Capnocytophaga species are facultative anaerobic, capnophilic, fusiform, gram-negative bacilli exhibiting gliding motility; they are normal inhabitants of the oropharyngeal flora [1]. In addition, they are opportunistic pathogens associated with periodontal diseases and animal bites, causing systemic infection in both immunocompetent and immunocompromised hosts [2, 3]. To date, 9 species have been described in the genus Capnocytophaga, including C. canimorsus, C. cynodegmi, C. ochracea, C. gingivalis, C. sputigena, C. haemolytica, C. granulosa, C. lead-betteri, and genospecies AHN8471 [4]. Infections caused by Capnocytophaga species are infrequent, and species-level biochemical identification is difficult; thus, case reports of C. sputigena infection are rare [5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15]. We report a case of C. sputigena bacteremia in a patient with a hematologic malignancy.
A 40-yr-old man was admitted to our hospital for allogeneic bone marrow transplantation (BMT). After receiving a reduced-intensity conditioning regimen with fludarabine and busulfan, stem cells were infused into the patient. One hour later, his body temperature had risen to 39.2℃ After each 2 sets of blood cultures were taken from the peripheral veins and a central venous catheter, empirical antibiotic therapy with intravenous piperacillin-tazobactam was administered. Four years earlier, the patient had diagnosed as having symptomatic CLL. The following year, he received autologous peripheral blood stem cell transplantation and maintained remission, but CLL relapsed 6 months before admission.
Physical examination revealed no definitive focus of infection; the patient had a flat abdomen, clear breath sounds, and mild hyperemia of the oral mucosa. His blood pressure was 148/90 mmHg, pulse was 80/min, and respiratory rate was 20 breaths/min. Hematological tests showed the followings: Hb, 10.2 g/dL; leukocyte count, 0.05×109/L; platelet count, 37×109/L; C-reactive protein level, 6.41 mg/dL; blood urea nitrogen (BUN)/creatinine levels, 13/0.85 mg/dL; and total protein/albumin levels, 5.1/3.4 g/dL.
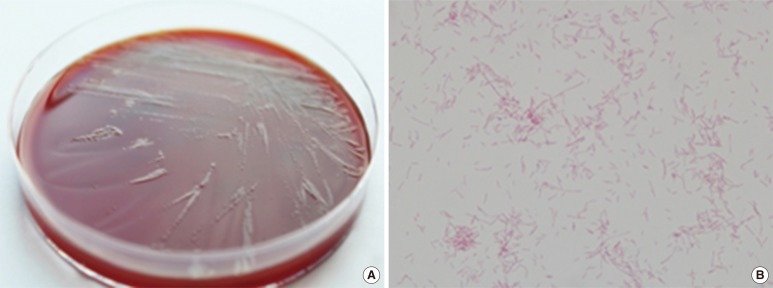
Two anaerobic blood cultures from the peripheral vein were positive after 3 days of incubation. The broths of positive cultures were inoculated onto blood agar plates (BAPs) and MacConkey agar plates (MACs), and incubated for 48 hr at 35℃ in 5% CO2. Gray-colored non-hemolytic colonies grew on BAPs (Fig. 1A), whereas no colonies grew on MACs. Smear preparations of colonies that grew on BAPs showed oxidase- and catalase-negative isolates and spindle-shaped gram-negative bacilli (Fig. 1B). By using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS; Bruker Daltonik GmbH, Bremen, Germany) and Vitek2 HN system (bioMérieux, Marcy l'Etoile, France), the organism was identified as C. sputigena with a Bruker score of 2.039 and a 99% probability of being a Capnocytophaga species.
Fig. 1.
Colonial and microscopic findings of Capnocytophaga sputigena. (A) Gray-colored non-hemolytic colonies on a blood agar plate after 48 hr of incubation at 35℃ with 5% CO2. (B) Thin, spindle-shaped, gram-negative bacilli from smear preparations of the blood agar plate (Gram stain, ×1,000).
To confirm the identity of the isolate, we conducted 16S rRNA gene sequencing using the MicroSeq 500 system (Applied Biosystems, Foster City, CA, USA) with PCR and sequencing kits designed with universal primers to cover all bacteria. Sequences were analyzed by using an ABI PRISM 3730 Series DNA Analyzer (Applied Biosystems). The first 500 bp of the 16S rRNA gene sequence of the isolate showed 99.6% identity with the GenBank sequence AF133536 (C. sputigena) and 93.6% identity with NR_07450 (C. ochracea).
Antimicrobial susceptibility was tested by using the E-test (AB Biodisk, Solna, Sweden) on BAPs incubated for 48 hr at 35℃ in 5% CO2, and the results were interpreted by using Clinical and Laboratory Standards Institute breakpoints for HACEK group infections [16]. The isolate was susceptible to ampicillin, ampicillin-sulbactam, cefotaxime, ceftriaxone, chloramphenicol, clarithromycin, imipenem, meropenem, and tetracycline, but resistant to ciprofloxacin, levofloxacin, and trimethoprim-sulfamethoxazole.
Treatment with intravenous piperacillin-tazobactam was maintained, and follow-up blood cultures from the peripheral veins and a central venous catheter on days 3 and 10 were negative. The patient was successfully treated with a 12-day course of intravenous piperacillin-tazobactam, and the BMT was successful as determined by bone marrow examination 20 days after stem cell infusion.
Although Capnocytophaga species are oropharyngeal microbiota, they are rare opportunistic pathogens, especially in patients with hematologic malignancy after high-dose chemotherapy [1, 2, 3]. Among different species, C. sputigena has been involved in abscesses, bacteremia, chorioamnionitis, empyema, endocarditis, osteomyelitis, pleuropneumonitis, sinusitis, and septic abortion [5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15]. Only 2 studies of Capnocytophaga infection, including bacteremia, periodontitis, and osteomyelitis, have been reported in Korea, but none of the cases identified the species of the causative organism [17]. To the best of our knowledge, this is the first report of C. sputigena bacteremia confirmed by 16S rRNA gene analysis in Korea.
Because conventional biochemical methods identify the genus level of Capnocytophaga species rather than the species level, the 16S rRNA gene analysis has been used for identification of C. sputigena [10, 11, 12, 13]. By using MALDI-TOF MS, however, a fast and accurate identification of C. sputigena is now possible [14, 18]. There have been no reports on clinical differences based on distinct Capnocytophaga species and the necessity for species-level identification. If more laboratories use MALDI-TOF MS and publish reports on Capnocytophaga species, it is likely that this information will be forthcoming.
In the present case, since symptoms occurred immediately after the stem cell infusion, the stored stem cells may have been contaminated with the pathogen. However, C. sputigena is known to be present in normal oral flora, but there have been no reports showing their presence on the skin. Therefore, we assume that the oral cavity flora is the more likely source of infection, although the patient had no symptoms of oral mucositis.
Multidrug-resistant Capnocytophaga species, which present with a pattern of resistance to β-lactams and ciprofloxacin have been previously reported [19, 20]; however, the present isolate was susceptible to β-lactams but resistant to ciprofloxacin. Although there is no consensus guideline for the treatment of Capnocytophaga infections, the antibiotics to which Capnocytophaga species are already known to be susceptible, such as clindamycin, imipenem/cilastatin, and β-lactamase inhibitors, are appropriate choices for patient management [3].
In conclusion, we report the first Korean case of C. sputigena bacteremia confirmed by 16S rRNA gene analysis and MALDI-TOF MS. The present findings indicate that C. sputigena is an opportunistic pathogen in humans, especially in immunocompromised patients, such as those with hematologic malignancies.
Footnotes
No potential conflicts of interest relevant to this article were reported.
References
- 1.Ooshima T, Nishiyama N, Hou B, Tamura K, Amano A, Kusumoto A, et al. Occurrence of periodontal bacteria in healthy children: a 2-year longitudinal study. Community Dent Oral Epidemiol. 2003;31:417–425. doi: 10.1046/j.1600-0528.2003.00112.x. [DOI] [PubMed] [Google Scholar]
- 2.Bonatti H, Rossboth DW, Nachbaur D, Fille M, Aspock C, Hend I, et al. A series of infections due to Capnocytophaga spp. in immunosuppressed and immunocompetent patients. Clin Microbiol Infect. 2003;9:380–387. doi: 10.1046/j.1469-0691.2003.00538.x. [DOI] [PubMed] [Google Scholar]
- 3.Jolivet-Gougeon A, Sixou JL, Tamanai-Shacoori Z, Bonnaure-Mallet M. Antimicrobial treatment of Capnocytophaga infections. Int J Antimicrob Agents. 2007;29:367–373. doi: 10.1016/j.ijantimicag.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Zbinden R, von Graevenitz A. Actinobacillus, Capnocytophaga, Eikenella, Kingella, Pasteurella, and other fastidious or rarely encountered gram-negative rods. In: Versalovic J, Carroll KC, Funke G, Jorgensen JH, Landry ML, Warnock DW, editors. Manual of clinical microbiology. 10th ed. Washington, DC: ASM Press; 2011. pp. 574–587. in press. [Google Scholar]
- 5.Imamura T, Miura T, Nakamura I, Kunihiro M. A case of septicemia due to Capnocytophaga sputigena. Kansenshogaku Zasshi. 1987;61:713–718. doi: 10.11150/kansenshogakuzasshi1970.61.713. [DOI] [PubMed] [Google Scholar]
- 6.Douvier S, Neuwirth C, Filipuzzi L, Kisterman JP. Chorioamnionitis with intact membranes caused by Capnocytophaga sputigena. Eur J Obstet Gynecol Reprod Biol. 1999;83:109–112. doi: 10.1016/s0301-2115(98)00240-1. [DOI] [PubMed] [Google Scholar]
- 7.García-Cía JI, Esteban J, Santos-O'Connor F, Román A, Soriano F. Mixed bacteremia with Capnocytophaga sputigena and Escherichia coli following bone marrow transplantation: case report and review. Eur J Clin Microbiol Infect Dis. 2004;23:139–141. doi: 10.1007/s10096-003-1063-7. [DOI] [PubMed] [Google Scholar]
- 8.Funada H, Machi T, Yoneyama H, Matsuda T, Miura H, Ezaki T, et al. Capnocytophaga sputigena bacteremia associated with acute leukemia. Kansenshogaku Zasshi. 1993;67:622–628. doi: 10.11150/kansenshogakuzasshi1970.67.622. [DOI] [PubMed] [Google Scholar]
- 9.Torrús D, González JA, Boix V, Portilla J. Aortic endocarditis due to Capnocytophaga sputigena . Med Clin (Barc) 1995;105:119. [PubMed] [Google Scholar]
- 10.Alanen A, Laurikainen E. Second-trimester abortion caused by Capnocytophaga sputigena: case report. Am J Perinatol. 1999;16:181–183. doi: 10.1055/s-2007-993854. [DOI] [PubMed] [Google Scholar]
- 11.Vandemeulebrouck B, Rasigade JP, Sobas C, Vialet A, Roubille M. Septicaemia with Capnocytophaga sputigena in a newborn child. Ann Biol Clin (Paris) 2008;66:215–219. doi: 10.1684/abc.2008.0212. [DOI] [PubMed] [Google Scholar]
- 12.Atmani S, Wanin S, Bellon G, Reix P. Capnocytophaga sputigena pleuropneumonitis: a case report. Arch Pediatr. 2008;15:1535–1537. doi: 10.1016/j.arcped.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 13.Chan JF, Wong SS, Leung SS, Li IW, To KK, Cheng VC, et al. Capnocytophaga sputigena primary iliopsoas abscess. J Med Microbiol. 2010;59:1368–1370. doi: 10.1099/jmm.0.022905-0. [DOI] [PubMed] [Google Scholar]
- 14.Li A, Tambyah P, Chan D, Leong KK. Capnocytophaga sputigena empyema. J Clin Microbiol. 2013;51:2772–2774. doi: 10.1128/JCM.00884-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.García Lozano T, Lorente Alegre P, Linares Latorre MD, Aznar Oroval E. Fatal bacteremia related to Capnocytophaga sputigena in a hematological patient with type T non-Hodgkin lymphoma. Diagnosis by 16S rRNA gene sequencing. Rev Argent Microbiol. 2012;44:170–172. [PubMed] [Google Scholar]
- 16.Clinical and Laboratory Standards Institute. Methods for antimicrobial dilution and disk susceptibility testing of infrequently isolated or fastidious bacteria. M45-A2. Wayne, PA: Clinical and Laboratory Standards Institute; 2010. [DOI] [PubMed] [Google Scholar]
- 17.Roh KH, Yong D, Cho DH, Woo K, Lee K, Chong Y. Three cases of bacteremia by Capnocytophaga spp. Korean J Clin Pathol. 2001;21:490–494. [Google Scholar]
- 18.Fedorko DP, Drake SK, Stock F, Murray PR. Identification of clinical isolates of anaerobic bacteria using matrix-assisted laser desorption ionization-time of flight mass spectrometry. Eur J Clin Microbiol Infect Dis. 2012;31:2257–2262. doi: 10.1007/s10096-012-1563-4. [DOI] [PubMed] [Google Scholar]
- 19.Gomez-Garces JL, Alos JI, Sanchez J, Cogollos R. Bacteremia by multidrug-resistant Capnocytophaga sputigena. J Clin Microbiol. 1994;32:1067–1069. doi: 10.1128/jcm.32.4.1067-1069.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang HK, Chen YC, Teng LJ, Hung CC, Chen ML, Du SH, et al. Brain abscess associated with multidrug-resistant Capnocytophaga ochracea infection. J Clin Microbiol. 2007;45:645–647. doi: 10.1128/JCM.01815-06. [DOI] [PMC free article] [PubMed] [Google Scholar]