Abstract
Background
Ischemic Heart Disease (IHD) was the leading cause of disease burden worldwide in 2010. The majority of IHD burden affected middle income regions. We hypothesized that IHD burden may vary among countries, even within the same broad geographic region.
Methods
Disability-adjusted life years (DALYs) due to IHD were estimated at the region level for seven “super-regions”, 21 regions, and 187 countries using geographically nested models for IHD mortality and prevalent non-fatal IHD(nonfatal acute myocardial infarction, angina pectoris, or ischemic heart failure). Acute myocardial infarction, angina, and heart failure disability weights were applied to prevalent cases. Absolute numbers of DALYs and age-standardized DALYs per 100,000 persons were estimated for each region and country in 1990 and 2010. IHD burden for world regions was analyzed by country, income, and age.
Results
About two-thirds of 2010 IHD DALYs affected middle income countries. In the North Africa/Middle East and South Asia regions—regions with high IHD burden—more than 29% of males and 24% of females struck by IHD were <50 years old. Age-standardized IHD DALYs decreased in most countries between 1990 and 2010, but increased in a number of countries in the Eastern Europe/Central Asia region (>1,000 per 100,000 increase) and South Asia region (>175 per 100,000). Age-standardized DALYs varied by up to eight fold among countries, by about 9,000 per 100,000 among middle income countries, about 7,400 among low income countries, and about 4,300 among high income countries.
Conclusions
The majority of IHD burden in 2010 impacted middle income regions, where younger adults were more likely to develop IHD in regions like South Asia and North Africa/Middle East. However, IHD burden varied substantially by country within regions, especially among middle income countries. A global or regional approach to IHD prevention will not be sufficient; research and policy should focus on the highest burden countries within regions.
Keywords: ischemic heart disease, national income, mortality, burden of disease, global health
Introduction
Ischemic heart disease is the leading cause of death in the world, and a major cause of disability due to nonfatal acute myocardial infarction (AMI), angina pectoris, or ischemic heart failure.1, 2 One purpose of the 2011 United Nations High Level Meeting on Non-communicable Diseases was to expand the mandate of global public health to encompass chronic, non-communicable diseases like IHD, and deliver the message that non-communicable diseases like IHD are no longer solely diseases of the high income world. However, these simple messages are based on evidence aggregated at the regional and global levels, and may belie important differences between countries within the same broad region or income category. In practical terms, country-level data have the most potential to inform tailored, population-specific disease control efforts by national governments and local health systems. Current and future population age structures are important considerations for individual countries’ IHD prevention and treatment strategies.
The Global Burden of Diseases, Injuries and Risk Factors 2010 Study (GBD 2010 Study) found that the global burden of disease due to chronic, non-communicable diseases and their risk factors increased substantially since 1990, in large part because of a growing and aging world population.1 IHD burden also increased in absolute magnitude, despite overall decrease in age-standardized rates of fatal IHD, angina, and nonfatal AMI, and only a small increase in age-standardized ischemic heart failure prevalence.2 For the first time, the GBD 2010 Study estimated disease burden at the level of individual countries. In this report, we extend our previous findings on global and regional trends in IHD mortality and disease burden to the country level, and explore variability in IHD burden by age, country, and national income.
Methods
Detailed GBD 2010 Study IHD burden estimation methods are available elsewhere.2–4 The core summary measurement of population health in the GBD 2010 Study was disability-adjusted life years (DALYs) in the years 1990 and 2010. DALYs represent the “health gap” between a population’s actual health and an ideal standard. DALYs are composed of years of life lost (YLL) to premature deaths and years lived with non-fatal disease disability (YLD).1 IHD deaths fall into two categories: acute myocardial infarction (AMI) deaths and sudden cardiac deaths. IHD has been consistently defined as an underlying cause of death across International Classification of Diseases (ICD) revisions (most recently ICD-10 I20-I25, ICD-9 410-414).5 A proportion of IHD deaths are erroneously assigned on death certificates to either nonfatal ICD conditions (e.g., “senility”) or conditions not defined as an underlying cause of death (for example, heart failure, hypertension, or cardiac conduction disorders). The GBD developed methods for systematically re-allocating these undefined or erroneously assigned deaths to IHD based on the total distribution of actual causes of death by the country, sex, age, and year.5, 6 For mortality and YLL estimates, the GBD 2010 Study assembled a global cause-of-death data base. Mortality data were mapped to GBD cause categories and distribution of deaths to IHD and other causes and regional mortality and temporal trends were estimated using the cause of death ensemble modeling (CODEm) approach.7 The cause of death correct (CoDCorrect) algorithm estimated total cardiovascular diseases as a proportion of all deaths, after which IHD deaths were fit into the total cardiovascular disease mortality envelope.
Non-fatal IHD prevalence and incidence (for nonfatal AMI, angina, and ischemic heart failure) were estimated from data gathered in systematic reviews of epidemiologic data using a Bayesian meta-regression method (DisMod-MR).2, 8 Disability from each case of AMI, angina, heart failure, and other diseases or injuries was estimated in a household survey of lay people in Bangladesh, Indonesia, Peru, Tanzania, and the U.S.A., and an international web-based survey of health professionals.9 Distribution of disability severity (mild, moderate, or severe) was based on either studies using a disease specific severity scale [Canadian Cardiovascular Society (CCS) classification for angina10 or distribution of Short Form 15 quality of life scores among heart failure patients in the U.S. Medical Expenditure Panel Survey. Because heart failure is not defined as an underlying cause of death in the ICD classification system, separate methods were developed in order to distribute heart failure deaths to IHD and other upstream causes of heart failure.11
The GBD dealt with the problem of absent or low quality epidemiologic data in some countries and regions by 1) incorporating covariates (national or regional levels of CVD risk factor exposures, national income, study-level differences in measurement method) and “borrowing strength” from nearby regions and years of observation in CODEm and DisMod-MR models, and 2) using standard assumptions about the relationship between disease-specific incidence, prevalence, case fatality, and mortality in DisMod-MR models.1, 8, 11 Both CODEm and DisMod-MR employed mixed effects, hierarchical models. Country-level fixed effects included IHD risk factors (mean cholesterol, blood pressure, alcohol consumption, diet, physical activity, income per capita, health system access, and levels of smoking and diabetes in CODEm mortality models) or age-standardized IHD mortality rate (in DISMOD-MR nonfatal models), and study-level fixed effects included study type, and measurement method (whether AMI studies used troponin biomarker, or whether angina was diagnosed using the Rose questionnaire or a physician’s diagnosis, or whether heart failure was defined according to New York Heart Association class, Framingham Heart Study criteria, or ICD discharge code). Random effects by region and country reflected the geographical design of the study (country within region, region within country), and allowed global model estimates to vary locally based on country-level data.
One thousand draws were taken of the posterior distributions of CODEm and DISMOD-MR covariate effects (beta coefficients). Ninety-five percent uncertainty intervals reported in the paper are data within the 2.5 and 97.5 percentiles of these posterior distributions. These covariate values were entered into 1,000 iterations of the estimation models. In this manner, uncertainty surrounding covariate effects was propagated forward into DALY estimates as Bayesian credible intervals.
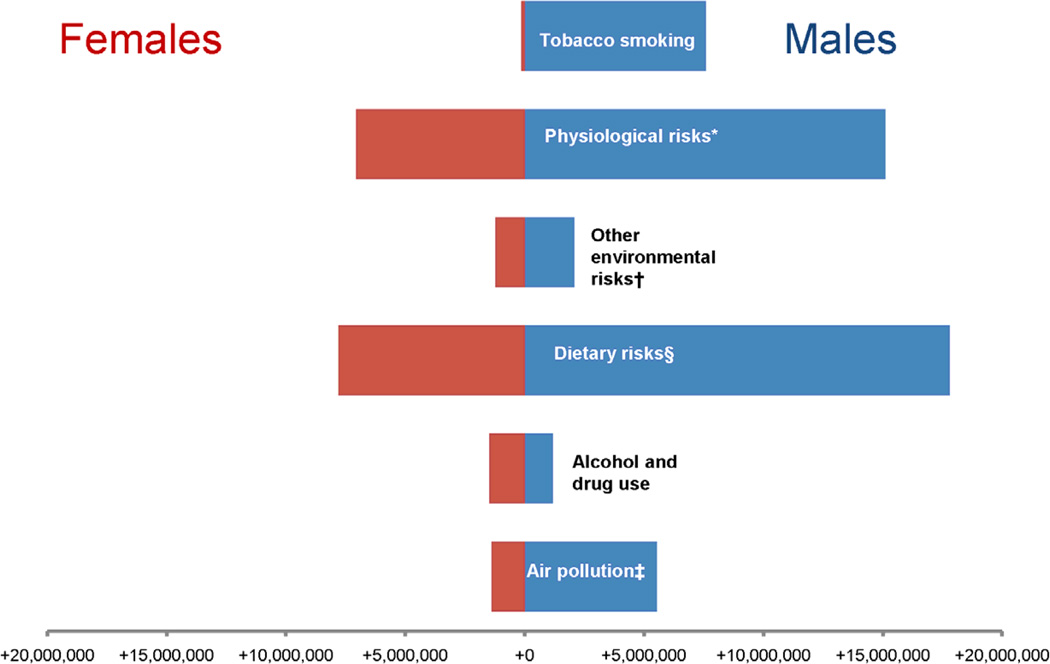
The Comparative Risk Assessment arm of the GBD 2010 estimated the burden of IHD attributable to risk factors.12 National and subnational risk factor surveys were analyzed in order to estimate for each risk factor a mean exposure, an optimal, minimum risk exposure was selected and the relative risk per unit of risk factor exposure was obtained from the literature. Attributable burden was calculated using the population attributable fraction method, assuming independent effects from each risk factor. The main risk factor clusters were tobacco consumption, physiologic factors (high fasting plasma glucose, high total cholesterol, high blood pressure, high body mass index), diet (diet low in fruits, diet low in vegetables, diet low in whole grains, diet low in nuts and seeds, diet high in processed meat, diet high in sugar-sweetened beverages, diet low in fiber, diet low in seafood omega-3 fatty acids, diet low in polyunsaturated fatty acids, diet high in trans fatty acids, diet high in sodium), air pollution (ambient particulate matter pollution or household air pollution from solid fuels) and other environmental risks (lead exposure).
Global, regional, and national burden of IHD are reported as absolute numbers of DALYs and age-standardized DALYs per 100,000 population. The World Health Organization (WHO) standard population was used to age-standardize data using the direct method. The GBD 2010 Study reported results for 21 world regions. For this report we simplified these regions into seven “super-regions”: High Income, East Asia/Pacific, North Africa/Middle East, sub-Saharan Africa, Latin American and Caribbean, Eastern Europe/Central Asia, and South Asia. GBD 2010 high income regions were North America, Western Europe, Australasia (Australia and New Zealand), and Asia Pacific High Income (Japan, South Korea, and Singapore)]; the remainder of countries were grouped into regions by geographic proximity and cause of death pattern. Per capita country income in 2010, measured as Gross National Income (GNI, 2010 $U.S.) using the Atlas method, was obtained from the World Bank, and was the basis for 2010 World Bank national income classifications used in Figure 3 and Figure 4 (high, upper middle, lower middle, and low income).13 Because per capita country income data are right-skewed (toward high income countries), GNI was natural log transformed for the Figure 4 plot of DALY rates by GNI.
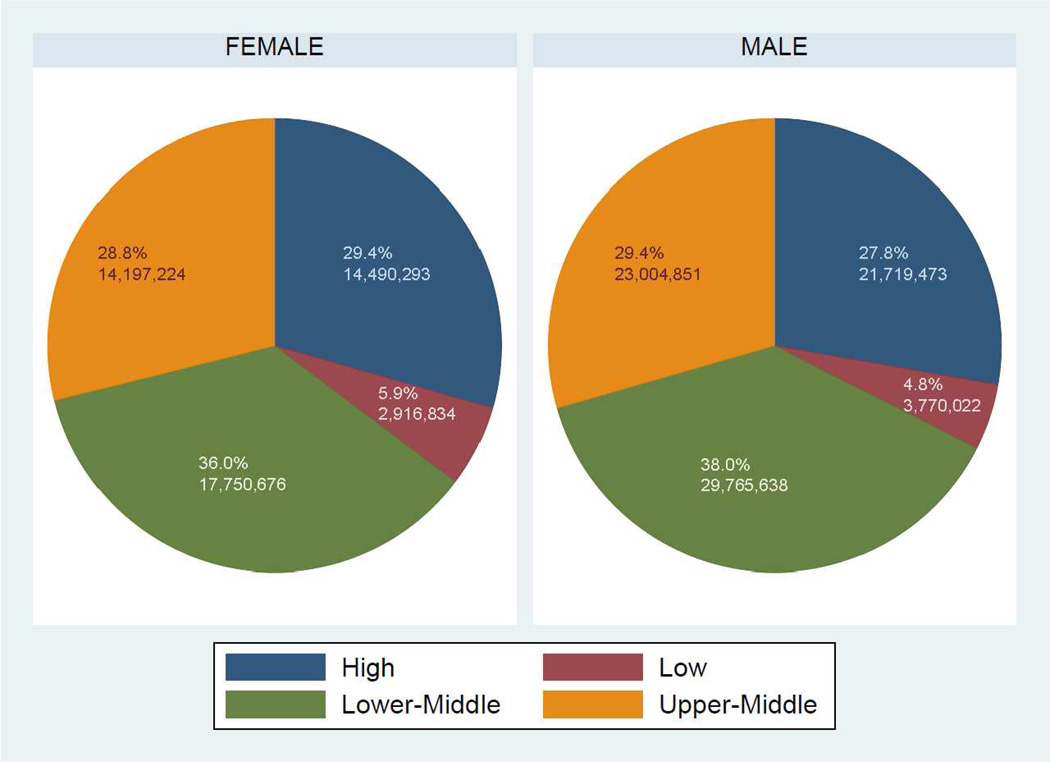
Figure 3.
World Bank income category composition of absolute numbers of ischemic heart disease (IHD) disability-adjusted life years (DALYs) in males and females in 2010, the Global Burden of Diseases, Injuries and Risk Factors 2010 Study
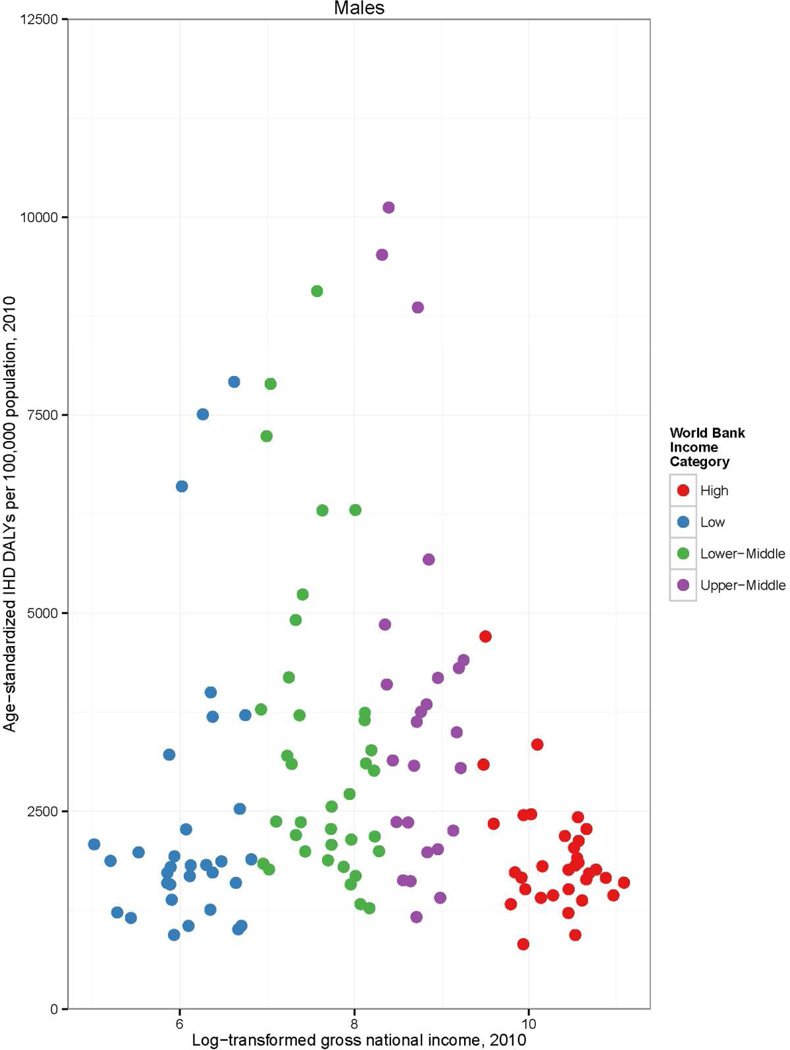
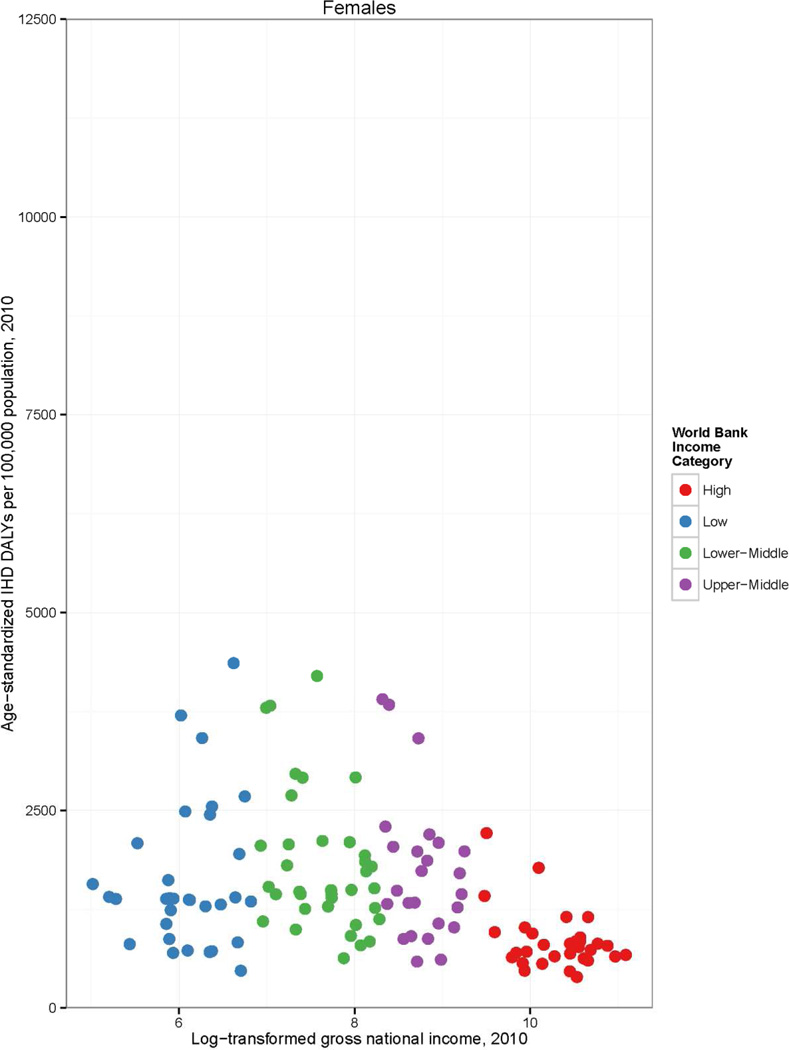
Figure 4.
Age-standardized ischemic heart disease (IHD) disability-adjusted life years (DALYs) per 100,000 population in 1990 and 2010, by country and World Bank income category, the Global Burden of Diseases, Injuries and Risk Factors 2010 Study
Results
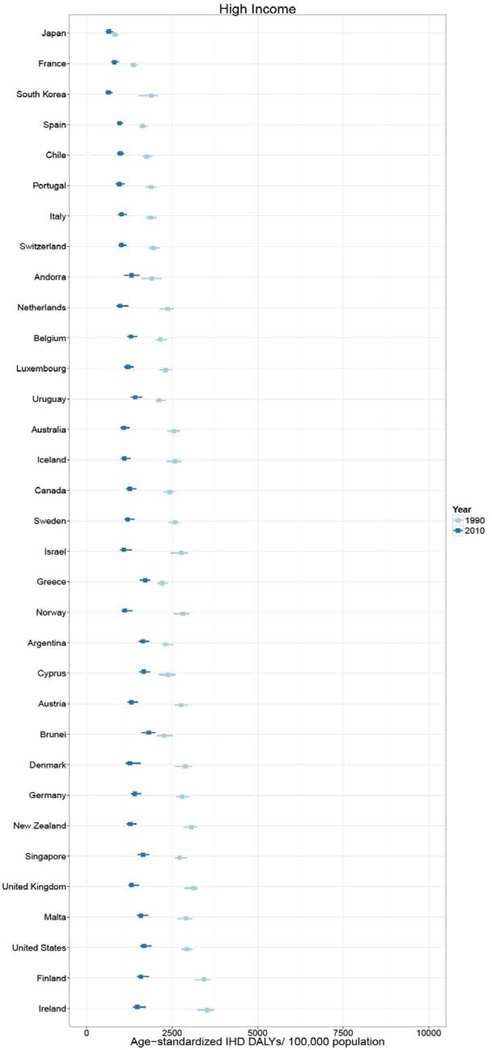
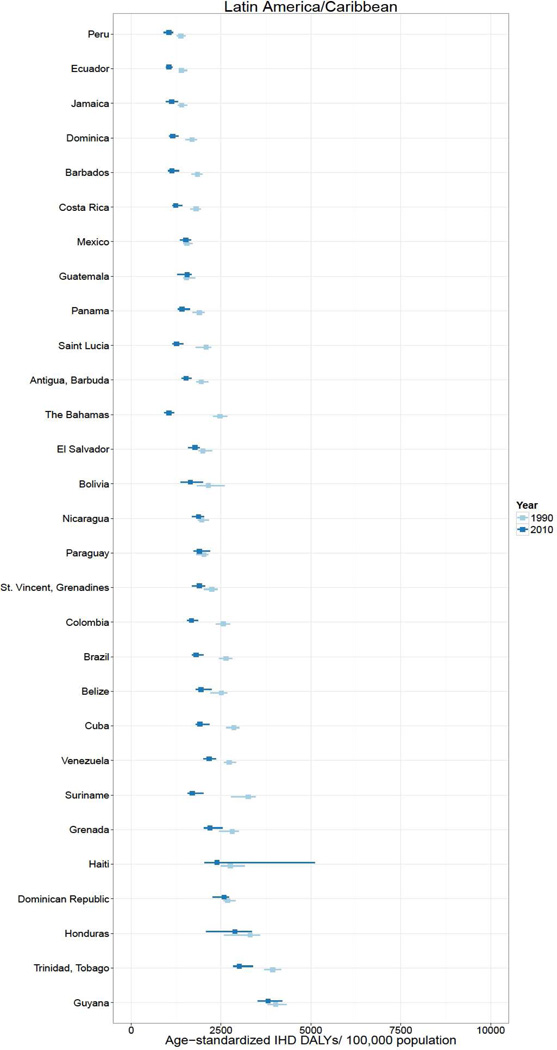
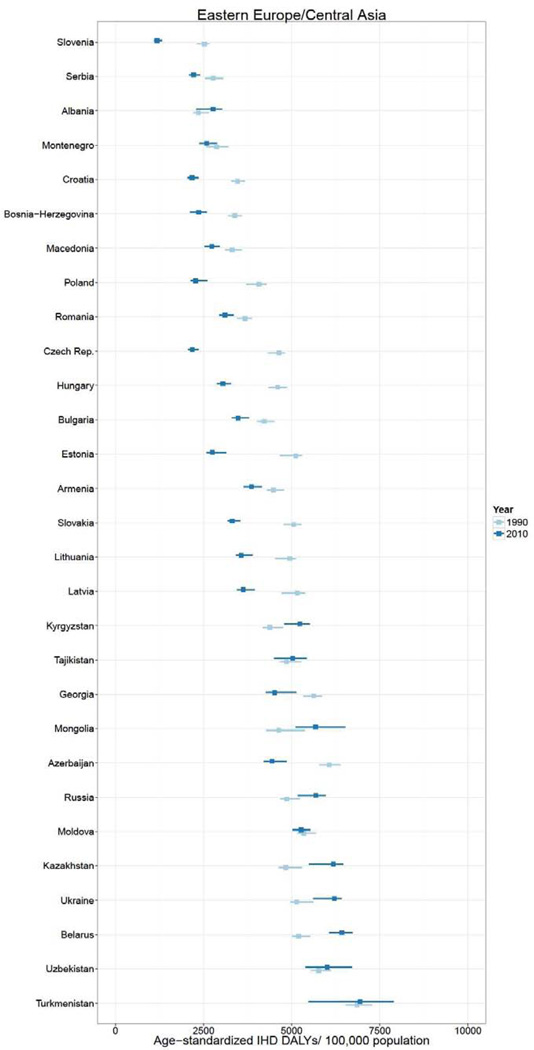
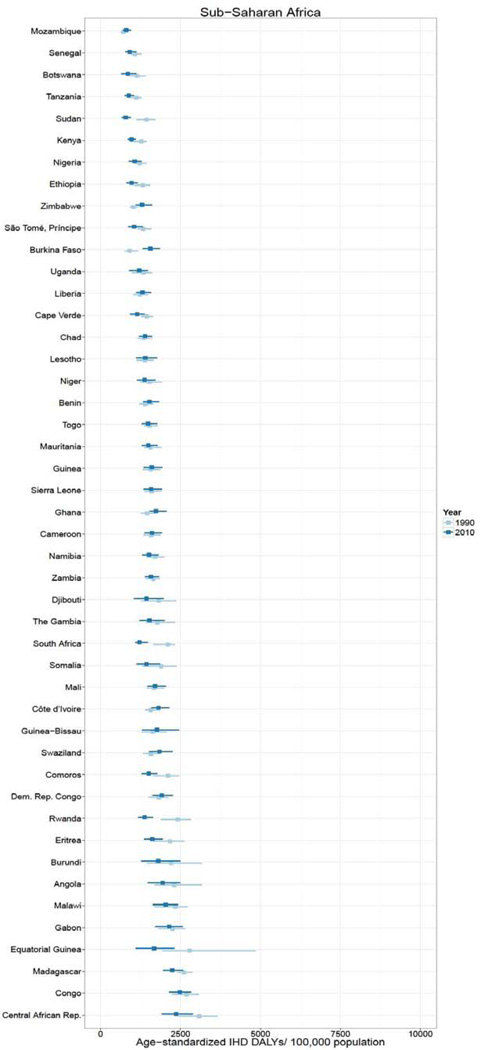
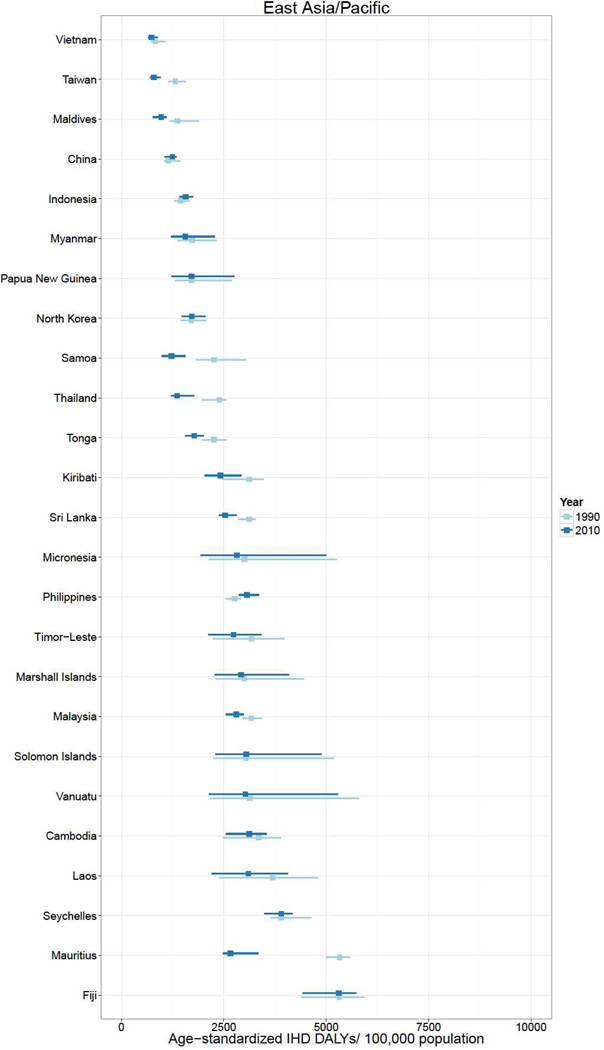
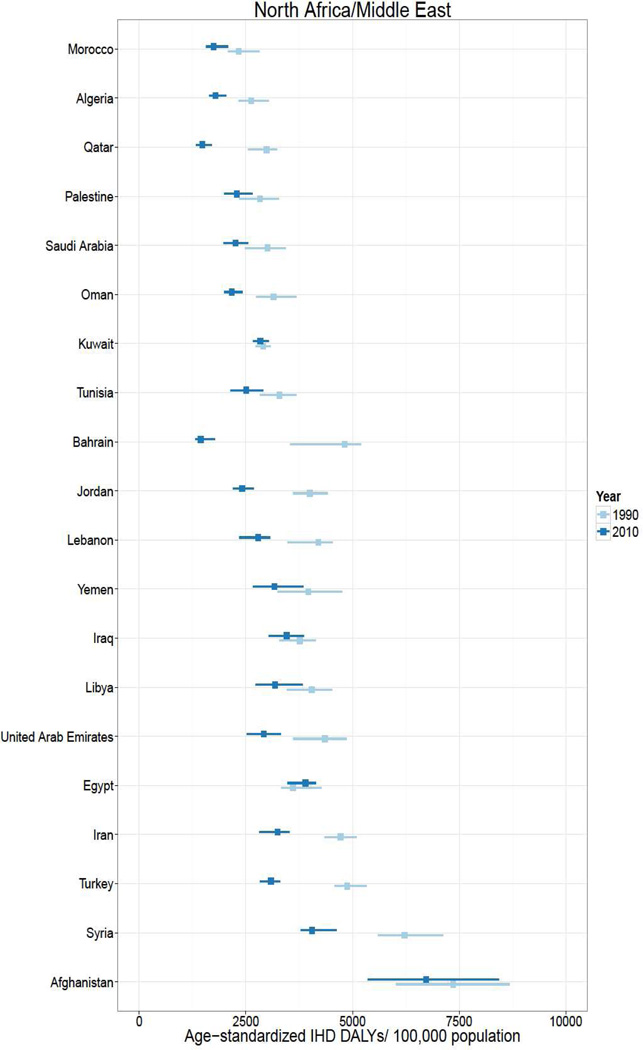
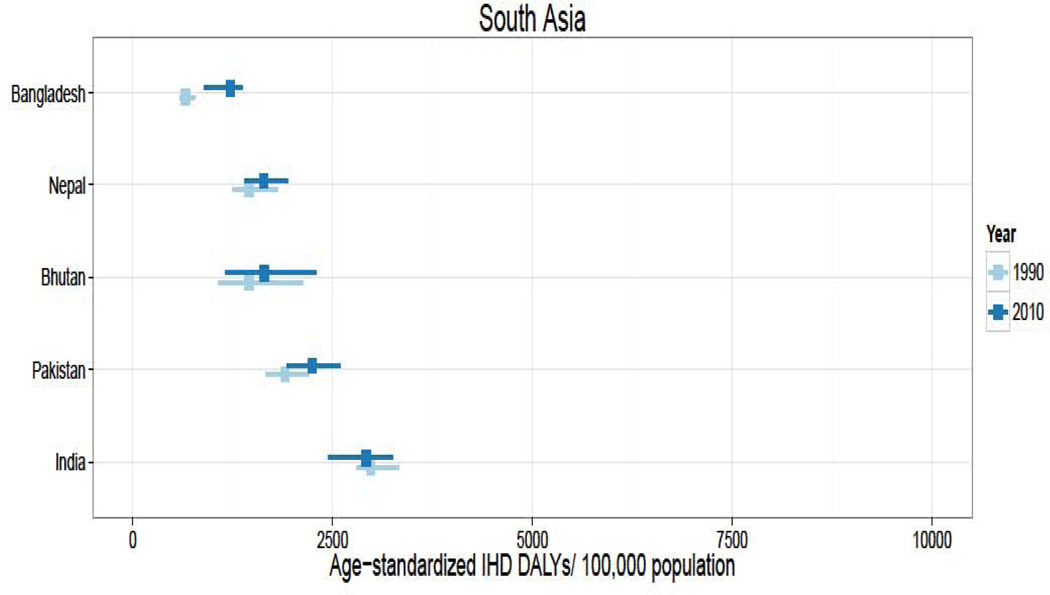
In 2010, over 129 million DALYs were attributed to IHD, representing the highest cause-specific disease burden in the world. Globally, Eastern Europe, Central Asia, North Africa/Middle East, and South Asia lost the highest age-standardized DALYs per 100,000 in the world in 2010.2 East Asia, sub-Saharan Africa, Andean Latin America, and the high income regions had the lowest age-standardized IHD burden rates. Age-standardized IHD DALY rates varied for countries within regions (Figure 1). Turkmenistan, Belarus, Kazakhstan and Ukraine had the world’s highest age-standardized IHD DALY rates (all >6,000 DALYs lost per 100,000). Sub-Saharan African countries and specific countries in the East Asia (Vietnam and Taiwan), Andean Latin America (Ecuador and Peru) and High Income regions (Japan, South Korea, and France) had the lowest (all <1,550 per 100,000). While age-standardized IHD DALYs per 100,000 decreased or change was not detected in most countries between 1990 and 2010, the rate increased most in a number of Eastern Europe and Central Asian countries (increases of >1,000 per 100,000 in Mongolia, Russia, Belarus, Ukraine, and Kazakhstan) and South Asian countries (>175 per 100,000 in Bangladesh, Nepal, Bhutan, and Pakistan).
Figure 1.
Age-standardized ischemic heart disease (IHD) disability-adjusted life years (DALYs) per 100,000 population in 1990 and 2010, by super-region and country, the Global Burden of Diseases, Injuries and Risk Factors 2010 Study
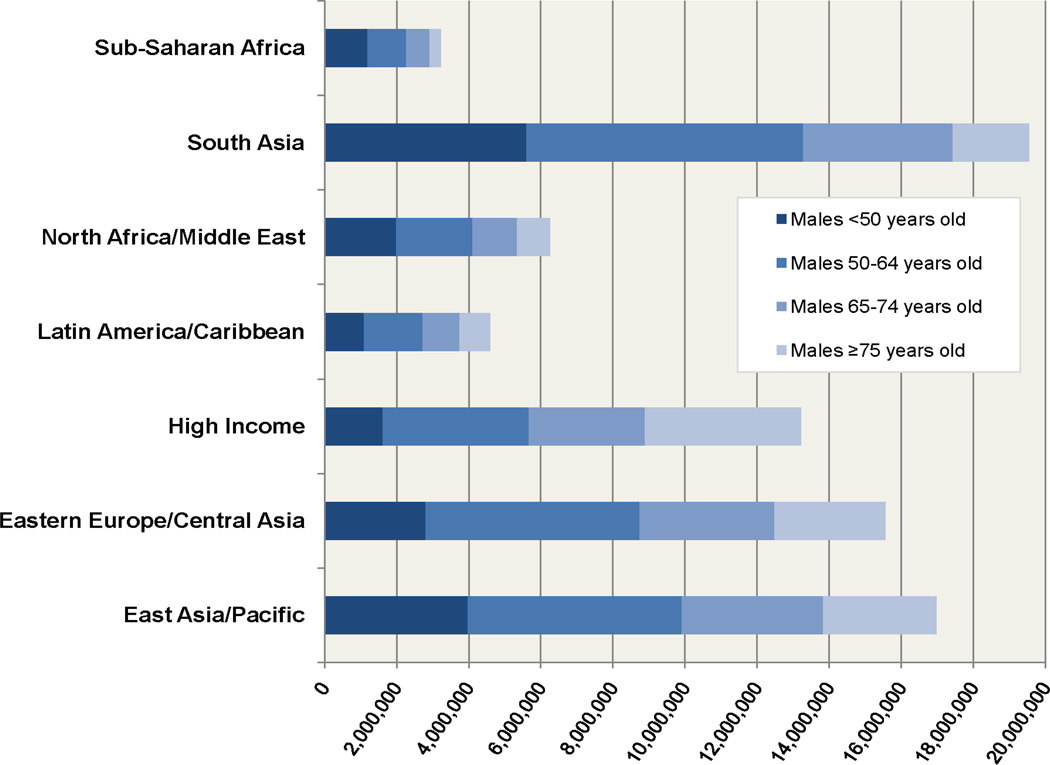
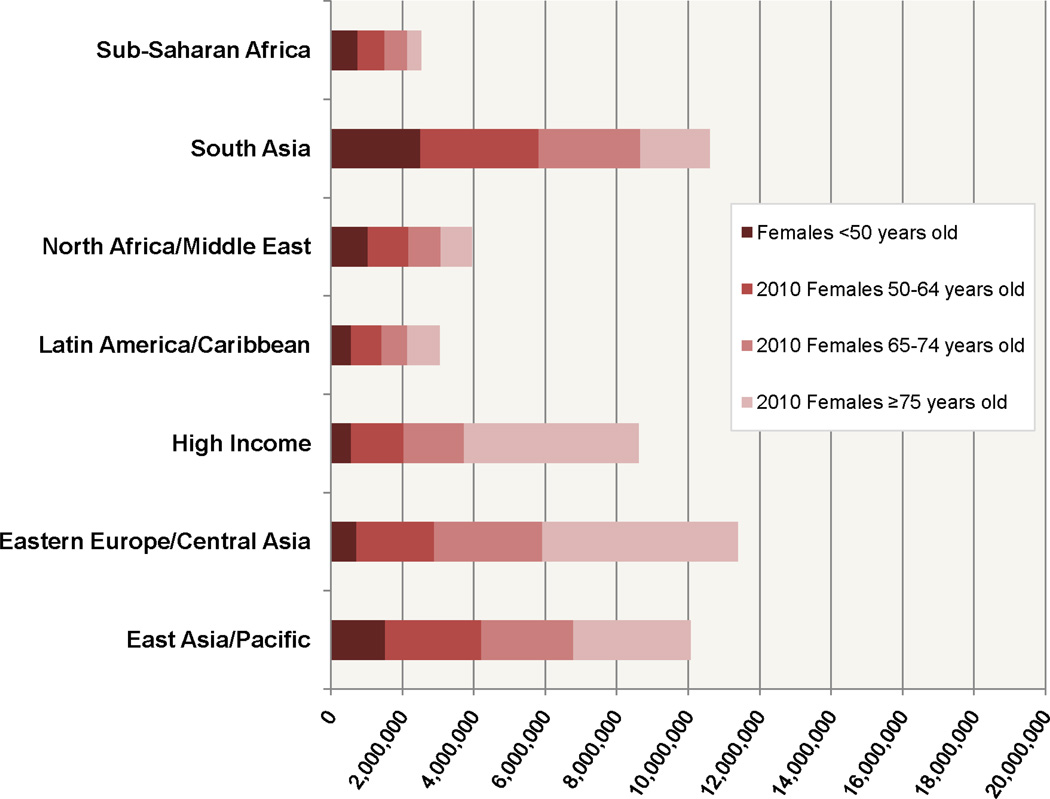
In the sub-Saharan Africa, North Africa and Middle East, and South Asia regions the burden of IHD weighed in much higher proportion on younger adults in 2010 [about a third of DALYs lost in males (37%, 32%, and 29%, respectively) and a quarter of DALYs lost in females <50 years old (30%, 26%, and 24%, respectively), Figure 2]. About two-thirds of the global burden of IHD burden affected populations in middle income countries (Figure 3). However, there was a high level of variability in age-standardized IHD DALYs per 100,000 within World Bank country income groups (Figure 4). For example, within the high income category, Chile had a rate of 1,142 DALYs lost per 100,000 and Finland had a rate of 3,128. Within middle income the range was even more remarkable: between 1,752 DALYs per 100,000 population (Botswana) and 13,955 (Belarus). Though these rates represent countries with vastly different contexts in terms of IHD risk factor levels and competing health risks, one possible implication of this wide variation is that some middle-income countries have achieved an IHD prevention standard comparable with high income countries.
Figure 2.
Age composition of absolute numbers of ischemic heart disease (IHD) disability-adjusted life years (DALYs) in males and females in 2010, by super-region, the Global Burden of Diseases, Injuries and Risk Factors 2010 Study
The two leading contributors of IHD DALYs in all countries in 2010 were physiological risks and dietary risks in aggregate (Figure 5). However, the third leading contributor to IHD DALYs varied by country. For example, in Russia, alcohol use was the third leading contributor of IHD DALYs (5,089,363 DALYs), behind physiological and dietary risks. In China, the third leading contributor to IHD DALYs was air pollution (8,803,667 DALYs). In Mexico, the third leading contributor to IHD DALYs was physical inactivity (446,088 DALYs).
Figure 5.
Absolute numbers of ischemic heart disease (IHD) disability-adjusted life years (DALYs) attributed to major risk factors in males and females in 2010, the Global Burden of Diseases, Injuries and Risk Factors 2010 Study
*high fasting plasma glucose; high total cholesterol; high blood pressure; high body mass index
†lead exposure
§Diet low in fruits; diet low in vegetables; diet low in whole grains; diet low in nuts and seeds; diet high in processed meat; diet high in sugar-sweetened beverages; diet low in fiber; diet low in seafood omega-3 fatty acids; diet low in polyunsaturated fatty acids; diet high in trans fatty acids; diet high in sodium
‡Ambient parXculate maYer polluXon; household air polluXon from solid fuels
Discussion
IHD was the world’s leading cause of disease burden in 2010. At the regional level, the highest per capita IHD burden rests on the Eastern Europe/Central Asia, North Africa/Middle East and South Asia regions. However, at the country level, there is considerable variability in age-standardized IHD DALY rates, with variation as high as 3,644 DALYs lost per 100,000 persons in the East Asia/Pacific super-region. Even within World Bank income groups, IHD rates varied considerably, by about 8,400 DALYs lost per 100,000 persons for low-middle income, 9,500 DALYs per 100,000 persons for high middle income, 4,300 DALYs per 100,000 persons for high income and 7,400 DALYs per 100,000 persons for low income countries.
In most countries, age-standardized IHD burden decreased between 1990 and 2010. Our prior work identified IHD “hot spot” regions where age-standardized IHD DALY rate actually increased significantly: South Asia, North Africa/Middle East, and Eastern Europe.2 Age-standardized rates benchmark a country’s success with IHD prevention on average in individuals over time, but absolute IHD burden is equally important for health planners. The global burden of IHD (absolute numbers of IHD DALYs) increased 29% between 1990 and 2010. Underlying this overall change was a 5% absolute decrease in the high income countries and a 59% increase in low and middle income countries. Of particular importance for sustained development in the middle income world is our finding that over a quarter of IHD burden in North Africa/Middle East, South Asia, and sub-Saharan Africa affects adults <50 years old, that is, adults in the prime of their lives.
The 2011 United Nations High Level Meeting on Non-communicable Diseases focused attention on the concept of the epidemiologic transition from maternal/fetal and infectious diseases to non-communicable diseases, and the observation that non-communicable diseases are no longer an epidemic of the high income world alone. Our paper paints a more complex epidemiologic picture for IHD not found in aggregate measures for “low and middle income countries” or “developing countries”. Particularly in the middle income regions that bear the largest absolute burden of IHD, the rate of IHD varies by nearly eight fold among countries. IHD prevention may be a top priority for middle income countries like Belarus, Kazakhstan, and Ukraine, but others like Botswana, Chile, and Peru may want to devote valuable prevention resources toward controlling other diseases, for example, lowering blood pressure to prevent stroke. The GBD 2010 analysis of IHD burden attributable to risk factors showed the universal importance of controlling dietary and physiological risks (classic behavioral risk factors), but also that prevention policies should be tailored to local priorities, e.g., cultivating healthier alcohol consumption behavior in Russia or reducing air pollution in China.
The GBD 2010 is a large and complex study, and by necessity early reports from the study emphasized broad global trends in disease burden. National-level estimates drill down to the level where most public health and health system decisions are made, and where most health system resources are allocated. We demonstrated that IHD burden varies considerably among countries—even within the same broad geographic region or income category. This observation of variability of IHD mortality of countries within broad WHO regions has been made by others for a smaller set of countries with adequate data,14 but the standardized, global data analysis of the GBD illustrates country-level variability all the more. Of course, IHD burden varies even among the states or provinces of large countries. We hope that the country level results from the GBD 2010 represent a step towards a standardized global epidemiologic surveillance with information about local contexts and local prevention needs. We anticipate future global burden work will extend disease burden estimates to the subnational level. Global trends are important, but local epidemiology is needed for efficient and equitable allocation of local resources.
Country level GBD 2010 estimates represent an advance for global public health, but important limitations must be acknowledged. First and foremost, IHD mortality and nonfatal IHD prevalence and incidence data are missing or of poor quality for some countries, particularly so in the sub-Saharan Africa region.5 The geographically hierarchical design of the GBD CODEm and DisMOD-MR mixed-effects models allow for “borrowing strength” among countries within broad regions for specific ages and years. The GBD 2010 does propagate uncertainty surrounding estimates for smaller countries and those with lower quality source data (as is illustrated in the credible intervals shown in Figure 1). However, a consequence of the GBD’s geographically hierarchical design is that it may under represent the amount of variability in IHD burden among countries in the same region and super-region.
“Complete” GBD 2010 country level IHD burden estimates are still estimated, and serve as a summary measure rather than a replacement for epidemiologic surveillance at the national level. We advocate for improved surveillance as the only way to achieve the goal of comparability that is at the heart of GBD. It may take decades for low and middle income nations (and even some high income nations like the U.S.) to achieve linkage of outpatient, inpatient, and mortality records for every citizen as part of a universal health insurance scheme that has been achieved by some countries. The World Health Report 2013, titled “Research for Universal Health Coverage”, emphasized that many low and middle income countries now have built a research infrastructure sufficient to enable them to become “producers of research”.15 Along the road to achieving the goal of universal health coverage for their people, low and middle income countries that are in the process of building health system capacity may need to develop innovative use of strategically placed subnational sentinel surveillance sites, mobile communications technology,16 and low cost, locally adaptable survey methods like the WHO STEPS program17 in order to take the first steps toward comprehensive local surveillance programs. Universal epidemiologic surveillance should go hand in hand with achieving universal health care.
In conclusion, using standard and comparable methods for measuring IHD burden across regions, countries and time periods, the GBD 2010 Study confirmed the prediction that the majority of IHD burden affects adults in middle income countries. Adults in low and middle income countries are more likely to be struck down by IHD in their prime working and providing years. Within broad GBD regions, and especially middle income regions, IHD rates varied considerably, leading us to conclude that the challenges of IHD surveillance, prevention, and control are ideally best met by acting at the country level.
Acronyms and abbreviations
- IHD
ischemic heart disease
- GBD 2010
Global Burden of Disease 2010 Study
- YLL
Years of Life Lost due to disability
- YLD
Years Lived with Disability
- ICD
International Classification of Diseases
- GNI
Gross National Income
- WHO
World Health Organization
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement: All authors have no conflicts of interest to report.
Disclaimer:
The views expressed in this article are those of the author and do not necessarily represent the views of the National Heart, Lung, and Blood Institute, National Institutes of Health, or the U.S. Department of Health and Human Services.
References
- 1.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 2.Moran AE, Forouzanfar MH, Roth G, Mensah GA, Ezzati M, Flaxman A, Murray CJL, Naghavi M. The Global Burden of Ischemic Heart Disease in 1990 and 2010: The Global Burden of Disease 2010 Study. Circulation. doi: 10.1161/CIRCULATIONAHA.113.004046. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forouzanfar MH, Moran AE, Flaxman AD, Roth G, Mensah GA, Ezzati M, Naghavi M, Murray CJL. Assessing the Global Burden of Ischemic Heart Failure. Part 2: Analytic Methods and Estimates of the Global Epidemiology of Ischemic Heart Disease in 2010. Global Heart. 2012;7(4):331–342. doi: 10.1016/j.gheart.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moran AE, Forouzanfar MH, Roth G, Mensah GA, Ezzati M, Flaxman A, Murray CJL, Naghavi M. Temporal trends in ischemic heart disease mortality in 21 world regions, 1980–2010: the Global Burden of Disease 2010 Study. Circulation. doi: 10.1161/CIRCULATIONAHA.113.004042. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moran AE, Oliver JT, Mirzaie M, Forouzanfar MH, Chilov M, Anderson L, Morrison JL, Khan A, Zhang N, Haynes N, Tran J, Murphy A, DeGennaro V, Roth G, Zhao D, Peer N, Pichon-Riviere A, Rubinstein A, Pogosova N, Prabhakaran D, Naghavi M, Ezzati M, Mensah GA. Assessing the Global Burden of Ischemic Heart Disease. Part 1: Methods for a Systematic Review of the Global Epidemiology of Ischemic Heart Disease in 1990 and 2010. Global Heart. 2012;7(4):315–329. doi: 10.1016/j.gheart.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naghavi M, Makela S, Foreman K, O'Brien J, Pourmalek F, Lozano R. Algorithms for enhancing public health utility of national causes-of-death data. Population health metrics. 2010;8:9. doi: 10.1186/1478-7954-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salomon JA, Vos T, Hogan DR, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2129–2143. doi: 10.1016/S0140-6736(12)61680-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hemingway H, Fitzpatrick NK, Gnani S, et al. Prospective validity of measuring angina severity with Canadian Cardiovascular Society class: The ACRE study. The Canadian journal of cardiology. 2004;20(3):305–309. [PubMed] [Google Scholar]
- 11.Forouzanfar MH, Moran AE, Flaxman AD, et al. Assessing the global burden of ischemic heart disease, part 2: analytic methods and estimates of the global epidemiology of ischemic heart disease in 2010. Glob Heart. 2012;7(4):331–342. doi: 10.1016/j.gheart.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The World Bank. [accessed December 16 2013];How we classify countries. 2013 http://data.worldbank.org/about/country-classifications.
- 14.Mirzaei M, Truswell AS, Taylor R, Leeder SR. Coronary heart disease epidemics: not all the same. Heart. 2009;95(9):740–746. doi: 10.1136/hrt.2008.154856. [DOI] [PubMed] [Google Scholar]
- 15.Dye C, Boerma T, Evans D, Harries A, Lienhardt C, McManus J, Pan T, Terry R, Zachariah R. Research for Universal Health Coverage: the World Health Report 2013. Luxembourg: World Health Organization; 2013. [Google Scholar]
- 16.Alkmim MB, Figueira RM, Marcolino MS, et al. Improving patient access to specialized health care: the Telehealth Network of Minas Gerais, Brazil. Bull World Health Organ. 2012;90(5):373–378. doi: 10.2471/BLT.11.099408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Heath Organization. [accessed December 16 2013];STEPwise approach to chronic disease risk factor surveillance (STEPS) 2013 http://www.who.int/chp/steps/riskfactor/en/index.html.