Introduction
Osteoid osteoma is a painful, benign bony tumor affecting a predominantly young patient population, with 60% occurring between ages 10 and 20 years old and a male predominance [19]. Nocturnal and rest pain are hallmarks. Symptoms vary from a mild ache to severe debilitating pain in response to excessive prostaglandin production. As such, the pain is classically responsive to aspirin due to its anti-prostaglandin effect [13]. Localized swelling and tenderness may be present on examination. Radiographically, osteoid osteoma is traditionally described as a 1–2-cm radiolucent lesion with a sclerotic border and central nidus consisting of vascular osteoid with focal mineralization. Imaging modalities including radiographs, bone scan, CT, and MRI can be helpful in the diagnosis of osteoid osteoma.
Jaffe [11] first described osteoid osteoma in 1935 in five patients with “localized osteomyelitis or bone abscess” with a “nidus-like focus” of osteoid and vascularity without histologic evidence of infection. Excision resulted in symptomatic resolution in all cases. Others have since reported on osteoid osteomas scattered across the skeleton, with 6–13% occurring in the hand and 1–2% specifically occurring in the carpus [4, 5]. Lesions may be intra-articular or extra-articular, intramedullary, subperiosteal, or intracortical, the latter of which is most readily visualized on radiographs.
Accurate and timely diagnosis is reliant upon a high index of suspicion. Osteoid osteoma in the carpus may be difficult to visualize on radiographs. Initial symptoms can be confused for osteomyelitis, De Quervain’s tenosynovitis, carpal tunnel syndrome, recent minor trauma, arthritis, neuroma, or, as in the case presented here, complex regional pain syndrome (CRPS) [2, 8]. Furthermore, as described herein, a missed or delayed osteoid osteoma diagnosis can lead to an unnecessary battery of tests, a litany of failed surgeries, and severely impaired quality of life.
Case Report
In August 2006, a 16-year-old, athletic, left-hand dominant male presented with atraumatic, insidious onset left wrist pain. An initial MRI reported a cyst within the trapezoid and nonspecific triquetral marrow changes. Cast immobilization and physical therapy offered no relief. Repeat MRI, seven months later, showed dorsal soft tissue thickening and led to a diagnosis of triquetral impingement ligament tear (TILT) syndrome [22]. He underwent dorsal limited synovectomy, curettage, and bone grafting of the so-called trapezoid cyst. Radiographs 1 year later showed bony excrescences dorsal to the triquetrum. A second surgeon performed excision of a triquetral bone spur and scar revision. Postoperatively, his symptoms worsened leading to a presumptive diagnosis of “causalgia.” A “dystrophile” [21] therapy program was continued for 9 months without improvement.
The patient, now a college freshman, was plagued by chronic pain and disability leading to his withdrawal from all athletic endeavors. A third doctor performed an extensive rheumatologic and infectious workup that was negative. MRI scans of the cervical spine, brachial plexus, and left wrist were all negative or inconclusive. He was diagnosed with CRPS. NSAIDs, neuroleptics, stellate ganglion block, topical capsaicin, lidocaine patches, and biofeedback therapy were all attempted by a pain management physician, but proved ineffective.
Upon presentation to our office in February of 2009, the patient had a radiocarpal effusion, ulnar wrist tenderness, and limited wrist ROM (30° extension, 30° flexion). Radiographs in February 2009 (Fig. 1) showed disuse osteoporosis and small bony fragments in the soft tissues dorsal to the carpus. In view of the history of curettage and packing of a triquetral cyst, the radiographic findings were interpreted as being due to postoperative change. Ultrasound-guided aspirations along with corticosteroid and local anesthetic injections were performed in April and November of 2009. The initial aspiration obtained 2 ml of yellow-tinged fluid, which was negative for infection or crystals. In August of 2010, an MRI of the wrist was performed due to persistent pain despite temporary relief from the injections and showed synovitis (most prominent dorsally) with bone marrow edema in the lunate, triquetrum, hamate, and capitate (Fig. 2). Small foci low signal was present dorsally and interpreted as either postoperative changes or calcium pyrophosphate or calcium hydroxyapatite deposition. A third ultrasound-guided aspiration and injection was performed in August of 2010, which was again negative for crystals and infection and provided temporary symptomatic relief. Based on clinical evaluation, a CT scan was ordered in September of 2010 with clinical information stating to rule out osteoid osteoma. The CT demonstrated a round radiolucency in the dorsal-radial aspect of the triquetrum measuring 7 mm in diameter with dense bone fragments incorporated within it (Fig. 3). There was partial fusion of the lunate and triquetrum. The findings were interpreted as compatible with an osteoid osteoma, although not absolutely diagnostic given postsurgical changes. A three-phase bone scan with technetium 99m methylene diphosphonate was performed to confirm the diagnosis of osteoid osteoma (Fig. 4). The bone scan showed a round focal area of increased blood flow, blood pool, and uptake in the region of the triquetrum (corresponding to the lesion seen on CT, Fig. 3). This pattern is typical of an osteoid osteoma and can be differentiated from inflammatory arthritis or CRPS, which would show diffuse (as opposed to focal) increased uptake.
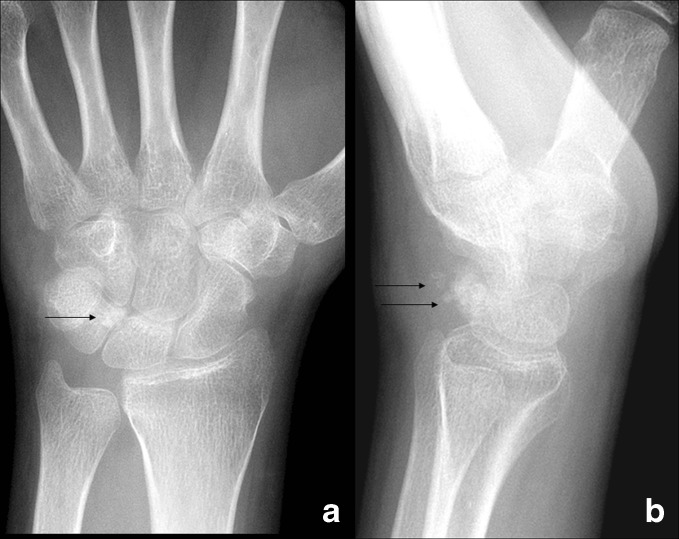
Fig. 1.
Radiographs of the left wrist from February of 2009 show osteoporosis. On the PA view (a), there is a faint area of sclerosis in the radial aspect of the triquetrum (arrow). On the lateral view (b), bone fragments in the soft tissues and bony excrescences (arrows) are present dorsally.
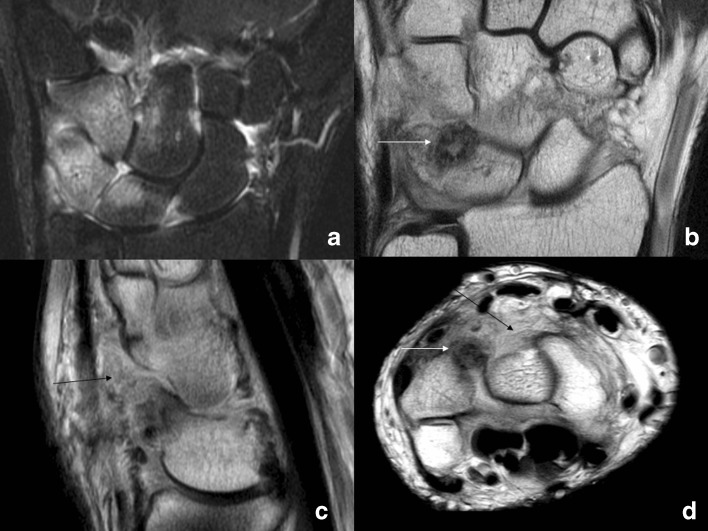
Fig. 2.
MRI of the left wrist performed in August of 2010. a On the coronal STIR, there is bone marrow edema in the lunate, triquetrum, hamate, and capitate, as well as synovitis in the radiocarpal, midcarpal, and carpometacarpal joints. The coronal (b), sagittal (c), and axial (d) proton density images show a round area of decreased signal (white arrows) in the dorsal aspect of the triquetrum corresponding to the “cyst” that had been curetted and grafted previously. There is synovial thickening (black arrows) in the soft tissues dorsally.
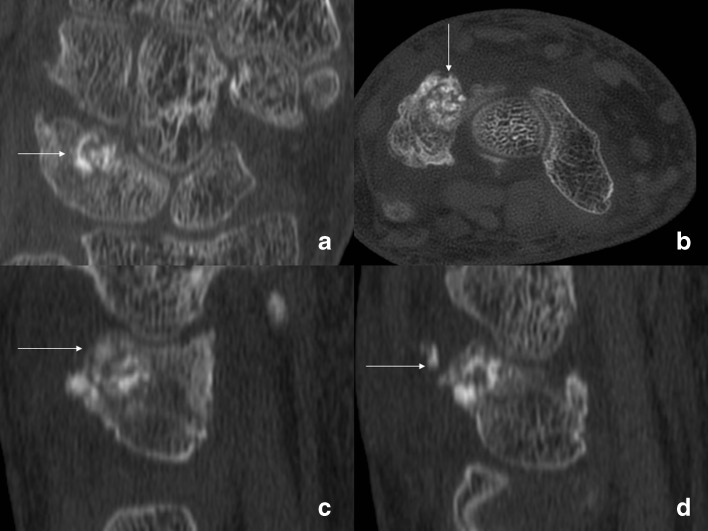
Fig. 3.
CT of the left wrist performed in September of 2010. The coronal (a), axial (b), and sagittal images (c, d) show a round lesion in the dorsal aspect of the triquetrum packed with incorporated bone graft (arrows) with some graft in the soft tissues dorsally. Fusion of the triquetrum and lunate is seen on the coronal view (a).
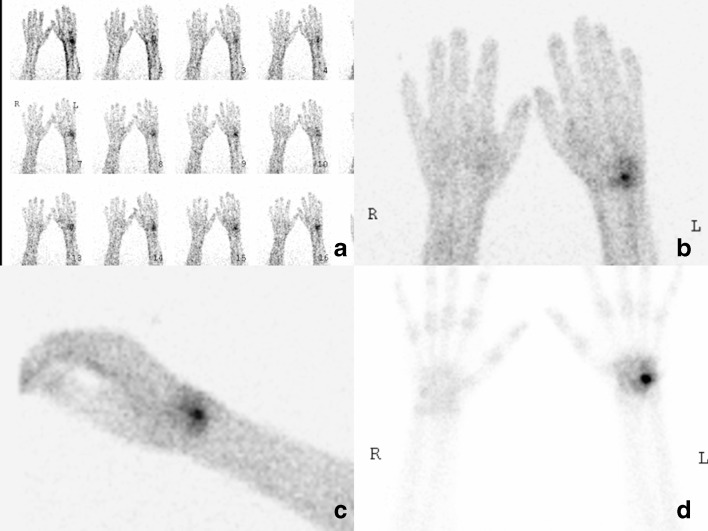
Fig. 4.
Three-phase bone scan of the wrists and hands performed in 2010. The intravenous injection of technetium 99m MPD was done in the right elbow. On the dynamic flow study (a), there is increased flow to the left wrist. The blood pool scans (b, c) show focal increased blood pool in the ulnar and dorsal aspects of the wrist around the left triquetrum. The delayed static image (d) shows a round focal area of high uptake in the left triquetrum typical of an osteoid osteoma. There is mild surrounding increased uptake consistent with synovitis. There is no diffuse periarticular uptake suggestive of CRPS.
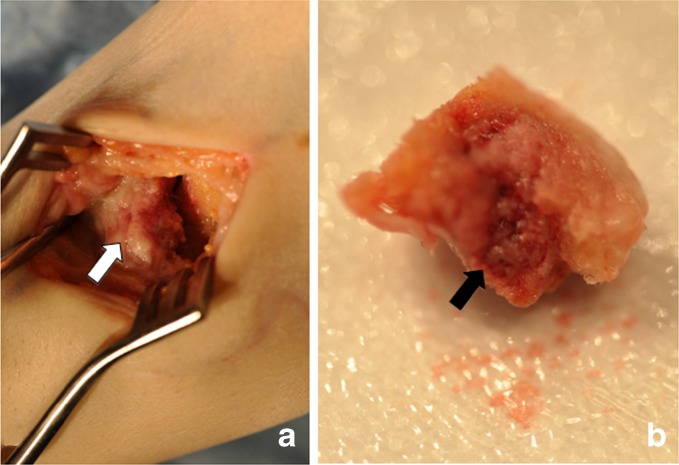
A triquetral osteoid osteoma was diagnosed 4 years after initial presentation. On November 18, 2010, the patient was taken to the operating room for excision. Antibiotics were held for intraoperative cultures, which were ultimately negative. A 4.5-cm dorsal wrist incision over the triquetrum and in line with the fourth way was made. Intraoperative findings included abundant synovitis, lunate-triquetral fusion, and erosions of the dorsal hamate and capitate (Fig. 5a). The triquetral lesion was hyperemic with surrounding pale, yellow tissue (Fig. 5b). Intraoperative frozen section and final histopathologic evaluation confirmed osteoid osteoma with cellular osteoblastic tissue, containing a focally hemorrhagic vascular nidus, with variably dense regions of bone composed of woven matrix.
Fig. 5.
Intraoperative photo (a) viewed through a dorsal approach showing the synostosis between the lunate and triquetrum (white arrow). Gross specimen removed (b) shows the central red hyperemic nidus with surrounding pale yellow tissue (black arrow).
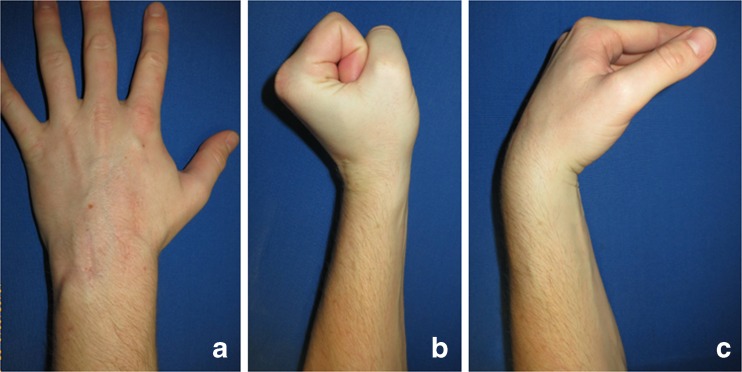
Immediate symptomatic relief was noted. By 4 months postoperatively, he had returned to all activities and continued to be asymptomatic at 2-year follow-up. Patient-rated wrist evaluation (PRWE) and disabilities of the arm, shoulder, and hand (DASH) scores were 1 and 1.67, respectively, at 2 years. Passive extension and flexion were 60 and 35°, respectively, compared to 80 and 70° on the contralateral side. Pronation, supination, grip strength, and pinch strength were symmetric bilaterally (Fig. 6).
Fig. 6.
Clinical photographs of the patient at 1-year follow-up show a well-healed dorsal incision (a), as well as excellent wrist extension and flexion (b, c).
Discussion
Osteoid osteoma can be difficult to diagnose due to its variable symptomatology, anatomic distribution, and radiographic manifestations. There are numerous reports of delayed diagnosis of osteoid osteoma in the literature resulting in unnecessary treatments and procedures. Few reports, however, exist about carpal osteoid osteoma. Murray et al. [17] identified 44 primary carpal neoplasms in a series of 26,800 primary bone tumors at the Mayo Clinic between 1909 and 1992, of which osteoid osteoma was the leading diagnosis (11 out of 44) and most commonly found in the scaphoid and capitate [17]. In this series, one osteoid osteoma of the triquetrum was noted. Bednar and colleagues [1] retrospectively reviewed the cases of 46 patients with histologically confirmed osteoid osteoma of the upper extremity over a 43-year time period and found only 6 within the carpus (4 scaphoid and 2 capitate). From the time of initial presentation, diagnosis took an average of 15 months. Imaging diagnosis was made based on radiographs in 76% of patients. Additional imaging modalities were required in the remaining 24% of patients including bone scan and/or computed tomography. Osteoid osteoma has been reported in each carpal bone previously [17]. Three reports of triquetral osteoid osteoma have been published with delayed diagnoses in each case (2 to 6 years) [10, 18]. Delayed or missed diagnosis is particularly common in the hand and wrist given the relative infrequency and variable imaging appearance. The classical radiographic appearance of osteoid osteoma is frequently not observed in carpal bones given their small size and irregular shapes. Furthermore, delayed appearance of osteoid osteoma lesions on imaging has been reported for up to 3 years after symptom onset [8]. Hartmann et al [8] published the dramatic case of a 44-year-old man with unremitting posttraumatic pain after minor injury. Conservative measures failed, as did digital nerve neurolysis. The patient was diagnosed with CRPS and ineffectively treated with repeat stellate ganglion blocks and a continuous brachial plexus catheter to block sensory afferents. The patient had several exploratory procedures over the next 3 years and even underwent an endoscopic thoracic sympathectomy. He became depressed, even suicidal, reportedly “demanding amputation.” Repeat CT imaging showed evidence of a small finger proximal phalanx osteoid osteoma. Following surgical excision and ablation, his symptoms resolved and ultimately he was able to return to work. This report, and one by Martorell in 1964 [16], are the only other reports of osteoid osteoma in the hand or wrist presenting as CRPS.
Katolik et al. [12] reported in 2009 on a 16-year-old girl with nearly 2 years of atraumatic right wrist and hand pain relieved with anti-inflammatory drugs. MRI was suggestive of osteomyelitis in the scaphoid, in addition to monoarticular radiocarpal arthritis, and led to open intralesional curettage. Intraoperative cultures were negative, but final pathology demonstrated osteoid osteoma. This case highlights not only the limitations of imaging modalities in diagnosing carpal osteoid osteoma, but also was the first report of carpal osteoid osteoma presenting as degenerative monoarticular arthritis. Our case is the first report of intercarpal (i.e., lunate-triquetral) arthritis and fusion, as part of the carpal osteoid osteoma complex.
Bone scan is a powerful tool for localizing an osteoid osteoma. Helms et al. [9] evaluated the efficacy of bone scan for a diagnosis of osteoid osteoma and described the “double-density sign”—a very hot central lesion with surrounding mild radionuclide uptake. This imaging characteristic is produced by the differential radionuclide uptake by the central vascular nidus and surrounding reactive tissue. Furthermore, in our case, bone scan served as a powerful tool to not only diagnose osteoid osteoma, but also differentiate from CRPS. Bottner [3] appreciated the diagnostic utility of bone scan, but stated that preoperative bone scan is not always necessary and that CT can more readily differentiate between osteoid osteoma and other pathologic processes such as Brodie’s abscess. CT is more sensitive (89%) than MRI (67%) for osteoid osteoma and found to “more precisely localize the nidus,” facilitating surgical localization and planning [9, 20]. The efficacy of CT can be further enhanced with the use of contrast to illuminate the vascular nidus [14]. More recently, Farid et al. [7] suggested the use of SPECT-CT to amplify the presence of the nidus and improve accuracy of osteoid osteoma diagnosis.
While MRI is a powerful diagnostic tool, findings in the setting of osteoid osteoma may be inaccurate or misleading. It is less sensitive than CT and can overestimate the aggressiveness of a lesion. Davies et al. [6] retrospectively reviewed [15] 43 patients with osteoid osteoma and found that the correct diagnosis was only made in 65% of patients. Twenty-one percent of lesions had a “poorly visualized” nidus, and 14% of lesions had no visualized nidus. They concluded that there is a substantial risk of missed diagnosis based on MRI alone. Although MRI has been found to be less sensitive and can overestimate the aggressiveness of a lesion, with increased spatial resolution techniques and a high clinical suspicion, MR imaging may be just as accurate [15].
In conclusion, early and accurate diagnosis of osteoid osteoma requires a high index of clinical suspicion in the hand and wrist given the relative infrequency and potential limitations of advanced imaging modalities. Bone scan and CT aid in the diagnosis of osteoid osteoma with CT being particularly helpful for surgical planning and visualization of the central nidus. MRI is less sensitive and can overestimate the aggressiveness of a lesion. Once identified, even on a delayed basis, surgical excision is curative and usually results in complete symptom resolution. However, given the potential morbidity of delayed or incorrect diagnoses as seen in the case presented (i.e., functional disability, withdrawal from athletics, unnecessary procedures, arthritis), osteoid osteoma must be considered in the differential for patients with hand and wrist pain. This case is the first to document intercarpal arthritis as a presenting finding of carpal osteoid osteoma, as well as one of the first to document osteoid osteoma in the triquetrum and CRPS as a presenting symptom of upper extremity osteoid osteoma.
Electronic supplementary material
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
Disclosures
ᅟ
Conflict of Interest:
Samuel A. Taylor MD, Samir K. Trehan, MD, Keith M. Crivello, MD, and Robert Schneider, MD have declared that they have no conflict of interest. Scott W. Wolfe, MD is a paid consultant for Extremity Medical Inc; receives payment for lectures including service on speakers bureaus from TriMed, Inc., SBI, Inc. and Extremity Medical, Inc.; receives royalties from Extremity Medical, Inc. and Elsevier, Inc.; patent with Extremity Medical, Inc., outside the work.
Human/Animal Rights:
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent:
Informed consent was waived from all patients for being included in the study.
Required Author Forms Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Worked performed at the Hand Surgery Service, Hospital for Special Surgery, New York, New York.
References
- 1.Bednar MS, McCormack RR, Jr, Glasser D, Weiland AJ. Osteoid osteoma of the upper extremity. J Hand Surg [Am] 1993;6:1019–1025. doi: 10.1016/0363-5023(93)90395-J. [DOI] [PubMed] [Google Scholar]
- 2.Bostan B, Sen C, Gunes T, Erdem M, Koseoglu RD. Osteoid osteoma of the trapezium: case report. J Hand Surg [Am] 2010;4:636–638. doi: 10.1016/j.jhsa.2009.12.032. [DOI] [PubMed] [Google Scholar]
- 3.Bottner F, Wortler K, Link T. Osteoid osteoma. J Bone Joint Surg (Br) 2000;2:306–307. [PubMed] [Google Scholar]
- 4.Campanacci M, Ruggieri P, Gasbarrini A, Ferraro A, Campanacci L. Osteoid osteoma. Direct visual identification and intralesional excision of the nidus with minimal removal of bone. J Bone Joint Surg (Br) 1999;5:814–820. doi: 10.1302/0301-620X.81B5.9313. [DOI] [PubMed] [Google Scholar]
- 5.Chamberlain BC, Mosher JF, Levinsohn EM, Greenberg JA. Subperiosteal osteoid osteoma of the hamate: a case report. J Hand Surg [Am] 1992;3:462–465. doi: 10.1016/0363-5023(92)90350-X. [DOI] [PubMed] [Google Scholar]
- 6.Davies M, Cassar-Pullicino VN, Davies AM, McCall IW, Tyrrell PN. The diagnostic accuracy of MR imaging in osteoid osteoma. Skelet Radiol. 2002;10:559–569. doi: 10.1007/s00256-002-0546-4. [DOI] [PubMed] [Google Scholar]
- 7.Farid K, El-Deeb G, Caillat Vigneron N. SPECT-CT improves scintigraphic accuracy of osteoid osteoma diagnosis. Clin Nucl Med. 2010;3:170–171. doi: 10.1097/RLU.0b013e3181cc648f. [DOI] [PubMed] [Google Scholar]
- 8.Hartmann T, Preis C, Gabriel A, Rath T, Ilias W. An osteoid osteoma as an undiagnosed cause of three years of severe pain. Anesth Analg. 1997;6:1344–1345. doi: 10.1097/00000539-199712000-00029. [DOI] [PubMed] [Google Scholar]
- 9.Helms CA. Osteoid osteoma. The double density sign. Clin Orthop Relat Res. 1987;222:167–173. [PubMed] [Google Scholar]
- 10.Herzberg G, Baaklini M, Al Saati M, Izem Y. Intra-articular sub-periosteal osteoid osteoma of the triquetrum. Case report. Chir Main. 2010;5:332–334. doi: 10.1016/j.main.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 11.JAFFE HL. Osteoid-osteoma. Proc R Soc Med. 1953;12:1007–1012. [PMC free article] [PubMed] [Google Scholar]
- 12.Katolik LI. Osteoid osteoma of the scaphoid presenting with radiocarpal arthritis: a case report. Hand (N Y) 2009;2:187–190. doi: 10.1007/s11552-008-9159-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kneisl JS, Simon MA. Medical management compared with operative treatment for osteoid-osteoma. J Bone Joint Surg Am. 1992;2:179–185. [PubMed] [Google Scholar]
- 14.Levine E, Neff JR. Dynamic computed tomography scanning of benign bone lesions: preliminary results. Skelet Radiol. 1983;4:238–245. doi: 10.1007/BF00354124. [DOI] [PubMed] [Google Scholar]
- 15.Liu PT, Chivers FS, Roberts CC, Schultz CJ, Beauchamp CP. Imaging of osteoid osteoma with dynamic gadolinium-enhanced MR imaging. Radiology. 2003;3:691–700. doi: 10.1148/radiol.2273020111. [DOI] [PubMed] [Google Scholar]
- 16.Martorell F. Sudeck's atrophy due to osteoid osteoma of the carpal navicular. Angiologia. 1964; 170–172. [PubMed]
- 17.Murray PM, Berger RA, Inwards CY. Primary neoplasms of the carpal bones. J Hand Surg [Am] 1999;5:1008–1013. doi: 10.1053/jhsu.1999.1008. [DOI] [PubMed] [Google Scholar]
- 18.Olmedo-Garcia N, Lopez-Prats F. Tetracycline fluorescence for the peroperative localization of osteoid osteoma of the triquetrum. Acta Orthop Belg. 2002;3:306–309. [PubMed] [Google Scholar]
- 19.Orthopaedic Surgery Essentials: Oncology and Basic Science. Lippincott Williams & Wilkins; 2007.
- 20.Shukla S, Clarke AW, Saifuddin A. Imaging features of foot osteoid osteoma. Skelet Radiol. 2010;7:683–689. doi: 10.1007/s00256-009-0737-3. [DOI] [PubMed] [Google Scholar]
- 21.Watson HK, Fong D. Dystrophy, recurrence, and salvage procedures in dupuytren's contracture. Hand Clin. 1991;4:745–755. [PubMed] [Google Scholar]
- 22.Watson HK, Weinzweig J. Triquetral impingement ligament tear (tilt) J Hand Surg (Br) 1999;3:321–324. doi: 10.1054/jhsb.1999.0070. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)