristics from VA administrative data sources (e.g., total number of PC patients as a proxy for facility size; VAMC versus CBOC for facility type). We obtained area characteristics from the Area Resource File (2008). We included urban/rural location (large urban as metropolitan areas with a population of 1 million or more versus small city/rural) and U.S. Census region (Northeast, Midwest, South and West).
Statistical Analysis
Analyses were conducted at the PC site-level, consistent with the unit of analysis of the key informant surveys. We rank ordered PC challenges reported to be moderately-to-extremely challenging to identify the top 20 challenges nationwide. We examined variations by organizational and area level characteristics using chi square statistics. We used logistic regression to examine relationships of PC challenges to facility size and region, using smaller practices (< 10,000 patients) and Western region as referents.
RESULTS
Characteristics of VA PC Practices
Of the 248 eligible primary care sites, 229 PC directors responded (92 % response rate), with 58 % representing VAMCs and 42 % CBOCs (Table 2). Practices served an average of about 27,000 PC patients, and 40 % of the sites were in large urban areas. As a national system, respondent facilities were roughly equally dispersed by region.
Table 2.
Description of Sites in Sample (n = 229 Sites)
| Number of Sites | Mean (Range) or Percent | |
|---|---|---|
| Facility Characteristics | ||
| Facility Type: VAMC | 133 | 58 % |
| CBOC | 96 | 42 % |
| Facility Size: Mean Number of Primary Care Patients (Range) | 229 | 27,495 (3,041–102,185) |
| Facility Size: < 10,000 patients | 43 | 19 % |
| 10,000 – 20,000 patients | 61 | 27 % |
| 20,001 – 30,000 patients | 39 | 17 % |
| 30,001 or more patients | 86 | 38 % |
| Area-level Characteristics | ||
| U.S. Census Region | ||
| Northeast | 37 | 16 % |
| Midwest | 57 | 25 % |
| South | 88 | 38 % |
| West | 47 | 21 % |
| Urban:* | 92 | 40 % |
| Other/Rural | 137 | 60 % |
VAMC VA Medical Center; CBOC Community-Based Outpatient Clinic
*Urban: Metropolitan w/population 1 million or more
Top Ranked VA PC Challenges
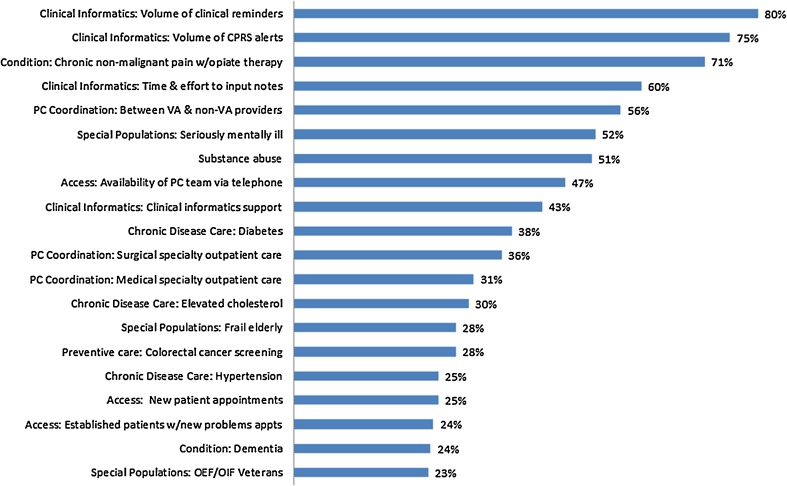
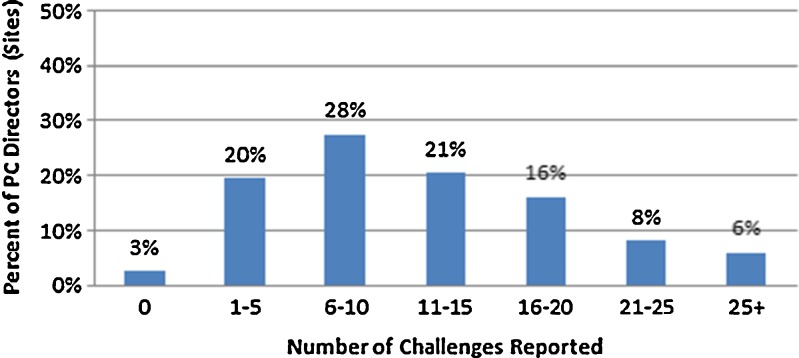
The top 20 challenges reported by VA PC directors reflected moderate-to-extremely challenging issues for 23 % to 80 % of VA PC practices and spanned all eight management domains (Fig. 1). The percentages of VA PC practices reporting each challenge nationally (all 48 issues) are shown in Table 1 by domain (Column 1). The distribution of the total count of VA PC challenges (rated moderate-to-extreme) is shown in Fig. 2. Only 3 % of VA PC directors (n = 6) reported that none of the management issues were moderately-to-extremely challenging, while 6 % reported 25 or more of the issues. On average, VA PC directors reported 16 moderate-to-extreme challenges.
Figure 1.
Top 20 challenges for primary care percent of directors reporting moderately-to-extremely challenging.
Figure 2.
Percent of directors reporting total count of challenges (range 0–48).
Four of the top 20 challenges reflected clinical informatics, including three of the four highest-ranked challenges, each of which affected over half of all VA PC practices. Specifically, clinical reminder volume, electronic medical record (EMR) alerts and time and effort to input notes were moderately-to-extremely challenging in 80 %, 75 % and 60 % of VA PC practices, respectively, while 43 % reported gaps in clinical informatics support (e.g., technical support for addressing EMR reminders or templates). In contrast, many other clinical informatics areas were not rated as particularly challenging (e.g., data availability on VA inpatient stays, other VA visits, lab test or diagnostic imaging results, EMR data processing time, etc.), with only 3–18 % of practices rating them as moderately-to-extremely challenging.
While we only asked about three challenging medical conditions (Table 1), management of chronic non-malignant pain requiring opiate therapy was the third most-reported challenge nationwide, with 71 % of directors reporting it as moderately-to-extremely challenging. Caring for patients with dementia was reported as moderately-to-extremely challenging by nearly one-quarter of PC directors. Of the four special patient populations we asked about, three were in the top 20, with PC management of patients with serious mental illness (SMI) rated as moderately-to-extremely challenging by 52 % of VA PC directors, and about one-quarter each reporting that caring for frail elderly and returning Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans were very challenging. Only one of the four MH/substance abuse items—substance abuse—was among the top 20 challenges, with 51 % of directors reporting their PC management as moderately-to-extremely challenging. Fewer than 20 % reported that posttraumatic stress disorder (PTSD), depression or anxiety were major challenges.
Three of four access items were represented in the top 20 challenges noted by VA PC directors, including telephone access to the PC team (47 %), and appointment availability for new patients (25 %) and for new problems for established patients (24 %). Three of the six PC coordination of care items were reflected in the top 20 challenges, with VA/non-VA care coordination being moderately-to-extremely challenging in 56 % of VA PC practices. About a third reported PC coordination with surgical (36 %) and medical (31 %) specialty outpatient care as moderately-to-extremely challenging.
For chronic disease care, caring for diabetes (38 %), elevated cholesterol (30 %) and hypertension (25 %) were among the top 20 challenges. Yet, PC management of coronary artery disease, chronic obstructive pulmonary disease (COPD) and degenerative joint disease were reported to be challenging by 10 % or less. For preventive care, only colorectal cancer screening (CRC) was among the top challenges (28 %).
Organizational and Area Variations in VA PC Challenges
We noted significant variations (p < 0.05) in reported challenges by organizational and area level characteristics (Table 1).
Type of VA Facility
VAMC-based PC directors reported more challenges managing elevated cholesterol compared to CBOCs. Care coordination at CBOCs represented greater challenges than VAMCs for inpatient and emergency care, and outpatient specialty MH care. In contrast, VAMCs reported greater challenges with availability of lab test results and historical pharmacy data compared to CBOCs.
Facility Size
Small sites (< 10,000 patients) reported fewer challenges for CRC screening than the large practices and fewer than all other sites for elevated cholesterol and chronic pain. Small sites were less likely than medium sites (10,000–20,000) to report challenges with peripheral vascular disease (PVD) and HIV, while they reported more challenges with PTSD. Medium sites reported more challenges than small sites in PC coordination with medical and surgical specialty care, while small sites’ coordination challenges were with inpatient and MH outpatient care.
Region
Western sites were more likely to report challenges compared to other regions. For example, Western sites were more likely to report challenges with PC management of SMI patients than all other regions; greater challenges in breast cancer screening, clinical reminder volume, and VA/non-VA care coordination than sites in the Midwest; and greater challenges in PC management of hypertension or substance abuse than sites in the Midwest or South.
Urban/Rural Location
Overall, rural practices faced more management challenges than large urban practices. For example, rural sites reported significantly more challenges than urban sites with PC management of COPD, PVD and HIV; PC coordination with any specialty outpatient care (medical, surgical, MH) and consult reports; as well as appointment availability for new problems for established patients.
Total Count of Challenges
The total count of challenges did not vary significantly by facility type or size. Rural sites were more likely to report challenges than urban (p = 0.025) and sites in the West compared to those in the Midwest (p = 0.002) (results not shown).
DISCUSSION
Prior to implementation of PACT in the VA, the nation’s largest integrated health system, PC directors reported serious challenges in key domains central to PCMH. Nationally, 30 % of the VA PC directors reported 16 or more PC management issues related to PCMH—some considered foundational to PCMH—were moderately-to-extremely challenging for their PC practices. Also, at least one challenge from every PCMH-related domain (access, preventive care, chronic diseases requiring care in PC, challenging medical conditions, MH/substance abuse, special populations, PC coordination of care, and clinical informatics) was included among the top 20 challenges nationwide. Understanding these challenges is critical context for the national roll-out of PACT.
The VA has had a fully implemented EMR for more than a decade, and has seen dramatic improvements in clinical quality attributed to its functionality.21 The Institute of Medicine has also independently rated VA’s EMR as among the best in the U.S. (IOM 2002). Yet, three of the top four challenges reported by VA PC directors nationally were focused on clinical informatics, with almost three out of four reporting clinical informatics as a moderate-extreme challenge across facility types, sizes, regions, and urban/rural locations. Outside the VA, great hope has been placed in the potential of health information technology (HIT), especially EMRs, to enable, if not drive, improvements in quality, efficiency, safety 22,23 and cost reductions,22,24 and as an essential tool in day-to-day PCMH functioning, if not one of its core principles.22,25,26 Green has further identified HIT as a key strategy for helping to alleviate the PC physician shortage.27 However, HIT has also been associated with interrupted work and increased provider burden.28 Given VA’s long HIT track record, VA PC experience with the overwhelming volume of EMR-based reminders and alerts in the context of inadequate clinical informatics support should raise caution for those assuming that “plugging in” an EMR will be a “fix all” for healthcare delivery challenges. More research is needed to improve PCMH-centric HIT functions supporting team-based care, care transitions, chronic disease management,29 and patient-centered care.25
Given that the VA provides care for a high volume of patients with multiple chronic conditions,30 the complexity of VA patients may invoke special challenges during PCMH implementation. Caring for complex patients in VA’s medical home context places special burdens on PC-based care management. For example, pain is the most commonly reported symptom in PC, and providers report difficulties in caring for patients with chronic pain,31 including pressure to prescribe and concerns with opioid treatment.32 We found that difficulties in caring for PC patients’ chronic pain are significant and national in scope, highlighting the need for PC-based innovations in chronic pain management,31 and raising questions about whether having some patients’ medical homes not based in PC could be more expedient.33 Also, given the much higher average age of VA users, challenges in management of PC needs among the many Veterans with dementia also presages challenges that non-VA PC providers are only just starting to experience.
These conditions, among others, accentuate the importance of strengthening links between PC and the medical home neighborhood. Regardless of PC’s ability to manage complex care needs, the need for specialty care services requires effective coordination. System integration, including that envisioned for accountable care organizations, may support the tenets of generalist-specialist coordination, but clearly requires explicit mechanisms to accomplish coordination goals. Despite the VA’s longstanding history as an integrated healthcare system, PC directors reported major challenges coordinating with medical, surgical, and MH outpatient specialty care, which were even worse among small VAMCs, rural practices and CBOCs, many of which are located anywhere from 30 to over 200 miles away from the nearest large VAMC. Challenges coordinating with non-VA providers is also of concern, as more than 30 % of Veterans use non-VA providers (e.g., Medicare providers, community providers delivering services not available in local VAs).34
Improving access is also a key component of PCMH, and has been central to a series of VA advanced clinic access initiatives for over a decade.35 Yet, one quarter of PC directors reported significant challenges with appointment availability for new patients and new problems for existing patients, and almost half reported major challenges with routine telephone access. Not surprisingly, pilot teams for PACT have given particular emphasis on improving access.36
Substantial gains in VA preventive care delivery pre-dated VA’s PACT initiative,21 reflecting prior investments in PC, at least in part.37 We were therefore not entirely surprised that VA PC directors reported the least amount of frustration with preventive care delivery, and even then, only with CRC screening, which requires iterative steps and specialty collaboration.17,38 To date, medical home improvements in the delivery of preventive services, including cancer screening, has received limited attention,39 suggesting VA’s successes in these areas warrant attention.
The VA is already addressing a number of the challenges identified here through different initiatives. For example, in clinical informatics, the VA has issued a toolkit on lab test results that includes guidance for managing alerts. There are also a number of efforts underway to help with pain management, including a PC Pain Champions Group and a PC Pain Community of Practice call. The VA is in the process of starting pilots for PACT Intensive Management for patients with complex and serious medical conditions. For coordination, electronic consultations and clinical tele-videoconferencing are being tested to help support delivery of care across specialties and sites.
This project has a few limitations. As a key informant survey, our findings reflect the views of PC directors, not all PC providers. Many of the VA PC directors provide clinical care in addition to their administrative duties, and we have no a priori reason to believe other frontline PC providers would report substantially fewer challenges. We also targeted VAMC-based and large CBOC-based PC directors, excluding a large number of very small CBOCs (typically 1–4 PC providers). Given that many of these smaller practices have fewer resources and are often even farther away from parent facilities, we do not expect them to reflect substantially different challenges—if anything, their challenges may be greater. Future research is needed to better understand the challenges faced by smaller PC practices. In addition, we are unable to explain why Western sites were more likely to report challenges than sites in other regions. In supplemental analyses (not shown), we found no statistically significant site-level differences in terms of facility type, facility size, or urban/rural location, suggesting that other unmeasured factors may account for regional differences.
Even with the VA’s many strengths, these PC management challenges heading into a national healthcare transformation initiative are critical to recognize. If PACT succeeds in the face of these challenges, then the VA’s experience will give insight into how to implement medical homes, especially in view of the clinical complexity of Veteran patients and site level differences that may require implementation adaptations. If, however, PACT’s early results are less than what was hoped for, these early challenges may provide important formative context for needed mid-course corrections. Regardless of the outcome, these challenges highlight the plight of PC providers, and the VA’s PACT initiative will shed critical insights into PCMH implementation outside the VA.
Acknowledgements
We would like to acknowledge funding from the VA Office of Patient Care Services for this operations project in support of VA primary care planning for patient-centered medical home implementation (Project # XVA 65–011). Additional analysis of these data was also supported by a VA HSR&D project examining implementation and impact of VA patient-centered medical homes (Project # IIR 09–082). Dr. Yano’s effort was funded by VA HSR&D Service through a Senior Research Career Scientist award (Project # RCS 05–195). We would also like to acknowledge Britney Chow, MPH for administrative support.
The views expressed in the manuscript are solely those of the authors, and do not necessarily represent the views of the U.S. Department of Veterans Affairs or the United States government.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Ornish D. The collapse of primary care. The Daily Beast: Newsweek; 2008. [Google Scholar]
- 2.Whitcomb ME, Cohen JJ. The future of primary care medicine. N Engl J Med. 2004;351(7):710–712. doi: 10.1056/NEJMsb045003. [DOI] [PubMed] [Google Scholar]
- 3.Rubinstein HG. Medical homes: the prescription to save primary care? AHIP Cover. 2008;49(1):44–47. [PubMed] [Google Scholar]
- 4.Yano E, Fleming B, Canelo I. VHA Clinical Practice Organizational Survey: national results for the PC director module. Sepulveda, CA: HSR&D Report No. MRC 05–093;2008.
- 5.O'Reilly KB. Doctors urge: Rescue primary care or work force shortage will mount. AMNews. Dec. 2008;8:2008. [Google Scholar]
- 6.Landon BE, Gill JM, Antonelli RC, Rich EC. Using evidence to inform policy: developing a policy-relevant research agenda for the patient-centered medical home. J Gen Intern Med. 2010;25(6):581–583. doi: 10.1007/s11606-010-1303-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacobson PD, Jazowski SA. Physicians, the Affordable Care Act, and primary care: disruptive change or business as usual? J Gen Intern Med. 2011;26(8):934–937. doi: 10.1007/s11606-011-1695-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel UB, Rathjen C, Rubin E. Horizon's patient-centered medical home program shows practices need much more than payment changes to transform. Health Aff (Millwood). 2012;31(9):2018–2027. doi: 10.1377/hlthaff.2012.0392. [DOI] [PubMed] [Google Scholar]
- 9.Nutting PA, Crabtree BF, Miller WL, Stewart EE, Stange KC, Jaen CR. Journey to the patient-centered medical home: a qualitative analysis of the experiences of practices in the National Demonstration Project. Ann Fam Med. 2010;8(Suppl 1):S45–56. doi: 10.1370/afm.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crabtree BF, Nutting PA, Miller WL, et al. Primary Care Practice Transformation Is Hard Work: Insights From a 15-Year Developmental Program of Research. Med Care. 2011. [DOI] [PMC free article] [PubMed]
- 11.Fields D, Leshen E, Patel K. Analysis & commentary. Driving quality gains and cost savings through adoption of medical homes. Health Aff (Millwood) 2010;29(5):819–826. doi: 10.1377/hlthaff.2010.0009. [DOI] [PubMed] [Google Scholar]
- 12.Steele GD, Haynes JA, Davis DE, et al. How Geisinger's advanced medical home model argues the case for rapid-cycle innovation. Health Aff (Millwood). 2010;29(11):2047–2053. doi: 10.1377/hlthaff.2010.0840. [DOI] [PubMed] [Google Scholar]
- 13.Wagner EH, Coleman K, Reid RJ, Phillips K, Abrams MK, Sugarman JR. The changes involved in patient-centered medical home transformation. Prim Care. 2012;39(2):241–259. doi: 10.1016/j.pop.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Nutting PA, Crabtree BF, Stewart EE, et al. Effect of facilitation on practice outcomes in the National Demonstration Project model of the patient-centered medical home. Ann Fam Med. 2010;8(Suppl 1):S33–44. doi: 10.1370/afm.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.James BC, Savitz LA. How Intermountain trimmed health care costs through robust quality improvement efforts. Health Aff (Millwood). 2011;30(6):1185–1191. doi: 10.1377/hlthaff.2011.0358. [DOI] [PubMed] [Google Scholar]
- 16.Reid RJ, Coleman K, Johnson EA, et al. The Group Health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood). 2010;29(5):835–843. doi: 10.1377/hlthaff.2010.0158. [DOI] [PubMed] [Google Scholar]
- 17.Yano EM, Soban LM, Parkerton PH, Etzioni DA. Primary care practice organization influences colorectal cancer screening performance. Health Serv Res. 2007;42(3 Pt 1):1130–1149. doi: 10.1111/j.1475-6773.2006.00643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soban LM, Yano EM. The impact of primary care resources on prevention practices. J Ambul Care Manag. 2005;28(3):241–253. doi: 10.1097/00004479-200507000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Yano E, Fleming B, Canelo I, et al. National Survey Results for the Primary Care Director Module of the VHA Clinical Practice Organizational Survey. Sepulveda, CA: VA HSR&D Center for the Study of Healthcare Provider Behavior;2008.
- 20.Yano EM, Schectman G, Stark R, Canelo I. 2008 VHA Primary Care Survey: National Survey Results. Sepulveda: VA Greater Los Angeles HSR&D Center of Excellence;2009.
- 21.Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348(22):2218–2227. doi: 10.1056/NEJMsa021899. [DOI] [PubMed] [Google Scholar]
- 22.Institute of Medicine. Leadership by example. Coordinating government roles in improving health care quality. Washington, DC: National Academy of Sciences;2002.
- 23.Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 24.Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood). 2005;24(5):1103–1117. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 25.Leventhal T, Taliaferro JP, Wong K, Hughes C, Mun S. The patient-centered medical home and health information technology. Telemed J E Health. 2012;18(2):145–149. doi: 10.1089/tmj.2011.0130. [DOI] [PubMed] [Google Scholar]
- 26.Finkelstein J, Barr MS, Kothari PP, Nace DK, Quinn M. Patient-centered medical home cyberinfrastructure current and future landscape. Am J Prev Med. 2011;40(5 Suppl 2):S225–233. doi: 10.1016/j.amepre.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 27.Green EP, Wendland J, Carver MC, Hughes Rinker C, Mun SK. Lessons learned from implementing the patient-centered medical home. Int J Telemed Appl. 2012;2012:103685. doi: 10.1155/2012/103685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fernandopulle R, Patel N. How the electronic health record did not measure up to the demands of our medical home practice. Health Aff (Millwood). 2010;29(4):622–628. doi: 10.1377/hlthaff.2010.0065. [DOI] [PubMed] [Google Scholar]
- 29.Bates DW, Bitton A. The future of health information technology in the patient-centered medical home. Health Aff (Millwood). 2010;29(4):614–621. doi: 10.1377/hlthaff.2010.0007. [DOI] [PubMed] [Google Scholar]
- 30.Yu W, Ravelo A, Wagner TH, et al. Prevalence and costs of chronic conditions in the VA health care system. Med Care Res Rev. 2003;60(3 Suppl):146S–167S. doi: 10.1177/1077558703257000. [DOI] [PubMed] [Google Scholar]
- 31.Evans L, Whitham JA, Trotter DR, Filtz KR. An evaluation of family medicine residents' attitudes before and after a PCMH innovation for patients with chronic pain. Fam Med. 2011;43(10):702–711. [PubMed] [Google Scholar]
- 32.Matthias MS, Parpart AL, Nyland KA, et al. The patient–provider relationship in chronic pain care: providers' perspectives. Pain Med. 2010;11(11):1688–1697. doi: 10.1111/j.1526-4637.2010.00980.x. [DOI] [PubMed] [Google Scholar]
- 33.Alakeson V, Frank RG, Katz RE. Specialty care medical homes for people with severe, persistent mental disorders. Health Aff (Millwood). 2010;29(5):867–873. doi: 10.1377/hlthaff.2010.0080. [DOI] [PubMed] [Google Scholar]
- 34.Liu CF, Bolkan C, Chan D, Yano EM, Rubenstein LV, Chaney EF. Dual use of VA and non-VA services among primary care patients with depression. J Gen Intern Med. 2009;24(3):305–311. doi: 10.1007/s11606-008-0867-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schall MW, Duffy T, Krishnamurthy A, et al. Improving patient access to the Veterans Health Administration's primary care and specialty clinics. Jt Comm J Qual Saf. 2004;30(8):415–423. doi: 10.1016/s1549-3741(04)30047-x. [DOI] [PubMed] [Google Scholar]
- 36.True G, Butler AE, Lamparska BG, et al. Open Access in the Patient-Centered Medical Home: Lessons from the Veterans Health Administration. J Gen Intern Med. 2012. [DOI] [PMC free article] [PubMed]
- 37.Yano EM, Simon BF, Lanto AB, Rubenstein LV. The evolution of changes in primary care delivery underlying the Veterans Health Administration's quality transformation. Am J Publ Health. 2007;97(12):2151–2159. doi: 10.2105/AJPH.2007.115709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dulai GS, Farmer MM, Ganz PA, et al. Primary care provider perceptions of barriers to and facilitators of colorectal cancer screening in a managed care setting. Cancer. 2004;100(9):1843–1852. doi: 10.1002/cncr.20209. [DOI] [PubMed] [Google Scholar]
- 39.Sarfaty M, Stello B, Johnson M, Sifri R, Borsky A, Myers RM. Colorectal Cancer Screening in the Framework of the Medical Home Model: Findings From Focus Groups and Interviews. Am J Med Qual. 2013. [DOI] [PubMed]