Abstract
Background
The steady rise in demand for total hip arthroplasty constitutes a significant and increasing burden on health care resources. The biggest contributors to the total cost of hip replacement procedures other than the price of the implant are hospital stay and postoperative rehabilitation. Blood management is one of the most adjustable factors that can impact length of stay and cost-efficiency while improving patient safety.
Questions/Purposes
The primary purpose of this retrospective study was to assess the potential impact of blood management interventions on length of hospital stay after primary unilateral total hip arthroplasty. This was achieved by first identifying which patient and surgical factors are associated with an increased risk of prolonged hospital stay. Subsequently, the significant factors were controlled for through a multivariate regression analysis to quantify the association between blood transfusions and increased hospital stay.
Methods
Retrospectively, the study included 2,104 primary total hip replacements. Eight hundred eighty-eight procedures were performed on males and 1,216 on females, with a mean age of 64 years at the time of the surgery (range 18–94 years) and BMI of 28.6 kg/m2 (range 12–51.5 kg/m2). The correlation between each factor and length of stay was analyzed separately using univariate regression analysis. Those variables with p ≤ 0.05 in the univariate model were selected for inclusion in the multivariate logistic regressions. Multiple linear regression was used to analyze the effect of each significant factor and derive odds ratios with adjustment for the other variables.
Results
Multivariate Poisson regression revealed that increased length of stay was significantly correlated to patient age (p = 0.05), the use of coumadin (p = 0.02) or lovenox/heparin (p = 0.007) as opposed to aspirin for anticoagulation, and allogeneic blood transfusion (p < 0.0001). The data shows that allogeneic blood transfusion is associated with a longer hospital stay regardless of absolute drop in hemoglobin level postoperatively or at discharge or the number of units transfused (OR = 1.18, 95% CI = 1.09 to 1.28, p < 0.001).
Conclusion
Transfusion of allogeneic blood is independently associated with increased hospital stay after total hip arthroplasty. Blood management modalities that can significantly reduce transfusion risk could impact length of stay as well as the total cost of hip replacement procedures.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-014-9384-x) contains supplementary material, which is available to authorized users.
Keywords: total hip arthroplasty, length of stay, blood management, allogeneic blood, autologous blood transfusion, anemia
Introduction
The established success of total hip arthroplasty (THA) in restoring mobility makes it one of the most effective interventions in medicine. The clinical course of patients undergoing such procedures has changed significantly in the last decade. Minimally invasive surgical approaches in addition to optimized anesthesia and pain management protocols have allowed earlier and more aggressive mobilization and rehabilitation [28, 35]. Such streamlining of clinical practice aims to reduce preoperative morbidity while increasing cost-efficiency.
The rising demand for hip replacement surgery constitutes a significant and increasing burden upon health care resources [22, 25]. Despite advances in operative technique and clinical management, postoperative hospital stay remains one of the most significant contributors to the total cost of THA procedures [37]. Reducing hospital length of stay (LOS) after hip replacement improves patient satisfaction as well as cost-efficiency [17–20]. Multimodal clinical “fast-track” pathways attempt to reduce length of stay in elective procedures without increasing complications by targeting patient education, preoperative discharge planning, preemptive pain and nausea management, and accelerated rehabilitation [21, 9]. Increased postoperative stay following primary THA has been attributed to several variables, namely older age, female gender, comorbidities, obesity, smoking, low preoperative hip scores, incision length, operative time, and incidence of blood transfusion [6, 8, 10, 12, 16, 18–20, 31, 43].
Preoperative anemia and allogeneic transfusions are both independently associated with increased overall morbidity and adverse outcomes such as prolonged hospitalization, suboptimal rehabilitation, and infections [4, 13, 32, 36, 43]. Blood management protocols aim to reduce exposure to allogeneic blood based on the individualized risk assessment and preoperative hemoglobin (Hb), the time available before surgery, the expected blood loss for the procedure, the strict transfusion thresholds, and the suitable modality for the given setting [2, 7]. Preoperative strategies rely on optimization of preoperative hemoglobin levels through preoperative work-up, iron supplementation and/or erythropoietin, as well as preoperative autologous blood donation. Intraoperative modalities such as hypotensive anesthesia, blood salvage, hemodilution, as well as intravenous or topical pharmacologic agents such as tranexamic acid or fibrin sealants aim to reduce blood loss and transfusion requirements. The potential of such interventions to reduce exposure to allogeneic blood makes blood management one of the most modifiable factors that might significantly impact length of stay [5, 14, 23].
The primary purpose of this retrospective study was to assess the potential impact of blood management interventions on length of hospital stay after primary unilateral total hip arthroplasty. This was achieved by first identifying which patient and surgical factors are associated with an increased risk of prolonged hospital stay. Subsequently, the significant factors were controlled for through a multivariate regression analysis to quantify the association between blood transfusions and increased hospital stay.
Patients and Methods
A retrospective analysis was conducted on 2,104 primary unilateral total hip replacement procedures performed between 2009 and 2012 by one of 13 surgeons at the authors’ institution. All patients underwent a preoperative work-up and given oral iron supplementation. Patients who were considered anemic (hemoglobin level below 12.5 g/dL) were advised to donate one unit of autologous blood 7 to 15 days prior to the date of surgery. No patient was allowed to donate less than 7 days prior to the procedure. Preoperatively, 343 patients (16.3%) were anemic among which 256 chose to donate autologous blood and 87 opted not to. The 1,761 non-anemic patients (83.7%) did not donate autologous units. This protocol was based on previous data from our institution showing no benefit and higher wastage rates for autologous blood donation in non-anemic patients undergoing total hip arthroplasty [3]. Patients received allogeneic transfusions if their hemoglobin (Hb) level dropped below 8.0 g/dL, and they displayed clinical symptoms of anemia (tachycardia and/or hypotension) despite an intravenous fluid bolus. The decision to transfuse autologous blood was made at the discretion of the anesthesiologist and medical attending, and strict transfusion guidelines were not enforced for autologous blood.
Gender, age, body mass index (BMI), preoperative Hb, autologous blood donation, number of autologous transfusions, number of allogeneic transfusions, postoperative Hb levels until date of discharge, and in-house complications were recorded. Length of stay was calculated as the number of days in hospital from the day of surgery to the day of discharge, with day of surgery being day 0. Patients who underwent revision THA, simultaneous bilateral THA, and patients with bleeding disorders were excluded. The study was approved by the institutional review board at the authors’ institution.
All procedures were performed under hypotensive spinal–epidural anesthesia using a standardized posterior approach. During the study period, 888 procedures were performed on males and 1,216 on females, with a mean age of 64 years at the time of the surgery (range 18–94 years) and BMI of 28.6 kg/m2 (range 12–51.5 kg/m2). Patients were divided by BMI into groups according to the World Health Organization (WHO) criteria; underweight (<18.5 kg/m2), normal weight (18.5 to 24.9 kg/m2), overweight (25 to 29.9 kg/m2), and obese (>30 kg/m2). Patients with BMI greater than 30 kg/m2 were further subdivided into three groups, 30 to 34.9 kg/m2, 35 to 39.9 kg/m2, and 40 kg/m2 or more (Table 1).
Table 1.
Demographic factors of patients in the study
| Factor | Number | Mean LOS | p value |
|---|---|---|---|
| Age (years) | |||
| <60 | 704 (33.5%) | 3.2 ± 1.2 | <0.0001a |
| 60–69 | 729 (34.6%) | 3.3 ± 1.2 | |
| 70–79 | 488 (23.2%) | 3.5 ± 1.2 | |
| ≥80 | 183 (8.7%) | 3.8 ± 1.6 | |
| Gender | |||
| Male | 888 (42.2%) | 3.3 ± 1.3 | <0.0001b |
| Female | 1,216 (57.8%) | 3.5 ± 1.2 | |
| Laterality | |||
| Left | 951 (45.2%) | 3.4 ± 1.3 | 0.4747b |
| Right | 1,153 (54.8%) | 3.4 ± 1.2 | |
| BMI (kg/m2)c | |||
| <18.5 | 25 (1.2%) | 3.2 ± 1.0 | <0.0001a |
| 18.5–24.9 | 588 (28.0%) | 3.4 ± 1.3 | |
| 25–29.9 | 761 (36.4%) | 3.3 ± 1.2 | |
| 30–34.9 | 435 (20.7%) | 3.4 ± 1.2 | |
| 35–39.9 | 183 (8.7%) | 3.5 ± 1.3 | |
| ≥40 | 107 (5.1%) | 3.8 ± 1.5 | |
aObtained from Kruskal–Wallis test
bObtained from Wilcoxon rank-sum test
cSome missing data
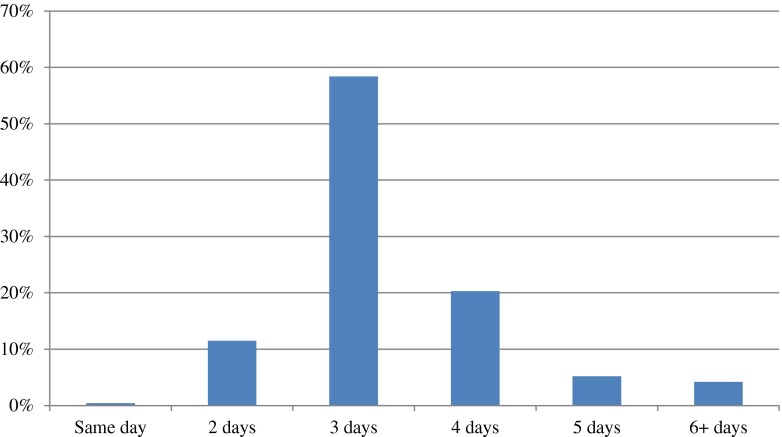
Descriptive statistics were used to illustrate patient demographics and health characteristics. Medians and the 25th and the 75th percentiles were calculated for length of stay; means and standard deviations were calculated for continuous variables, namely age, BMI, preoperative and postoperative hemoglobin levels, and hemoglobin drop directly postoperatively and at discharge. Frequency distributions were used for categorical variables, including gender, laterality, surgeon, day of the procedure, preoperative or postoperative anemia, type of anticoagulant, preoperative autologous blood donation, and blood transfusion, whether autologous, allogeneic, or both. The correlation between each factor and length of stay was analyzed separately using Kruskal–Wallis test, Wilcoxon rank-sum, or Pearson’s chi-square as appropriate. Those variables with p ≤ 0.05 in the univariate model were selected for inclusion in the multivariate logistic regressions. Multiple linear regression was used to analyze the effect of each significant factor and derive odds ratios with adjustment for the other variables. Regression employed the length of stay as the dependent variable and the preselected risk factors as the independent variables. All analyses were conducted using SAS for Windows 9.2 (SAS Institute Inc., Cary, NC, USA). All tests were two-sided and a critical p value of 0.05 was set for all comparisons (Fig. 1).
Fig. 1.
Patient distribution by length of stay following primary THA.
Results
The mean duration of hospital stay for all the patients was 3.4 days with a range of 1 to 18 days. The median LOS was 3 days with an inter-quartile range (i.e., 25th and 75th percentile) of 3 to 4 days. Tables 1, 2, and 3 display the individual categories for each factor, the number of cases in each category, and the mean length of stay. Older age, female gender, higher BMI, and lower hemoglobin levels were associated with longer hospital stay. The vast majority of patients (91%) were discharged within 4 days, and 70% of the patients were actually able to leave the hospital after 3 days (Tables 1, 2, and 3).
Table 2.
The effect of hemoglobin level and blood transfusions on LOS
| Factor | Number | Mean LOS | p value |
|---|---|---|---|
| Preop Hb (g/dL) | |||
| <12 | 190 (9.0%) | 3.7 ± 1.6 | 0.002a |
| 12–12.9 | 403 (19.2%) | 3.5 ± 1.2 | |
| 13–13.9 | 637 (30.3%) | 3.4 ± 1.1 | |
| ≥14 | 874 (41.5%) | 3.3 ± 1.3 | |
| Autologous blood | |||
| Did not donate | 1,848 (87.8%) | 3.4 ± 1.2 | <0.0001b |
| Donate | 256 (12.2%) | 3.6 ± 1.4 | |
| Blood transfusion | |||
| None | 1,792 (85.2%) | 3.3 ± 1.2 | <0.0001a |
| Autologous only | 96 (4.6%) | 3.5 ± 1.1 | |
| Allogeneic only | 182 (8.7%) | 4.0 ± 1.8 | |
| Autologous + allogeneic | 34 (1.6%) | 4.2 ± 1.3 | |
| No. of allogeneic units received | |||
| 0 | 1,888 (89.7%) | 3.3 ± 1.2 | <0.0001a |
| 1 | 173 (8.2%) | 4.0 ± 1.6 | |
| 2 | 32 (1.5%) | 4.1 ± 1.8 | |
| 3 | 7 (0.3%) | 4.9 ± 3.6 | |
| 4 | 3 (0.1%) | 5.7 ± 0.6 | |
| 7 | 1 | 5 | |
aObtained from Kruskal–Wallis test
bObtained from Wilcoxon rank-sum test
Table 3.
Surgical factors of patients in the study
| Factor | Number | Mean LOS | p value |
|---|---|---|---|
| Surgeon (TKA) | |||
| 1 | 59 (2.8%) | 2.9 ± 1.1 | <0.0001a |
| 2 | 36 (1.7%) | 2.8 ± 0.7 | |
| 3 | 512 (24.3%) | 3.4 ± 1.4 | |
| 4 | 7 (0.3%) | 3.1 ± 0.4 | |
| 5 | 51 (2.4%) | 3.2 ± 0.8 | |
| 6 | 185 (8.8%) | 3.4 ± 1.1 | |
| 7 | 19 (0.9%) | 3.6 ± 1.1 | |
| 8 | 421 (20.0%) | 3.4 ± 1.4 | |
| 9 | 301 (14.3%) | 3.3 ± 1.2 | |
| 10 | 136 (6.5%) | 3.4 ± 1.2 | |
| 11 | 71 (3.4%) | 3.5 ± 1.4 | |
| 12 | 239 (11.4%) | 3.5 ± 1.2 | |
| 13 | 67 (3.2%) | 3.7 ± 1.2 | |
| Day of operation | |||
| Monday | 461 (21.9%) | 3.2 ± 0.9 | <0.0001a |
| Tuesday | 93 (4.4%) | 3.2 ± 1.0 | |
| Wednesday | 543 (25.8%) | 3.6 ± 1.5 | |
| Thursday | 271 (12.9%) | 3.5 ± 1.4 | |
| Friday | 554 (26.3%) | 3.4 ± 1.2 | |
| Saturday | 182 (8.7%) | 3.1 ± 1.3 | |
| Anticoagulation | |||
| None | 29 (1.4%) | 3.4 ± 1.0 | <0.0001a |
| Aspirin | 1,573 (74.8%) | 3.3 ± 1.1 | |
| Aspirin + coumadin | 200 (9.5%) | 3.6 ± 1.4 | |
| Aspirin + coumadin + lovenox/heparin | 21 (1.0%) | 4.7 ± 2.3 | |
| Aspirin + lovenox/heparin | 26 (1.2%) | 4.0 ± 3.2 | |
| Coumadin | 215 (10.2%) | 3.6 ± 1.1 | |
| Coumadin + lovenox/heparin | 34 (1.6%) | 4.4 ± 2.1 | |
| lovenox | 6 (0.3%) | 3.8 ± 1.6 | |
*obtained from Kruskal–Wallis test
A number of preoperative factors were found to be significant predictors of length of stay when subjected to univariate analysis but not significant after multivariate analysis. These variables included female gender, higher BMI, lower preoperative and postoperative hemoglobin levels until postoperative day 2 and on discharge, autologous blood donation, and the surgeon performing the procedure. Multivariate Poisson regression revealed that longer length of stay was significantly associated with older patient age (p = 0.05), the use of coumadin (p = 0.02) or lovenox/heparin (p = 0.007) as opposed to aspirin for anticoagulation, and allogeneic blood transfusion (p < 0.0001). However, after accounting for confounding factors, prolonged hospital stay was not associated with the absolute drop in hemoglobin level (p = 0.63), the number of allogeneic units transfused, or autologous blood donation (p = 0.61) or transfusion (p = 0.65). In addition, having surgery on Monday was associated with decreased hospital stay (p = 0.005) (Table 4).
Table 4.
Multivariate regression analysis to adjust for confounding factors
| Variable | OR (95% CI) | Pr > |t| |
|---|---|---|
| Age (in years) | 1.00 (1.00, 1.00) | 0.05a |
| Sex (female vs. male) | 1.05 (0.99, 1.11) | 0.09 |
| BMI (kg/m2) | 1.00 (1.00, 1.01) | 0.12 |
| Preop Hb (g/dL) | 0.99 (0.96, 1.03) | 0.74 |
| Postop Hb (g/dL) | 1.01 (0.98, 1.05) | 0.53 |
| Hb drop (g/dL) | 0.99 (0.96, 1.01) | 0.33 |
| Day of operation (Friday (reference)) | ||
| Monday | 0.91 (0.82, 0.998) | 0.05a |
| Tuesday | 0.93 (0.80, 1.08) | 0.35 |
| Wednesday | 1.04 (0.96, 1.13) | 0.29 |
| Thursday | 1.00 (0.92, 1.09) | 0.97 |
| Saturday | 0.92 (0.84, 1.02) | 0.10 |
| Blood thinner use | ||
| Aspirin | 1.02 (0.93, 1.12) | 0.65 |
| Coumadin | 1.09 (1.01, 1.18) | 0.02a |
| Lovenox/Heparin | 1.17 (1.05, 1.31) | 0.006a |
| Preop autologous blood | ||
| Donation vs No donation | 1.03 (0.92, 1.15) | 0.61 |
| Blood transfusion | ||
| Autologous (yes vs no) | 1.03 (0.90, 1.18) | 0.64 |
| Allogeneic (yes vs no) | 1.18 (1.09, 1.28) | <.0001a |
aSignificant association with longer length of stay
Discussion
This study aims to evaluate the effect of allogeneic transfusions and potential impact of blood management on duration of hospitalization after primary hip arthroplasty. In accordance with previous data in the literature, the results confirm that there are a number of independent preoperative factors that can be used to predict the length of stay. However, this study adds the association between heparin, lovenox, or warfarin and length of stay as compared to aspirin, as well as lack of association between LOS and autologous blood donation or transfusion. In addition, our data shows that allogeneic blood transfusion is associated with a longer hospital stay regardless of absolute drop in hemoglobin level postoperatively or at discharge or the number of units transfused (OR = 1.18, 95% CI = 1.09 to 1.28, p < 0.001).
Some of the results that were only significant in the univariate analysis might be accounted for by different medical comorbidities of the patients, and the lack of American Society of Anesthesiologists (ASA) grading for our cohort is a limitation of this study. Medical comorbidities clearly correlate with prolonged course of hospitalization [6, 8, 42], especially with the ASA scores of 3 and 4 [12]. In addition, univariate analysis involves measurement of one variable at a time, while multivariate analysis involves multiple variable and accounts for confounding effect. Thus, univariate analysis served to determine which factors would be significant enough to be considered in the multivariate regression model. Another limitation is the retrospective nature of the data, as well as the lack of reported outcome scores, blood loss, and operative times. Although the participation of different surgeons in the study precluded the standardization of incision length or implant type, the inclusion of multiple surgeons with differing experience contributes to providing results that are reproducible in high-volume orthopedic practices. No other blood management modalities were employed in this study.
Understanding the patient and surgical factors that might serve as predictors of longer hospital stay is essential for better planning and cost-efficacy of total hip replacement procedures. Patient demographic factors that correlate with increased LOS have been reported in the literature, namely older age, female gender, medical comorbidities, poor preoperative mobility, and higher BMI. However, our data adds to other studies that failed to establish a relation between BMI and LOS after adjusting for other factors [20]. It could be explained by the fact that slimmer and frailer elderly patients who have low BMI are likely to stay in the hospital for a longer period of time. Female patients tended to stay longer in hospital than males undergoing joint replacement procedures, although this effect did not remain significant after conducting multivariate analysis. Our data showed a significant correlation between age and length of stay and confirms the current literature [8, 12, 33, 41, 43]. In addition, the data revealed that anticoagulation with heparin and/or warfarin were associated with longer hospital stay than with aspirin. Although this might be due to the fact that aspirin is easily administered orally and does not require blood testing, this is an interesting finding that warrants further investigation. Some of the results that were only significant in the univariate analysis might be accounted for by different medical comorbidities of the patients, and the lack of the American Society of Anesthesiologists (ASA) grading for our cohort is a limitation of this study. Medical comorbidities clearly correlate with prolonged course of hospitalization [6, 8, 42], especially with the ASA scores of 3 and 4 [12]. Another limitation is the retrospective nature of the data, as well as the lack of reported outcome scores and operative times.
Allogeneic blood transfusion has been associated with an increased length of stay after elective hip replacement surgery [43]. Although in some cases it might reflect complicated procedures with more blood loss and longer recovery, we failed to detect a significant association between the increased length of stay and hemoglobin drop, the number of units, or the transfusion of autologous blood. In addition, recent data suggests that the transfusion of allogeneic blood is also independently associated with significantly increased rates of upper and lower respiratory tract infections as well as wound infections [13, 32]. The association of allogeneic blood with longer hospital stay and increased complications has been attributed to immunomodulation, where allogeneic red blood cells may result in cytoskeletal changes in host red blood cells and alteration of host T cell regulation even if white blood cells are filtered out [1, 11, 39]. In addition, inherent risks of infection transmission and febrile reactions among other transfusion-related complications persist despite advances in blood safety. The elective nature of joint replacement procedures and the efficacy and safety of various available blood management modalities allow the optimization of factors that determine allogeneic transfusion risk. Preoperative hemoglobin level has been shown to be the only variable to independently predict the need for blood transfusion after primary hip or knee arthroplasty [15]. Interestingly, there was no association between the hemoglobin levels or postoperative drop in hemoglobin and LOS in our multivariate analysis. The significant association detected in this study was the transfusion of any allogeneic blood regardless of the number of units transfused. Allogeneic blood transfusion is a major predictor of a longer LOS, and it has been reported to be the best predictor of discharge around the third postoperative day. Transfusion of one or more allogeneic blood units increases the risk of staying more than 3 days after joint arthroplasty by 3-fold [20]. Implementing a blood management protocol was shown to reduce the length of stay from 6 (5–8) days to 5 (3–7) and 4 (3–6) days for total hip replacement and total knee replacement respectively (p < 0.001) [24]. The algorithm relied on preoperative optimization of Hb level with oral iron supplementation with or without erythropoietin, adhering to a transfusion threshold, and employing modalities such as tranexamic acid, hypotensive anesthesia, or cell salvage in anemic patients. In addition, the protocol decreased the rate of readmission within 90 days from 13.5 to 8.2% (p = 0.02) [24]. Since significant blood loss in joint replacement surgery can be anticipated, blood management modalities such as hypotensive anesthesia, preoperative blood salvage, and autologous blood donation in anemic patients decrease transfusion risk as well as LOS and total cost [20, 30, 36, 38].
Studies have suggested that the posterior approach in total hip is associated with longer postoperative hospitalization than the anterior approach [29]. Other data comparing the use of short versus standard femoral stems in patients less than 70 years old has reported significantly shorter mean postoperative stay for the short stem group by 2 days, resulting in 10% cost-saving per patient [40]. In addition, shorter incision lengths have shown to contribute to earlier discharge [34]. Some authors have reported increased length of stay for procedures done at the end of the week. This was attributed to the lack of physiotherapy and rehabilitation during the weekend in several institutions [8, 20]. The day of surgery did not influence the length of stay in this study except for a significant reduction when the procedure was performed on Monday. The association between poorer preoperative mobility and increased LOS stresses the importance of early and aggressive postoperative mobilization and rehabilitation. Although early aggressive rehabilitation protocols have proven effective [26, 27, 34], more research is needed to clarify this association.
The current data reveals a significant association between allogeneic blood transfusions and prolonged hospital stay after accounting for potential confounders and regardless of the number of units transfused. Although the immunomodulatory effects of allogeneic blood are not fully understood, it has been shown to independently correlate with a higher risk of postoperative infections and complications [32, 13]. Although the difference in the mean length of stay between categories of significant variables is sometimes less than half a day and may not be significant in an individual patient, it would give rise to a significant cost-saving over time. Blood management strategies such as preoperative hemoglobin optimization, selecting anemic patients for management options like preoperative autologous blood donation, and enforcing strict transfusion criteria can significantly reduce allogeneic transfusion requirements and the associated increased risk of increased hospital stay and cost of total hip arthroplasty procedures.
Electronic Supplementary Material
(PDF 1224 kb)
(PDF 1224 kb)
Acknowledgements
The authors would like to thank Dr. Michael Alexiades, Dr. Mathias Bostrom, Dr. Charles Cornell, Dr. Alejandro Della Valle, Dr. Mark Figgie, Dr. David Mayman, Dr. Douglas Padgett, Dr. Michael Parks, Dr. Amar Ranawat, Dr. Chitranjan Ranawat, Dr. Thomas Sculco, and Dr. Geoffrey Westrich for enrolling their patients in the Center for Blood Preservation at Hospital for Special Surgery, as well as Michele Prigo, EdD, CHES, the coordinator of the blood center for her help in data collection.
Disclosures
Conflict of Interest: Friedrich Boettner, MD reports personal fees from Ethicon, Ortho Development, DJ Ortho and Smith and Nephew, grants from Smith and Nephew, outside the submitted work. Jad Bou Monsef, MD has declared that he has no conflict of interest.
Human/Animal Rights:
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent:
Informed consent was obtained from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Therapeutic Study Level IV: Retrospective case series. See Levels of Evidence for a complete description.
References
- 1.Baumgartner JM, Silliman CC, Moore EE, et al. Stored red blood cell transfusion induces regulatory T cells. J Am Coll Surg. 2009;208(1):110–119. doi: 10.1016/j.jamcollsurg.2008.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bierbaum BE, Callaghan JJ, Galante JO, et al. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999;81(1):2–10. doi: 10.2106/00004623-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Boettner F, Altneu EI, Williams BA, et al. Nonanemic patients do not benefit from autologous blood donation before total hip replacement. HSS J Musculoskelet Hosp Spec Surg. 2009 doi: 10.1007/s11420-009-9145-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borghi B, Casati A. Incidence and risk factors for allogenic blood transfusion during major joint replacement using an integrated autotransfusion regimen. The Rizzoli Study Group on Orthopaedic Anaesthesia. Eur J Anaesthesiol. 2000;17(7):411–417. doi: 10.1046/j.1365-2346.2000.00693.x. [DOI] [PubMed] [Google Scholar]
- 5.Bozic KJ, Lau E, Kurtz S, et al. Patient-related risk factors for periprosthetic joint infection and postoperative mortality following total hip arthroplasty in Medicare patients. J Bone Joint Surg Am. 2012;94(9):794–800. doi: 10.2106/JBJS.K.00072. [DOI] [PubMed] [Google Scholar]
- 6.Bozic KJ, Wagie A, Naessens JM, et al. Predictors of discharge to an inpatient extended care facility after total hip or knee arthroplasty. J Arthroplast. 2006;21(6 Suppl 2):151–156. doi: 10.1016/j.arth.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 7.Callaghan JJ, Spitzer AI. Blood management and patient specific transfusion options in total joint replacement surgery. Iowa Orthop J. 2000;20:36–45. [PMC free article] [PubMed] [Google Scholar]
- 8.Dall GF, Ohly NE, Ballantyne JA, et al. The influence of pre-operative factors on the length of in-patient stay following primary total hip replacement for osteoarthritis: a multivariate analysis of 2302 patients. J Bone Joint Surg. 2009;91(4):434–440. doi: 10.1302/0301-620X.91B4.21505. [DOI] [PubMed] [Google Scholar]
- 9.Dawson-Bowling SJ, Jha S, Chettiar KK, et al. A multidisciplinary enhanced recovery programme allows discharge within two days of total hip replacement; three- to five-year results of 100 patients. Hip Int Jof Clin Exp Res Hip Pathol Ther. 2014 doi: 10.5301/hipint.5000100. [DOI] [PubMed] [Google Scholar]
- 10.Epps CD. Length stay, discharge disposition, and hospital charge predictors. AORN J. 2004;79(5):975–976. doi: 10.1016/S0001-2092(06)60729-1. [DOI] [PubMed] [Google Scholar]
- 11.Fernandez MC, Gottlieb M, Menitove JE. Blood transfusion and postoperative infection in orthopedic patients. Transfusion. 1992;32(4):318–322. doi: 10.1046/j.1537-2995.1992.32492263444.x. [DOI] [PubMed] [Google Scholar]
- 12.Foote J, Panchoo K, Blair P, et al. Length of stay following primary total hip replacement. Ann R Coll Surg Engl. 2009;91(6):500–504. doi: 10.1308/003588409X432356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Friedman R, Homering M, Holberg G, et al. Allogeneic blood transfusions and postoperative infections after total hip or knee arthroplasty. J Bone Joint Surg Am. 2014;96(4):272–278. doi: 10.2106/JBJS.L.01268. [DOI] [PubMed] [Google Scholar]
- 14.Goodnough LT, Shander A. Patient blood management. Anesthesiology. 2012;116(6):1367–1376. doi: 10.1097/ALN.0b013e318254d1a3. [DOI] [PubMed] [Google Scholar]
- 15.Guerin S, Collins C, Kapoor H, et al. Blood transfusion requirement prediction in patients undergoing primary total hip and knee arthroplasty. Transfus Med. 2007;17(1):37–43. doi: 10.1111/j.1365-3148.2006.00698.x. [DOI] [PubMed] [Google Scholar]
- 16.Hayes JH, Cleary R, Gillespie WJ, et al. Are clinical and patient assessed outcomes affected by reducing length of hospital stay for total hip arthroplasty? J Arthroplast. 2000;15(4):448–452. doi: 10.1054/arth.2000.4346. [DOI] [PubMed] [Google Scholar]
- 17.Hunt GR, Crealey G, Murthy BV, et al. The consequences of early discharge after hip arthroplasty for patient outcomes and health care costs: comparison of three centres with differing durations of stay. Clin Rehabil. 2009;23(12):1067–1077. doi: 10.1177/0269215509339000. [DOI] [PubMed] [Google Scholar]
- 18.Husted H, Hansen HC, Holm G, et al. Length of stay in total hip and knee arthroplasty in Danmark I: volume, morbidity, mortality and resource utilization. A national survey in orthopaedic departments in Denmark. Ugeskr Laeger. 2006;168(22):2139–2143. [PubMed] [Google Scholar]
- 19.Husted H, Hansen HC, Holm G, et al. What determines length of stay after total hip and knee arthroplasty? A nationwide study in Denmark. Arch Orthop Trauma Surg. 2010;130(2):263–268. doi: 10.1007/s00402-009-0940-7. [DOI] [PubMed] [Google Scholar]
- 20.Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop. 2008;79(2):168–173. doi: 10.1080/17453670710014941. [DOI] [PubMed] [Google Scholar]
- 21.Ibrahim MS, Twaij H, Giebaly DE, et al. Enhanced recovery in total hip replacement: a clinical review. Bone Joint J. 2013;95-B(12):1587–1594. doi: 10.1302/0301-620X.95B12.31303. [DOI] [PubMed] [Google Scholar]
- 22.Jacobs JJ. United States bone and joint decade: the burden of musculoskeletal diseases in the United States. American Academy of Orthopaedic Surgeons 2008.
- 23.Jans O, Jorgensen C, Kehlet H, et al. Role of preoperative anemia for risk of transfusion and postoperative morbidity in fast-track hip and knee arthroplasty. Transfusion. 2013 doi: 10.1111/trf.12332. [DOI] [PubMed] [Google Scholar]
- 24.Kotze A, Carter LA, Scally AJ. Effect of a patient blood management programme on preoperative anaemia, transfusion rate, and outcome after primary hip or knee arthroplasty: a quality improvement cycle. Br J Anaesth. 2012;108(6):943–952. doi: 10.1093/bja/aes135. [DOI] [PubMed] [Google Scholar]
- 25.Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 26.Larsen K, Hansen TB, Thomsen PB, et al. Cost-effectiveness of accelerated perioperative care and rehabilitation after total hip and knee arthroplasty. J Bone Joint Surg Am. 2009;91(4):761–772. doi: 10.2106/JBJS.G.01472. [DOI] [PubMed] [Google Scholar]
- 27.Larsen K, Sorensen OG, Hansen TB, et al. Accelerated perioperative care and rehabilitation intervention for hip and knee replacement is effective: a randomized clinical trial involving 87 patients with 3 months of follow-up. Acta Orthop. 2008;79(2):149–159. doi: 10.1080/17453670710014923. [DOI] [PubMed] [Google Scholar]
- 28.Lenssen AF, de Bie RA. Role of physiotherapy in peri-operative management in total knee and hip surgery. Injury. 2006;37(Suppl 5):S41–S43. doi: 10.1016/S0020-1383(07)70011-6. [DOI] [PubMed] [Google Scholar]
- 29.Martin CT, Pugely AJ, Gao Y, et al. A comparison of hospital length of stay and short-term morbidity between the anterior and the posterior approaches to total hip arthroplasty. J Arthroplast. 2013;28(5):849–854. doi: 10.1016/j.arth.2012.10.029. [DOI] [PubMed] [Google Scholar]
- 30.Martinez V, Monsaingeon-Lion A, Cherif K, et al. Transfusion strategy for primary knee and hip arthroplasty: impact of an algorithm to lower transfusion rates and hospital costs. Br J Anaesth. 2007;99(6):794–800. doi: 10.1093/bja/aem266. [DOI] [PubMed] [Google Scholar]
- 31.Moller AM, Pedersen T, Villebro N, et al. Effect of smoking on early complications after elective orthopaedic surgery. J Bone Joint Surg. 2003;85(2):178–181. doi: 10.1302/0301-620X.85B2.13717. [DOI] [PubMed] [Google Scholar]
- 32.Newman ET, Watters TS, Lewis JS, et al. Impact of perioperative allogeneic and autologous blood transfusion on acute wound infection following total knee and total hip arthroplasty. J Bone Joint Surg Am. 2014;96(4):279–284. doi: 10.2106/JBJS.L.01041. [DOI] [PubMed] [Google Scholar]
- 33.Oldmeadow LB, McBurney H, Robertson VJ. Predicting risk of extended inpatient rehabilitation after hip or knee arthroplasty. J Arthroplast. 2003;18(6):775–779. doi: 10.1016/S0883-5403(03)00151-7. [DOI] [PubMed] [Google Scholar]
- 34.Peck CN, Foster A, McLauchlan GJ. Reducing incision length or intensifying rehabilitation: what makes the difference to length of stay in total hip replacement in a UK setting? Int Orthop. 2006;30(5):395–398. doi: 10.1007/s00264-006-0091-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peters CL, Shirley B, Erickson J. The effect of a new multimodal perioperative anesthetic regimen on postoperative pain, side effects, rehabilitation, and length of hospital stay after total joint arthroplasty. J Arthroplast. 2006;21(6 Suppl 2):132–138. doi: 10.1016/j.arth.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 36.Rosencher N, Kerkkamp HE, Macheras G, et al. Orthopedic Surgery Transfusion Hemoglobin European Overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion. 2003;43(4):459–469. doi: 10.1046/j.1537-2995.2003.00348.x. [DOI] [PubMed] [Google Scholar]
- 37.Sigurdsson E, Siggeirsdottir K, Jonsson H, Jr, et al. Early discharge and home intervention reduces unit costs after total hip replacement: results of a cost analysis in a randomized study. Int J Health Care Finance Econ. 2008;8(3):181–192. doi: 10.1007/s10754-008-9036-0. [DOI] [PubMed] [Google Scholar]
- 38.Spahn DR. Anemia and patient blood management in hip and knee surgery: a systematic review of the literature. Anesthesiology. 2010;113(2):482–495. doi: 10.1097/ALN.0b013e3181e08e97. [DOI] [PubMed] [Google Scholar]
- 39.Sparrow RL. Red blood cell storage and transfusion-related immunomodulation. Blood Transfus Trasfusione Sangue. 2010;8(Suppl 3):s26–s30. doi: 10.2450/2010.005S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tahim AS, Stokes OM, Vedi V. The effect of femoral stem length on duration of hospital stay. Hip Int Jof Clin Exp Res Hip Pathol Ther. 2012;22(1):56–61. doi: 10.5301/HIP.2012.9035. [DOI] [PubMed] [Google Scholar]
- 41.Vincent HK, Alfano AP, Lee L, et al. Sex and age effects on outcomes of total hip arthroplasty after inpatient rehabilitation. Arch Phys Med Rehabil. 2006;87(4):461–467. doi: 10.1016/j.apmr.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 42.Wang T, Ackland T, Hall S, et al. Functional recovery and timing of hospital discharge after primary total hip arthroplasty. Aust N Z J Surg. 1998;68(8):580–583. doi: 10.1111/j.1445-2197.1998.tb02104.x. [DOI] [PubMed] [Google Scholar]
- 43.Weber EW, Slappendel R, Prins MH, et al. Perioperative blood transfusions and delayed wound healing after hip replacement surgery: effects on duration of hospitalization. Anesth Analg. 2005;100(5):1416–1421. doi: 10.1213/01.ANE.0000150610.44631.9D. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)