Abstract
Purpose
The purpose of this study was to retrospectively compare and review the clinical outcomes between the distal clavicular locking plate and clavicular hook plates in the treatment of unstable distal clavicle fractures; moreover, the relevant literature of the two fixation methods was reviewed systematically to identify the non-union, complications, or functional scores, according to the treatment methods and determine which treatment method is better.
Methods
Sixty-six patients with 66 unstable distal clavicle fractures who underwent open reduction and internal fixation with either a distal clavicular locking plate (36 patients) or a clavicular hook plate (30 patients ) were evaluated. The main outcome comparisons included Constant score, rate of non-union, rate of complication, and rate of returning to work three months postoperatively.
Results
No significant difference was found between locking plate and hook plate groups in union rate and Constant score (P > 0.05). However, the results indicated that the distal clavicular locking plate group had a significantly lower rate of complications (P < 0.05) and symptomatic hardware (P < 0.05). In addition, the distal clavicular locking plate facilitated the return to work better than the clavicular hook plate (P < 0.05).
Conclusions
Both distal clavicular locking plate and clavicular hook plate achieved good results in the treatment of unstable distal clavicle fractures; however, internal fixation with a distal clavicular locking plate had greater ability to return to their previous work after surgery in three months and fewer complications than the clavicular hook plate.
Keywords: Distal clavicle fractures, Hook plate, Locking plate
Introduction
Lateral clavicle fractures are a rare entity, accounting for approximately 15 %–25 % of all clavicle fractures [1, 2]. The treatment of distal clavicle fractures depends on the classification of the fracture. Today, there is a wide variety of surgical techniques for the treatment for these fractures. If surgery of distal clavicle fractures is indicated, many implants or surgical methods are available, including Kirschner wires [3], coracoclavicular screw fixation [4, 5], hook plate fixation [6–13], or locking plate fixation [14–20]. Although there are many types of operative procedures, no procedures are considered to be the gold standard treatment. The optimal treatment of unstable distal clavicle fractures is still controversially discussed in the literature. Unstable distal clavicle fractures often require open reduction and internal fixation. Most studies report using hook plate and locking plate on a small number of cases, as incidence of this specific injury is low. Comparison of data found in published literature remains difficult, since most studies do not focus on comparison between the treatment of hook plate and locking plate. The present study retrospectively compared the clinical outcomes of the two surgical methods, either hook plate or locking plate in patients of unstable distal clavicle fractures, to evaluate any differences with regard to method of fixation, non-union, complications, or functional scores. Furthermore, the relevant literature of the two fixation methods was reviewed systematically, to identify the non-union, complications, or functional scores, according to the treatment methods and determine which treatment method is better. We hypothesized which is the best construct for fixation of distal clavicle fractures: locking plate or hook plate?
Materials and methods
This study was approved by the Ethics Committee of our institute. Informed consent was obtained from all patients.
Using our trauma database, we identified 73 patients who were treated between February 2007 and November 2010 for unstable distal clavicle fractures. Inclusion criteria for this study were: (a) acute fractures, (b) Neer type II fractures, (c) internal fixation with either distal clavicular locking or clavicular hook plates, and (d) normal shoulder function before injury. There were 73 patients who met the inclusion criteria; however, seven patients could not be followed and were excluded. Therefore, 66 patients were included in this study. We performed a retrospective cohort study with a prospective evaluation and comparison for two different groups of patients: 36 patients who underwent fixation of distal clavicular locking plate and 30 patients who received fixation of clavicular hook plate. All patients were examined with standard radiographs and clinical outcomes. Prospective database records and individual patient charts were reviewed to obtain surgical data, including the rate of nonunion and complications. Radiographs and functional evaluation from the postoperative and follow-up periods were reviewed for evidence of Constant score, rate of non-union, rate of complication, and rate of returning to work three months postoperatively.
Surgical procedure
The treating surgeon determined the fixation method according to the fracture’s condition. The more comminuted fractures which were close to the acromioclavicular joint were treated with hook plate while repairing ligament. The displaced distal clavicle fractures with a less severe injury of coracoclavicular ligament and the fracture fragment was bigger than 2 cm from the X-ray photograph were treated by locking plate.
Hook plate group
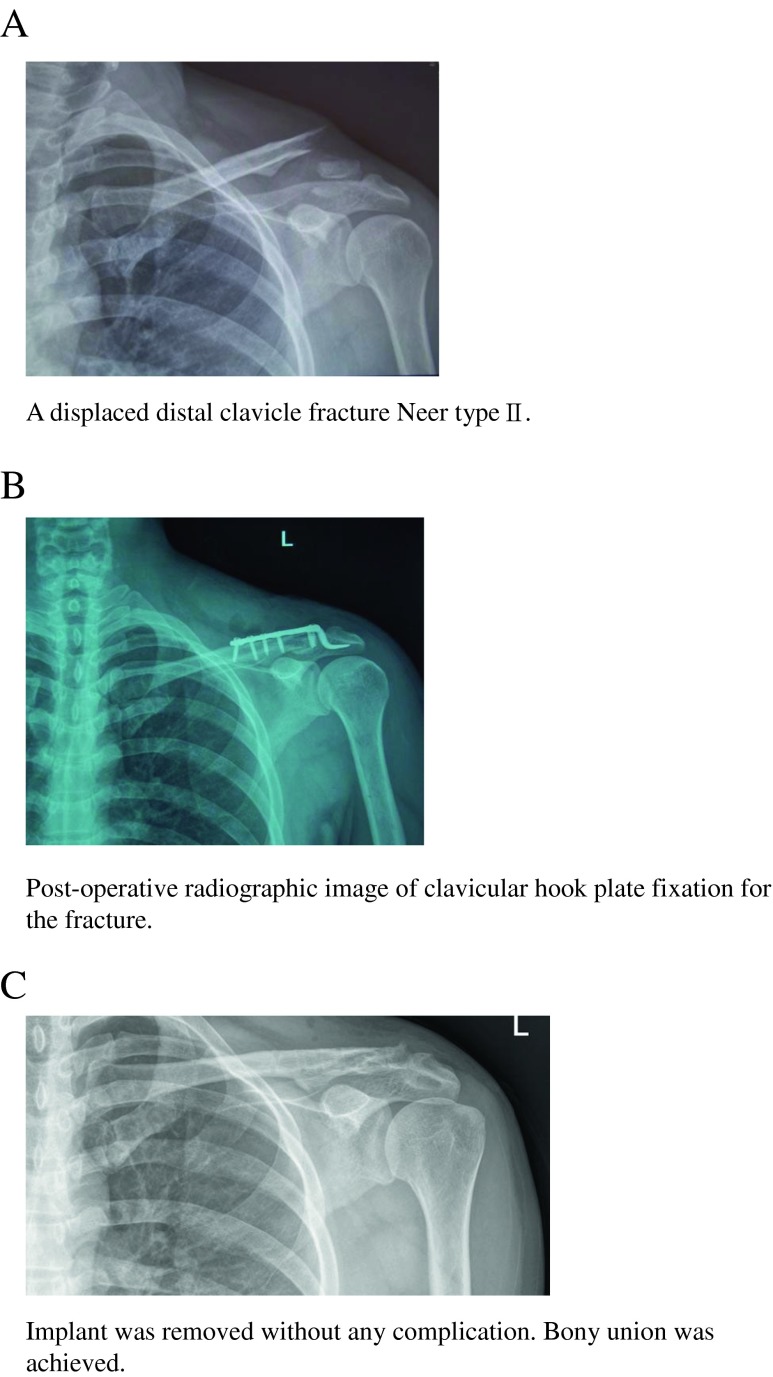
After general anaesthesia was administered, the patient was placed in the beach chair position. In the clavicular hook plate group, a standard anterior approach to the clavicle was performed. The fracture was exposed and reduced under direct visualization. A tunnel was made in the subacromial space posterior to the acromioclavicular joint and the hook was inserted into this tunnel. If necessary, the plate was bent to fit the shape of the clavicle (Fig. 1a).
Fig. 1.
a A displaced distal clavicle fracture Neer type II. b Postoperative radiographic image of clavicular hook plate fixation for the fracture. c Implant was removed without any complication. Bony union was achieved
Locking plate group
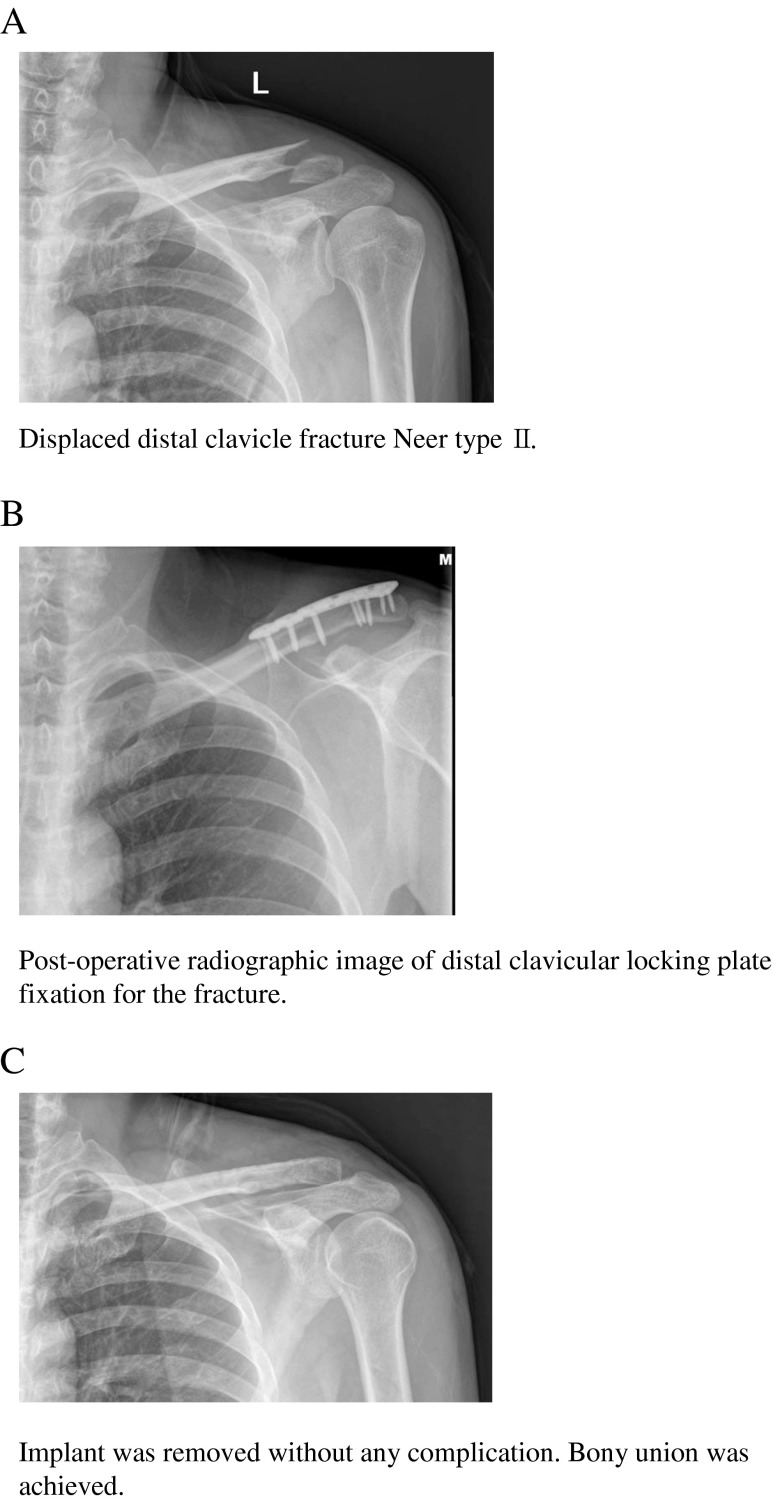
In the distal clavicular locking plate group, with the patient in the beach chair position, a standard anterior approach to the clavicle was normally used. The fracture was reduced under direct visualization and the initial reduction was held with Kirschner wires while the locking plate was applied. Then, the distal clavicular locking plates were placed on the reduced clavicular fracture with the maximum number of locking screws incorporated into the distal fragment (Fig. 2a). In all circumstances, care was taken not to violate or span the acromioclavicular joint during locking plate fixation.
Fig. 2.
a Displaced distal clavicle fracture Neer type II. b Postoperative radiographic image of distal clavicular locking plate fixation for the fracture. c The implant was removed without any complication. Bony union was achieved
Postoperative management
In the two groups, the operated shoulder was protected with a sling allowing for range of motion (ROM) exercises. Mobilization was started as soon as possible and full range of motion was usually achieved after three to four weeks. Heavy manual work was not allowed until the fracture union was confirmed by radiographs.
Clinical assessment
All patients had clinical follow-up and radiographs at four, eight, and 12 weeks, six months, one year (Figs. 1b, 2b), and then annually thereafter. During follow-up, radiographs were used to assess fracture union. Standard radiographs (anteroposterior view, AP view) were obtained for all 66 patients. These radiographs were examined for evidence of fracture healing and implant position. Shoulder function was evaluated using the Constant-Murley score at the last follow-up [21]. In this system, subjective and objective clinical data were included, with a maximum score of 100 points. Pain (15 points), activities of daily living (20 points), range of motion (ROM) of the shoulders (40 points), and muscle power (25 points) were evaluated. Hook plates were routinely removed at a planned second surgery (Fig. 1c), whereas the locking plate was only removed if requested by the patient or it became symptomatic after fracture union (Fig. 2c).
Statistical analysis
Statistical analysis was performed using SPSS 13.0 (SPSS Inc., Chicago, IL, USA). Differences between the distal clavicular locking and clavicular hook plate groups were compared using an independent t-test and chi-square test. Statistical significance was defined as 0.05, and a p-value < 0.05 was taken to indicate a statistically significant difference.
Results
A summary of the patients’ profiles and results is shown in Table 1. The distal clavicular locking plate group included 36 patients with an average age of 42.5 years. Twenty-nine patients (80.6 %) had vehicular trauma, five patients (13.9 %) had a fall and two patients (5.6 %) had a fall from height. The clavicular hook plate group included 30 patients with an average age of 41.1 years. Twenty-two patients (73.3 %) had vehicular trauma, four patients (13.3 %) had a fall, one patient (3.3 %) had a fall from height, and three patients (10.0 %) had an injury during sports. Both groups were similar with respect to age, gender, and confounding medical conditions (P > 0.05). The average clinical follow-up was 28.6 and 27.2 months in the distal clavicular locking plate and clavicular hook plate groups, respectively (P > 0.05). The mean time of bone union was 3.5 months (three to six months) and 3.8 months (three to six months) in the distal clavicular locking plate and clavicular hook plate groups, respectively (P > 0.05). In the distal clavicular locking plate group, all but one fracture (97.2 %) healed in six months. In the clavicular hook plate group, all but two fractures (93.3 %) healed in six months. There was no difference in the union rate between the locking plate (97.2 %) and hook plate (93.3 %) groups (P > 0.05). The mean time of implant removal was 7.1 months (six to 12 months) and 6.5 months (six to ten months) in the distal clavicular locking plate and clavicular hook plate groups, respectively (P > 0.05). The mean Constant scores were 95.5 and 93.3 points in the distal clavicular locking and clavicular hook plate groups, respectively. The mean Constant scores between the involved shoulder in the two groups were not different (P > 0.05). The distal clavicular locking plate group had two complications (5.6 %), including one partial loss of reduction and one non-union in six months. Complications occurred in seven patients (23.3 %) in the clavicular hook plate group, and consisted of two partial losses of reduction, three patients with symptomatic hardware, one non-union in six months, and one hardware failure. Overall, 23.3 % of complications occurred in the clavicular hook plate group compared with 5.6 % in the distal clavicular locking plate group. Clearly, the distal clavicular locking plate group had fewer complications than the clavicular hook plate group (P < 0.05). In the distal clavicular locking plate group, all but two patients (94.4 %) returned to their previous work three months postoperatively. In the clavicular hook plate group, 22 patients (73.3 %) returned to their previous work three months postoperatively. There was a significant difference in returning to work between the distal clavicular locking and clavicular hook plate groups (P < 0.05).
Table 1.
Patient profiles and clinical results
| Variables | Locking plate group | Hook plate group | P-value |
|---|---|---|---|
| Age (yr) | 42.5 ± 10.7 | 41.1 ± 10.3 | 0.46 |
| Gender | |||
| Male | 20 (55.6 %) | 17 (56.7 %) | 0.93 |
| Female | 16 (44.4 %) | 13 (43.3 %) | 0.93 |
| Fracture side | |||
| Right | 23 (63.9 %) | 16 (53.3 %) | 0.39 |
| Left | 13 (36.1 %) | 14 (46.7 %) | 0.39 |
| Follow-up (months) | 28.6 ± 6.2 | 27.2 ± 6.1 | 0.19 |
| Union rate (%) | 97.2 % | 93.3 % | 0.45 |
| Constant score (points) | 95.5 ± 5.9 | 93.3 ± 8.1 | 0.15 |
| Complications (%) | 5.6 % | 23.3 % | 0.04 |
| Return to work in three months (%) | 94.4 % | 73.3 % | 0.02 |
Discussion
Unstable distal clavicular fractures are prone to non-union or delayed union because of their specific biomechanical configuration. Opposing forces of the sternocleidomastoid muscle on one hand and gravity and the pull of the pectoralis muscle on the other may result in significant fragment dislocation, particularly in unstable fractures where the medial fragment is detached from the coracoclavicular (CC) ligaments [17]. The classification and treatment of distal clavicle fractures depend on where the fracture occurs in relation to the conoid and trapezoid ligaments. Neer [22] classified distal clavicle fractures into the following three types: type I fractures, in which the coracoclavicular ligaments are intact; type II fractures, in which the coracoclavicular ligaments are torn from the medial fragment and only the trapezoid ligament remains attached to the lateral fragment; and type III fractures, which involve extension into the acromioclavicular joint. Neer type I and III fractures are inherently stable and do not displace. Therefore, Neer type I and III fractures can be treated non-operatively with a sling for comfort and early ROM exercises as pain allows. The treatment of Neer type II distal clavicle fractures is controversial. Several studies have recommended open reduction and internal fixation in Neer type II distal clavicle fractures because of the tendency to displace and have a higher risk of non-union compared with other clavicle fracture types [13, 22–25].
Plate fixation systems are increasingly used for the treatment of distal clavicle fractures. Two newer implant designs were used in the recent series, including the hook plate and locking plate. The hook plate allows for improved fixation by providing a hook that articulates with the undersurface of the acromion, which serves to reduce the distraction forces on the lateral fracture segment. Reports of successful fracture union with this plate design are common. Complications reported with this design have also been relatively frequent, including implant failure and metaphyseal fracture, impingement, rotator cuff tears or even hook migration and acromial fracture as the implant penetrates the subacromial space and require plate removal. It is therefore important to exercise caution when using hook plate [6–13]. In a recent study, Tan et al. [26] reported 74 % of patients in the hook plate group had mild to severe shoulder pain. Kashii et al. [8] observed one patient had acromial fracture, and hook cutout occurred in 19 of 34 patients who underwent hook plate fixation. ElMaraghy et al. [27] used cadaveric models for subacromial morphometric assessment of the clavicular hook plate. They noticed that despite the posterior orientation of the subacromial hook, the base of the hook still rested in the middle of the supraspinatus fossa. The occurrence of bursal inflammation in this space because of the presence of the subacromial hook could further narrow the distance between the supraspinatus tendon and the subacromial arch, predisposing patients to postoperative complications associated with rotator cuff impingement. Moreover, most of the authors who used the hook plate recommended the removal of the plates as soon as the bony union was achieved to prevent acromial osteolysis and impingement. Nevertheless, reported functional outcomes were satisfactory, regardless of what kind of evaluation method was used [6, 8–10, 12, 28]. In the present study, we found no evidence of subacromial impingement or rotator cuff injuries, although the clavicular hook plate was inserted into the subacromial space; however, complications occurred in seven patients (23.3 %) in the clavicular hook plate group (two partial losses of reduction, three patients with symptomatic hardware, one non-union in six months, and one hardware failure). All the hook plates were removed in an average time of 6.5 months (six to ten months). These observations suggest that this type of hook contact predisposes subacromial structures and the undersurface of the acromion to inflammation and impingement, leading to shoulder pain and function limitation.
With the advent of the locking plate, several site-specific locking plates, including a distal clavicle locking plate, are now available to provide improved fixation with few complications and the advantage of a lower rate of subsequent surgery for hardware removal [14]. Studies have reported excellent results of distal clavicle fractures treated with locking plate [14, 15, 17, 26, 29, 30]. Treatment for unstable distal clavicle fractures using a locking T-plate and a CC PDS (polydioxansulfate) cerclage can provide good and reliable clinical results and a 100 % union rate [16]. Internal fixation with a 2.4-mm distal clavicle T-plate, coracoclavicular ligament repair, and augmentation of the ruptured coracoclavicular ligaments using a PDS cord holds anatomic reduction and allows early full mobilization of the injured shoulder girdle to accomplish a fast return of shoulder function. There is no need for hardware removal because of its low profile. The 53 % hardware removal was due to cultural beliefs and not due to pain, prominence, or cosmetic appearance [20]. Tan et al. [26] revealed that the locking plate fixation exhibited excellent results in activities of daily living, shoulder pain, and ROM in Neer type II distal clavicle fractures. The T-plate, unlike the hook plate, avoids the need to interfere with the scapuloclavicular joint, and therefore does not lead to iatrogenic subacromial impingement or rotator cuff damage, so that the function of the shoulder joint is less compromised. Klein et al. [29] reported a complication rate of 22.7 % in patients treated with a hook plate for unstable lateral clavicle fracture.
In the present study, patients in the locking plate group demonstrated excellent function and high union rates with few complications. The patients got early shoulder ROM and returned to work in a shorter time. Few patients had obvious clinical symptoms that adversely affected their activities of daily living throughout the follow-up period. We observed a high rate of union (97.2 %) and a low complication rate (5.6 %) using this treatment strategy. Our results were compatible with the results of literature [14–20] and only one non-union occurred in six months in our series. Although the functional shoulder score showed no difference between the distal clavicular locking plate and clavicular hook plate groups, the distal clavicular locking plate group had greater ability to return to their previous work in three months after surgery compared to the clavicular hook plate group. Twelve (33 %) patients’ locking plates were removed in an average time of 7.1 months (six to 12 months) since the patient’s requests of cultural beliefs or they became symptomatic after fracture union. The patients who had the implants were afraid of getting in trouble during the security check of airlines or having to provide the relevant hospital certification. Furthermore, they may not be checked with MRI when necessary. They were reluctant to let the implants stay in the body when the fracture was cured. In addition, the implant is not an original part of the human body after all. We determined that the distal clavicular locking plate gave very stable fixation with early shoulder ROM. The patients treated with this method had a grater ability to return to work in a shorter time.
We reviewed and compared systematically the difference of postoperative radiographic and clinical results between the hook plate fixation and the locking plate fixation of the distal clavicle fractures from the relevant literature (Table 2) [6–20, 26, 28–31]. It showed that the non-union rate of the locking plate group (0.16 %) had no significant difference compared to the hook plate group (0.02 %) in the studies reviewed (Table 3). The complication rate in the locking plate group was statistically low (7.5 %) compared to the hook plate group (30.4 %), that is consistent with the present study (Table 4), and it showed significant difference between the two groups in the studies reviewed. Since not all studies reported the functional outcome scores of the distal clavicle fractures and they used different functional evaluation instruments, it was difficult to analyse and compare the function between the different treatment modalities. Consequently, we reviewed and compared the functional outcome scores evaluated by Constant score between the hook plate group (nine studies) [6, 7, 9–13, 31, present study] and the locking plate group (eight studies) [14–20, 30, present study] in distal clavicle fractures. The mean Constant scores were 91.9 and 93.6 in the hook plate and locking plate groups, respectively. The mean Constant score between the two groups were not different significantly which is similar to that in the present study (Table 5).
Table 2.
The retrospective series that used locking plates and hook plate for fixation are compared
| Author | Number of patients | Average follow-up | Fixation method | Union rate | Complications | Functional result | Implant removal |
|---|---|---|---|---|---|---|---|
| Klein et al. [29] | 13 | 12 months | Locking plate | 100 % | One infection | ASES 77.1 | 5 |
| Kalamaras et al. [15] | 8 | 13.6 months | Locking plate | 100 % | One superficial infection One malreduction |
Constant 96 | 0 |
| Herrmann et al. [17] | 7 | 8.3 months | Locking plate | 100 % | None | Constant 93.3 DASH 15.3 |
2 |
| Kaipel et al. [18] | 11 | 4 months | Locking plate | 100 % | Two screw loosening | Constant 89.8 ROWE 99.4 |
3 |
| Yu et al. [30] | 6 | 17 months | Locking plate | 100 % | None | Constant 97.5 | NA |
| Andersen et al. [14] | 20 | 30.7 months | Locking plate | 95 % | One infected nonunion One peri-implant fracture |
ASES 79.0 | 4 |
| Largo et al. [20] | 19 | 5.3 years | Locking plate | 95 % | One breakage of plate One delayed union |
Constant 91.5 DASH 1.4 |
10 |
| Martetsch-lager et al. [16] | 30 | 12.2 months | Locking plate | 100 % | None | Constant 92.3 DASH 6.2 |
NA |
| Tan et al. [26] | 19 | 22.4 months | Locking plate | 100 % | None | UCLA 34.11 | NA |
| Schliemann et al. [19] | 14 | 38 months | Locking plate | 100 % | Three calcifications of the CC ligaments | Constant 93.5 Taft 11.2 |
7 |
| Huang et al. (present study) | 36 | 26.6 months | Locking plate | 97 % | One partial losses of reduction One delayed union |
Constant 95.5 | 12 |
| Lee et al. [12] | 32 | 24.3 months | Hook plate | 100 % | One screw loosening | Constant 90 | 32 |
| Haidar et al. [10] | 22 | 39 months | Hook plate | 95 % | One plate disengaged from clavicle One delayed union and malunion One minor wound breakdown One non-union One plate unhooked of acromion One clavicular stress fracture |
Constant 89 DASH 4.6 |
21 |
| Kashii et al. [8] | 34 | 12.4 months | Hook plate | 100 % | One plate displacement One acromial fracture One rotator cuff tear |
JOA score 98.3 (90–100) |
34 |
| Mizue et al. [28] | 16 | 19 months | Hook plate | 100 % | Four pain Four acromial hole widening |
JOA score 95.1 (86.5–100) |
14 |
| Muramatsu et al. [6] | 15 | 15.5 months | Hook plate | 100 % | 13 (some migration of the plate including 4 severe migration) | Constant 89 (75–95) |
12 |
| Renger et al. [9] | 44 | 27.4 months | Hook plate | 95 % | 37 (2 infection, 3 acromial osteolysis, 2 hypertrophic scar, 30 impingement) | Constant 92.4 (74–100) | NA |
| Tiren et al. [11] | 28 | 65 months | Hook plate | 96 % | One ACJ arthrosis One wound infection |
Constant 97 DASH 3.5 |
27 |
| Lu et al. [31] | 7 | 6.9 months | Hook plate | 100 % | 0 | Constant 93.9 (89–99) |
7 |
| Tambe et al. [7] | 18 | 25 months | Hook plate | 93 % | One deep infection One fracture of the clavicle Five asymptomatic acromial osteolysis |
Constant 88.5 (63–100) |
17 |
| Meda et al. [13] | 31 | 40 months | Hook plate | 100 % | Two superficial infections Six impingement signs |
Constant 94 ASES 26 |
25 |
| Tan et al. [26] | 23 | 22.09 months | Hook plate | 100 % | One superficial infection | UCLA 30.91 | 15 |
| Klein et al. [29] | 22 | 12 months | Hook plate | 94.7 % | Five (1 infection, 3 peri-implant fractures, 1 medial screw fixation failure) | ASES72.4 | 13 |
| Huang et al. (present study) | 30 | 19.2 months | Hook plate | 97 % | Two partial losses of reduction Three symptomatic hardware One delayed union One hardware failure |
Constant 93.3 | 30 |
NA not available
Table 3.
Nonunion rate between hook plate fixation and locking plate fixation
| Group | Non-union | Union | Total |
|---|---|---|---|
| Hook plate group | 7 (0.02 %) | 315 (98 %) | 322 |
| Locking plate group | 3 (0.16 %) | 183 (98.4 %) | 186 |
| Total | 10 (2.0 %) | 498 (98 %) | 508 |
Chi square test p > 0.05
Table 4.
Complication rate between hook plate fixation and locking plate fixation
| Group | Complication (+) | Complication (−) | Total |
|---|---|---|---|
| Hook plate group | 98 (30.4 %) | 224 (69.6 %) | 322 |
| Locking plate group | 14 (7.5 %) | 172 (92.5 %) | 186 |
| Total | 112 (22 %) | 396 (78 %) | 508 |
Chi square test p < 0.05
Table 5.
Constant score between hook plate fixation and locking plate fixation
| Clinical results | Hook plate group | Locking plate group | P value |
|---|---|---|---|
| Constant score (points) | 91.9 | 93.6 | p > 0.05 |
The main limitation of the present study is the small number of cases. In addition, the study was retrospective and not randomized, which could produce selection bias. Therefore, the efficacy of the distal clavicular locking plate or clavicular hook plates in the treatment of unstable distal clavicle fractures should be assessed in studies involving a larger number of cases. A multicentre study may help to further investigate different treatment modalities and define guidelines for the management of unstable distal clavicle fractures.
In conclusion, this present study suggests that distal clavicular locking and clavicular hook plates for the treatment of unstable distal clavicle fractures can achieve good results; however, internal fixation with a distal clavicular locking plate provided greater ability to return to their previous work after surgery in three months and fewer complications than a clavicular hook plate. Considering these promising results of locking plate fixation, this procedure can be regarded as suitable for the treatment of unstable distal clavicle fractures.
Acknowledgments
Conflict of interest statement
None declared.
IRB approval/research ethics committee, or local equivalent state
This study was approved by the Ethics Committee of our institutes. Informed consent was obtained from all patients.
Footnotes
Chunlin Zhang, Junwu Huang and Yi Luo are all co-first authors.
Contributor Information
Chunlin Zhang, Phone: +86-13761904091, FAX: +86-2166301082, Email: shzhangchunlin@gmail.com.
Junwu Huang, Email: shanghaidazhi@163.com.
References
- 1.Edwards DJ, Kavanagh TG, Flannery MC. Fractures of the distal clavicle: a case for fixation. Injury. 1992;23:44–46. doi: 10.1016/0020-1383(92)90125-C. [DOI] [PubMed] [Google Scholar]
- 2.Van der Meijden OA, Gaskill TR, Millett PJ. Treatment of clavicle fractures: current concepts review. J Should Elb Surg. 2012;21:423–429. doi: 10.1016/j.jse.2011.08.053. [DOI] [PubMed] [Google Scholar]
- 3.Kao FC, Chao EK, Chen CH, et al. Treatment of distal clavicle fracture using Kirschner wires and tension-band wires. J Trauma. 2001;51:522–525. doi: 10.1097/00005373-200109000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Macheras G, Kateros KT, Savvidou OD, et al. Coracoclavicular screw fixation for unstable distal clavicle fractures. Orthopedics. 2005;28:693–696. doi: 10.3928/0147-7447-20050701-18. [DOI] [PubMed] [Google Scholar]
- 5.Chen CH, Chen WJ, Shih CH. Surgical treatment for distal clavicle fracture with coracoclavicular ligament disruption. J Trauma. 2002;52:72–78. doi: 10.1097/00005373-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Muramatsu K, Shigetomi M, Matsunaga T, et al. Use of the AO hook-plate for treatment of unstable fractures of the distal clavicle. Arch Orthop Trauma Surg. 2007;127:191–194. doi: 10.1007/s00402-006-0284-5. [DOI] [PubMed] [Google Scholar]
- 7.Tambe AD, Motkur P, Qamar A, et al. Fractures of the distal third of the clavicle treated by hook plating. Int Orthop. 2006;30:7–10. doi: 10.1007/s00264-005-0019-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kashii M, Inui H, Yamamoto K. Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop Relat Res. 2006;447:158–164. doi: 10.1097/01.blo.0000203469.66055.6a. [DOI] [PubMed] [Google Scholar]
- 9.Renger RJ, Roukema GR, Reurings JC, et al. The clavicle hook plate for Neer type II lateral clavicle fractures. J Orthop Trauma. 2009;23:570–574. doi: 10.1097/BOT.0b013e318193d878. [DOI] [PubMed] [Google Scholar]
- 10.Haidar SG, Krishnan KM, Deshmukh SC. Hook plate fixation for type II fractures of the lateral end of the clavicle. J Shoulder Elbow Surg. 2006;15:419–423. doi: 10.1016/j.jse.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 11.Tiren D, Van Bemmel AJ, Swank DJ, et al. Hook plate fixation of acute displaced lateral clavicle fractures: mid-term results and a brief literature overview. J Orthop Surg Res. 2012;7:2. doi: 10.1186/1749-799X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee YS, Lau MJ, Tseng YC, et al. Comparison of the efficacy of hook plate versus tension band wire in the treatment of unstable fractures of the distal clavicle. Int Orthop. 2009;33:1401–1405. doi: 10.1007/s00264-008-0696-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meda PV, Machani B, Sinopidis C, et al. Clavicular hook plate for lateral end fractures: a prospective study. Injury. 2006;37:277–283. doi: 10.1016/j.injury.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 14.Andersen JR, Willis MP, Nelson R, et al. Precontoured superior locked plating of distal clavicle fractures: a new strategy. Clin Orthop Relat Res. 2011;469:3344–3350. doi: 10.1007/s11999-011-2009-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalamaras M, Cutbush K, Robinson M. A method for internal fixation of unstable distal clavicle fractures: early observations using a new technique. J Shoulder Elbow Surg. 2008;17:60–62. doi: 10.1016/j.jse.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 16.Martetschläger F, Kraus TM, Schiele CS, et al. Treatment for unstable distal clavicle fractures (Neer 2) with locking T-plate and additional PDS cerclage. Knee Surg Sports Traumatol Arthrosc. 2012;21(5):1189–1194. doi: 10.1007/s00167-012-2089-0. [DOI] [PubMed] [Google Scholar]
- 17.Herrmann S, Schmidmaier G, Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury. 2009;40:236–239. doi: 10.1016/j.injury.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 18.Kaipel M, Majewski M, Regazzoni P. Double-plate fixation in lateral clavicle fractures-a new strategy. J Trauma. 2010;69:896–900. doi: 10.1097/TA.0b013e3181bedf28. [DOI] [PubMed] [Google Scholar]
- 19.Schliemann B, Roßlenbroich SB, Schneider KN, et al. Surgical treatment of vertically unstable lateral clavicle fractures (Neer 2b) with locked plate fixation and coracoclavicular ligament reconstruction. Arch Orthop Trauma Surg. 2013;133:935–939. doi: 10.1007/s00402-013-1737-2. [DOI] [PubMed] [Google Scholar]
- 20.Largo RD, Rudin MA, Hotz TK, et al. Anatomic reconstruction of unstable lateral clavicular fractures. J Trauma. 2011;71:1348–1351. doi: 10.1097/TA.0b013e3182095dd1. [DOI] [PubMed] [Google Scholar]
- 21.Constant CR, Murley AHG. A clinical method of functional assessment of the shoulder. Clin Orthop. 1987;214:160–164. [PubMed] [Google Scholar]
- 22.Neer CS., 2nd Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 23.Kona J, Bosse MJ, Staheli JW, et al. Type II distal clavicle fractures: a retrospective review of surgical treatment. J Orthop Trauma. 1990;4:115–120. doi: 10.1097/00005131-199004020-00002. [DOI] [PubMed] [Google Scholar]
- 24.Post M. Current concepts in the treatment of fractures of the clavicle. Clin Orthop. 1989;245:89–101. [PubMed] [Google Scholar]
- 25.Yamaguchi H, Arakawa H, Kobayashi M. Results of the Bosworth method for unstable fractures of the distal clavicle. Int Orthop. 1998;22:366–368. doi: 10.1007/s002640050279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tan HL, Zhao JK, Qian C, et al. Clinical results of treatment using a clavicular hook plate versus a T-plate in neer type II distal clavicle fractures. Orthopedics. 2012;35:e1191–e1197. doi: 10.3928/01477447-20120725-18. [DOI] [PubMed] [Google Scholar]
- 27.ElMaraghy AW, Devereaux MW, Ravichandiran K, et al. Subacromial morphometric assessment of the clavicle hook plate. Injury. 2010;41:613–619. doi: 10.1016/j.injury.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 28.Mizue F, Shirai Y, Ito H. Surgical treatment of comminuted fractures of the distal clavicle using Wolter clavicular plates. J Nippon Med Sch. 2000;67:32–34. doi: 10.1272/jnms.67.32. [DOI] [PubMed] [Google Scholar]
- 29.Klein SM, Badman BL, Keating CJ, et al. Results of surgical treatment for unstable distal clavicular fractures. J Shoulder Elbow Surg. 2010;19:1049–1055. doi: 10.1016/j.jse.2009.11.056. [DOI] [PubMed] [Google Scholar]
- 30.Yu C, Sun YH, Zhao CQ, et al. Treatment of distal clavicle fracture with distal radius volar locking compression plate. Chin J Traumatol. 2009;12:299–301. [PubMed] [Google Scholar]
- 31.Lu C, Kao F, Hsu K, et al. Evaluation of a clavicle hook plate for fixation of unstable distal end comminuted clavicle fractures: seven case reports. Formos J Musculoskelet Disord. 2011;2:102–105. doi: 10.1016/j.fjmd.2011.06.005. [DOI] [Google Scholar]