Abstract
Background
Injured elderly patients experience high rates of undertriage to trauma centers (TCs) while debate continues regarding the age defining a geriatric trauma patient. We sought to identify when mortality risk increases in injured patients due to age alone, to determine whether TC care was associated with improved outcomes for these patients, and to estimate the added admissions burden to TCs using an age threshold for triage.
Methods
We performed a retrospective cohort study of injured patients treated at TCs and non-TCs in Pennsylvania from April 1, 2001, to March 31, 2005. Patients were included if they were between ages 19 to 100 years and had sustained minimal injury (ISS<9). The primary outcome was in-hospital mortality. We analyzed age as a predictor of mortality using the fractional polynomial method.
Results
A total of 104,015 patients were included. Mortality risk significantly increased at 57 years (OR: 5.58; 95% CI: 1.07-29.0; p=0.04) relative to 19-year-old patients. TC care was associated with a decreased mortality risk compared to non-TC care (OR: 0.83; 95% CI: 0.69-0.99; p=0.04). Using an age of 70 as a threshold for mandatory triage, we estimated TCs could expect an annual increase of approximately one additional admission per day.
Conclusions
Age is a significant risk factor for mortality in trauma patients, and TC care improves outcomes even in older, minimally injured patients. An age threshold should be considered as a criterion for TC triage. Using the clinically relevant age of 70 as this threshold would not impose a substantial increase on annual TC admissions.
Keywords: Trauma, Geriatric, Age, Elderly, Triage
Introduction
Traumatic injury remains a leading cause of morbidity and mortality across all ages in the United States.1 Evidence shows that regionalized trauma systems and triage of critically injured patients to trauma centers (TC) reduce injury-related mortality by as much as 25% compared to non-trauma centers.2 Current triage criteria demonstrate insufficient sensitivity with respect to identifying older trauma patients requiring higher-level trauma care and thus, exhibit a tendency for undertriage.3-5 However, adults ages 65 years and older constitute the fastest-growing segment of the U.S. population. This age group is projected to constitute 19.3% of the population by the year 2030,6 and trauma systems are already seeing a disproportionate increase in geriatric trauma patients, as 23.7% of patients in the National Trauma Data Bank of 2011 were 65 years and older.7 Thus, it is imperative that we incorporate into our guidelines filters that facilitate identifying and triaging those elderly patients requiring definitive TC care.
Elderly trauma patients differ significantly from their younger counterparts, having a greater number of preexisting comorbidities,8-11 a higher risk of complications,9,12,13 and an increased probability of mortality.11,13-15 These findings suggest that older age is an excellent candidate for a triage criterion; yet, debate persists regarding the exact age beyond which a trauma patient is considered ‘elderly’.16 The objectives of this study were to identify when age becomes an independent risk factor for mortality in trauma patients and to determine if TC care is superior to non-TC care for elderly trauma patients with minimal injury severity. We hypothesized that age is an independent risk factor for mortality in trauma patients and that TC care, by comparison to non-TC care, is associated with reduced mortality for elderly patients, independent of injury severity. We secondarily determined the increased burden of admission for TCs using an increasing threshold age as a mandatory criterion for transport to a TC.
Methods
Data Source and Patient Selection
We performed a retrospective study of patient discharge data obtained from the Pennsylvania Trauma Outcomes Study (PTOS) and the Pennsylvania Health Care Cost Containment Council (PHC4) between April 1, 2001, and March 31, 2005. The PTOS includes patient discharge data obtained from accredited Pennsylvania trauma centers, while the PHC4 includes discharge data from all Pennsylvania trauma (TC) and non-trauma centers (non-TC).17,18 These data encompass every region of Pennsylvania and thus represent urban and rural populations. From both the PTOS and PHC4 data, we included patients between 19 and 100 years of age with an acute trauma diagnosis code (800-999), excluding late effect of injuries (905-909), foreign bodies (930-939), trauma complications (958), poisoning (960-989), external causes (990-995), and complications of medical and surgical care (966-999) in our analysis. Patients with solitary hip fractures (820.0-820.9) resulting from falls from the same level with no other injuries were also excluded. Because we wished to determine the use of age as a triage criterion independent of that established for injury severity, we restricted our analysis to subjects with minor injuries (i.e. ISS<9). Our primary analysis was performed with PHC4; we used PTOS to confirm that the population of patients treated at TCs was fully captured. This project was approved by the Institutional Review Board at the University of Pittsburgh.
Patient Variables
Our primary outcome was in-hospital mortality. We abstracted the following data: age, gender, ICD-9-CM codes for principal diagnosis and up to fourteen secondary diagnoses, injury severity (i.e. Injury Severity Score (ISS)), physiologic severity, hospital identification, year of admission, insurance, length of stay, and patient discharge disposition. Mechanism of injury was categorized as blunt, penetrating, or burns. Abbreviated injury scale (AIS) score and ISS were calculated using ICD-9 to AIS/ISS conversion software (ICDMAP90; The Johns Hopkins University and Tri-Analytics Inc, Baltimore, MD).19 Using the standard formula, ISS was calculated from AIS. Thirty comorbidities were identified per the methods of Elixhauser;20 each comorbidity was individually entered into the model. An alternate method of comorbidity adjustment using the Charlson-Deyo comorbidity score did not alter the results.21
Hospital Variables
Hospitals were classified as TCs using a list of accredited level I and level II centers published by the Pennsylvania Trauma Systems Foundation for the years studied.22 All other institutions were grouped as non-TCs.
Statistical Analysis
Univariate analyses of continuous and categorical variables were performed with Student’s t test and Pearson χ2 test as appropriate. Statistical significance was determined at p<0.05. We performed multivariate logistic regression to assess the association between age and the risk of mortality and to calculate crude and adjusted odds ratios (OR) with 95% confidence intervals (95% CI) after adjusting for differences in case mix. We explored for differences in outcome by age using the fractional polynomial method.23 After univariate analyses, all significant predictors and potential confounders were included in the full multivariate model. Effect modifications determined a priori were analyzed and retained in the model if p<0.05 for the interaction term. All statistical analyses were conducted with Stata 12 SE software (College Station, TX).
Results
Patients
A total of 104,015 subjects in the PHC4 sample were analyzed (Table 1). Of this cohort, 44,739 (43.0%) were treated at a TC. Compared to patients treated at a non-TC, those treated at a TC were more often male, younger, and more likely to have sustained an injury of greater magnitude (Table 1). The prevalence of comorbidities differed significantly for all but paralysis, liver disease, and coagulopathy (Table 2). Overall, the prevalence of comorbidities was higher at non-TCs than at TCs (Table 2). These distributional proportions were similar to the 39,140 subjects identified in the PTOS dataset (data not shown).
Table 1.
| TC | Non-TC | P value | |
|---|---|---|---|
| Number, n | 44,739 | 59,276 | |
| Age, mean yrs (SD) | 51.4 (21.4) | 64.1 (20.7) | <0.000 |
| Female, n (%) | 19,360 (43.3) | 36,077 (60.9) | <0.000 |
| ISS, mean (SD) | 3.30 (1.9) | 3.16 (1.7) | <0.000 |
| Mortality, n (%) | 283 (0.63) | 447 (0.75) | 0.02 |
TC, trauma center
Non-TC, non-trauma center
Table 2.
| TC | Non-TC | P value | |
|---|---|---|---|
| Congestive heart failure (%) | 2,212 (4.9) | 4,766 (8.0) | <0.000 |
| Arrhythmias (%) | 3,139 (7.0) | 5,918 (10.0) | <0.000 |
| Valvular disease (%) | 1,224 (2.7) | 2,457 (4.2) | <0.000 |
| Pulmonary circulation disorders (%) | 164 (0.4) | 366 (0.6) | <0.000 |
| Peripheral vascular disease (%) | 675 (1.5) | 1,851 (3.1) | <0.000 |
| Hypertension (%) | 10,854 (24.3) | 21,463 (36.2) | <0.000 |
| Paralysis (%) | 243 (0.5) | 275 (0.5) | 0.07 |
| Neurological disorders, other (%) | 751 (1.7) | 1,772 (3.0) | <0.000 |
| Chronic pulmonary disease (%) | 4,299 (9.6) | 8,020 (13.5) | <0.000 |
| Diabetes, uncomplicated (%) | 4,254 (9.5) | 8,302 (14.0) | <0.000 |
| Diabetes, complicated (%) | 601 (1.3) | 1,474 (2.5) | <0.000 |
| Hypothyroidism (%) | 2,377 (5.3) | 5,537 (9.3) | <0.000 |
| Renal failure (%) | 727 (1.6) | 1,432 (2.4) | <0.000 |
| Liver disease (%) | 283 (0.6) | 391 (0.7) | 0.59 |
| Peptic ulcer disease (%) | 151 (0.3) | 410 (0.7) | <0.000 |
| AIDS (%) | 72 (0.2) | 28 (0.1) | <0.000 |
| Lymphoma (%) | 106 (0.2) | 206 (0.4) | 0.001 |
| Metastatic cancer (%) | 166 (0.4) | 384 (0.7) | <0.000 |
| Solid tumor | 397 (0.9) | 800 (1.4) | <0.000 |
| Rheumatoid arthritis/collagen vascular disease (%) | 540 (1.2) | 1,234 (2.1) | <0.000 |
| Coagulopathy (%) | 566 (1.3) | 701 (1.2) | 0.23 |
| Obesity (%) | 575 (1.3) | 1,275 (2.2) | <0.000 |
| Weight loss (%) | 219 (0.5) | 429 (0.7) | <0.000 |
| Electrolyte disorder (%) | 2,383 (5.3) | 4,742 (8.0) | <0.000 |
| Blood loss anemia (%) | 155 (0.4) | 415 (0.7) | <0.000 |
| Deficiency anemia (%) | 1,386 (3.1) | 3,481 (5.9) | <0.000 |
| Alcohol abuse (%) | 4,946 (11.1) | 1,779 (3.0) | <0.000 |
| Drug abuse (%) | 2,438 (5.5) | 704 (1.2) | <0.000 |
| Psychoses (%) | 1.574 (3.5) | 1,640 (2.8) | <0.000 |
| Depression (%) | 2,668 (6.0) | 4,321 (7.3) | <0.000 |
TC, trauma center
Non-TC, non-trauma center
Outcomes
For the entire cohort of minimally injured (ISS<9) subjects, in-hospital mortality occurred in 730 patients (0.70%). Of subjects treated at non-TCs, 447 died (0.75%), whereas in-hospital mortality occurred in 283 patients (0.63%) treated at TCs (p=0.02) (Table 1). Age was independently associated with an increased risk of death (adjusted OR per year 1.05; 95% CI 1.04-1.06; p<0.001). Figure 1 shows the effect of increasing age when examined as a continuous variable in a multivariate, fractional polynomial model. Increased mortality is seen nearly throughout the entire distribution, as age increases from the lowest to the highest value (Figure 1). By comparison to the youngest subjects (19 years), we identified a threshold for increased risk of death at 57 years of age (OR: 5.58, 95% CI: 1.07-29.0; p=0.04). Treatment at a TC was associated with a lower mortality risk compared to treatment at a non-TC (adjusted OR 0.83; 95% CI 0.69-0.99; p=0.04) (Figure 2). The association between age and mortality did not vary with treatment at a TC (interaction between TC and age, p=0.25).
Figure 1. Adjusted odds ratio for mortality as a function of age.

The adjusted odds ratios for mortality are presented relative to the youngest aged population (18-years). Dashed lines represent the 95 percent confidence intervals for the estimated odds ratios.
Figure 2. Adjusted odds ratio for mortality in patients treated at TCs compared to NTCs.
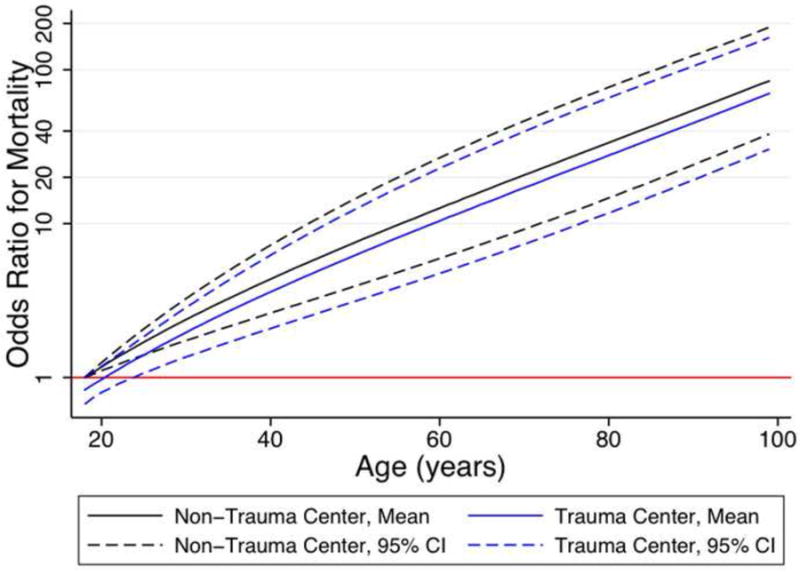
The adjusted odds ratios for mortality are presented relative to the youngest aged population (18-years). Dashed lines represent the 95 percent confidence intervals for the estimated odds ratios. TC=trauma center; NTC=non-trauma center.
Standardizing the covariates to the population means, we calculated the predicted probabilities of mortality with increasing age, comparing care delivered at a TC to a non-TC. As shown in Figure 3, TC care was associated with a reduced predicted probability of death by comparison to a non-TC. This absolute benefit increased with increasing age. At the age of 70, care at a TC was associated with a predicted 0.4% (range: 0.2-0.7%) absolute reduction in the risk of death. We then calculated the number of patients needed to transfer from non-TCs to TCs (i.e. number needed to treat) to save one life as the threshold age for transfer increased (Figure 4). Using age 70 as an example, 244 (range: 139-438) patients would need to be transferred to save 1 life. These calculations were subsequently used to calculate the proportional and absolute effect on TC admission volumes (figure 5). As shown in Figure 5, with increasing age the annual proportional increase and mean daily increase in TC admissions decreases. Again, using age 70 as an example, TCs would experience an estimated 38% increase in annual admissions and slightly less than 1 additional admission per day.
Figure 3. Predicted probability of mortality in patients treated at TCs compared to those treated at NTCs.
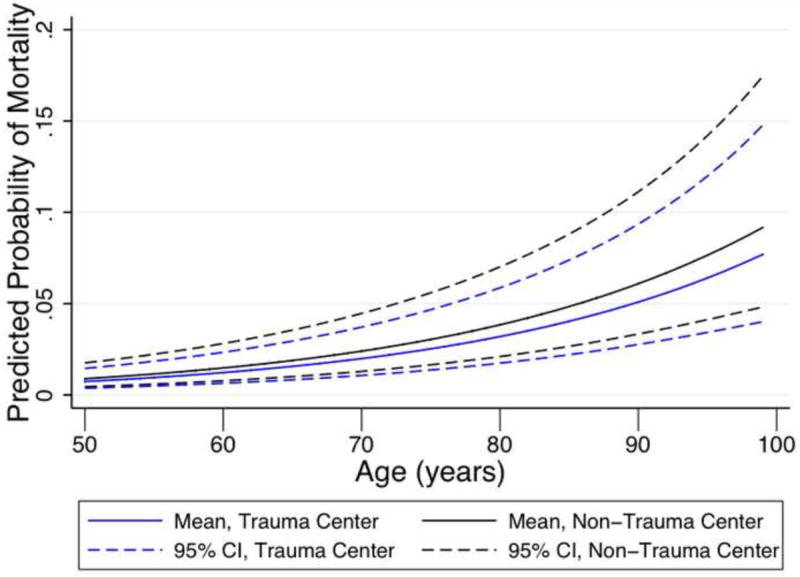
The predicted probabilities of mortality are presented relative to the 50 year aged population. Dashed lines represent the 95 percent confidence intervals for the estimated predicted probabilities. TC=trauma center; NTC=non-trauma center.
Figure 4. Number needed to transfer to save one life using each age as a criterion for triage to a transfer center.
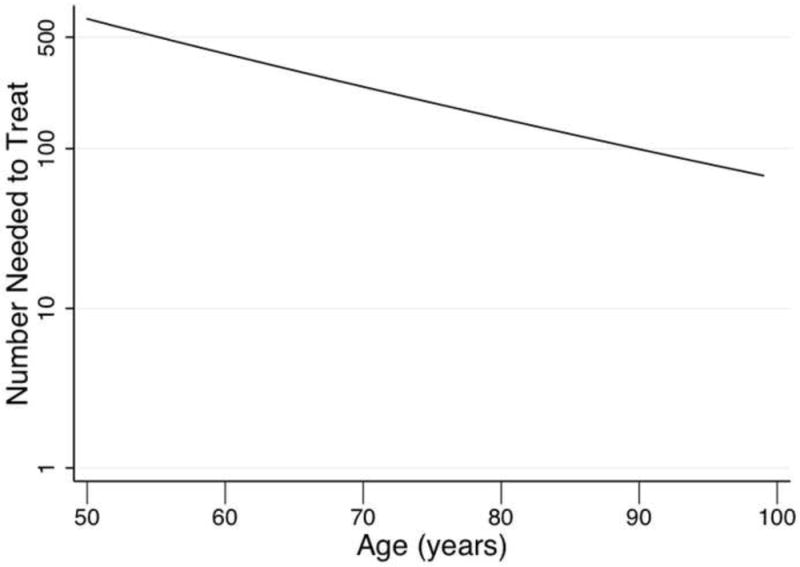
The numbers of patients needed to be transferred to save one life are presented relative to the 50 year aged population.
Figure 5. Estimated increases in annual and daily admissions to trauma centers using age as a criterion for triage.
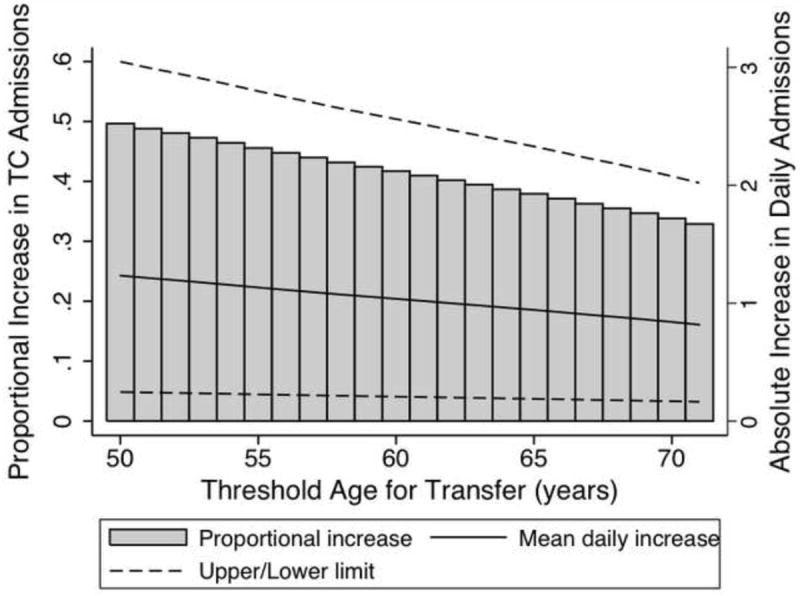
The estimated proportion increase in trauma center admission for each threshold age is represented by each bar (left ordinate). The mean absolute increase in daily trauma center admission is represented by the solid line (right ordinate). Dashed lines represent the ranges of increases in daily admission.
Discussion
The development of regionalized trauma systems and the triage of critically injured patients to TCs effectively reduce injury-related mortality by as much as 25% when compared to non-TCs.2 Evidence-based criteria to identify the most severely injured patients requiring a higher level of care, beginning in 1976 with the promulgation of the American College of Surgeons Committee on Trauma’s triage criteria, have been inherent to this success. Subsequent research, however, has identified the suboptimal performance of these criteria with respect to target rates of over- and undertriage, particularly in certain subgroups such as elderly trauma patients.3-5 Current criteria assume that the mechanism of trauma imparts equal severity of injury across all populations, neglecting that as physiologic reserve diminishes with age, so too does the ability to tolerate even minor trauma.24,25 Oreskovich et al. found an overall mortality of 15% in patients above age 70, much higher than the 3% mortality expected in younger patients with the same mean ISS.14 Our data suggests that increasing age is associated with an increasing risk of death even among minimally injured patients. TC care is associated with improved outcomes in this population, with a clinically relevant difference in outcome noted in elderly (>70) patients. Thus, an age threshold should be incorporated into triage guidelines to ensure that elderly patients receive optimal, higher-level care.
The American College of Surgeons’ triage criteria suggests 55 years as an age beyond which transport to a TC should be considered.26 This guideline is based upon research performed over two decades ago.13 Similarly, the Eastern Association for the Surgery of Trauma recommends that “advanced patient age should lower the threshold for field triage directly to a trauma center.”27 What remains to be determined is the age at which such higher care should be delivered. Numerous studies have identified an increased risk of mortality associated with an age as low as 50 years to as high as 80 years, yet there exists no agreed-upon definition of the geriatric trauma patient.16,27 Such a wide discrepancy may be related to the varying methods of quantifying age. Age must be modeled appropriately to truly define the geriatric trauma patient. Age dichotomies and categories are arbitrary, and other work suggests that the mortality associated with age is not truly linear.13 We thus used a fractional polynomial regression to identify the appropriate nonlinear model of risk, with our analysis identifying a significant increase in mortality risk beginning at age 57 years.
We show an increased risk of mortality in older patients treated at non-TCs compared to those treated at TCs at all ages regardless of injury severity. This benefit remains stable with increasing age, and the estimated increase in patient volume associated with using age as a triage criterion actually diminishes with increasing age. Using an age threshold of 70 years, we estimated that 244 patients would need to be transferred to a TC to save one additional life; this amounts to approximately one added patient per trauma center per day in Pennsylvania. It may seem as though this asks TCs, already managing a high volume of patients, to assume an additional burden they cannot bear. Bhattacharyya et al. have shown, however, that TCs accommodate a similarly increased volume depending on the day of the week, the month, and even the temperature.28 This suggests that TCs are capable of handling this estimated increase in volume. MacKenzie et al. were unable to show a statistically significant difference in mortality among minimally injured patients treated at TCs compared to those treated at non-TCs, although they did note a non-significant improvement in mortality for older patients treated at TCs.2 Importantly, they defined minimal injury as a maximum AIS 3 and older patients as age>55. Our analysis demonstrates that TC care significantly reduces relative and absolute mortality for older patients with mild injuries. By including only minimally injured patients and by modeling age as a continuous variable, our analysis was able to detect significant differences in mortality that may have been masked in other studies.
Our study has several limitations. We controlled for many confounding variables, but it is possible that residual bias due to insufficient controlling for covariates persists. In particular, our data did not include mechanism of injury classification. By restricting our analysis to patients with an ISS<9, a cohort in which mechanism of injury should have a reduced impact on mortality outcomes, we attempted to attenuate the absence of this variable. With respect to preexisting comorbidities, we were only able to assess up to fourteen secondary diagnoses per patient. Our data show a higher prevalence of comorbidities in patients treated at non-TCs, and it is possible that comorbidities were under-coded at TCs. However, this would likely bias our results toward the null. Lastly, we focused on in-hospital mortality rather than longer-term outcomes. Though TC care may reduce in-hospital mortality, this may simply reflect a displacement of mortality outcomes to long-term care facilities rather than hospitals.29 Alternatively, patients treated at non-TCs may be in the company of their families more frequently and have care withdrawn more often than occurs for patients treated at TCs.
In conclusion, we have shown that older trauma patients have a significantly increased risk of mortality beginning with a significance threshold of 57 years. Trauma center care appears to be associated with reduced mortality in this population sustaining minor injury and that may otherwise not meet contemporary criteria for triage to a TC. This improved outcome is clinical relevant at an age threshold of 70 years, which would necessitate a small increase in daily TC admission to improve mortality outcome. Further studies of the effects of trauma center care on outcomes in the minimally injured elderly are warranted.
References
- 1.Minino AM, Xu J, Kochanek KD, Tejada-Vera B. Death in the United States, 2007. NCHS data brief. 2009 Dec;(26):1–8. [PubMed] [Google Scholar]
- 2.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. The New England journal of medicine. 2006 Jan 26;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 3.Ma MH, MacKenzie EJ, Alcorta R, Kelen GD. Compliance with prehospital triage protocols for major trauma patients. The Journal of trauma. 1999 Jan;46(1):168–175. doi: 10.1097/00005373-199901000-00029. [DOI] [PubMed] [Google Scholar]
- 4.Chang DC, Bass RR, Cornwell EE, Mackenzie EJ. Undertriage of elderly trauma patients to state-designated trauma centers. Arch Surg. 2008 Aug;143(8):776–781. doi: 10.1001/archsurg.143.8.776. discussion 782. [DOI] [PubMed] [Google Scholar]
- 5.Phillips S, Rond PC, 3rd, Kelly SM, Swartz PD. The failure of triage criteria to identify geriatric patients with trauma: results from the Florida Trauma Triage Study. The Journal of trauma. 1996 Feb;40(2):278–283. doi: 10.1097/00005373-199602000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Vincent GK, Velkoff VA U.S. Census Bureau. Population estimates and projections P25-1138. Washington, DC: U.S. Dept. of Commerce, Economics and Statistics Administration, U.S. Census Bureau; 2010. The next four decades the older population in the United States : 2010 to 2050. http://purl.access.gpo.gov/GPO/LPS126596. [Google Scholar]
- 7.Nance ML. [February 7, 2012];National Trauma Data Bank 2011 Annual Report. 2011 http://www.facs.org/trauma/ntdb/pdf/ntdbannualreport2011.pdf.
- 8.Morris JA, Jr, MacKenzie EJ, Edelstein SL. The effect of preexisting conditions on mortality in trauma patients. JAMA : the journal of the American Medical Association. 1990 Apr 11;263(14):1942–1946. [PubMed] [Google Scholar]
- 9.Perdue PW, Watts DD, Kaufmann CR, Trask AL. Differences in mortality between elderly and younger adult trauma patients: geriatric status increases risk of delayed death. The Journal of trauma. 1998 Oct;45(4):805–810. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- 10.Grossman MD, Miller D, Scaff DW, Arcona S. When is an elder old? Effect of preexisting conditions on mortality in geriatric trauma. The Journal of trauma. 2002 Feb;52(2):242–246. doi: 10.1097/00005373-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 11.McGwin G, Jr, MacLennan PA, Fife JB, Davis GG, Rue LW., 3rd Preexisting conditions and mortality in older trauma patients. The Journal of trauma. 2004 Jun;56(6):1291–1296. doi: 10.1097/01.ta.0000089354.02065.d0. [DOI] [PubMed] [Google Scholar]
- 12.DeMaria EJ, Kenney PR, Merriam MA, Casanova LA, Gann DS. Survival after trauma in geriatric patients. Annals of surgery. 1987 Dec;206(6):738–743. doi: 10.1097/00000658-198712000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Finelli FC, Jonsson J, Champion HR, Morelli S, Fouty WJ. A case control study for major trauma in geriatric patients. The Journal of trauma. 1989 May;29(5):541–548. doi: 10.1097/00005373-198905000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Oreskovich MR, Howard JD, Copass MK, Carrico CJ. Geriatric trauma: injury patterns and outcome. The Journal of trauma. 1984 Jul;24(7):565–572. [PubMed] [Google Scholar]
- 15.Gubler KD, Davis R, Koepsell T, Soderberg R, Maier RV, Rivara FP. Long-term survival of elderly trauma patients. Arch Surg. 1997 Sep;132(9):1010–1014. doi: 10.1001/archsurg.1997.01430330076013. [DOI] [PubMed] [Google Scholar]
- 16.Caterino JM, Valasek T, Werman HA. Identification of an age cutoff for increased mortality in patients with elderly trauma. The American journal of emergency medicine. 2010 Feb;28(2):151–158. doi: 10.1016/j.ajem.2008.10.027. [DOI] [PubMed] [Google Scholar]
- 17. [July 22, 2010];Pennsylvania Trauma Systems Foundation Annual Report, 2007. 2007 http://www.ptsf.org/about_us/annual_reports.
- 18. [July 22, 2010];About the Council. 2011 http://www.phc4.org/
- 19.MacKenzie EJ, Steinwachs DM, Shankar B. Classifying trauma severity based on hospital discharge diagnoses. Validation of an ICD-9CM to AIS-85 conversion table. Medical care. 1989 Apr;27(4):412–422. doi: 10.1097/00005650-198904000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical care. 1998 Jan;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of clinical epidemiology. 1992 Jun;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 22. [July 22, 2010];Trauma center accreditation status. 2000-2004 Oct; http://www.ptsf.org.
- 23.Royston P, Ambler G, Sauerbrei W. The use of fractional polynomials to model continuous risk variables in epidemiology. International journal of epidemiology. 1999 Oct;28(5):964–974. doi: 10.1093/ije/28.5.964. [DOI] [PubMed] [Google Scholar]
- 24.Bergeron E, Clement J, Lavoie A, et al. A simple fall in the elderly: not so simple. The Journal of trauma. 2006 Feb;60(2):268–273. doi: 10.1097/01.ta.0000197651.00482.c5. [DOI] [PubMed] [Google Scholar]
- 25.Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001 Jan;50(1):116–119. doi: 10.1097/00005373-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 26.American College of Surgeons. Committee on Trauma. ATLS, advanced trauma life support program for doctors. 7. Chicago: American College of Surgeons; 2004. [Google Scholar]
- 27.Jacobs DG, Plaisier BR, Barie PS, et al. Practice management guidelines for geriatric trauma: the EAST Practice Management Guidelines Work Group. The Journal of trauma. 2003 Feb;54(2):391–416. doi: 10.1097/01.TA.0000042015.54022.BE. [DOI] [PubMed] [Google Scholar]
- 28.Bhattacharyya T, Millham FH. Relationship between weather and seasonal factors and trauma admission volume at a Level I trauma center. The Journal of trauma. 2001 Jul;51(1):118–122. doi: 10.1097/00005373-200107000-00019. [DOI] [PubMed] [Google Scholar]
- 29.Davidson GH, Hamlat CA, Rivara FP, Koepsell TD, Jurkovich GJ, Arbabi S. Long-term survival of adult trauma patients. JAMA : the journal of the American Medical Association. 2011 Mar 9;305(10):1001–1007. doi: 10.1001/jama.2011.259. [DOI] [PubMed] [Google Scholar]


