Abstract
Objective
To explore the association between baseline life-space mobility and nursing home (NH) admission among community-dwelling older adults over six years.
Methods
Using data from a prospective, observational cohort study consisting of a random sample of 1000 Medicare beneficiaries ≥ 65 years of age stratified by race (African American and non-Hispanic White), sex, and rural/urban residence. Baseline life-space mobility was assessed during in-home interviews. Participants were contacted by telephone every six months to ascertain NH admissions, Life-Space Assessment (LSA) scores and vital status (living or deceased). Using multivariate logistic regression, the significance and independence of the relationship of life-space mobility with NH admission was examined.
Results
Over six years, the odds of NH admission increased 2% for every one point lower baseline life-space score independent of previously recognized risk factors.
Discussion
The LSA may be a useful tool to identify older adults at risk for NH admission.
Keywords: Geriatric Assessment, Risk Factors, Nursing Homes
Introduction
The cost of nursing home (NH) care is projected to be $164.5 billion in the United States by 2014 (Centers for Medicare and Medicaid Services Office of the Actuary, 2011). Studies have shown that NH admission has been associated with variable quality of care and early mortality for many residents as well as psychological or emotional upheaval for caregiving families (Gaugler, Yu Krichbaum, & Wyman, 2009). In an attempt to avoid these outcomes, characteristics of NH residents and risk factors for NH admission have been extensively studied over the past two decades, particularly in specific populations such as persons with dementia (Andel, Hyer & Slack, 2007;McCann et al., 2005; Yaffe et al., 2002) or among recently hospitalized older adults (Rudberg, Sager & Zhang, 1996). Common predictive risk factors include older age, cognitive impairment, difficulty with basic and instrumental activities of daily living (ADL and IADL), lack of social support, prior NH use, and functional disability (Akamigbo & Wolinsky, 2006, 2007; Andel et al., 2007; Bharucha, Panday, Shen, Hiroko, & Ganguli, 2005; Gaugler, Duval, Anderson & Kane, 2009; Luppa et al., 2010; McCann et al., 2005; Rudberg et al., 1996; Smith, Kokmen & O'Brien, 2000; Yaffe et al., 2002).
Unfortunately, while valuable, recognition of these known risk factors may not serve as a trigger for intervention or the identification may come too late to delay the older adult's transition to NH care. Other tools to identify community-dwelling older adults at risk for subsequent NH admission prior to profound loss of ADL or IADL ability have the potential to allow the initiation of interventions to delay NH admission.
The assessment of life-space mobility may provide such a method of early identification. The University of Alabama at Birmingham (UAB) Life-Space Assessment (LSA) is a validated tool that measures community mobility based on the distance through which a person reports moving during the four weeks preceding the assessment (Allman, Sawyer & Roseman, 2006; Baker, Bodner, & Allman, 2003; Parker, Baker & Allman 2001; Peel et al., 2005). The LSA provides a single measure that incorporates where and how often a person goes to specific areas ranging from the home to outside one's town with any use of equipment or personal assistance. This measure has been used to assess mobility and changes in mobility among community-dwelling older adults with different disease profiles, levels of disability, environmental and social resources (Allman et al., 2006; Peel et al., 2005). Life-Space may reflect, in part, underlying disability as conceptualized in the literature (; Freedman et al., 2011; LaPlante, 2010) since maintenance of life-space requires carrying out multiple mobility-related activities such as transferring, walking, driving or using public transportation. Moreover, life-space also reflects disability in the domain of participation in society to the degree to which movement within one's environment is required to be involved in social activities (Brown et al., 2009). According to the 2005 Institute of Medicine (IOM) Workshop on Disability in America, the maintenance of social participation is perhaps the most important functional outcome for individuals, families, and society and is closely related to quality of life. The IOM report suggested that social participation may be more amenable to interventions than difficulties with specific activities (Sawyer & Allman 2010; Whiteneck, 2006). Peel et al. (2005) showed that 3 variables measuring specific mobility-related tasks and physical abilities (Activities of Daily Living (ADL), Instrumental Activities of Daily Living (IADL), and Short Physical Performance Battery (SPPB) explained only 45.5% of the variability in LSA scores. In fact, over 60% of their study sample had no ADL difficulty at baseline but demonstrated variation in life-space scores. Variability in life-space scores among those with no ADL difficulty demonstrated the ability of the life-space measure to capture elements of social participation not recognized using traditional measures of function. The LSA can identify changes in community mobility that often precede ADL or IADL difficulty and could potentially serve as a warning sign for future NH placement, if the underlying cause for the LSA decline were addressed.
Thus, we sought to determine if life-space mobility, as measured by the Life-Space Assessment, would independently predict NH admission among a cohort of community-dwelling older adults over a subsequent six-year period.
Methods
Setting and participants
Data for these analyses are from the UAB Study of Aging, which was designed to understand subject-specific factors predisposing older adults to mobility decline and racial differences in mobility changes associated with aging. Study of Aging participants were recruited from a random sample of Medicare beneficiaries aged 65 years or older, living in central Alabama, stratified by county, race (African American or non-Hispanic White) and sex, with recruitment set to achieve a balanced sample in terms of race, sex, and rural/urban residence. Persons unable to answer questions on the telephone or living in NHs at the beginning of the UAB Study of Aging were ineligible for recruitment. Additionally, if potential participants were unable to answer the initial 14 sociodemographic questions without assistance, they were not enrolled. Once enrolled, participants provided contact information for two persons who would know their health status if the participant were not able to be contacted at subsequent follow-up interviews. Trained interviewers conducted baseline in-home interviews between November 1999 and February 2001. Telephone follow-up interviews to assess NH admission and vital status were conducted at six-month intervals. If participants were not able to answer questions on the telephone follow-up, vital status was determined from their provided contact. Potential participants for the present study included participants in the UAB Study of Aging who had known vital status and had completed at least one six-month follow-up telephone interview during six years of follow-up. A more detailed description of the recruitment and study design for this cohort of 1000 community-dwelling older adults has been published elsewhere (Allman et al., 2006; Baker et al., 2003). The UAB Institutional Review Board approved the study protocol.
Study variables
Life-Space Assessment (LSA)
The LSA measures community mobility during the four weeks preceding the assessment by asking about movement to specific life-space levels ranging from within one's dwelling to beyond one's town (Allman et al., 2006; Baker et al., 2003; Parker et al.,2001; Peel et al., 2005). Frequency of movement and use of assistance, either from equipment or another person, were assessed. Specifically, participants were asked: “During the past 4 weeks, have you: 1) been to other rooms in your home besides the room where you sleep; 2) been to an area outside your home such as your porch, deck or patio, hallway of an apartment building, or garage; 3) been to places in your neighborhood other than your own yard or apartment building; 4) been to places outside your neighborhood, but within your town; and 5) been to places outside your town?”
For each life-space level, participants were asked how many days within the week they attained that level and whether they needed help from assistive devices or another person to move to that level. On average, completion of the LSA requires less than 5 minutes. A composite score was calculated based on life-space level, degree of independence in achieving each level, and the frequency of attaining each level. Life-Space composite scores ranged from 0 to 120 with higher scores representing greater community mobility. Based on our previous work, scores exhibit a pattern of normal distribution, and scores of 60 and higher corresponded to an “unrestricted life-space,” indicating that persons achieving these LSA scores generally moved independently beyond walking distance of their home or into their neighborhood (Sawyer & Allman, 2010). The LSA test-retest reliability between face-to-face and telephone interviews completed within two weeks of each other showed an intraclass correlation coefficient of 0.96 (95% confidence interval 0.95, 0.97) (Baker et al., 2003). For descriptive purposes, we show the distribution of life-space scores by quartiles: 0-29 (quartile 1); 30-59 (quartile 2); 60-89 (quartile 3); and 90 and higher (quartile 4).
NH admissions and vital status
For the current study telephone follow-up interviews were completed every six months for up to six years. During each six-month follow-up telephone interview, participants or a contact person identified by the participant at baseline were asked if the participant had been admitted to a NH during the previous six months. If there was a positive response to the question during any follow-up telephone calls, the participants were defined as having had a NH admission. Nursing home admission was defined by any report of a NH admission, regardless of type, during the follow-up period of study. If a participant or proxy was unavailable at the time of follow-up, the interview was coded as missing. If vital status was undetermined at the time of the six-year follow-up, the participant status was defined as unknown. Reported deaths were confirmed using the Social Security Death Index. Length of available follow-up was defined as the number of interview periods prior to a NH admission, death, or the last available interview, whichever occurred first. Type of nursing home admission (post-acute versus long-term or custodial) was not recorded during the data collection.
Sociodemographic variables
Age, sex, race, and marital status were self-reported at baseline.
Socioeconomic variable
Self-reported income was recorded at baseline and included nine categories ranging from less than $5,000 annually to more than $50,000 annually (Williams et al., 2007). In previous work (Peel et al., 2005; Williams et al., 2007), the income levels ≥$8,000 corresponded to income that ranged from “just enough to get by on” ($8,000 to $11,999) to “allows you to do more or less what you want” ($30,000 to $39,999) (Williams et al., 2007, p. 318). For this analysis, we dichotomized income levels as income < $8,000 or income ≥ $8,000.
Comorbidity count
A comorbidity count assigned one point for each disease category of the Charlson Comorbidity Index without consideration of severity (Charlson, Pompei, Ales & MacKenzie, 1987). Self-reported diseases were verified by review of prescription medications, physician or clinic questionnaires, or by report of the disease on hospital discharge summary.
Depression
The 15 item Geriatric Depression Scale (GDS) Short Form was used to assess depressive symptoms. A cut-off score of ≥ six was used to indicate a positive screen for depression (Sheikh and Yesavage, 1986).
Cognition
The Mini Mental State Exam (MMSE), a multi-item cognitive assessment based on orientation to time and place of residence, immediate and short term memory, attention, and language use ranged from 0-30 with higher scores representing greater cognition. (Folstein, Folstein & McHugh, 1975).
Activities of daily living (ADL)
ADL were measured by self-report and included eating, toileting, dressing, transferring, and bathing (Kovar & Lawton, 1994). The tasks selected for the ADL scales were those used in a major national survey of older adults (Dawson, Hendershot, & Fulton, 1987). For each item, participants were asked: “Do you have any difficulty performing the task?” If participants answered “no,” a score of 0 was assigned. If participants answered “yes” or reported that they were unable to perform a task, a score of 1 was assigned. Scores ranged from 0 (no difficulty) to 5 (difficulty with all ADLs).
Statistical analysis
Descriptive characteristics of the study participants were calculated by obtaining frequencies, proportions, means, standard deviations, and medians. Chi-square tests were performed for categorical variables and t-tests were performed for continuous variables to test for significant differences between groups. Potential risk factors for NH admission were identified based on literature review and included age, sex, race, cognition, income, ADL/IADL difficulty, and marital status. The relationship between the study variables and NH admission status was examined in bivariate analyses. The significance and independence of the relationship of life-space mobility with subsequent NH admission was explored in a multivariate logistic regression model (Agresti 2002). The model adjusted for the following covariates: age, sex, race, urban/rural status, marital status, income ≥ $8,000, comorbidity count, MMSE score, depression, ADL, baseline LSA score, and length of follow-up (time to first NH admission, time to death, or last contact) available for study participants. Life-space was used as a continuous variable in the regression model to demonstrate the independent association of life-space and nursing home admission across the full continuum of mobility.
The Statistical Package for the Social Sciences version 21 (SPSS Chicago IL) was used for statistical analyses.
Results
Figure 1 shows the participant flow diagram for the current study. For these analyses, 998 participants had at least one telephone interview over six years of follow-up. Length of follow-up ranged from six months to six years for these participants. Mean follow-up for those admitted to a NH was 4.5 years in contrast to 4.8 years for those not admitted (p value=0.162). At 72 months, there were 2 participants in the nursing home and 88 participants in the community with unknown vital status. Among the group with known vital status at 72 months there were a total of 303 confirmed deaths. For those admitted to the nursing home, the mortality rate was 55.6% (35/63) compared to 31.7% (268/845) among those without a NH admission (p<.001).
Figure 1. Participant Flow Diagram.
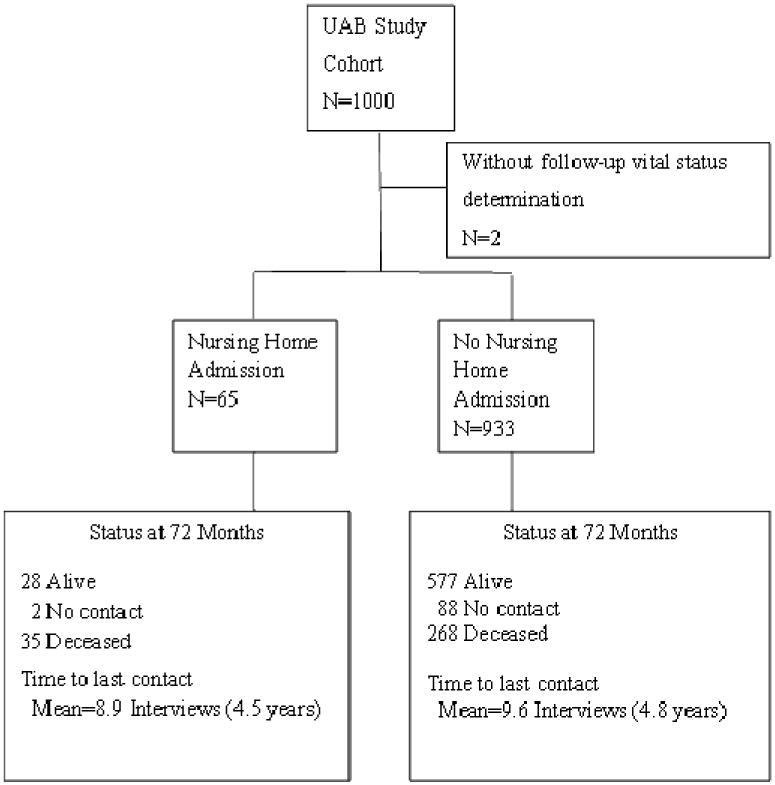
Table 1 shows the baseline characteristics of study participants by NH status, including the proportion in each of the four life-space categories to provide a description of the distribution of participants along the life-space continuum. Participants admitted to the NH were older, had higher depressive symptoms and comorbidity counts, were from a rural county, had more baseline difficulty with ADL, and had lower cognition scores, self-reported income and LSA scores when compared to those who did not have a NH admission. The 65 participants admitted to the NH were more likely to be female and less likely to be African American, although this did not reach statistical significance.
Table 1. Baseline Characteristics of Participants With and Without a Nursing Home Admission Over 6 Years.
| Baseline Characteristics | NH Admission | No NH Admission | P value |
|---|---|---|---|
| N= 65 | N=933 | ||
| Mean Age (SD) | 79.6 (7.0) | 75.0 (6.6) | <0.001 |
| Female, n (%) | 37 (56.9) | 461 (49.4) | 0.241 |
| African American, n (%) | 27 (41.5) | 472 (50.6) | 0.158 |
| Rural residence, n (%) | 42 (64.6) | 472 (50.6) | 0.029 |
| Married, n (%) | 15 (23.1) | 496 (53.2) | <0.001 |
| Income greater than $8,000, n (%) | 42 (64.6) | 721 (77.4) | 0.019 |
| Mean comorbidity count, n (SD) | 2.9 (1.6) | 2.2 (1.6) | 0.001 |
| Mean cognition score, n (SD) | 23 (5.7) | 25.1 (4.7) | 0.001 |
| Mean GDS, n (SD) | 3.6 (3.1) | 2.3 (2.2) | <0.001 |
| Mean ADL score, n (SD) | 1.25 (1.3) | 0.77 (1.2) | 0.003 |
| Mean LSA score, n (SD) | 47.3 (22.8) | 65.2 (24.6) | <0.001 |
| Life-Space score 0-29, n (%) | 12 (18.5) | 81 (8.7) | |
| Life-Space score 30-59, n (%) | 37 (56.9) | 283 (30.3) | |
| Life-Space score 60-89, n (%) | 11 (16.9) | 376 (40.3) | |
| Life-Space score >90, n (%) | 5 (7.7) | 193 (20.7) | <0.001 |
Note. NH: Nursing Home; GDS: Geriatric Depression Scale; ADL: Activities of Daily Living; LSA: Life-Space Assessment. Bolding indicates significant difference between groups. Chi-square tests were performed for categorical variables and t-tests were performed for continuous variables.
Forty-nine of 413 (11.9%) participants with restricted life-space at baseline (scores < 60) were admitted to a nursing home during the six years of follow-up; in contrast, only 16/585 (2.7%) with higher life-space scores experienced a nursing home admission (p<0.001). Results of the regression model demonstrate that the association between LSA scores and nursing home admission are independent of other known predictors (Table 2). Other factors that were independently associated with NH admission included being White and unmarried. Although the number of African Americans who had nursing home admissions (N=27; 41%) was fewer than Whites (N=35; 58.5%), the percentage of African Americans admitted to a nursing home (5.4%) was not significantly different from the percent of Whites (7.6%) in bivariate analyses. Likewise, the proportion of females (7.4%) admitted to nursing homes was not significantly different from that of males (5.6%) in bivariate analyses. However, after adjusting for time to last contact, time to death or 1st NH admission, and income, the logistic regression showed that the odds of a NH admission for African Americans were 34% lower than Whites (p=.002).
Table 2. Multivariate Logistic Regression of Potential Risk Factors for Nursing Home Admissiona,b.
| Risk Factor | Odds Ratio | P value | 95% CI |
|---|---|---|---|
| Agec | 1.037 | 0.089 | 0.994-1.081 |
| Female | 0.796 | 0.479 | 0.424-1.496 |
| African American | 0.343 | 0.002 | 0.175-0.674 |
| Rural residence | 1.716 | 0.074 | 0.949-3.104 |
| Married | 0.296 | 0.001 | 0.146-0.599 |
| Comorbidity Count | 1.119 | 0.187 | 0.947-1.324 |
| MMSE | 0.987 | 0.682 | 0.928-1.050 |
| GDS | 1.102 | 0.092 | 0.984-1.233 |
| ADL | 0.797 | 0.061 | 0.628-1.011 |
| Baseline LSA Score | 0.976 | 0.002 | 0.960-0.991 |
Note. CI: Confidence Interval; GDS: Geriatric Depression Scale; ADL: Activities of Daily Living; LSA: Life-Space Assessment.
Analyses were restricted to participants without missing values.
Adjusted for time to last contact, time to death or 1st NH admission, income greater than $8,000.
Age was continuous per year.
Although the average time to follow-up or NH admission was similar, death was a competing risk factor for those with lower life-space scores. We controlled for this competing risk in the model by adjusting for length of follow-up.
A subanalysis of participants without ADL difficulty (N=604) was examined. Baseline LSA scores remained an independent predictor of NH admission even after adjusting for the factors listed in Table 2 (p=0.018) (data not shown).
Discussion
Over six years of follow-up, restricted life-space (scores < 60) were associated with 4.4 times greater risk of being admitted to a nursing home than observed for those unrestricted life-space (11.9% vs. 2.7%; p<0.001). The association between nursing home admission and life-space remained significant and independent after adjusting for other factors previously reported to be associated with NH admissions including ADL difficulty. The odds of NH admission increased 2% for every one point lower baseline life-space score among community-dwelling older adults. This finding suggests that the LSA may be a useful tool to identify community-dwelling older adults at risk for NH admission prior to significant loss of ADL ability.
The rate of nursing home admissions in this cohort was low relative to other studies, which may have been due to the age and baseline health status of the study sample. This study included participants aged 65 years and older with a mean age of 75 years. Nationally, only 2% of those aged 65-74 years are nursing home residents, this prevalence rises to 14% among those aged 85 years and older (Federal Interagency Forum on Aging-Related Statistics, 2012). Locally, we estimated that 1.5% of Alabama residents aged 65-74 live in a nursing home and the prevalence increased to 16.6% for Alabama residents aged 85 or older (Baker & Allman, 2004). In this study there were 65 participants admitted to NHs over six years, a prevalence of approximately 1% per year.
Similar to previous studies, we found that being African American or married was associated with a lower frequency of NH admission (Akamigbo & Wolinsky, 2006 2007; Gaugler, Yu et al., 2009). However, unlike previous studies using similar cohorts, we did not find age to be a predictive factor. In a model in which age was examined as a categorical variable, it remained nonsignificant. We also did not find cognitive impairment or ADL difficulty to be significant predictors of NH admission (Bharucha et al., 2005).
There are several potential reasons for these differences in findings. Although participants with cognitive impairment were not excluded from our study, potential participants had to be capable of communicating on the telephone to make arrangements for the in-home assessment and answer the initial 14 sociodemographic questions without assistance. Thus, over the six years of follow-up, the number of participants who might be expected to develop significant dementia might be smaller than that seen in other studies that included individuals with known dementia at baseline. Because our cohort was community-dwelling at baseline, ADL limitations also may have been less prevalent than is usually seen among patients admitted to the NH.
Previous authors have commented on an inability to identify older adults who experience functional decline at an early enough time for successful interventions to prevent or delay NH admission (Bharucha et al., 2005; Gaugler, Yu et al., 2007; Luppa et al., 2010; Rudberg et al., 1996). The LSA permits identification of clinically important changes in function reflecting changes in mobility and social participation. These changes frequently precede the development of ADL difficulties. Thus, using the LSA to assess community mobility may identify community-dwelling older adults at risk for NH admissions at a time when interventions may be implemented to prevent the development of functional decline requiring nursing home admission.
Previous studies (Allman et al., 2006; Peel et al., 2005) have shown the LSA to be reliable and easily administered in clinical and home settings as well as by telephone, with the questionnaire taking an average of five minutes to complete. The LSA reflects not only traditional measures of physical function and performance, but also sociodemographic and neuropsychological factors. Among community-dwelling older adults the LSA may be an appropriate instrument to determine baseline mobility levels and to follow changes that occur over time and with interventions. Knowledge of a patient's LSA score alone would not delay the need for NH admission, but recognition of a decline over time, specifically when the LSA score dropped lower than 60, could prompt the clinician to refer the older adult for further assessment.
A major strength of this study included having a racially balanced population-based sample of community-dwelling older adults who were prospectively followed for six years. Potential limitations included the use of self- or personal contact-report at six month intervals to determine NH admission. Because data was collected every six months, we may have missed admissions to the NH, particularly among persons who died during an interval. The type of NH admission, either long-term (custodial) or post-acute was unknown; however a retrospective review revealed that approximately 9 of the 75 participants admitted to the NH returned home, suggesting few post-acute admissions. The NH admission rate in this study is slightly lower than that seen in the general Alabama population (1% per year compared to 1.5% per year) and may reflect a bias in initial recruitment of those less likely to be admitted to a NH. We recognize that we have a relatively large number of control variables and we note this as a limitation.
This study has shown that a baseline Life-Space Assessment score independently predicted NH admission over the course of six years of follow-up in a cohort of community-dwelling older adults, even after controlling for previously recognized risk factors such as ADL difficulty. Decline in life-space scores, particularly at higher levels, occurs prior to ADL decline, and may identify an at-risk population for nursing home admission. Although not yet studied, the LSA may have the potential to target high risk individuals in future trials attempting to delay NH admissions. In particular, persons with LSA scores <60 should be targeted in studies to evaluate the impact of standard physical and occupational therapy interventions on functional status, mobility, and the transition of older adults from independent community living to long term care.
Supplementary Material
Contributor Information
Kendra D. Sheppard, University of Alabama at Birmingham.
Patricia Sawyer, University of Alabama at Birmingham.
Christine S. Ritchie, University of California San Francisco, Jewish Home San Francisco Center for Research on Aging.
Richard M. Allman, Birmingham/Atlanta VA Geriatric Research, Education and Clinical Center, University of Alabama at Birmingham.
Cynthia J. Brown, Birmingham/Atlanta VA Geriatric Research, Education and Clinical Center University of Alabama at Birmingham.
References
- Agresti A. Categorical data analysis. 2nd. New York: Wiley-Interscience; 2002. [Google Scholar]
- Akamigbo AB, Wolinsky FD. Reported expectations for nursing home placement among older adults and their role as risk factors for nursing home admissions. Gerontologist. 2006;46(4):464–473. doi: 10.1093/geront/46.4.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akamigbo AB, Wolinsky FD. New evidence of racial differences in access and their effects on the use of nursing homes among older adults. Med Care. 2007;45:672–679. doi: 10.1097/MLR.0b013e3180455677. [DOI] [PubMed] [Google Scholar]
- Allman RM, Sawyer P, Roseman JM. The UAB Study of Aging: background and insights into life-space mobility among older Americans in rural and urban settings. Aging Health. 2006;2:417–429. [Google Scholar]
- Andel R, Hyer K, Slack A. Risk factors for nursing home placement in older adults with and without dementia. J Aging Health. 2007;19(2):213–28. doi: 10.1177/0898264307299359. [DOI] [PubMed] [Google Scholar]
- Baker PS, Allman RM. Charting the course: State of Alabama long-term care needs assessment. 2004 Retrieved September 2012 from http://www.aging.uab.edu/subchannel/research/pdf/charting the course.pdf.
- Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc. 2003;51(11):1610–1614. doi: 10.1046/j.1532-5415.2003.51512.x. [DOI] [PubMed] [Google Scholar]
- Bharucha AJ, Pandav R, Shen C, Hiroko HD, Ganguli M. Predictors of nursing facility admission: A 12-Year epidemiological study in the United States. J Am Geriatr Soc. 2005;52:434–439. doi: 10.1111/j.1532-5415.2004.52118.x. [DOI] [PubMed] [Google Scholar]
- Brown CJ, Roth DL, Allman RM, Sawyer P, Ritchie CS, Roseman JM. Trajectories of life-space mobility after hospitalization. Ann Intern Med. 2009;150:372–378. doi: 10.7326/0003-4819-150-6-200903170-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services (CMS) Office of the Actuary. National Health Expenditure Projections 2010-2030. [Accessed March 1, 2013];2011 Available https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/proj2010.pdf.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Dawson O, Hendershot G, Fulton J. Advance Data, Vital and Health Statistics. Vol. 133. Hyattsville, MD: US Public Health Service; 1987. National Center for Health Statistics: Functional Limitations of Individuals Age 65 Years and Over. [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key Indicators of Well-Being. Retrieved September 2012 from http://www.agingstats.gov.
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Freedman VF, Kasper JD, Cornman JC, Agree EM, Bandeen-Roche K, Mor V, et al. Wolf DA. Validation of new measures of disability and functioning in the National Health and Aging Trends Study. J Gerontol A Biol Sci Med Sci. 2011;66A(9):1013–1021. doi: 10.1093/gerona/glr087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, Duval S, Anderson KA, Kane RL. Predicting nursing home admission in the U.S: A meta-analysis. BMC Geriatr. 2009;7:13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovar MG, Lawton MP. Functional disability: Activities and instrumental activities of daily living. In: Lawton R, Teresi J, editors. Focus on assessment techniques Ann Rev Gerontol Geriatr. Vol. 14. 1994. pp. 57–75. [Google Scholar]
- LaPlante MP. The classic measure of disability in activities of daily living is biased by age but an expanded iadl/adl measure is not. Journal of Gerontology: Social Sciences. 2010;65B(6):720–732. doi: 10.1093/geronb/gbp129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luppa M, Luck T, Weyerer S, Konig HH, Brahler E, Riedel-Heller SG. Prediction of institutionalization in the elderly. A systematic review. Age Ageing. 2010;39(1):31–38. doi: 10.1093/ageing/afp202. [DOI] [PubMed] [Google Scholar]
- McCann JJ, Hebert LE, Li Y, Wolinsky FD, Gilley DW, Agarwal NT, et al. Evans DA. The effect of adult day care services on time to nursing home placement in older adults with Alzheimer's disease. Gerontologist. 2005;45(6):754–63. doi: 10.1093/geront/45.6.754. [DOI] [PubMed] [Google Scholar]
- Parker M, Baker PS, Allman RM. A life-space approach to functional assessment of mobility in the elderly. J Gerontol Soc Work. 2001;35:35–55. [Google Scholar]
- Peel C, Sawyer PB, Roth DL, Brown CJ, Bodner EV, Allman RM. Assessing mobility in older adults: The UAB study of aging life-space assessment. Phys Ther. 2005;85(10):1008–1019. [PubMed] [Google Scholar]
- Rudberg MA, Sager MA, Zhang J. Risk factors for nursing home use after hospitalization for medical illness. J Gerontol A Biol Sci Med Sci. 1996;51(5):M189–M194. doi: 10.1093/gerona/51a.5.m189. [DOI] [PubMed] [Google Scholar]
- Sawyer P, Allman RM. Resilience in mobility in the context of chronic disease and aging: Cross-sectional and prospective findings from the UAB Study of Aging. In: Fry PS, Keyes CLM, editors. New frontiers of resilient aging, life strengths and wellness in late life. New York: Cambridge University Press; 2010. pp. 310–339. [Google Scholar]
- Sheikh JI, Yesavage JA. Geriatric Depression Scales (GDS): recent evidence and development of a shorter version. Clinical Gerontologist. 1986;5:165–173. [Google Scholar]
- Smith GE, Kokmen E, O'Brien PC. Risk factors for nursing home placement in a population-based dementia cohort. J Am Geriatr Soc. 2000;48(5):519–25. doi: 10.1111/j.1532-5415.2000.tb04998.x. [DOI] [PubMed] [Google Scholar]
- Whiteneck G. Conceptual models of disability: Past, present, and future. In: Field MJ, Jette AM, Martin L, editors. Workshop on disability in America: A new look—summary and background papers. Washington DC: National Academies Press; 2006. [Google Scholar]
- Williams BR, Baker PS, Allman RM, Roseman JM. Bereavement among African American and White older adults. J Aging Health. 2007;19:313–333. doi: 10.1177/0898264307299301. [DOI] [PubMed] [Google Scholar]
- Yaffe K, Fox P, Newcomer R, Sands L, Lindquist K, Dane K, Covinsky KE. Patient and caregiver characteristics and nursing home placement in patients with dementia. JAMA. 2002;287(16):2090–7. doi: 10.1001/jama.287.16.2090. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


