SUMMARY
Objective
To systematically review Indian literature on delays in TB diagnosis and treatment.
Methods
We searched multiple sources for studies on delays in pulmonary TB and chest symptomatic patients. Studies were included if numeric data on any delay were reported. Patient delay was defined as the time interval between onset of symptoms and the patient’s first contact with a healthcare provider. Diagnostic delay was defined as the time interval between the first consultation with a healthcare provider and diagnosis. Treatment delay was defined as the time interval between diagnosis and initiation of anti-TB treatment. Total delay was defined as time interval from the onset of symptoms until treatment initiation.
Results
Among 541 potential citations identified, 23 studies met our inclusion criteria. Included studies used a variety of definitions for onset of symptoms and delays. Median (IQR) estimates of patient, diagnostic and treatment delay were 18.4 (14.3-27.0), 31.0 (24.5-35.4) and 2.5 days (1.9-3.6), respectively, for TB and chest symptomatic patients combined. The median total delay was 55.3 days (46.5-61.5). About 48% of all patients first consulted private providers and 2.7 healthcare providers, on average, were consulted before diagnosis. Number and type of provider first consulted were the most important risk factors for delay.
Conclusions
These findings underscore the need to develop novel strategies for reducing patient and diagnostic delays and engaging first-contact healthcare providers.
Keywords: Tuberculosis, Delayed Diagnosis, Delivery of Health Care, Care Seeking Behaviour, India
INTRODUCTION
Early case detection and treatment is critical for controlling tuberculosis (TB)1, but national TB programs are heavily dependent on passive case finding. Studies suggest that diagnosis of TB is often delayed2 and one major reason is repeated visits at the same healthcare level and non-specific antibiotic therapies.3 Overall diagnostic delay has been attributed to both patients and the health system.4
Delayed diagnosis of TB can enhance the transmission of infection, worsen the disease, increase the risk of death, and may be a reason why TB incidence has not declined substantially, despite the global scale-up of DOTS.5 Hence, studies about health care seeking behaviour and diagnostic delays provide important information for program managers.
India has the highest TB burden among the 22 high TB burden countries with an estimated incidence of 2.2 million cases in 2011.1 In 1997, India started implementing the Directly Observed Treatment Short-course (DOTS) strategy under the Revised National TB Control Programme (RNTCP) and covered the entire country by 2006. Despite this scale-up of DOTS, TB incidence continues to remain high indicating that there could be substantial ongoing transmission.
India has a complex and highly heterogeneous health care delivery system, with both public sector and private sector (both formal and informal) health care providers (HCPs). Private and informal HCPs are often the first source of care for any illness6-8 and also TB.9 There is evidence, albeit limited, that patients with TB symptoms often begin seeking advice in the informal private sector (chemists and unqualified practitioners), then seek care from qualified practitioners, and eventually end up in the public sector for free treatment.10 Patients move from one provider to another, before they are finally diagnosed and started on anti-TB treatment.10-12 Although two systematic reviews have been published on diagnostic delays,2, 3 they did not report healthcare seeking behavior of patients with presumed TB and included few studies from India.
METHODS
Objective
We aimed to systematically review the literature from India about care seeking behaviour, patient, diagnostic and treatment delays for pulmonary TB patients and chest symptomatics as well as the risk factors for delays.
Search strategy
With the assistance of a medical librarian, we searched PubMed, Embase, and Web of Science -from January 2000 to May 2013, without any language restrictions using the following search terms, adapted from previous reviews2, 3: #1. “tuberculosis”[Mesh] OR “Mycobacterium tuberculosis” [Mesh] OR “tuberculosis”[tiab]; #2. “delayed diagnosis”[Mesh] OR (diagnosis*[tiab] AND delay* [tiab]) OR (treatment* [tiab] AND delay* [tiab]) OR (case [tiab] AND finding [tiab]); #3.”patient acceptance of health care”[Mesh] OR ((health [tiab] OR healthcare [tiab]) AND seeking [tiab] AND (behaviour* [tiab] OR behaviour*)) OR (care [tiab] AND seeking [tiab]); #4. “India”[Mesh] OR “India*” [tiab]; #6. #1 AND #4 AND #5.
In addition, we carried out an electronic search of several Indian journals to increase the yield of relevant studies, especially from non-indexed journals: Indian Journal of Tuberculosis, Indian Journal of Public Health, Indian Journal of Community Medicine, National Medical Journal of India, and Indian Journal of Medical Research. Additional studies were identified by contacting the authors of primary studies and experts in the field of TB, and by searching the reference lists of primary studies, and previous systematic reviews. We requested unpublished data from organizations such as Central TB Division (Ministry of Health and Family Welfare, Government of India), RNTCP, and IUATLD, South East Asia.
Inclusion/exclusion criteria
With respect to study designs, we included cross-sectional surveys, prospective patient recruitment and retrospective analysis of medical records. Participants included chest symptomatics (individuals with cough ≥2 weeks and suspected for TB) patients, pulmonary TB (PTB) patients (smear-negative, new smear positive or re-treatment patients), pulmonary and extra-pulmonary TB (EPTB) (if data were presented for PTB separately).Outcome measures included health seeking behaviour, ‘delays’ such as patient delay, health system, diagnostic delay, treatment delay and total delay, risk factors for patient delay, and health system delay (defined later).
If there were duplicate publications of same study, the most recent publication which reported full data was included. Studies reporting health seeking behaviour and ’delays’ for only EPTB, and studies not reporting data separately for PTB and EPTB (if our attempt to obtain disaggregated data from the authors for PTB failed) and purely qualitative studies were excluded. Additionally, the studies which reported only health seeking behaviour, but not duration of delays were excluded.
Study selection
Citations identified by the search were independently assessed by two review authors (CTS and ZZQ). In the next stage, full text articles were retrieved to identify all eligible studies, using the inclusion and exclusion criteria listed above. Disagreements between the reviewers were resolved by a third reviewer (MP).
Quality assessment
Since tools such as QUADAS13 are meant for diagnostic accuracy studies, and as there are no quality assessment tools for studies on diagnostic delays, we used a few indicators to summarize quality of included studies:
Retrospective analysis of already collected data: Yes/No
Representative sample of TB patients were included: Yes/No
TB patients confirmed by either smears or culture: Yes/No
Diagnostic delays separately reported as patient and health system delays: Yes/No
Risk factors for diagnostic delays were reported: Yes/No
All included studies were assessed independently by two reviewers (CTS and ZZQ).
Data extraction and analysis
Two reviewers (CTS and ZZQ) extracted the data from included studies using a data extraction form, adapted from the previous reviews. Disagreements were resolved either through discussion or by consulting a third reviewer (MP). The data extracted included name of the first author, year of publication, year of study, study characteristics (design, location, urban/rural, setting, sample size) and patient characteristics (age, gender, education), type of participants (chest symptomatics, newly diagnosed smear positive/negative, retreatment pulmonary TB patients), ‘delays’, health care seeking behaviour, and risk factors for delays.
We adopted the conceptual framework used in our previous systematic review (Figure 1) for extracting data on ‘delays’. This was adapted from the terminology for delays used in a study by Yimer et al.4 Patient delay (PD) was defined as the time interval between onset of symptoms suggestive of PTB and the patient’s first contact with a HCP. Diagnostic delay (DxD) was defined as the time interval between the first consultation with a HCP and diagnosis. Treatment delay (RxD) was defined as the time interval between diagnosis and initiation of anti-TB treatment. Total delay was defined as time interval from the onset of symptoms until treatment initiation. In this review, health system delay (HSD) includes DxD and RxD. This modification was made considering that both DxD and RxD are caused by health system or HCPs consulted by the patients (Figure 1).
Figure 1.
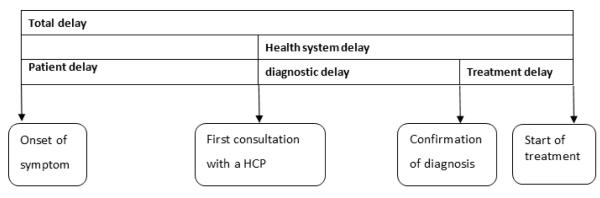
Conceptual framework on definitions of “delays” (this is a schematic; the size/length of components do not represent actual durations). [adapted from Yimer et al.4]
Of the six studies done among CS patients, two studies reported DxD. One study defined DxD as the interval between first visit to HCP and collection of a sputum, while the other did not define DxD. PD was reported in all six studies and defined PD same as that for PTB patients, and none of them reported RxD as it was not applicable. Hence, we do not provide separate definitions for various ‘delays’ for studies done among CS studies.
Where necessary, authors of the studies were contacted for additional information. For average duration for each ‘delay’, we extracted the average (median) reported in the included studies. We extracted mean estimates from studies that did not provide data on median ‘delays’. We only extracted the average “total delays” reported in the primary studies, and did not sum up various “delays” to get the total. If the duration of ‘delays’ was reported in weeks or months we transformed them into number of days. For health seeking behaviour, we extracted the percentage of patients who first consulted a private practitioner; average (median or mean) number of HCPs consulted before a diagnosis was made. Significant risk factors for longer PD and DxD were extracted, if multivariate analyses were carried out and reported.
Data analysis
We generated a summary of results table to describe the characteristics and results of each of the included studies, including health seeking behaviour and the outcomes on delays. A separate summary of results table was prepared for significant risk factors by multivariate analysis for prolonged delays. Since time duration is generally not normally distributed, we preferred median for our analysis. We summarized time duration (in days) for each type of delays by constructing box plots to depict median, inter quartile range (IQR), minimum and maximum. We compared each of the delays between two groups of study participants namely chest symptomatic and PTB patients (any type), and conducted subgroup analyses (e.g. urban versus rural), where appropriate.
RESULTS
Study selection
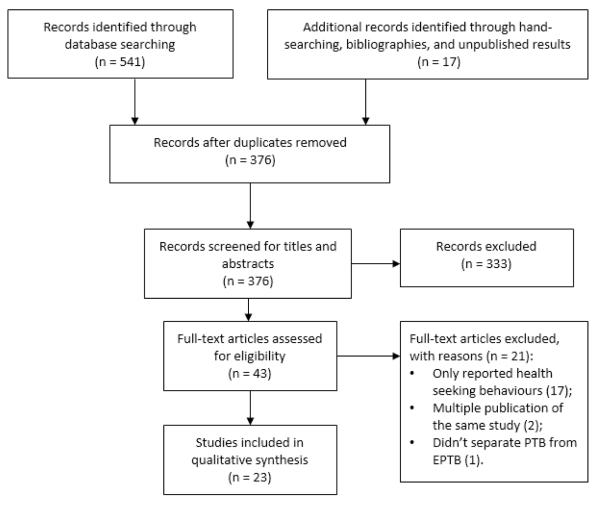
We identified 541 potentially eligible citations from the database searches, and 15 studies from hand-searching and screening of bibliographies including studies published before the year 2000. Two additional unpublished reports were obtained from Central TB Division, RNTCP. We removed duplicates and screened the titles and abstracts of the remaining 376 records. 43 publications were selected for full-text screening, after which, 23 articles were included in the final analysis (Figure 2). A list of excluded studies with reasons for exclusion is available from the review authors upon request.
Figure 2.
Study selection flow chart
Characteristics of the included studies
Table 2 provides a summary of all included studies. These studies were published between the year of 1998 and 2013, while research was actually conducted between 1996 and 2012. All except two studies were cross-sectional designs. The majority of the studies were conducted in three states namely Tamil Nadu (n=7)14-20, Maharashtra (n=5)21-25 and Karnataka (n=4).12, 26-28 The remaining studies were carried out in the states of Delhi29, West Bengal 30, 31, Andhra Pradesh30, Himachal Pradesh32, Haryana33, and Sikkim34, or covered several regions.35 Six studies were conducted in urban areas, five in rural areas, and ten of them in both areas. Additionally, five studies collected the data by community surveys, while the remaining studies collected data by recruiting patients from RNTCP (n=15) and the National Tuberculosis Program (NTP) (n=3) which preceded RNTCP.
Table 2.
Characteristics of included studies and key outcomes (n=23)
| Citation [reference] | Year of study |
Location | urban / rural |
Study setting |
Sampl e size |
Sample characteristics |
Patient delay (PD) (d) |
Diagn ostic delay (DxD) (d) |
Treat ment delay (RxD) (d) |
Total delay (TD) (d) |
% of patients who first consulted Private HCP |
Average number HCP visited before reaching a diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Studies on delays in Pulmonary TB (PTB) patients
| ||||||||||||
| Ananthakrishnan et. al (2012) * 14 | 2007 | Chennai, Tamil Nadu |
Urban | 10 Tuberculo sis Units |
219 PTB |
aged< 55 years- 86.7%, males- 62%, No or primary education- 44% |
11.4 | _ | _ | _ | 64.4% | 2.8 |
|
| ||||||||||||
| Bawankule et. al. (2010) * 25 | 2007 | Wardha, Maharastra |
Rural | Tertiary care hospital |
53 PTB | Mean age-28.2 years, Male- 69.8%, up to primary education- 39.6% |
95.0 | 47.01 | _ | 118.0 | 26.4% | 4.3 |
|
| ||||||||||||
| Dhanvij et. al (2009) * 21 | 2007 | Wardha, Maharashtr a |
Rural | Tertiary care hospital |
39 PTB | Mean age-39.3 years, Males- 71% |
47.2 | 25.0 | 1.8 | 73.9 | 48.7% | 1.9 |
|
| ||||||||||||
| Dhingra et. al. (2002) * 29 | 2001 | New Delhi, Delhi |
Urban | 4 TB sub centres |
301 PTB |
mean age-33 years, Male- 53.1%, Illiterate- 49.2% |
18.8 | _ | _ | _ | 56.8% | _ |
|
| ||||||||||||
| Uplekar et al. (1998) + 24 | _ | Pune & Mumbai, Maharastra |
Both | Private and public health institution s |
173 PTB |
aged>45 years- 20%, Male-65%, Illiterate-31% |
21.2 | 36.7 | 3.4 | _ | 86% | _ |
|
| ||||||||||||
| Balasubramanian et. al (2004) * 16 | 1999 | Tiruvallur, Tamil Nau |
Rural | TB patients registered under DOTS |
566 new SPP2 |
Male-76.5% | 14.0 | 31.0 | _ | 45.0 | 53.0% | _ |
|
| ||||||||||||
| Chakraborty et. al. (2001) * 26 | _ | 2 districts, Karnataka |
District TB centre Tuberculo sis Units |
147 new SPP |
Male-74.8%, Illiterate-34.7% |
267.7 | 39.4 | _ | _ | 10.9% | 12.3 | |
|
| ||||||||||||
| Goel et. al. (2011) * 27 | 2006- 07 |
Udupi district Karnataka |
Both | Communit y survey |
98 new SPP |
aged>45 years- 38.8%, Male- 58%, Illiterate- 63.2% |
30.0 | 54.5 | 2.0 | 57.5 | 76.5% | 2.5 |
|
| ||||||||||||
| Jagadish et. al. (2012) * 28 | 2009 | Bangalore, Karnataka |
Urban | Tuberculo sis Units/dist rict medical centres |
468 new SPP |
Mean age-38.5 years, Male- 69.7%, up to primary-40.6% |
24.0 | 18.03 | _ | 41.0 | 49.8% | _ |
|
| ||||||||||||
| Pantoja et al. (2010) 12 | 2005 | Bangalore, Karnataka |
Urban | Under registry of RNTCP |
658 PTB |
Mean age - 36 years, above 45 years - 30% of PTB patients; Males - 65%; Illiterate - 35% |
7.0 | 35.03 | _ | 51.0 | 75.0% | 3.3 |
|
| ||||||||||||
| Paul PLOS one (2012)* i30 | 2010 | Bardhaman, West Bengal &Nalagond a, Andhra Pradesh |
Rural | 2027 new SPP |
mean age- 39years male- 79%, |
_ | _ | 8.0 | _ | _ | _ | |
|
| ||||||||||||
| Pradhan et al (2010) * 22 | 2005- 06 |
Mumbai, Maharastra |
Urban | DOTS centres |
266 new SPP |
mean age-31 years, Male- 59%, up to primary school- 37% |
6.0 | 31.0 | 4.0 | _ | 82.3% | 2.0 |
|
| ||||||||||||
| Rajeswari et al. (2002) * 18 | 1997- 1998 |
Chennai, Madurai, Chingleput and Vellore Tamil Nadu |
Both | Private and public health institution s |
531 new SPP |
aged> 45 years- 38%, Male-72%, Illiterate-30% |
20.0 | 23.0 | _ | 60.0 | 54.0% | _ |
|
| ||||||||||||
| Selvam et. al. (2007) * 19 | 2003 | all districts of Tamil Nadu |
Both | Tuberculo sis Units |
601 new SPP |
mean age-43 years, Male- 73%, Illiterate- 39% |
28.0 | 28.04 | _ | 62.0 | 43.0% | _ |
|
| ||||||||||||
| Tamhane et al. (2012) * 23 | 2002 | Mumbai, Maharashtr a |
Urban | DOTS Centres 12 wards |
150 new SPP |
median age-30 years, Male- 50%, illiterate- 25% |
15.0 | 31.0 | 2.0 | _ | 65.0% | _ |
|
| ||||||||||||
| Thakur et al. (2012) * 31 | 2009- 2010 |
Mandi district hospital, Himachal Pradesh |
Both | Patients under RNTCP |
234 new SPP |
aged> 35 years 50.9%, Male- 66.6%,Illiterate- 25.6% |
15.0 | 33.5 | 1.0 | 36.0 | 22.0% | _ |
| India Central TB Division (2013) * i 35 | 2011- 12 |
India central TB division’s internal Evaluation done across India |
_ | 5 NSP patients from each of the 330 Microscop y Centers in 66 districts |
1644 new SPP |
Mean age - 37 years, Male - 66% Female - 34% |
15.0 | 4.0 | 3.0 | _ | 48.0% | 2.2 |
|
| ||||||||||||
|
Median delays for
PTB patients (range) |
19.4
(6.0- 267.7) |
31.0
(4.0 to 54.5) |
2.5
(1.0- 8.0) |
57.5
(36.0 to 118.0) |
51.4%
(10.9%- 82.3%) |
2.5 (1.9-12.3) | ||||||
| Studies on delays in chest symptomatic patients | ||||||||||||
| Grover et. al (2003) * 33 | 1998- 2000 |
2 villages and Chandigarh City, Haryana |
Both | Communit y survey |
192 | aged 15-44 years- 45.5%, male-58%, Illiterate-32.5% |
56.6 | _ | _ | _ | 34.3% | _ |
|
| ||||||||||||
| Balasangameshwara et. al (1998) i15 | 1996- 1997 |
Dharmapuri , Tamil Nadu |
Both | Private and public health institution s |
673 | media age- 48years, (urban) & 42 (rural) |
18.0 | 35.0 | _ | 53.0 | 42.3% rural; 36.4% urban |
_ |
|
| ||||||||||||
| Charles et. al. (2010) * 17 | 2008 | Chennai & Madurai, Tamil Nadu |
Both | Communit y survey |
444 | male 51.2% | 16.0 | _ | _ | _ | 38.0% | _ |
|
| ||||||||||||
| Sudha et al (2003) * 20 | 1997 | Chennai & Madurai, Tamil Nadu |
Both | Communit y survey |
649 | Male-45.9%, >45 years- 52.3%, Up to primary -37% |
10.0 | _ | _ | _ | 37.7% | _ |
|
| ||||||||||||
| Tobgay et al. (2006) * 34 | 2003 | Eastern Sikkim |
Rural | 2 Tuberculo sis Units& 4 microscop y centres |
323 | median age 30 years, male- 58.8%, up to primary-33.1% |
21.0 | 7.0 | _ | _ | 26.0% | _ |
|
| ||||||||||||
| Ghosh et al. (2010)****32 | 2008 | Patpur, Bankura West Bengal |
Both | Communit y survey |
64 | age ≥45 years- 18.7%, Male-68.7% |
7.0 | _ | _ | _ | 37.5% | _ |
|
Median delays for
both PTB and chest symptomatic patients (range) |
18.4
(6.0- 267.7) |
31.0
(4.0 to 54.5) |
2.5
(1.0- 8.0) |
55.3
(36.0 to 118.0) |
48.0%
(10.9%- 82.3%) |
2.7 (1.9-12.3) | ||||||
Reported diagnostic delay and treatment delays together as health system delay.
New SPP: New smear positive patients
Reported diagnostic delay and treatment delays together as health system delay.
Reported diagnostic delay and treatment delays together as health system delay.
The average total delays were extracted from the primary studies (not by summing up patient delay, diagnostic delay and treatment delay to get the total when it was not reported by the authors).
Among 16 records reported health system delay, five reported diagnostic delay whereas one reported treatment delay only. Ten studies reported both delays; however, four of studies didn’t separate diagnostic and treatment delay, but reported them together as health system dely. In the box plot of health system delay, we use health system delays in these four studies as diagnosis delay, because it is relatively much larger than treatment delay.
Prospective recruitment;
Cross sectional study;
Retrospective cohort.
The study participants in the included studies were new PTB patients (n=17), which included new smear positive PTB patient (n=11); and CS patients (n=6). One14 of the sixteen studies conducted among PTB patients excluded HIV-TB co-infected patients. The sample sizes of the studies carried out in new PTB patients ranged from 53 to 2027; and from 192 to 649 in the studies conducted among CS patients.
Heterogeneity in definitions
Included studies used a variety of definitions for onset of symptoms and delays. The symptoms suggestive of PTB and various types of HCPs reported in the included studies are summarized in Table 1. Nine studies17, 20, 21, 23, 25, 29, 31-33 used onset of symptoms as any of the five cardinal TB manifestations i.e. cough ≥ 3 wks with/without chest pain, with or without fever, with or without loss of weight, with or without haemoptysis. Five of these nine studies also included other symptoms of TB3, 6, 14, 26, 27such as breathlessness, loss of appetite and wheezing. One study23 had included symptoms which patients perceived as TB. Furthermore, one study 34 defined cough lasting 3 weeks as onset of symptoms, and another study 18 defined it as coughing ≥ 2 weeks. Three studies15, 16, 28 defined coughing as onset of symptoms without a specific duration. Nine studies, did not report any or clear definition for onset of symptoms.
Table 1.
‘TB-related symptoms’ and first contact with health care providers / facilities used to define patient delay and diagnostic and health system delays
| “Symptoms” | Five cardinal TB symptoms: cough of ≥2 weeks or ≥3 weeks, chest pain, fever, loss of weight, haemoptysis. |
| Symptoms relevant to TB: breathlessness, loss of appetite | |
| Other symptoms/signs that patients attributed to TB | |
| Health care provider |
Traditional healers: faith healers, religious priest etc. |
| Pharmacies or chemist shops | |
| Non-allopathic practitioners: Homeopathy, Ayurveda, Unani, Siddha, acupuncturist etc. | |
| Unqualified medical practitioners: non-licensed practitioners, village health guides, traditional midwives etc. | |
| Qualified allopathic health care providers of both public and private sectors, specialist such as internal medicine and chest medicine etc. |
The first contact of the patient with a HCP used for defining DxD also varied across the included studies. Six studies14, 16, 18, 31-33used qualified allopathic practitioner for defining first contact with HCP. However, three studies19, 21, 34 defined initial contact as a patient seeking care from either a qualified or an unqualified HCP. This includes non-allopathic practitioners such as Homeopathy, Ayurveda, Unani, Siddha, acupuncturist, faith healers, etc. Seven studies3, 4, 12, 15, 26, 29defined self-medication, visiting pharmacies and chemists shops as the first contact with a HCP. The remaining seven studies did not provide a clear definition of a HCP.
Six studies18, 23, 24, 28, 31, 33 defined health system delay (HSD) as the interval between the first contact with a HCP and the confirmation of TB diagnosis (i.e. DxD). However, four studies17, 19, 24, 34 defined the end point of HSD as the initiation of (correct) anti-TB treatment. Additionally, six studies22-24, 28, 30, 31 separately defined the interval between confirmation of diagnosis and initiation of anti-TB treatment as treatment delay. Nine studies did not provide definitions for either HSD or DxD and RxD.
Because of this heterogeneity in definitions, a decision was made to not perform meta-analysis, but instead summarize the results as simple averages in tables and distribution plots. Even these numbers need to be interpreted cautiously because of the underlying heterogeneity. Notably, the study by Bawankule et al.25 included patients who were severely ill and hospitalized in a tertiary care hospital. This study was identified as an outlier in the box plots, when compared to studies that included ambulatory patients.
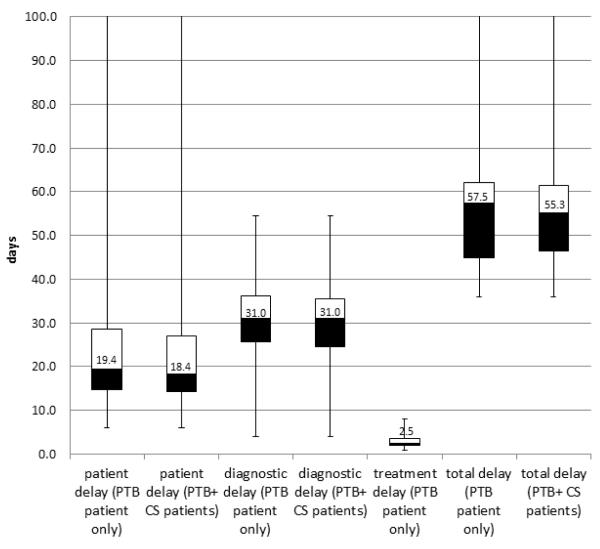
Patient delay
The reported average PD for PTB patients (n=17 studies) and for all patients including CS patients (n= 6 studies) had the same range, i.e. from 6.0 to 267.7 days, but medians were 19.4 days and 18.4 respectively. There was much variability across studies, as shown in Table 2.
Health system delay (diagnostic and treatment delays)
The reported DxD among PTB patients ranged from 4.0 to 54.5 days, and the median was 31.0 days (Figure 3). The median and the range were the same for all 16 studies (14 studies on PTB patients and two studies on CS patients) which reported DxD. The reported RxDs (in eight studies on PTB patients) ranged from 1 to 8 days, with a median of 2.5 days. None of the studies done among chest symptomatics reported data on treatment delay (Table 2).
Figure 3. Distribution of patient delay (PD), diagnostic delay (DxD), treatment delay (RxD), and total delay (TD) among PTB patients and chest symptomatics in India.
Box plots depict the median (central line), inter quartile range (IQR) (box) and range (whiskers).
PTB - pulmonary TB
CS - chest symptomatic
Total delay
Total delay data were reported in 10 studies (nine studies on PTB patients and one study on CS patients). Total delay ranged from 36.0 to 118.0 days in studies on PTB patients and median delay was 57.5 days (Figure 3). The median TD in all studies (including chest symptomatics) was 55.3 days and the range was 36.0 to 118.0 days (Table 2).
Care seeking and number of providers seen
Although there was a lot of variation, ranging from 11% to 82%, on average 48% (median) of TB patients (both PTB and chest symptomatic patients) first visited private/informal sectors. Additionally, median number of HCPs consulted before reaching a diagnosis (reported in eight studies) was 2.7 (range 1.9 to 12.3) (Table 2).
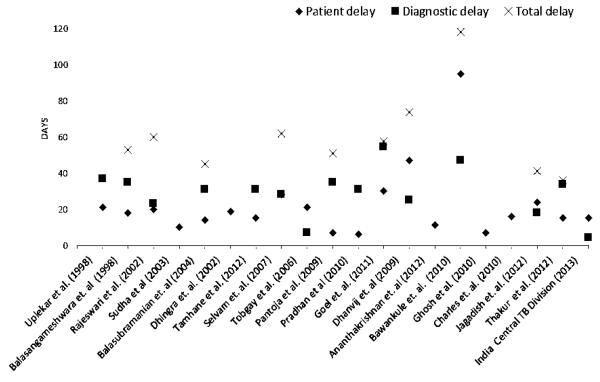
Subgroup analysis by study period
Among 20 studies where the time period of the research was clearly reported, four studies were conducted prior to the implementation of DOTS. All types of delays (except RxD) were plotted according to the year of study, but not according to the years of publication (Figure 4). Treatment delays were not included in the graph due to the limited amount of data (only eight studies reported RxD). This plot shows no evidence that PD, DxD and TD have reduced over time. However, considerable heterogeneity is evident, and study populations and definitions are not consistent across studies. As mentioned earlier, the study by Bawankule et al.25 is the outlier (Figure 4)
Figure 4. Patient delay, diagnostic delay and total delay* among PTB and chest symptomatic patients, with studies ordered chronologically.
*The total delays were extracted from the primary studies (not by summing up patient delay, diagnostic delay and treatment delay to get the total when it was not reported by the authors).
Subgroup analysis: rural versus urban
We did a sub-group analysis on six studies done in urban setting and five studies in rural setting (Table 3). Of these 11 studies, ten included PTB patients while the study by Tobgay et al. (2006)34 was carried out among CS patients. The sample of patients studied in urban and rural settings ranged from 150 to 468 and 53 to 2027, respectively.
Table 3.
Rural versus urban comparison of ‘delays’ and health seeking behavior of PTB and CS patients
| Patient delay (days) |
Diagnostic delay (days) |
Treatment delay (days) |
Total delay (days) |
% private sector as first point of care |
Average number of HCPs consulted |
|
|---|---|---|---|---|---|---|
| median (IQR) | median (IQR) | median (IQR) | median (IQR) | median | median | |
| Urban (n=6) | 13.2 (6.75.-20.1) | 31.0 (18.8-31) | 3.0 (2.5-3.5) | 46.0 (43.5-48.5) | 65% | 2.8 |
| Rural (n=5) | 34.1 (17.5-58.0) | 28.0 (20.5-35.0) | 4.9 (3.3-6.4) | 73.9 (59.5-96.0) | 38% | 3.1 |
| Total (n=23) | 18.4 (14.3-27.0) | 31.0 (24.5-35.4) | 2.5 (1.9-3.6) | 55.3 (46.5-61.5) | 48% | 2.7 |
PTB: pulmonary TB
CS: chest symptomatic
HCP: healthcare provider
The median PD, DxD and TD in urban areas were 13.2 days, 31.0 days, and 46.0 days; whereas those in rural areas were 34.1 days, 28.0 days, and 73.9 days. PD and TD were higher in rural areas but DxD was nearly the same in both urban and rural areas. The percentage of private sector as first point of care was much higher in urban than in rural areas (65% versus 38%) (Table 3). The treatment delays were not compared because of the limited available data in these 11 studies.
Significant risk factors for delays
Risk factors for delay were not reported in all the included studies – only 5 studies reported adjusted odd ratios (aOR) for delays from multivariable analysis. Tables 4 and 5 only included the risk factors that were positively associated with PD and HSD. Prolonged PD appeared to be strongly associated with the type of HCP as the first contact, especially if first action after onset of symptoms was self-medication as well as the inability to pay HCP (aORs were 7.831 and 2.923 respectively). Two studies reported that first contact of patient with government HCP was a risk factor for prolonged PD (aORs were 2.218 and 2.7634) (Table 4).
Table 4.
Significant risk factors for patient delay by multivariate analysis
| Covariates | Risk factor for patient delay | Adjusted Odds ratio (aOR) |
95 % CIs | Reference |
|---|---|---|---|---|
| first contact | self-medication | 2.28 | 1.0-5.18 | Tobgay 200634 |
| self-medication/consulting drug store |
7.8 | 4.17-14.58 | Thakur 201231 | |
| use of traditional healer | 2.18 | 1.03-4.61 | Tobgay 200634 | |
| Initial consultation with government HCP (compared with private provider ) |
2.2 | 1.5-3.4 | Rajeswari 200218 | |
| first contact with government HCP | 2.76 | 1.15-6.62 | Tobgay 200634 | |
|
monetary
concerns |
family income < 3000 rupee | 2.5 | 1.23-6.15 | Thakur 201231 |
| inability to pay the HCP | 2.9 | 1.1-7.1 | Tamhane 201223 | |
| cost of treatment > 400 rupee | 2.52 | 1.17-5.38 | Tobgay 200634 | |
|
smoking/
alcohol |
alcohol use | 1.6 | 1-2.4 | Rajeswari 200218 |
| smoking | 1.9 | 1.3-2.6 | Selvam 200719 | |
|
accessibility of
healthcare facilities |
mode of transportation | 2 | 1.3-3.1 | Selvam 200719 |
| residing 2 km from a health facility | 1.6 | 1-2.4 | Rajeswari 200218 | |
| stigma | high stigma | 1.81 | 0.99-3.32 | Thakur 201231 |
PD = Patient delay
HCP= Health care Provider
Table 5.
Significant risk factors for health system delay by multivariate analysis
| Covariate | Risk factor for health system delay | Adjusted Odds ratio (aOR) |
95% CIs | Reference |
|---|---|---|---|---|
| first contact | private HCP | 33.1 | 13.44-81.5 | Tobgay 200634 |
| private HCP | 6.68 | 2.75-16.23 | Thakur 201231 | |
| private HCP | 4 | 2.6-6.4 | Rajeswari 200218 | |
| non-allopathic HCP | 12.3 | 1.4-104.9 | Tamhane 201223 | |
| non-government sector | 2 | 1.5-2.7 | Selvam 200719 | |
|
number of
HPCs visited |
>3 consultations with a HCP | 5 | 1.4-17.4 | Tamhane 201223 |
| Multiple health seeking encounters with HCP |
8 | 4.0-16.2 | Thakur 201231 | |
|
monetary
concerns |
cost of treatment (>400 rupee) | 2.5 | 1.22-5.13 | Tobgay 200634 |
| expenses (> median) incurred before initial diagnosis |
2.58 | 1.34-4.95 | Thakur 201231 | |
|
accessibility
of healthcare facilities |
longer distance of healthcare facility | 1.8 | 1.2-2.5 | Selvam 200719 |
| distance > 2km from residence to health facility |
1.8 | 1.1-28 | Rajeswari 200218 | |
|
smoking/
alcohol |
alcohol use | 1.6 | 1-2.6 | Rajeswari 200218 |
|
duration of
coughing |
shorter duration of cough | 2.6 | 1.6-4.3 | Rajeswari 200218 |
| longer duration of cough | 2.5 | 1.8-3.6 | Selvam200719 |
HSD = Health system delay
HCP= Health care Provider
In contrast, initially seeking care from private HCP was clearly a significant risk factor for prolonged HSD (aORs were 33.134, 6.6831 and 4.018). Although above-mentioned odds ratios vary, this factor still ranks the most strongly associated factor with HSD. In addition, visiting a non-allopathic HCP first was also an important risk factor (aOR=12.323). We also found that consulting multiple HCPs was associated with prolonged HSD (aOR=8.031) (Table 5).
DISCUSSION
Principal findings
Despite the widespread implementation of the DOTS strategy, TB incidence continues to be high in India1. Our review shows that patient and health system delays are considerable, and may partially explain the current epidemiology.5, 36 A sizeable fraction of persons with PTB or presumed PTB first visit informal and private sector providers, particularly in urban areas, and multiple visits to HCPs appears to be an important risk factor for total delay. Data on risk factors for delays are limited and further work is necessary to better understand patient pathways to care in India and to understand why patients seek private sector care and why they move between providers.
The previous review by Sreeramareddy et al.2 included 39 studies from 45 low- and-middle income countries, and estimated average patient delay, health system delay and total delay as 31.7 days, 28.4 days and 67.8 days, respectively. Patient delay in our review was much lower but diagnostic delay was slightly higher than that of previous review which included only 3 studies from India and did not include treatment delay or consider treatment initiation as an end point for health system delay.
The average patient delay (18.4 days) in our review is only slightly longer than the 2 weeks of cough criterion that is used to screen for TB. However, average patient delay was twice as much in rural areas where the majority of India’s population lives, suggesting patient delay may still be a substantial problem for many. In addition, diagnostic delays both in rural and urban areas were high. These results suggest that even when patients seek care in a timely manner, significant time can be lost after their first contact with the healthcare system. Incentivizing first-contact and informal providers to refer persons with TB symptoms to the RNTCP may be one approach to reducing such delay.
Total delay in our review was lower than that reported (72 days) by Storla et al.3 which included studies from high income countries, and a single study from India. Storla and colleagues neither summarized patient and health system delays separately nor reported treatment delays. Hence any comparisons of our results with those of the previous reviews should be interpreted cautiously.
Factors such as type of healthcare provider, treatment cost, income, accessibility to health care facilities were significantly associated with delays in our review similar to summary results reported by Storla et al.3 However, Storla et al. reported that factors such as HIV, female gender, negative sputum smear, income and education were also associated with delays, but these factors were not reported in our review since only five of the 23 included studies had assessed the risk factors for delays.
Studies included in the review spanned a period of 1998 to 2013, and there is insufficient evidence to conclude that delays have reduced during this period. However, time trend data must be interpreted with caution because representative data collected using the same definitions is not available over time.
Strengths and limitations of the review
Our search strategy was rigorous and multiple sources were searched. Two reviewers independently selected studies and extracted data. Authors were contacted up to three times to retrieve relevant data. Where possible, we analyzed the data separately as patient, health system and total delay. We also conducted subgroup analyses to better understand the reasons for variations in delays reported across studies.
However, our review had limitations. There was considerable variation in how key terms were defined in the primary studies, such as ‘patient delay’, ‘health system delay’, ‘diagnostic delay’, treatment delay’, ‘health care provider’ and ‘symptoms’. The start point and end point of ‘delay’ differ and therefore the duration of ‘delay’ varied. Almost inevitably, there was an element of poor recall or recall bias in each study. Most studies included newly diagnosed smear-positive patients to minimize the recall bias. Diagnostic delay is likely to be higher for smear-negative TB patients but most studies recruited only smear-positive patients. Furthermore, while some studies accounted for first-contact care from unqualified HCPs, others only accounted for qualified HCPs.
Another limitation is generalizability of the results since most of the studies interviewed patients from government health facilities and recruited participants mainly from hospitals and clinics (often TB centers) and there were few studies from poorer, highly populated, and high TB burden states. Future studies should focus on patients from private health facilities and patients and symptomatics identified during population-based surveys to obtain representative data and in high-burden states. As with any systematic review, it is possible that we missed some studies.
Policy implications and research directions
In India, patients with TB symptoms spend a considerable length of time consulting various healthcare providers before final diagnosis. First consultation with a private/informal health care provider was common, and a significant risk factor for prolonged health system delay. These results underscore the importance of private sector engagement to shorten the care-seeking pathway. Recognizing this reality, the RNTCP has announced a National Strategic Plan (2012 – 2017) with the goal of “universal access to quality TB diagnosis and treatment for all TB patients in the community” and this plan envisions large-scale engagement of the private sector to reduce diagnostic delays and improve quality of care.37 More accurate, rapid molecular tests combined with information and communication technologies (ICT), and innovative delivery approaches to engage the private sector could be tried out to reduce overall delay and improve case notification.38
From a research perspective, there is a need for RNTCP to collect standardized data on diagnostic and treatment delays as part of routine monitoring and evaluation. Ideally, such data should include patients in both public and private sectors, and capture information on how many providers were seen before TB diagnosis, how long the process took, and what costs were incurred by patients.
Our review also underscores the need to better understand the quantitative relationship between diagnostic delays and TB transmission, and determine the likely number of secondary cases generated by the long pathway to care. Here, there are several unknowns.5, 39, 40 How big a reduction in diagnostic delay is necessary before a meaningful decline in TB incidence occurs? Do delays before diagnosis translate directly to duration of infectiousness or do most transmission events cluster toward the beginning or end of the infectious period? Do symptoms correlate with infectiousness? Does the risk of transmission vary dramatically across individuals (e.g. a few individuals with long delays may account for much of the avertible secondary cases)? Our review does not address these issues, but may be helpful to mathematical modelers exploring these complex questions.
Acknowledgements
We are very grateful to the authors of the included studies who provided us unpublished or additional data and verified the data extracted by us. We thank Ms. Genevieve Gore, a medical librarian at McGill University, Montreal, for her support. We acknowledge helpful input from Dr Puneet Dewan and Dr David Dowdy. SS is supported by a fellowship from Research Institute of McGill University Health Centre. RS is supported by a Harvard T32 post-doctoral HIV Clinical Research Fellowship (NIAID AI 007433). MP is supported by a salary award from Fonds de recherche du Québec – Santé.
Footnotes
Conflicts of interest: The authors have no financial or industry conflicts to declare. MP is a consultant for the Bill and Melinda Gates Foundation (BMGF). Views expressed reflect his own.
References
- 1.World Health Organization . Global tuberculosis report 2012. Geneva: 2012. [Google Scholar]
- 2.Sreeramareddy C, Panduru K, Menten J, Van den Ende J. Time delays in diagnosis of pulmonary tuberculosis: a systematic review of literature. BMC Infectious Diseases. 2009;9(1):91. doi: 10.1186/1471-2334-9-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC public health. 2008;8:15. doi: 10.1186/1471-2458-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yimer S, Bjune G, Alene G. Diagnostic and treatment delay among pulmonary tuberculosis patients in Ethiopia: a cross sectional study. BMC Infectious Diseases. 2005;5(1):112. doi: 10.1186/1471-2334-5-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dye C, Williams BG. The population dynamics and control of tuberculosis. Science. 2010;328(5980):856–61. doi: 10.1126/science.1185449. [DOI] [PubMed] [Google Scholar]
- 6.Ministry of Health and Family Welfare Report of the National Commission on Macroeconomics and Health. 2012.
- 7.Sudhinaraset M, Ingram M, Lofthouse HK, Montagu D. What is the role of informal healthcare providers in developing countries? A systematic review. PLoS One. 2013;8(2):e54978. doi: 10.1371/journal.pone.0054978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gautham M, Binnendijk E, Koren R, Dror DM. ‘First we go to the small doctor’: first contact for curative health care sought by rural communities in Andhra Pradesh & Orissa, India. The Indian journal of medical research. 2011;134(5):627–38. doi: 10.4103/0971-5916.90987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Y, Ehiri J, Tang S, et al. Factors associated with patient, and diagnostic delays in Chinese TB patients: a systematic review and meta-analysis. BMC medicine. 2013;11(1):156. doi: 10.1186/1741-7015-11-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Finnie RK, Khoza LB, van den Borne B, Mabunda T, Abotchie P, Mullen PD. Factors associated with patient and health care system delay in diagnosis and treatment for TB in sub-Saharan African countries with high burdens of TB and HIV. Tropical Medicine & International Health. 2011;16(4):394–411. doi: 10.1111/j.1365-3156.2010.02718.x. [DOI] [PubMed] [Google Scholar]
- 11.Suganthi P, Chadha VK, Ahmed J, et al. Health seeking and knowledge about tuberculosis among persons with pulmonary symptoms and tuberculosis cases in Bangalore slums. The international journal of tuberculosis and lung disease : the official journal of the International Union against Tuberculosis and Lung Disease. 2008;12(11):1268–73. [PubMed] [Google Scholar]
- 12.Pantoja A, Floyd K, Unnikrishnan KP, et al. Economic evaluation of public-private mix for tuberculosis care and control, India. Part I. Socio-economic profile and costs among tuberculosis patients. The international journal of tuberculosis and lung disease : the official journal of the International Union against Tuberculosis and Lung Disease. 2009;13(6):698–704. [PubMed] [Google Scholar]
- 13.Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine. 2011;155(8):529–36. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 14.Ananthakrishnan R, Jeyaraju AR, Palani G, Sathiyasekaran BWC. Care seeking behavior of the TB patients who were registered in an urban government tuberculosis control in Chennai, Tamilnadu, India. Journal of Clinical and Diagnostic Research. 2012;6(6):990–3. [Google Scholar]
- 15.Balasangameshwara VHSV, Jagannath PS, Sumathi G, Vasudevan K, Toru Mori. Health seeking pattern and patient & provider delay in tuberculosis case finding process. The international journal of tuberculosis and lung disease : the official journal of the International Union against Tuberculosis and Lung Disease. 1998;2(11)(Suppl 2):s401–s2. [Google Scholar]
- 16.Balasubramanian R, Garg R, Santha T, et al. Gender disparities in tuberculosis: report from a rural DOTS programme in south India. The International Journal of Tuberculosis and Lung Disease. 2004;8(3):323–32. [PubMed] [Google Scholar]
- 17.Charles N, Thomas B, Watson B, Chandrasekeran V, Wares F. Care seeking behavior of chest symptomatics: a community based study done in South India after the implementation of the RNTCP. PloS one. 2010;5(9):e12379. doi: 10.1371/journal.pone.0012379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rajeswari R, Chandrasekaran V, Suhadev M, Sivasubramaniam S, Sudha G, Renu G. Factors associated with patient and health system delays in the diagnosis of tuberculosis in South India. The international journal of tuberculosis and lung disease : the official journal of the International Union against Tuberculosis and Lung Disease. 2002;6(9):789–95. [PubMed] [Google Scholar]
- 19.Selvam JM, Wares F, Perumal M, et al. Health-seeking behaviour of new smear-positive TB patients under a DOTS programme in Tamil Nadu, India, 2003. The international journal of tuberculosis and lung disease : the official journal of the International Union against Tuberculosis and Lung Disease. 2007;11(2):161–7. [PubMed] [Google Scholar]
- 20.Sudha G, Nirupa C, Rajasakthivel M, et al. Factors influencing the care-seeking behaviour of chest symptomatics: a community-based study involving rural and urban population in Tamil Nadu, South India. Tropical Medicine & International Health. 2003;8(4):336–41. doi: 10.1046/j.1365-3156.2003.01010.x. [DOI] [PubMed] [Google Scholar]
- 21.Dhanvij P, Joshi R, Kalantri S. Delay in diagnosis of tuberculosis in patients persenting to a teriary care hospital in rural central india. Journal of Mahatma Gandhi Institute of Medical Sciences. 2009;14(ii):56–63. [Google Scholar]
- 22.Pradhan A, Kielmann K, Gupte H, Bamne A, Porter JD, Rangan S. What‘outliers’ tell us about missed opportunities for tuberculosis control: a cross-sectional study of patients in Mumbai, India. BMC public health. 2010;10(1):263. doi: 10.1186/1471-2458-10-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tamhane A, Sathiakumar N, Vermund S, Kohler CL, Karande A, Ambe G. Pulmonary tuberculosis in Mumbai, India: Factors responsible for patient and treatment delays. International Journal of Preventive Medicine. 2012;3(8) [PMC free article] [PubMed] [Google Scholar]
- 24.Uplekar M, Juvekar S, Morankar S, Rangan S, Nunn P. Tuberculosis patients and practitioners in private clinics in India. The international journal of tuberculosis and lung disease : the official journal of the International Union against Tuberculosis and Lung Disease. 1998;2(4):324–9. [PubMed] [Google Scholar]
- 25.Bawankule S, Quazi S, Gaidhane A, Khatib N. Delay in DOTS for new pulmonary tuberculosis patient from rural area of Wardha District, India. Online Journal of Health and Allied Sciences. 2010;9(1) [Google Scholar]
- 26.Chakraborty A, Krishnamurthy M, Sashidhara A, Juvekar S. Missed opportunities for diagnosis of Pulmonary Tuberculosis: A study among rural patients seeking relief on their own under the tuberculosis programme in India. Indian Journal of Tuberculosis. 2001;48(4):181–92. [Google Scholar]
- 27.Goel K, Kondagunta N, Joycee Soans S, Ramachandra Bairy A, Goel P. REASONS FOR PATIENT DELAYS & HEALTH SYSTEM DELAYS FOR TUBERCULOSIS IN SOUTH INDIA. Indian Journal of Community Health. 2012;23(2):87–9. [Google Scholar]
- 28.Jagadish S, Saraswathi S, Divakar S. A study of impact of determinants of patients and health system delay on tuberculosis diagnosis and treatment in Bangalore. Indian journal of Community Health. 2012;24(4):319–24. [Google Scholar]
- 29.Dhingra VK, Rajpal S, Taneja DK, Kalra D, Malhotra R. Health care seeking pattern of tuberculosis patients attending an urban TB clinic in Delhi. The Journal of communicable diseases. 2002;34(3):185–92. [PubMed] [Google Scholar]
- 30.Paul D, Busireddy A, Nagaraja SB, et al. Factors Associated with Delays in Treatment Initiation after Tuberculosis Diagnosis in Two Districts of India. Plos One. 2012;7(7) doi: 10.1371/journal.pone.0039040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thakur R, Murhekar M. Delay in diagnosis and treatment among TB patients registered under RNTCP Mandi, Himachal Pradesh, India, 2010. The Indian journal of tuberculosis. 2013;60(1):37–45. [PubMed] [Google Scholar]
- 32.Ghosh S, Sinhababu A, Taraphdar P, Mukhopadhyay DK, Mahapatra BS, Biswas AB. A study on care seeking behavior of chest symptomatics in a slum of Bankura, West Bengal. Indian journal of public health. 2010;54(1):42–4. doi: 10.4103/0019-557X.70553. [DOI] [PubMed] [Google Scholar]
- 33.Grover A, Kumar R, Jindal S. Treatment seeking behaviour of chest symptomatics. Indian Journal of Tuberculosis. 2003;50(2):87–94. [Google Scholar]
- 34.Tobgay KJ, Sarma PS, Thankappan KR. Predictors of treatment delays for tuberculosis in Sikkim. The National medical journal of India. 2006;19(2):60–3. [PubMed] [Google Scholar]
- 35.Central TB Division - Ministry of Health and Family Welfare - New Delhi. Annual Report (internal) 2013.
- 36.Dye C. The potential impact of new diagnostic tests on tuberculosis epidemics. The Indian journal of medical research. 2012;135(5):737–44. [PMC free article] [PubMed] [Google Scholar]
- 37.Sachdeva KS, Kumar A, Dewan P, Kumar A, Satyanarayana S. New vision for Revised National Tuberculosis Control Programme (RNTCP): Universal access - “reaching the un-reached”. Indian J Med Res. 2012;135(5):690–4. [PMC free article] [PubMed] [Google Scholar]
- 38.Pai M. Promoting affordable and quality tuberculosis testing in India. J Lab Physicians. 2013;5(1):1–4. doi: 10.4103/0974-2727.115895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dowdy DW, Basu S, Andrews JR. Is passive diagnosis enough? The impact of subclinical disease on diagnostic strategies for tuberculosis. Am J Respir Crit Care Med. 2013;187(5):543–51. doi: 10.1164/rccm.201207-1217OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dowdy DW, Dye C, Cohen T. Data needs for evidence-based decisions: a tuberculosis modeler’s ‘wish list’. The international journal of tuberculosis and lung disease : the official journal of the International Union against Tuberculosis and Lung Disease. 2013;17(7):866–77. doi: 10.5588/ijtld.12.0573. [DOI] [PMC free article] [PubMed] [Google Scholar]