Abstract
Background
African Americans have more severe hypertensive nephrosclerosis than white Americans, possibly at similar levels of blood pressure. Glomerular volume is increased in African Americans relative to whites, but it is uncertain how this relates to nephrosclerosis and whether it contributes to or compensates for glomerulosclerosis.
Methods
Stereological disector/fractionator estimates of glomerular number (Nglom) and average glomerular volume (Vglom) were obtained on autopsy kidneys of 171 African Americans and 131 whites. Eighty-eight African Americans and 49 whites were identified as hypertensive. Nephrosclerosis was measured morphometrically as the percentage of glomerulosclerosis, proportion of cortical fibrosis and interlobular artery intimal thickness, and analyzed with Vglom by age, race, gender, body mass index (BMI) and blood pressure.
Results
African Americans were more frequently hypertensive (58.5%) than whites (35.8%) and when hypertensive had higher levels of blood pressure (P = 0.02). Nglom was significantly lower in hypertensive compared with non-hypertensive subjects among white women (P = 0.02) but not white males (P = 0.34) or African American females (P = 0.10) or males (P = 0.41). For each race and gender, glomerulosclerosis, cortical fibrosis and arterial intimal thickening were statistically correlated with age (P < 0.001) and hypertension (P < 0.001) and increased Vglom with hypertension (P < 0.001) and BMI (P < 0.001). In multivariate analysis, African American race was associated with increased Vglom (P = 0.01) and arterial intimal thickening (P < 0.01), while interactions between race and blood pressure indicated that the severity of nephrosclerosis including increased Vglom was linked most directly to hypertension without significant contributions from race. The hypertension-associated enlargement of Vglom was present with mild degrees of glomerulosclerosis and changed little as the severity of glomerulosclerosis increased.
Conclusions
Glomerular hypertrophy was identified as an integral feature of hypertensive nephropathy and appeared to precede rather than compensate for glomerulosclerosis. An effect of race on Vglom and arterial intimal thickening seemed to be related to the more frequent and more severe hypertension among African Americans.
Keywords: gender, glomerulomegaly, glomerulosclerosis, hypertension, race
INTRODUCTION
Hypertension is a disease of aging. It is identified in fewer than 10% of persons under 35 years of age but affects >60% of the US population after age 65 [1, 2]. It is more prevalent and tends to be more severe and to begin at an earlier age in African Americans than whites, and African Americans have a greater risk of end-stage renal disease (ESRD) attributable to hypertension [2, 3, 4].
Hypertension results in a complex of progressive kidney changes recognized as arteriosclerosis, cortical fibrosis, tubular atrophy and loss, and glomerulosclerosis that are pathologically referred to as arteriolar or hypertensive nephrosclerosis [3, 5, 6, 7]. Glomeruli become globally sclerotic in two distinct patterns. One is termed obsolescence and the other solidification [8, 9, 10, 11]. The predominant form of glomerulosclerosis in hypertensive nephropathy is obsolescence that is recognized by collapse of the glomerular tuft and intracapsular fibrosis [7, 12]. Obsolescence is considered to be the result of reduced glomerular perfusion because of arteriosclerotic narrowing of preglomerular arteries and arterioles. Glomerular solidification expands the glomerular tuft by an increased accumulation of mesangial matrix and is proposed to be a complication of glomerular hyperfiltration secondary to a loss of afferent arteriolar autoregulation [8, 9, 10, 11, 13, 14].
A linear concept of the progression of hypertensive nephropathy suggests that the severity of nephrosclerosis, and particularly the extent of glomerulosclerosis, corresponds to a reduction in glomerular filtration rate (GFR). Contrast-enhanced computed tomography imaging of the kidneys of transplant donors have shown an age-related loss of cortical volume that correlates with a reduction in GFR [7, 12, 15]. Despite this tendency, individuals at increased risk of chronic kidney disease by virtue of obesity, lipid abnormalities, hypertension and microalbuminuria demonstrate increases in cortical volume and GFR with mild and moderate nephrosclerosis [7, 12, 15]. In these situations, single nephron filtration rates are increased, and the increase is thought to be the result of a compensatory enlargement in the volume of functioning glomeruli [7, 12, 15].
On the basis of clinical observations and experimental models of nephron deficiency, glomerular hypertrophy is suggested to precede glomerulosclerosis with the glomerulosclerosis being attributed to glomerular hypertension [8, 16, 17]. This concept may explain glomerular solidification but is difficult to reconcile with glomerular obsolescence being the principal form of glomerulosclerosis found in hypertensive nephropathy, at least in its early and intermediate stages [18, 19, 20]. However, it is not at all clear whether glomerular obsolescence is a direct result of reduced glomerular perfusion, or whether arteriosclerosis, glomerular obsolescence and glomerular solidification share a common developmental mechanism [7, 8, 10, 12, 15]. In the later stages of hypertensive nephropathy, glomerular solidification certainly becomes prominent, if not the predominant form of glomerulosclerosis, as renal function decompensates [8, 10, 21].
Renal biopsy and autopsy studies have found that African Americans have larger glomeruli than whites [22–25]. Furthermore, the African American Study of Kidney Disease (AASK) and Hypertension biopsy series of hypertensive nephrosclerosis showed that African Americans had more severe renal arteriosclerosis and glomerulosclerosis than whites, that glomerular solidification was more frequent and that the severity of the changes could not be attributed to racial differences in blood pressure [9, 10]. These observations suggested that the glomerular hypertrophy of African Americans reflects their greater risk of hypertension-associated kidney disease.
Our research over the last decade has analyzed glomerular number (Nglom) and glomerular volume (Vglom) in a large sample of kidneys by the fractionator/disector method to test the hypothesis that low Nglom may contribute to higher rates of hypertension among African Americans [18, 19, 20, 26]. The studies have not identified any significant difference in Nglom between hypertensive and non-hypertensive African Americans, and no significant racial difference has been found despite African Americans being much more frequently hypertensive [18, 19, 20, 26]. Throughout the several analyses, an inverse relationship with Nglom was found to be the strongest determinant of Vglom. This inverse relationship is seen soon after adult glomerular size is attained and appears to be an inherent feature of kidney growth in which for any level of Nglom, total glomerular volume tends toward a middle range [18, 19, 24, 26]. Nevertheless, among adults, African Americans were found to have larger glomeruli than whites despite the similar numbers of glomeruli [18, 19, 24, 26].
The aims of this current study are to evaluate the microanatomical changes of hypertensive nephrosclerosis and their relationships to age, race, gender, body mass index (BMI) and blood pressure. The associations emphasized variations in glomerular volume in an attempt to delineate relationships between Vglom, race and glomerulosclerosis.
MATERIALS AND METHODS
Specimen and subject data collection
This research used human autopsy tissue. The study was approved by the Institutional Review Board of the University of Mississippi Medical Center and the Human Research Ethics Committee of Monash University. Permission for autopsy was obtained from first-of-kin.
Right kidneys were collected at autopsy and perfusion fixed with 10% formaldehyde at the University of Mississippi Medical Center (Jackson, MS, USA) between the years 1998 through 2005. The research was a study of glomerular number and volume in persons without known renal disease who, because of their residence in Mississippi, may have been at high risk for primary hypertension and hypertensive vascular disease. The inclusion criteria required that kidneys be: (i) equal or approximately equal in size, (ii) grossly normal or show mild-to-moderate arteriolonephrosclerosis with a uniformly granular subcapsular cortex. Kidneys from patients with diabetes were analyzed if they showed mild-to-moderate arteriolonephrosclerosis but were excluded if there was microscopically a diabetic nephropathy. On this basis, kidneys of 11 diabetics were used, 9 African Americans and 2 whites.
The exclusion criteria consisted of: (i) kidneys involved by coarse pits or angular or depressed cortical scars, in order to exclude examples of ischemic nephropathy and pyelonephritis and not to have glomerular number reduced by severe renal scarring and advanced glomerulosclerosis. (ii) Kidneys of patients who had premorbid clinically diagnosed kidney disease. This was never a problem, as patients in this category were autopsied for complications of dialysis and in one instance death due to pulmonary emboli complicating a membranous nephropathy. (iii) Cases of congenital heart disease including bicuspid aortic valves, hereditary hypertrophic cardiomyopathy, dilated cardiomyopathy and cor pulmonale because normal cardiac function, and blood pressure regulation may not have been present and heart weight would be increased independent of blood pressure.
Included subjects were 1 month to 89 years old. Twenty-two were under 1 year of age and 13 were older than 65. The study cohort consisted of 86 African American males, 94 African American females, 87 white males and 52 white females. The causes of death were coronary artery disease (CAD) and/or hypertensive cardiac disease, 26%; cerebrovascular disease (CVD), 7%; pulmonary embolus, 7%; neoplastic, hematologic or infectious disease, 13%; pulmonary disease, 10%; accident, 12%; homicide, 5%; suicide, 6%; neurological disease not CVD, 3%; unknown, 4%; sudden infant death syndrome, 3%; cardiac not CAD or hypertensive disease, 4%; and complications of prematurity, 1%.
Clinical information was obtained from University of Mississippi Medical Center records and from the investigative reports of the county Medical Examiner. Blood pressures without medication were obtained from on 115 African Americans and 67 whites. Blood pressure from terminal hospital admissions were not used unless patients were diagnosed as hypertensive and blood pressures were elevated. Mean arterial blood pressure (MAP) was calculated from an average of at least three blood pressure determinations.
The patients were categorized on the basis of a history of hypertension, consistently elevated blood pressure (≥140/90 mmHg), the presence of cardiomegaly and the severity of intrarenal arteriolosclerosis as previously described [19, 20]. Patients were also categorized on the basis of diabetes, death due to CAD or CVD and treatment for hypertension. Patients were recorded as treated for hypertension if there was any statement of such treatment in the medical records or medical examiners' reports.
Measurement of total glomerular number (Nglom) and mean glomerular volume (Vglom)
Kidneys were perfused with 10% buffered formalin and then bisected and immersed in 10% formalin for 10 days. Afterward, both halves of the kidney were cut into slices 4 mm thick and every fourth slice of both halves was sampled for stereology beginning with the first slice selected as a random number from 1 to 4. The selected slices were sent to Monash University where they were processed for embedding in glycolmethacrylate for the stereological estimation of total glomerular number (Nglom) and mean glomerular tuft volume (Vglom, µm3 × 106) using the physical disector/fractionator method [27].
Measurement of glomerulosclerosis, cortical fibrosis and arteriolosclerosis
Representative kidney blocks from the upper pole and the mid-portion of the kidney not sampled for stereology were paraffin embedded. Sections were cut at 4 μm and stained with periodic acid-Schiff (PAS)-hematoxylin and picrosirius red stains for fibrillar collagen.
Measurement of the percentage of glomerulosclerosis and arterial intimal thickening used PAS-hematoxylin stained sections. The percentage of sclerotic glomeruli was estimated by counting sclerosed and non-sclerosed glomeruli in non-overlapping ×100 microscopic fields moving from the subcapsular surface to inner cortex with at least 400 glomeruli being counted per subject. The severity of arteriosclerosis was measured as a ratio of the thickness of the intima to the outer wall diameter at a magnification of ×400 in interlobular arteries 90–250 µm in diameter using the linear measurement function of Image-Pro Plus morphometric software (Media Cybernetics Inc., Bethesda, MD, USA). Cortical fibrosis was measured in ×200 images as the proportion of cortex staining red with the picrosirius stain using the automated Image-Pro Plus area counting function.
Statistical methods
Data were collected into Microsoft Excel™ and analyzed with Stata™ (College Station, TX, USA) software. Multilinear least squares regression was used to evaluate the independent variables of age, race, gender, BMI, CAD/CVD death, diabetes and treatment of hypertension on the dependent structural variables of Vglom, glomerulosclerosis, cortical fibrosis and arterial intimal thickening. Multilinear regression models were used to evaluate the interactions of Vglom, glomerulosclerosis, cortical fibrosis and arterial intimal thickening with race and MAP. To evaluate possible effects of influential outliers, least squares regressions were checked with robust regression models using Huber maximum likelihood and scaled estimators of high-leveraged outliers. Differences between groups were analyzed using a t-test if data passed normality and equal variance tests and by a Mann–Whitney rank sum test if they did not. Spearman's rank-order correlation evaluated pairwise relationships between variables. Discrete variables were compared by χ2-tests. For all statistical procedures, a P-value of <0.05 was considered significant.
RESULTS
Age relationships to hypertension and Vglom
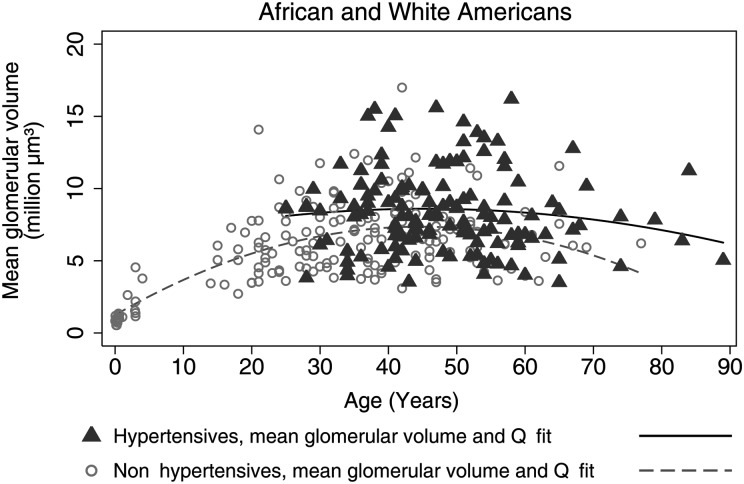
Medical Examiner investigations of sudden unexpected deaths accounted for 57% of the autopsies with 51% of these deaths being the result of CAD or CVD. The youngest hypertensive subject at death was 25 years of age. MAP reached hypertensive levels (≥107 mmHg) somewhat earlier and the level of blood pressure was higher (P = 0.02) for African Americans than whites. Vglom increased during childhood and adolescent growth. Adult size was reached at 18–20 years of age (Figure 1), and from early adulthood to old age the Vglom of hypertensive subjects was larger than those without hypertension (P < 0.001).
FIGURE 1:
The relationship between Vglom and age by quadratic prediction plots comparing hypertensive and non-hypertensive subjects. Vglom increases with growth during adolescence and early adulthood to plateau at ∼25 years of age. For hypertensive subjects, Vglom was larger than for non-hypertensive subjects from early adulthood through old age (P < 0.001).
Nglom ranged from 210 332 to 2 702 079 with an average of 918 210 ± 326 077. For all subjects, females had 10% fewer glomeruli than males with the gender difference being only significant for whites (African American males 941 903 ± 351 504, n = 86, African American females 877 169 ± 328 866, n = 94, P = 0.20; white males 986 338 ± 314 387, n = 87; white females 839 253 ± 294 790, n = 52, P = 0.01). Fewer glomeruli were found in kidneys with more glomerulosclerosis (r = −0.190, P < 0.01). This modest reduction in glomerular number was the result of the trend for lower Nglom to be found in kidneys of hypertensive subjects with increased glomerulosclerosis.
Different patterns of glomerulosclerosis and their relationship to ageing and blood pressure
From infancy to ∼3 years of age, up to 8% ‘congenital’ global glomerulosclerosis was found [23]. At the end of adolescence, glomerular obsolescence began to be observed. In the early stages, obsolescence was recognized by thickening and wrinkling of the glomerular capillary basement membranes and collapse of the tuft toward the hilar pole. In the late stages, the collapsed tuft became a brightly PAS-positive hyaline knot surrounded by intracapsular fibrosis that filled Bowman's space within a largely intact Bowman's capsule basement membrane [10, 11]. Occasional perihilar segmental glomerulosclerosis with hyalinosis was found in juxtamedullary glomeruli. These glomeruli were infrequently identified mainly in obese subjects who died of CAD/CVD but in numbers that were too few to enumerate meaningfully in the 400 or more glomeruli counted per subject.
Glomerular solidification was defined by the following features [10, 11]: (i) in the early stages by focal segmental glomerulosclerosis (FSGS) that consisted of segmental effacement of glomerular capillaries by increased mesangial matrix and by adhesions to Bowman's capsule. (ii) The later stages consisted of consolidated PAS-positive basement membranes and mesangial matrix surrounded by a fragmented Bowman's capsule basement membrane. This combination of FSGS and solidification was found in three subjects. All three had severe hypertension and severe intimal fibrosis of arcuate and interlobular arteries. One subject was a 36-year-old African American female with a MAP of 154 mmHg, 1 028 482 glomeruli and 1.25% glomerulosclerosis. One was a 57-year-old African American male with a MAP of 136 mmHg, 875 516 glomeruli and 11.8% glomerulosclerosis. The third was a 56-year-old white male with a MAP of 152 mmHg, 1 142 909 glomeruli and 27.8% glomerulosclerosis. In each case, global glomerulosclerosis consisted of ∼50% solidified and 50% obsolescent glomeruli.
Early in adulthood, the number of obsolete glomeruli, hereafter referred to as glomerulosclerosis, rarely exceeded 2–3%. At age 30–40, glomerulosclerosis began to increase. The rate of increase depended upon whether or not the subjects were hypertensive and, if hypertensive, on the magnitude of the elevation of blood pressure. For non-hypertensive subjects, glomerulosclerosis was related to age (P < 0.001) but without a significant contribution from MAP (P = 0.45). For hypertensive subjects, the percentage of glomerulosclerosis was related to age (P < 0.001) and MAP (P < 0.001).
Clinical and kidney structural features of hypertensive and non-hypertensive subjects 18–70 years old
The average age at death for all hypertensive subjects was 48.7 ± 12.2 with a range of 25–89 years. Fourteen of the 135 hypertensive subjects (10.4%) died with or were identified as having hypertension at or before age 30 (Table 1). The youngest of these 14 patients were 17, 19 and 20 years old. The oldest non-hypertensive person was 69 years old. In order to evaluate Nglom and Vglom in subjects of similar age, comparisons were made between hypertensive and non-hypertensive subjects between 18 and 70 years old. The clinical and pathological features of these subjects are summarized in Table 2.
Table 1.
Subjects dying with hypertension or being identified as hypertensive before age 30
| Race | Age at death (years) | Gender | BMI (kg/m2) | Nglom | MAP (mmHg) | Cause of death | Age (years) at diagnosis of hypertension |
|---|---|---|---|---|---|---|---|
| AA | 25 | Female | 33.1 | 993 299 | 115 | Postpartum cardiomyopathy | 23 |
| AA | 25 | Female | 50.0 | 1 066 778 | 109 | Pulmonary embolus | 25 |
| AA | 28 | Male | 41.2 | 1 163 809 | Myocardial infarct | 28 | |
| AA | 28 | Male | 26.1 | 1 332 604 | 112 | Rheumatic heart disease | 27 |
| AA | 29 | Female | 25.5 | 638 228 | Pulmonary embolus | 29 | |
| White | 30 | Male | 33.1 | 1 208 151 | 119 | Pulmonary embolus | 27 |
| AA | 39 | Female | 24.3 | 874 539 | 118 | Stroke | 25 |
| AA | 42 | Male | 43.0 | 1 162 345 | 113 | Myocardial infarct | 28 |
| AA | 42 | Female | 35.8 | 709 290 | 132 | Stroke | 17 |
| AA | 43 | Female | 22.1 | 917 875 | 115 | Myocardial infarct | 29 |
| AA | 43 | Male | 29.2 | 394 733 | Pulmonary embolus | 20 | |
| White | 44 | Female | 26.9 | 751 245 | 117 | Stroke | 28 |
| AA | 46 | Male | 26.9 | 1 012 409 | 120 | Myocardial infarct | 27 |
| White | 49 | Male | 30.5 | 939 893 | 119 | Myocardial infarct | 19 |
| 11AA, 3W | 7 male, 7 female | 32.0 ± 8.1 | 940 371 ± 252 942 | 117 ± 6 |
AA, African American; Nglom, number of glomeruli per kidney (right).
Table 2.
Clinical and kidney microanatomical features of the study cohort from 18 to 70 years old by race and hypertension status
| African American |
P | White |
P | P race | |||
|---|---|---|---|---|---|---|---|
| Hypertensive, n = 86 (58.5) | Non-hypertensive, n = 61 | Hypertensive, n = 44 (35.8) | Non-hypertensive, n = 79 | <0.001 | |||
| Age (years) | 46 (40.8–54) | 35 (26.5–42) | <0.001 | 49 (39–54.8) | 42 (31–52) | <0.01 | 0.52/0.001 |
| Men | 50 (58.1) | 27 (44.3) | 0.43 | 33 (75) | 43 (54.4) | 0.35 | 0.47/0.59 |
| BMI (kg/m2) | 31.2 ± 11.4 | 29.9 ± 7.0 | 0.41 | 31.8 ± 10.2 | 29.3 ± 7.9 | 0.13 | 0.78/0.67 |
| MAP (mmHg) | 119 (114–131) | 94 (91–98) | <0.001 | 113 (113–119) | 96 (92–99) | <0.001 | 0.02/0.39 |
| CAD or CVD death | 47 (54.7) | 13 (21.3) | 0.01 | 25 (56.8) | 15 (19.0) | <0.01 | 0.98/0.95 |
| Diabetes | 9 (10.5) | 0 | 0.01 | 1 (2.3) | 1 (1.3) | 0.7 | 0.23/0.89 |
| Treated hypertension | 42 (48.8) | – | 20 (45.5) | – | 0.96/– | ||
| Nglom: men | 953 558 ± 350 054 | 1 021 582 ± 326 581 | 0.41 | 946 339 ± 348 970 | 1 019 957 ± 319 696 | 0.34 | 0.93/0.98 |
| Nglom: women | 830 322 ± 234 445 | 920 912 ± 213 297 | 0.10 | 699 526 ± 184 651 | 922 265 ± 291 882 | 0.02 | 0.10/0.98 |
| Vglom (µm3 × 106): men | 8.18 (7.13–11.33) | 7.04 (5.92–8.28) | 0.01 | 7.45 (5.95–8.89) | 5.75 (4.55–7.73) | 0.01 | 0.04/0.04 |
| Vglom: women | 8.92 (5.95–10.05) | 5.92 (4.80–8.03) | 0.01 | 8.74 (6.57–9.88) | 6.12 (4.62–6.97) | 0.01 | 0.80/0.47 |
| Glomerulosclerosis (%) | 2.96 (1.29–6.85) | 0.96 (0.36–2.38) | <0.001 | 2.64 (1.60–4.74) | 1.03 (0.54–2.48) | <0.001 | 0.37/0.39 |
| Cortical fibrosis | 0.05 (0.02–0.11) | 0.02 (0–0.08) | <0.001 | 0.05 (0.03–0.08) | 0.02 (0.01–0.04) | <0.001 | 0.53/0.94 |
| Arterial intimal thickening | 0.11 (0.06–0.18) | 0.02 (0–0.08) | <0.001 | 0.08 (0.04–0.16) | 0.03 (0–0.06) | <0.001 | 0.10/0.66 |
Continuous values expressed as mean ± standard deviation if data are normally distributed, or median (25th–75th percentiles) for non-normally distributed data. Discrete values expressed as number (%).
P for race indicates probabilities of racial differences for hypertension/non-hypertension.
Significant differences are bolded.
BMI, body mass index; MAP, mean arterial pressure; CAD, coronary artery disease; CVD, cerebrovascular disease.
There were proportionately more hypertensive African Americans than whites (P < 0.001), and hypertensive African Americans had a greater MAP than hypertensive whites, P = 0.02. CAD/CVD accounted for 54.7% of deaths among African Americans and 56.8% of white deaths. Nine diabetic African Americans were all hypertensive and five died at a median of 52 years of age from CAD/CVD. One of two white diabetics was hypertensive and died at 37 from CAD/CVD. Proportionately similar numbers of subjects of both races were treated for hypertension. The indicated anti-hypertensive medications consisted of beta-blocking agents, angiotensin converting enzyme inhibitors, hydrochlorthiazide, calcium channel blockers and for one subject spironolactone.
Hypertensive African American males and females and white males had somewhat, but not significantly, fewer glomeruli than non-hypertensive subjects of the same gender. Eleven hypertensive white females, however, had significantly fewer glomeruli than 36 non-hypertensive white females (P = 0.02). Hypertensive subjects had larger glomeruli than their non-hypertensive counterparts among all race and gender groups, and African American males had significantly larger glomeruli than white males (P < 0.001 for all males, P = 0.04 for hypertensive males). There were no significant racial differences in the severity of glomerulosclerosis, cortical fibrosis and arteriosclerosis.
For 18- to 70-year-old subjects, a strong inverse correlation was seen between Vglom and Nglom, and strong direct correlations were found between Vglom, hypertension and BMI (Table 3). Pairwise relationships showed the severity of glomerulosclerosis, cortical fibrosis and arteriosclerosis to be strongly correlated with age and hypertension. Multivariate least squares and robust regressions were similar for the dependent structural variables of Vglom, glomerulosclerosis, cortical fibrosis and arterial intimal thickening when analyzed for the clinical variables of age, race, gender, BMI, hypertension, diabetes, CAD/CVD and hypertension treatment (Table 4). All structural variables were significantly associated with hypertension but not gender. African American race was significantly related to Vglom (P = 0.01) and arterial intimal thickening (0.01–0.001) by least squares and robust regression. Diabetes was significantly correlated with cortical fibrosis. The average Vglom (9.90 ± 3.72) and percent glomerulosclerosis (6.58 ± 6.14) of diabetics were greater than that of hypertensive non-diabetics (Vglom, 8.43 ± 2.70; percent glomerulosclerosis, 4.98 ± 6.09), but neither difference was significant with the small number of diabetics (Vglom, P = 0.11, percent glomerulosclerosis, P = 0.43). In multivariate least squares but not robust regression, diabetes was significantly related to Vglom. The treatment of hypertension was not linked to any of the dependent variables.
Table 3.
The study cohort aged 18–70
| BMI | Nglom | Vglom | GS | CF | It | HTN | |
|---|---|---|---|---|---|---|---|
| Age | 0.005 0.93 | −0.092 0.13 |
0.131 0.03 | 0.605 <0.001 | 0.431 <0.001 | 0.527 <0.001 | 0.348 <0.001 |
| BMI | 0.097 0.11 |
0.234 <0.001 | −0.095 0.11 | −0.069 0.25 | −0.030 0.61 | 0.050 0.41 | |
| Nglom | −0.383 <0.001 | −0.190 <0.01 | −0.144 0.02 | −0.091 0.13 | −0.132 0.03 | ||
| Vglom | 0.131 0.02 | 0.218 <0.01 | 0.190 <0.01 | 0.360 <0.001 | |||
| GS | 0.648 <0.001 | 0.558 <0.001 | 0.395 <0.001 | ||||
| CF | 0.538 <0.001 | 0.406 <0.001 | |||||
| It | 0.532 <0.001 |
Spearman rank-order pairwise correlation between age, BMI, Nglom, Vglom, hypertension and the structural features of hypertensive nephropathy.
Within the cells, the upper number is the Spearman correlation coefficient and the lower number is the P-value. For P < 0.05, there is a significant relationship between the two variables. Variables with significant relationships are indicated in bold.
BMI, body mass index; GS, glomerulosclerosis; CF, cortical fibrosis; It, arterial intimal thickening; HTN, hypertension.
Table 4.
The study cohort aged 18–70
| Least squares regression |
Robust regression |
|||
|---|---|---|---|---|
| Vglom (m3 × 106) | Vglom (m3 × 106) | |||
| Coefficient | P | Coefficient | P | |
| Age | 0.013 | 0.35 | 0.014 | 0.31 |
| Race | −0.841 | 0.01 | −0.841 | 0.01 |
| Gender | −0.449 | 0.16 | −0.273 | 0.39 |
| BMI | 0.067 | <0.001 | 0.063 | <0.001 |
| Hypertension | 1.114 | <0.01 | 1.303 | 0.001 |
| Diabetes | 1.920 | 0.02 | 0.990 | 0.21 |
| CAD/CVD | 0.229 | 0.51 | 0.308 | 0.37 |
| Treated hypertension | 0.207 | 0.63 | 0.012 | 0.98 |
| Glomerulosclerosis | Glomerulosclerosis | |||
| Age | 0.150 | <0.001 | 0.071 | <0.001 |
| Race | −1.493 | 0.01 | 0.266 | 0.17 |
| Gender | 0.224 | 0.68 | 0.234 | 0.22 |
| BMI | −0.047 | 0.10 | −0.015 | 0.13 |
| Hypertension | 1.920 | 0.01 | 0.604 | 0.01 |
| Diabetes | 0.777 | 0.57 | 1.973 | <0.001 |
| CAD/CVD | 0.365 | 0.62 | −0.256 | 0.22 |
| Treated hypertension | −1.066 | 0.15 | 0.003 | 0.99 |
| Cortical fibrosis | Cortical fibrosis | |||
| Age | 0.001 | <0.001 | 0.001 | <0.001 |
| Race | −0.014 | 0.03 | −0.006 | 0.16 |
| Gender | 0.005 | 0.44 | −0.002 | 0.64 |
| BMI | −0.001 | 0.06 | −0.0002 | 0.18 |
| Hypertension | 0.028 | <0.001 | 0.017 | 0.01 |
| Diabetes | 0.044 | <0.01 | 0.034 | 0.001 |
| CAD/CVD | −0.012 | 0.07 | −0.012 | 0.01 |
| Treated hypertension | −0.003 | 0.70 | 0.004 | 0.46 |
| Arterial intimal thickening | Arterial intimal thickening | |||
| Age | 0.002 | <0.001 | 0.002 | <0.001 |
| Race | −0.028 | 0.01 | −0.022 | 0.001 |
| Gender | −0.002 | 0.82 | −0.006 | 0.39 |
| BMI | −0.001 | 0.06 | −0.0003 | 0.36 |
| Hypertension | 0.062 | <0.001 | 0.040 | <0.001 |
| Diabetes | −0.037 | 0.08 | −0.019 | 0.26 |
| CAD/CVD | 0.018 | 0.15 | 0.013 | 0.08 |
| Treated hypertension | −0.027 | 0.31 | −0.007 | 0.44 |
Multivariate analysis by least squares and robust regression showing the relative contributions of the clinical factors of age, race, gender, BMI, hypertension, diabetes, CAD/CVD death, and treatment of hypertension to Vglom, glomerulosclerosis, cortical fibrosis and arterial intimal thickening.
Assigned scores: male = 1, female = 2; African American race = 1, white race = 2. Hypertension = 1, diabetes = 1, CAD/CVD = 1 and treated hypertension = 1 (all verses 0).
Significant relationships are bolded.
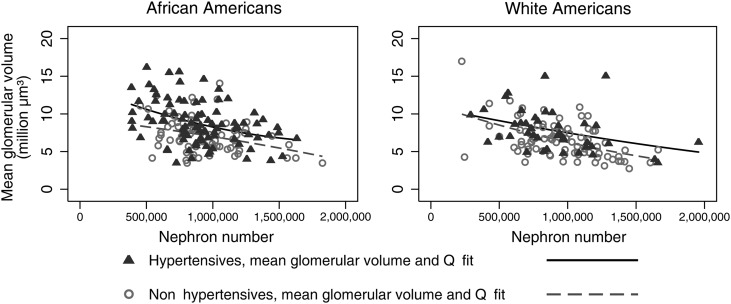
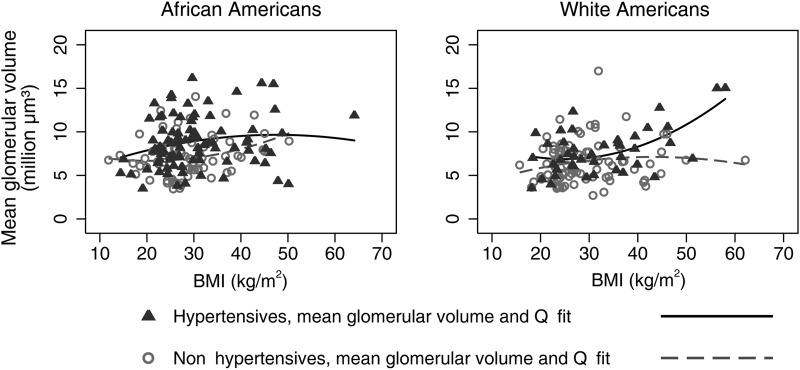
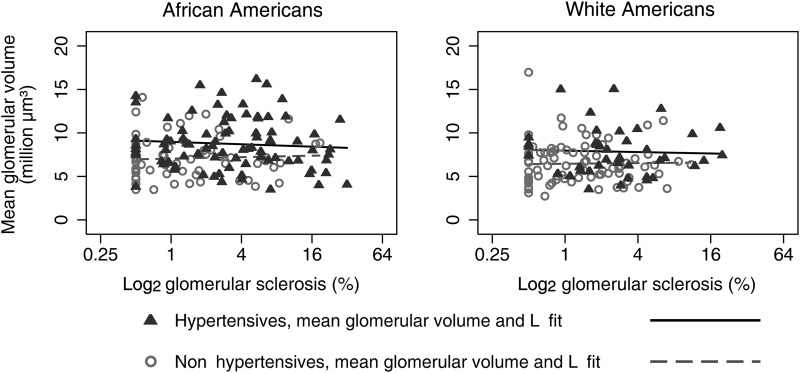
The increases in Vglom with hypertension were present for both African Americans and whites throughout the range of Nglom (Figure 2) and BMI (Figure 3). Figure 4 presents the relationships between Vglom and glomerulosclerosis and shows that, compared with non-hypertensives, the increased Vglom was found in hypertensive subjects with only mild glomerulosclerosis. With advanced glomerulosclerosis, there was a slight but not significant tendency toward convergence of Vglom between hypertensive and non-hypertensive subjects (African Americans non-hypertension, r = 0.105, P = 0.26; hypertension, r = −0.152, P = 0.23; whites non-hypertension, r = 0.089, P = 0.74; hypertension, r = −0.047, P = 0.94).
FIGURE 2:
Subjects 18–70 years old showing by quadratic prediction plots an inverse relationship between Vglom and Nglom for African Americans and whites in which the Vglom of hypertensive subjects are larger than that of non-hypertensive subjects throughout the range of Nglom. Multivariable robust regression (Vglom-dependent variable): African Americans, coefficient Nglom = −2.86e−06, P < 0.001, coefficient hypertension = 1.71, P < 0.001; whites, coefficient Nglom = −3.24e−06, P < 0.001, coefficient hypertension = 1.14, P = 0.01.
FIGURE 3:
Subjects 18–70 years old showing by quadratic prediction plots a direct relationship between Vglom and BMI for African Americans and whites in which the Vglom of hypertensive subjects are larger than that of non-hypertensive subjects throughout the range of BMI. Multivariable robust regression (Vglom-dependent variable): African Americans, coefficient BMI = 0.047, P = 0.04, coefficient hypertension = 1.78, P < 0.001; whites, coefficient BMI = 0.076, P = 0.001, coefficient hypertension = 1.55, P < 0.001.
FIGURE 4:
Subjects 18–70 years old demonstrating by linear regression the relationships between Vglom and log 2 of percent glomerulosclerosis among hypertensive and non-hypertensive subjects for African Americans and whites. The Vglom of hypertensive subjects was larger than that of non-hypertensive subjects (P < 0.001). The enlargement was present throughout the range of glomerulosclerosis with the difference being most pronounced with early, or mild, glomerulosclerosis. With more advanced glomerulosclerosis, there was a slight but not significant tendency toward the convergence of Vglom in both races (African Americans hypertension, r = −0.152, P = 0.23; non-hypertension, r = 0.105, P = 0.26); whites hypertension, r = −0.047, P = 0.94; non-hypertension, r = 0.089, P = 0.74).
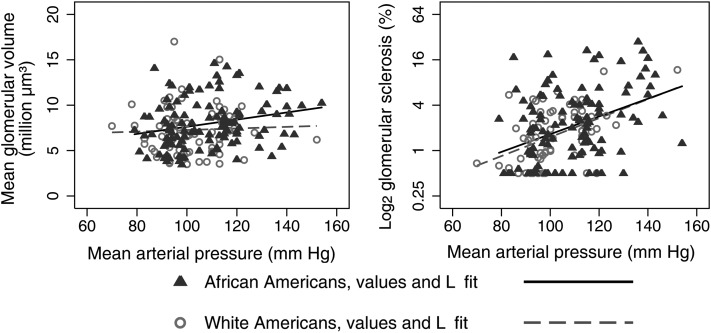
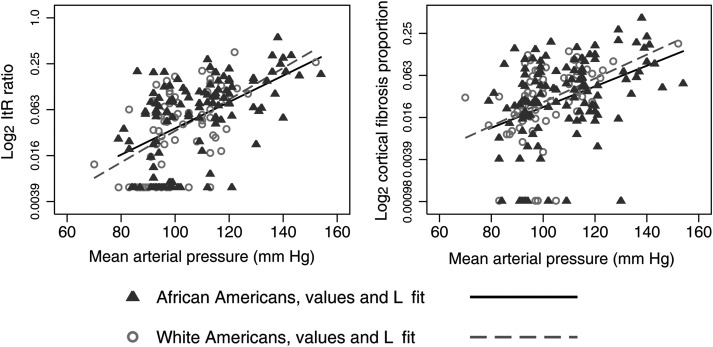
Effects of race and blood pressure on glomerulosclerosis, arteriosclerosis, cortical fibrosis and Vglom among subjects 18–70 years old
In models evaluating race and MAP, a strong direct correlation was found between MAP and arterial intimal thickening, cortical fibrosis and glomerulosclerosis for both races, and a significant increase in Vglom with increasing MAP was found for African Americans but not whites (Table 5). A 10 mmHg increase in MAP produced a 0.41 µm3 × 106 increase in Vglom for African Americans and a 0.21 µm3 × 106 increase for whites (Figure 5). Nevertheless, racial interactions with MAP were not significant for any of the variables including Vglom, and incremental increases in MAP produced nearly identical increases in glomerulosclerosis, cortical fibrosis and arterial intimal thickening in both races (Figures 5 and 6).
Table 5.
The study cohort aged 18–70
| MAP Coef (P) |
Interaction Coef (P) | Model r2 (P) | ||
|---|---|---|---|---|
| African American | White | |||
| Vglom (µm3 × 106) | 0.042 (<0.01) | 0.023 (0.43) | −0.635 (0.15) | 0.054 (<0.01) |
| Glomerulosclerosis | 0.126 (<0.001) | 0.088 (<0.001) | −0.914 (0.16) | 0.184 (0.01) |
| Cortical fibrosis | 0.001 (<0.001) | 0.002 (<0.001) | −0.005 (0.52) | 0.196 (<0.001) |
| Intimal thickening | 0.003 (<0.001) | 0.003 (<0.001) | −0.007 (0.54) | 0.341 (<0.001) |
Multivariate least squares regression showing the relationships of race, MAP and their interactions with the pathological features of hypertensive nephropathy.
Coefficients are presented for the non-interactive effects of MAP for Vglom, glomerulosclerosis (%), cortical fibrosis, and arterial intimal thickening and for the MAP race interactions. Model r2 is adjusted and reflects interactions.
MAP, mean arterial pressure (mmHg); Coef, coefficient; P, probability.
FIGURE 5:
Subjects 18–70 years old showing for African Americans and whites the linear relationships between MAP and Vglom and MAP and the log 2 of percent glomerulosclerosis. The Vglom of African Americans increased 0.41 μm3 × 106 for a 10 mmHg increase in MAP (P < 0.001) compared with 0.23 μm3 × 106 for whites (P = 0.43), the MAP-race interaction was not significant, P = 0.15. The relationship between the log 2 of percent glomerulosclerosis and MAP showed that for any level of MAP, glomerulosclerosis was similar in the two races, P = 0.16.
FIGURE 6:
Subjects 18–70 years old showing for African Americans and whites the linear relationships between MAP and the log 2 of arterial intimal thickening and MAP and the log 2 of the proportion of cortical fibrosis. For any level of MAP, arterial intimal thickening and the proportion of cortical fibrosis was nearly the same in the two races (interaction, P = 0.54 for arterial intimal thickening; P = 0.52 for cortical fibrosis).
DISCUSSION
The findings demonstrated that age and blood pressure were the principal factors linked to the severity of the microanatomical changes of the kidney that can be subsumed under the term hypertensive nephrosclerosis. The Vglom of African American males was larger than that of white males, and in multivariate analyses, African American race was significantly associated with increased arterial intimal thickening. The findings suggested a racial effect, but it appeared to be related to the proportionately greater number of hypertensive African Americans and their more severe hypertension. Additionally, we show that Vglom was increased with hypertension and BMI, findings that may correspond to data reported from imaging studies in which many patients with mild-to-moderate nephrosclerosis and metabolic factors contributing to chronic kidney disease have elevated GFR and single nephron filtration rates [7, 12, 15].
Glomerular solidification that has been associated with loss of preglomerular vascular resistance was seen in the kidneys of only three subjects in the study and, in these kidneys, occurred with severe arteriosclerotic intimal thickening and equal proportions of glomerular obsolescence. In the other kidneys, glomerular obsolescence was the nearly exclusive pattern of glomerular loss.
The infrequency of glomerular solidification in these autopsies contrasts with the high frequency reported in the AASK biopsies [9, 28]. The latter was a cross-sectional analysis of patients with mild-to-moderate renal insufficiency having average serum creatinine levels of 2.9 ± 0.7 mg/dL and GFR of 51.7 ± 13.6 mL/min/1.73 m2. Among these biopsies, there was an average of 42 ± 3% global glomerulosclerosis with African Americans having 50 ± 5%. This compares, in our autopsies, with an average 5.0 ± 6.1% glomerulosclerosis among hypertensive subjects who died of non-renal causes attributed in the majority of cases to CAD/CVD.
The kidneys in our autopsies were examples of mild-to-moderate nephrosclerosis with the three subjects noted above being severely hypertensive and having features of ‘decompensated nephrosclerosis’ [21]. The discerned patterns of glomerulosclerosis and their association with restrictive preglomerular vascular disease indicate that the progression of hypertensive nephropathy was similar in both races [3, 5, 6, 7]. Glomerular collapse associated with a restrictive afferent arteriolopathy rather than segmental glomerulosclerosis is the principal mode of glomerular injury in spontaneously hypertensive rats. This is a widely used experimental model of chronic hypertension in which glomerulosclerosis is attributed to reduced glomerular perfusion [29]. In our observational human studies, glomerular obsolescence with preglomerular arteriosclerosis closely resembled these animal studies.
In the current study, only white women demonstrated a significant relationship between elevated blood pressure and low glomerular number. This may indicate that low Nglom plays a role in the hypertension of white women, or it may be a false association related to the small number of 11 white hypertensive women in our sample. Low nephron number was not seen in individuals identified as being hypertensive or dying with hypertension before age 30 who might be anticipated to have a predisposing nephron deficit. The findings generally contradict the hypothesis of essential hypertension being related to low glomerular number proposed by Keller et al. [30].
Keller et al. [30] described two distinct groups of subjects in which 10 hypertensives had a range of 531 140–954 893 glomeruli and 10 non-hypertensives a range of 884 458–1 959 914 glomeruli. The centile distribution of Nglom for their hypertensive subjects is essentially the same that we have reported for hypertension among both African Americans and whites [19, 20]. But the median Nglom for their non-hypertensives is above the 75th percentile for our non-hypertensive subjects and for other reported distributions of glomerular number in the human kidney [18, 19, 20, 31]. They seem to have found a small group of subjects in which very high nephron number protected against hypertension [30]. In our autopsy sample, the mildly reduced number of glomeruli in hypertensive subjects is more compatible with a model in which lower Nglom is the result of glomerular loss owing to obsolescence.
The principal determinant of adult Vglom is an apparently innate inverse relationship to Nglom in which low glomerular number is associated with large glomerular volume [18, 24, 25, 30, 32]. BMI and hypertension are correlated with increased Vglom independently of each other and of Nglom [24, 25, 32]. In this regard, glomerular hypertrophy acts in a dependent manner to hypertension and as having developmental associations with glomerulosclerosis and arterial intimal thickening. The relationships suggest that the enlarged glomeruli may be susceptible to collapse and obsolescence when there is a reduction in glomerular blood flow [29].
Our methods and findings resemble those of Kasiske [33] in his analysis of atherosclerotic vascular disease and age-associated changes of the kidney in autopsies from the Hennepin County Medical Examiner's office. In pairwise regression, mean glomerular area, intrarenal arterial wall thickening and percent glomerulosclerosis were significantly correlated with age and hypertension; whereas in multivariate regression, glomerular area was related to atherosclerotic CAD but not glomerulosclerosis. This is similar to the associations that we find between glomerulosclerosis and glomerular volume in which increased Vglom correlated with hypertension. In neither study was glomerulosclerosis associated with a compensatory increase in glomerular size [33]. The treatment of hypertension was also evaluated in both studies with no effect on glomerular size being demonstrated [33]. Hypertension and CAD/CVD as well as treatment for hypertension are closely linked phenomena, and independent associations with any particular manifestation of hypertension-associated disease may be difficult to find; nonetheless, the absence of any relationship between glomerulosclerosis and average glomerular size brings into question whether a compensatory increase in Vglom actually occurs in kidneys with age-related glomerular loss.
The increased African American risk for non-diabetic kidney disease including FSGS and hypertension has a genetic component related to apolipoprotein L1 gene (APOL1) sequence variants. Among African Americans, subjects with one APOL1 risk allele are found to have an OR of 1.26 and those with two risk alleles an OR of 7.3 for hypertension-associated ESRD that has been related to a susceptibility for glomerulosclerosis [4, 34]. We are currently investigating the relationships between APOL1 risk alleles and the structural features of hypertensive nephropathy. The initial results show a strong linkage to hypertension but also suggest that APOL1 risk alleles may be associated with excessive glomerular enlargement [35].
In summary, we show that in the setting of mild-to-moderate nephrosclerosis, glomerular hypertrophy is a primary attribute of hypertensive nephropathy. We suggest that glomerular hypertrophy precedes the later glomerular collapse that leads to glomerular obsolescence through a mechanism that simultaneously promotes preglomerular arteriolosclerosis. Our choice of independent and dependent variables was based upon the current physiological concepts of essential hypertension being the result of abnormal pressure natriuresis or oxidative stress and the structural changes of nephrosclerosis, particularly the vasculopathies, being secondary to the elevation of blood pressure [5, 36, 37]. Many investigators in this field, however, have proposed that hypertension is secondary to age-related vascular changes [5, 6, 38]. The current and similar descriptive and observational studies are not designed to evaluate the causality of clinical and structural relationships, and the strength of the associations between blood pressure and nephrosclerosis make it difficult to separate any effect of race. It is anticipated that the continuing genetic studies may clarify a racial effect on glomerular and vascular structure and possibly a link to blood pressure [3].
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflicting interests and no financial disclosures. The results presented in this paper have not been published previously in whole or part, except in abstract format.
ACKNOWLEDGEMENTS
This research was funded by grants from the National Institutes of Health (NIH 1 RO1 DK065970-01), NIH Center of Excellence in Minority Health (5P20M000534-02), the National Medical Research Council of Australia, Janseen-Cilag Australia Pty Ltd and the American Heart Association (Southeastern Affiliate).
REFERENCES
- 1.Law CM, de Swiet M, Osmond C, et al. Initiation of hypertension in utero and its amplification throughout life. Br Med J. 1993;306:24–27. doi: 10.1136/bmj.306.6869.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fields LE, Burt VL, Cutler JA, et al. The burden of adult hypertension in the United States 1999 to 2000: a rising tide. Hypertension. 2004;44:398–404. doi: 10.1161/01.HYP.0000142248.54761.56. [DOI] [PubMed] [Google Scholar]
- 3.Murea M, Freedman BI. Essential hypertension and risk of nephropathy: a reappraisal. Curr Opin Nephrol Hypertens. 2010;19:235–241. doi: 10.1097/MNH.0b013e3283366344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freedman BI, Kopp JB, Langefeld CD, et al. The apolipoprotein L1 (APOL1) gene and nondiabetic nephropathy in African Americans. J Am Soc Nephrol. 2010;21:1422–1426. doi: 10.1681/ASN.2010070730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson RJ, Feig DI, Nakagawa T, et al. Pathogenesis of essential hypertension: historical paradigms and modern insights. J Hypertens. 2008;26:381–391. doi: 10.1097/HJH.0b013e3282f29876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tracy RE. Blood pressure related separately to parenchymal fibrosis and vasculopathy of the kidney. Am J Kidney Dis. 1992;20:124–131. doi: 10.1016/s0272-6386(12)80539-7. [DOI] [PubMed] [Google Scholar]
- 7.Glassock RJ, Rule AD. The implications of anatomical and functional changes of the ageing kidney: with emphasis on the glomeruli. Kidney Int. 2012;82:270–277. doi: 10.1038/ki.2012.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fogo A, Ichikawa I. Evidence for a pathogenetic link between glomerular hypertrophy and sclerosis. Am J Kidney Dis. 1991;17:666–669. doi: 10.1016/s0272-6386(12)80347-7. [DOI] [PubMed] [Google Scholar]
- 9.Marcantoni C, Ma LJ, Federspeil C, et al. Hypertensive nephrosclerosis in African Americans versus Caucasians. Kidney Int. 2002;62:172–180. doi: 10.1046/j.1523-1755.2002.00420.x. [DOI] [PubMed] [Google Scholar]
- 10.Marcantoni C, Fogo AB. Perspectives on arterionephrosclerosis: from pathology to potential pathogenesis. J Nephrol. 2007;20:518–524. [PubMed] [Google Scholar]
- 11.Hughson MD. Hypertension and Vascular Diseases of Kidney, Chapter 12. In: Silva FG, D'Agati VD, Nadasdy T, Laszik Z, Zhou XJ, editors. Silva's Diagnostic Renal Pathology. New York: Marc Strauss; 2009. pp. 436–464. [Google Scholar]
- 12.Rule AD, Cornell LD, Poggio ED. Senile nephrosclerosis. Does it explain the decline in glomerular filtration with ageing? Nephron Physiol. 2011;119:6–11. doi: 10.1159/000328012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hill GS. Hypertensive nephrosclerosis. Curr Opinions Nephrol Hypertens. 2008;17:266–270. doi: 10.1097/MNH.0b013e3282f88a1f. [DOI] [PubMed] [Google Scholar]
- 14.Hill GS, Heudes D, Bariety J. Morphometric study of arterioles and glomeruli in the aging kidney suggests focal loss of autoregulation. Kidney Int. 2003;63:1027–1036. doi: 10.1046/j.1523-1755.2003.00831.x. [DOI] [PubMed] [Google Scholar]
- 15.Rule AD, Semret MH, Amer H, et al. Associations of kidney function and metabolic risk factors with density of glomeruli on renal biopsy samples from living donors. Mayo Clin Proc. 2011;86:282–290. doi: 10.4065/mcp.2010.0821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brenner BM, Chertow GM. Congenital oligonephropathy and the etiology of adult hypertension and progressive renal injury. Am J Kidney Dis. 1994;23:171–175. [PubMed] [Google Scholar]
- 17.Esposito C, He C-J, Striker GE, et al. Nature and severity of the glomerular response to nephron reduction in strain-dependent mice. Am J Pathol. 1999;154:891–897. doi: 10.1016/S0002-9440(10)65336-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hughson MD, Farris AB, Douglas-Denton R, et al. Glomerular number and size in autopsy kidneys: the relationship to birth weight. Kidney Int. 2003;63:2113–2122. doi: 10.1046/j.1523-1755.2003.00018.x. [DOI] [PubMed] [Google Scholar]
- 19.Hughson MD, Douglas-Denton R, Bertram JF, et al. Hypertension, glomerular number, and birth weight in African Americans and Whites in the Southeastern United States. Kidney Int. 2006;69:671–678. doi: 10.1038/sj.ki.5000041. [DOI] [PubMed] [Google Scholar]
- 20.Hughson MD, Gobe G, Douglas-Denton RN, et al. Associations of glomerular number and birth weight with clinicopathological features of African Americans and whites. Am J Kidney Dis. 2008;52:18–28. doi: 10.1053/j.ajkd.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 21.Bohle A, Ratschek M. The compensated and decompensated forms of nephrosclerosis. Pathol Res Pract. 1982;174:357–367. doi: 10.1016/S0344-0338(82)80017-4. [DOI] [PubMed] [Google Scholar]
- 22.Pesce CM, Schmidt K, Fogo A, et al. Glomerular size and the incidence of renal disease in African Americans and Caucasians. J Nephrol. 1994;7:355–358. [Google Scholar]
- 23.Abdi R, Slakey D, Kittur D, et al. Heterogeniety of glomerular size in normal donor kidneys. Impact of race. Am J Kidney Dis. 1998;32:43–46. doi: 10.1053/ajkd.1998.v32.pm9669422. [DOI] [PubMed] [Google Scholar]
- 24.Hughson MD, Hoy WE, Douglas-Denton RN, et al. Towards a definition of glomerulomegaly: clinical-pathological and methodological considerations. Nephrol Dial Transplant. 2010;26:2202–2208. doi: 10.1093/ndt/gfq688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Samuel T, Hoy WE, Douglas-Denton R, et al. Determinants of glomerular volume in different cortical zones of the human kidney. J Am Soc Nephrol. 2005;16:3102–3109. doi: 10.1681/ASN.2005010123. [DOI] [PubMed] [Google Scholar]
- 26.Hoy WE, Hughson MD, Zimanyi M, et al. Nephron number, birth weight and body mass index. Clin Nephrol. 2010;74(S1):105–112. doi: 10.5414/cnp74s105. [DOI] [PubMed] [Google Scholar]
- 27.Bertram JF. Analyzing renal glomeruli with the new stereology. Int Rev Cytol. 1995;161:111–172. doi: 10.1016/s0074-7696(08)62497-3. [DOI] [PubMed] [Google Scholar]
- 28.Fogo A, Breyer JA, Smith MC, et al. Accuracy of the diagnosis of hypertensive nephrosclerosis in African Americans: a report from the African American Study of Kidney Disease (AASK) Trail. AASK Pilot Study Investigators. Kidney Int. 1997;15:244–252. doi: 10.1038/ki.1997.29. [DOI] [PubMed] [Google Scholar]
- 29.Leh S, Hultsrom M, Rosenberger C, et al. Afferent arteriolopathy and glomerular collapse but not segmental sclerosis induce tubular atrophy in old spontaneously hypertensive rats. Virchows Arch. 2011;459:99–108. doi: 10.1007/s00428-011-1100-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keller G, Zimmer G, Mall G, et al. Nephron number in patients with primary hypertension. N Engl J Med. 2003;348:101–108. doi: 10.1056/NEJMoa020549. [DOI] [PubMed] [Google Scholar]
- 31.Nyengaard JR, Bendtsten TF. Glomerular number and size in relation to age, kidney weight, and body surface in normal man. Anat Rec. 1992;232:194–201. doi: 10.1002/ar.1092320205. [DOI] [PubMed] [Google Scholar]
- 32.Puelles VG, Zimanyi MA, Samuel T, et al. Estimating individual glomerular volume in the human kidney: clinical perspectives. Nephrol Dial Transplant. 2011;27:1880–1888. doi: 10.1093/ndt/gfr539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kasiske BL. Relationship between vascular disease and age-associated changes in the human kidney. Kidney Int. 1987;31:1153–1159. doi: 10.1038/ki.1987.122. [DOI] [PubMed] [Google Scholar]
- 34.Genovese G, Friedman DJ, Ross MD, et al. Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science. 2010;329:841–845. doi: 10.1126/science.1193032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hoy WE, Hughson MD, Winkler CA, et al. Interaction between APOL1 genotype and body mass index correlate with glomerular volume and number: insights into the African American predisposition to chronic kidney disease (abstract) J Am Soc Nephrol. 2012;23:77A. [Google Scholar]
- 36.Hall JE, Mizelle HL, Hildebrandt DA, et al. Abbnormal pressure natriuresis, a cause or consequence of hypertension? Hypertension. 1990;15:547–549. doi: 10.1161/01.hyp.15.6.547. [DOI] [PubMed] [Google Scholar]
- 37.Cowley AW. Renal medullary oxidative stress, pressure natriuresis, and hypertension. Hypertension. 2008;52:777–786. doi: 10.1161/HYPERTENSIONAHA.107.092858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tracy RE. Renovasculopathies of hypertension and the rise of blood pressure with age in blacks and whites. Semin Nephrol. 1996;16:126–133. [PubMed] [Google Scholar]