Abstract
Purpose
We sought to analyse clinical and oncological outcomes of patients after guided resection of periacetabular tumours and endoprosthetic reconstruction of the remaining defect.
Methods
From 1988 to 2008, we treated 56 consecutive patients (mean age 52.5 years, 41.1 % women). Patients were followed up either until death or February 2011 (mean follow up 5.5 years, range 0.1–22.5, standard deviation ± 5.3). Kaplan–Meier analysis was used to estimate survival rates.
Results
Disease-specific survival was 59.9 % at five years and 49.7 % at ten and 20 years, respectively. Wide resection margins were achieved in 38 patients, whereas 11 patients underwent marginal and seven intralesional resection. Survival was significantly better in patients with wide or marginal resection than in patients with intralesional resection (p = 0.022). Survival for patients with secondary tumours was significantly worse than for patients with primary tumours (p = 0.003). In 29 patients (51.8 %), at least one reoperation was necessary, resulting in a revision-free survival of 50.5 % at five years, 41.1 % at ten years and 30.6 % at 20 years. Implant survival was 77.0 % at five years, 68.6 % at ten years and 51.8 % at 20 years. A total of 35 patients (62.5 %) experienced one or more complications after surgery. Ten of 56 patients (17.9 %) experienced local recurrence after a mean of 8.9 months. The mean postoperative Musculoskeletal Tumor Society (MSTS) score was 18.1 (60.1 %).
Conclusion
The surgical approach assessed in this study simplifies the process of tumour resection and prosthesis implantation and leads to acceptable clinical and oncological outcomes.
Keywords: Periacetabular tumours, Three-dimensional planning, Rapid prototyping, Guided osteotomy, Patient-specific implants, Endoprosthetic reconstruction, Custom made
Introduction
Resection of musculoskeletal sarcomas of the pelvis and consecutive reconstruction of the remaining defect is still one of the most demanding procedures in orthopaedic surgery. Upon their detection, most such tumours have large dimensions and are located in close proximity to neurovascular and visceral structures [1]. A fortiori, adequate surgical margins are critical to prevent local recurrence and to reach favourable oncological outcomes [2]. While external hemipelvectomy has been the ultimate surgical procedure for many years for locally advanced pelvic sarcomas, the introduction of multimodal therapeutic concepts and improved reconstruction techniques has made limb-salvage procedures increasingly successful [3]. Reconstructing periacetabular bone defects represents a special challenge, as load transfer from the axial skeleton to the lower extremity must be assured [4]. Thus, the precondition for maintaining a functional hip joint is a stable anchorage of the distal femoral resection area at the remaining proximal pelvic structures. The best type of reconstruction following periacetabular tumour resection remains unclear. Techniques such as flail hip, hip transposition or arthrodesis reportedly led to significant leg-length discrepancy, limited range of motion or poor ambulation [5]. Though allografts or autografts can restore the pelvic anatomy and provide good functional results, especially in young patients, a high rate of nonunion and infection has been reported [6–8]. Reconstruction with pelvic megaprostheses helps maintain vertical stability and restore painless joint function without significant leg-length discrepancies. On the other hand, studies analysing complication rates associated with this procedure show considerably high rates of infection, prosthetic loosening and component dislocation, so that some authors recommend excision arthroplasty rather than prosthetic reconstruction [4, 9–11]. However, recent studies suggest that after 3D reconstruction of the patient’s pelvis, a computer-designed hemipelvic custom-made prosthesis can simplify the implantation process and therefore may help decrease the associated complications and facilitate functional recovery [12–14]. Some authors even suggest the use of intra-operative navigation software to improve the accuracy of the pelvic osteotomy [15, 16]. However, only case series have been published so far, and long-term outcome after navigated pelvic tumour surgery remains to be determined [17, 18].
For more than 25 years, we have used a computer-aided, 3D planning system in our clinic to engineer patient-specific osteotomy guides that allow accurate pelvic resection planes for custom-fitting fixation of pelvic endoprostheses. In this study, we report the first long-term results using this surgical system.
Materials and methods
Between 1988 and 2008, we treated 56 consecutive patients with guided periacetabular tumour resection and implantation of a custom-made endoprosthesis which was fixed at the remaining iliac bone. Mean patient age at the time of surgery was 52.5 [range 13–77, standard deviation (SD) ± 16.1]; 33 of the 56 patients (58.9 %) were men. Data was collected prospectively in our interdisciplinary tumour database. Patients were monitored either until death or 7 February 2011, which was the last time point of data acquisition. The institutional review board approved the research protocol (approval no. 5230/11).
All operations were performed at the University Hospital of the Technical University Munich. All patients underwent surgical staging studies, including local X-ray and computed tomography (CT). Since the beginning of the 1990s, the extent of bone and soft tissue involvement and the presence of skip lesions were determined by magnetic resonance imaging (MRI) of the entire pelvis, including the entire femur diaphysis. Staging was completed by chest and abdominal CT, bone scintigraphy and positron emission tomography (PET). The shortest distance between skin and tumour within the later surgical approach was used for biopsy. Contraindications for endoprosthetic reconstruction were limited life expectancy, poor therapeutic compliance or extensive tumour infiltration of soft tissues, intrapelvic organs or neurovascular structures. Indications for treatment included 21 primary and 28 secondary bone tumours. Twenty-one patients had a single metastatic lesion; seven patients had more than one metastatic bony lesions. Staging studies excluded visceral metastases in all cases. In seven patients, the diagnosis was a primary soft tissue sarcoma (Table 1).
Table 1.
Disease types and list of histologically proven diagnoses (n=56). Primary tumour staging according to the American Joint Committee on Cancer (AJCC)
| Primary tumours (n = 28): | AJCC staging: | |||
| IB | IIA | IIB | III | |
| Chondrosarcoma (10) | 1 | 2 | 6 | 1 |
| Ewing’s sarcoma (6) | - | - | 6 | - |
| Osteosarcoma (4) | - | - | 3 | 1 |
| Hemangiopericytoma (1) | - | - | - | 1 |
| Undifferentiated pleomorphic sarcoma (not otherwise specified) (3) | - | - | - | 3 |
| Fibrosarcoma (2) | - | - | 1 | 1 |
| Liposarcoma (2) | - | 1 | - | 1 |
| Totals | 1 | 3 | 16 | 8 |
| Secondary bone tumours (n = 28): | Single lesions | Multiple lesions | ||
| Renal cell carcinoma (12) | 10 | 2 | ||
| Mamma carcinoma (5) | 2 | 3 | ||
| Thyroid cancer (3) | 2 | 1 | ||
| Non-small-cell lung carcinoma (NSCLC) (2) | 2 | - | ||
| Oral cancer (2) | 2 | - | ||
| Prostate cancer (1) | - | 1 | ||
| Nasopharyngeal carcinoma (1) | 1 | - | ||
| Rectal cancer (1) | 1 | - | ||
| Esophageal cancer (1) | 1 | - | ||
| Total | 21 | 7 | ||
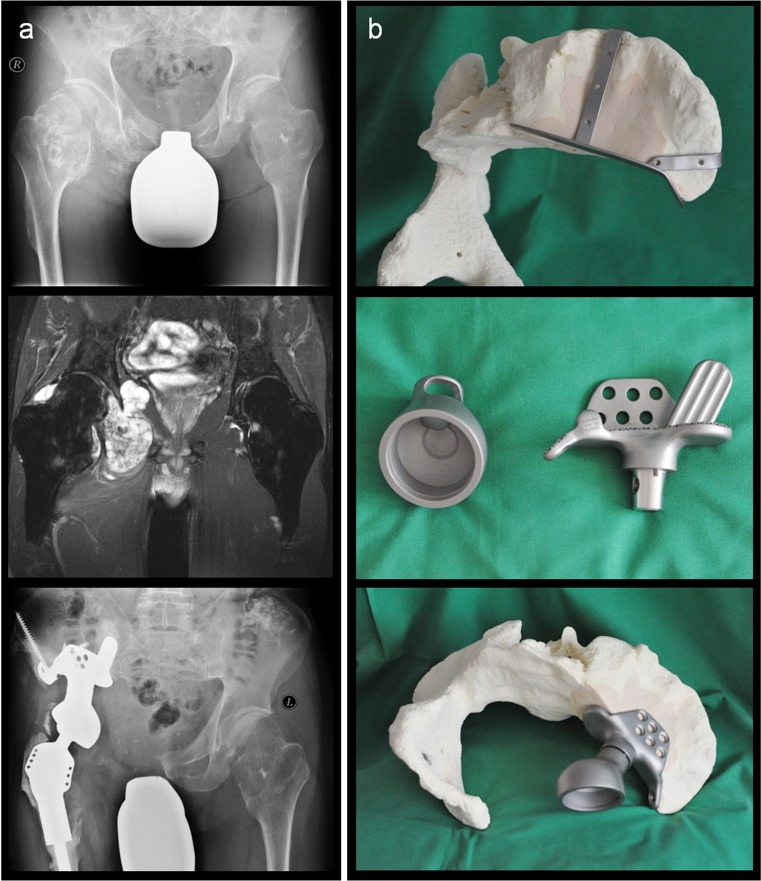
Prior to surgery, all cases were discussed in an interdisciplinary tumour board. Tumour restaging was performed in case of preoperative chemo- or radiation therapy. The surgical technique, perioperative protocol and preliminary results are described elsewhere [19]. Pre-operatively, a 3D polyurethane model of the patient’s pelvis was fabricated according to data obtained by high-resolution CT. This model facilitated visual and haptic perception both before and during surgery. In close co-operation with the engineers, the surgeon marked the levels of osteotomy in the polyurethane model. Based on the marked resection planes, special osteotomy guides and the prosthesis were designed (Orthodynamics GmbH, Lübeck, Germany; formerly ESKA-Implants). Prosthetic components were composed of cobalt–chromium–molybdenum (CoCroMo) alloy and coated with titanium–niobium. The surface area of the prosthesis in contact with the host bone has a macro-porous-coated structure with hexapodal forms (Spongiosa Metal®) with a porosity of ∼70 % and pore sizes from 200 to 2000 μm to enhance osseointegration. To increase primary stability of the prosthetic system, an intramedullary stem is cemented into the medullary cavity of the remaining bone. Additionally, an extramedullary plate can be fixed at the facies glutealis of the iliac bone. A step-by-step adjustment of anteversion of the acetabular component is possible. Cup inserts are made of ultra-high-molecular-weight polyethylene (UHMWPE) (ID 28, 32 and 36 mm; designs: standard, elevated, constrained). Prior to surgery, osteotomy guides and the custom-made part of the prosthesis were fitted to the simulated bony resection planes (Fig. 1). Design, manufacturing and delivery of patient-specific guides and implants took approximately three weeks.
Fig. 1.
a Preoperative radiograph (top panel) and magnetic resonance imaging (coronal T2-weighted turbo spin-echo) (middle panel) of a 44-year-old patient with a painful mass at the right hemipelvis and hereditary multiple exostoses. Histological analysis revealed a secondary chondrosarcoma (American Joint Committee on Cancer staging IIB). Radiograph 3.5 years postoperatively (bottom panel), with a stable prosthesis and a good functional outcome (Musculoskeletal Tumor Society rating 70%). b Osteotomy guide (top panel) and prosthetic component for bony fixation (middle panel) are custom made. The acetabular component is a modular off-the-shelf product, and its anteversion can be adjusted step by step relative to the component fixed at the remaining iliac bone (bottom panel). (Left panel reproduced from [19], with permission)
Postoperatively, all patients were permitted weight-bearing with 10 kg for a period of six weeks. Load was increased by 10 kg per week until full body weight was achieved. Until then, we recommended low-molecular-weight heparins to prevent thromboembolism. At follow-up, all patients were monitored for local recurrence and metastases using history, physical examination and radiographic studies according to the recommendations of the Musculoskeletal Tumor Center Munich [20]. Functional evaluation of the affected limb was assessed using the Musculoskeletal Tumor Society (MSTS) score [21].
We used SigmaStat 3.5® software (Systat) for all statistical analyses. For descriptive statistics, values are reported as mean, SD and range. Follow-up for Kaplan–Meier survival analyses started from the day of surgery and ended on the day of death or on 7 February 2011, the last time point of data acquisition. Clinical follow-up was defined as the period between surgery and the patient’s last clinic visit (mean 5.5, range 0.1–22.5, SD ± 5.3 years). Kaplan–Meier analysis was also used to evaluate revision-free implant survival. The log-rank test (Mantel-Cox) was used to determine whether differences in survival between groups were significant. Cox proportional hazards regression model was used to assess independent effects on patient survival. The level of significance was set at p ≤ 0.05.
Results
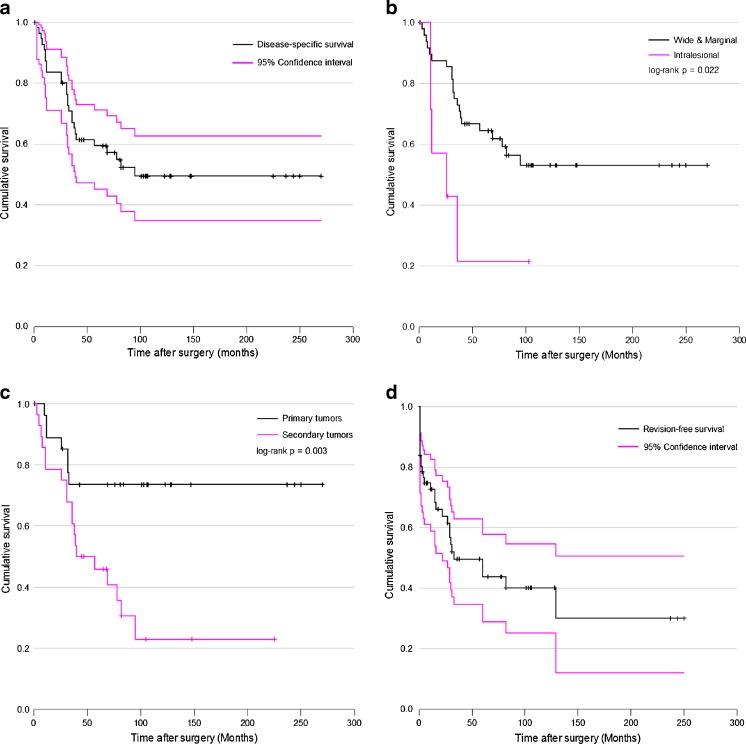
At the last time point of data acquisition, 23 of 56 patients were still alive either with (n = 8) or without (n = 15) evidence of disease. Twenty-six patients died because of the underlying malignancy (n = 26), and seven died due to other causes (n = 7). Overall survival rate was 49.4 % [95 % confidence interval (CI) = 35.5 –61.6] at five years and 37.9 % (95 % CI = 23.6 –50.4) at ten and 20 years. Estimated disease-specific survival rate was calculated by treating deaths from causes other than the disease as censored data: 59.9 % (95 % CI = 45.1 –71.1) at five years, and 49.7 % (95 % CI = 34.6–62.8) at ten and 20 years, respectively (Fig. 2a). Cox regression identified gender [female, p = 0.028; hazard ratio (HR) = 2.39; 95 % CI = 1.09 –5.21) as an independent predictor of disease-specific survival. Wide resection margins were achieved in 38 patients; 11 patients underwent marginal and seven intralesional resection. Disease-specific survival rates for wide and marginal resections showed no statistically significant difference (p = 0.652). However, there was a statistically significant difference in survival rates between patients with wide or marginal and intralesional resection (p = 0.022) (Fig. 2b). The disease-specific survival rate for patients with primary tumours was 73.7 % (95 % CI = 52.5–86.6) at five, ten and 20 years and was significantly affected by tumour stage at the time of surgery [American Joint Committee on Cancer (AJCC) staging > IIb, p = 0.032, HR = 5.3, 95 % CI = 1.2–24.5 %). For patients with pelvic metastases, survival rate was 46.2 % (95 % CI = 26.7–63.0 %) at five years and 23.1 % (95 % CI = 7.2–43.5) at ten years. Survival for patients with secondary tumours was significantly worse than for patients with primary tumours (p = 0.003) (Fig. 2c).
Fig. 2.
Kaplan–Meier curves showing a overall disease-specific survival, b survival for patients after wide or marginal and intralesional tumor resection, c survival after primary and secondary tumor resection, d revision-free survival
In 29 patients (51.8 %), at least one re-operation was necessary, resulting in a revision-free survival of 50.5 % (95 % CI = 35.4–63.4) at five years, 41.1 % (95 % CI = 25.8–56.0) at ten years and 30.6 % (95 % CI = 12.3–51.6) at 20 years (Fig. 2d). Implant survival with event data points defined as external hemipelvectomy and septic or aseptic implant removal was 77.0 % (95 % CI = 60.3–87.2) at five years, 68.6 % (95 % CI = 48.2–81.8) at ten years and 51.8 % (95 % CI = 18.6–76.3) at 20 years; 35 patients (62.5 %) experienced one or more complications postsurgery (Table 2).
Table 2.
List of complications related to surgery
| Complications | Number (%) |
|---|---|
| Infection | 14 (25) |
| Dislocation | 11 (19.6) |
| Superficial wound problems | 10 (17.9) |
| Local recurrence | 10 (17.9) |
| Deep vein thrombosis | 7 (12.5) |
| Lymphoedema | 5 (8.9) |
| Sciatic nerve palsy | 5 (8.9) |
| Aseptic loosening | 3 (5.4) |
| Femoral nerve palsy | 2 (3.6) |
| Pulmonary embolism | 1 (1.8) |
| Intestinal fistula | 1 (1.8) |
| Deep haematoma | 1 (1.8) |
Ten of 56 patients (17.9 %) had a local recurence after a mean of 8.9 (range 3–16, SD ± 4.6) months. Six of those patients died of the disease, three died of other causes and one was still alive at the last time point of data acquisition. To control the local disease, one patient had to be treated by external hemipelvectomy. Recurrence-free survival was 80.4 % (95 % CI = 66.9–89.6) at ten years and was significantly lower for patients with intralesional resection than for patients with wide or marginal resection (p = 0.005). There was no statistical difference between primary and secondary tumours (p = 0.260). For primary tumours, tumour stage (AJCC staging > II b, p = 0.069, HR = 8.2, 95 % CI = 0.8–79.4) was not identified as an independent predictor for tumour recurrence. It is noteworthy that three of the four primary tumours that showed later recurrence were soft tissue tumours (AJCC stage III).
Periprosthetic infection occurred in 14 patients (25 %). In eight of these cases, infection was diagnosed within the first 30 days of the initial surgery. The treatment strategy consisted of extensive debridement, local antiseptic irrigation and systemic antibiotic therapy. Six patients experienced an infection diagnosed at a later time point; four of them were treated by resection arthroplasty, and in two cases, an external hemipelvectomy was performed. Further indications for revision surgery were aseptic loosening of the pelvic fixation in three and recurrent dislocation in six cases. In all these cases, a prosthetic component revision was successful. One patient required endovascular treatment with coiling of a parietal branch of the internal iliac artery due to a deep postoperative haematoma. In another patient, surgical intervention was necessary due to an intestinal fistula.
The mean postoperative MSTS score for all patients was 18.1 of 30 (60.1 %, range 30–87 %, SD ± 12.6). Regarding isolated parameters, the highest mean scores were achieved in pain reduction (3.7) and emotional acceptance (3.9); the lowest mean score was seen in the use of walking aids (2.5). In three patients, an external hemipelvectomy was necessary. All other patients were ambulatory, but most of them used walking aids and walked with a pronounced limp. No relevant leg-length discrepancies were observed. After asking the patients if they would repeat the surgery under the same circumstances, only three patients answered no. The 23 patients who were still alive at the end of the study showed a mean MSTS score of 19.5 of 30 (64.9 %, range 33–87 %, SD ± 12.3) at a mean clinical follow-up of 9.5 (range 2.3–22.5, SD ± 5.8) years.
Discussion
In periacetabular tumours, resection of the hip joint is often necessary to achieve tumour-free resection margins. Though prosthetic reconstruction can result in higher functional scores than resection arthroplasty, it is associated with higher complication rates, with up to 50 % of patients requiring septic or aseptic implant removal [1, 5, 10, 22, 23]. Periacetabular tumour resection must be highly accurate and requires detailed preoperative planning. Resecting too much bone leads to tumour-free margins but makes the implantation of custom-made prostheses difficult. Therefore, 3D planning of the osteotomy may have implications not only for the adequacy of the resection margins but also for the biomechanical stability of the prosthesis. However, using physical or virtual pelvic models still requires the surgeon to measure the definitive length of the resection line between predefined anatomical landmarks during the operation. This procedure is error prone, as these landmarks are not always easily accessible intraoperatively [14]. Furthermore, an osteotomy performed freehand can lead to inaccurate resection planes impeding the implantation of the prosthesis. To minimise the risk of prosthesis failure and increase tumour resection accuracy, some authors suggest using computer-assisted navigation technologies [16–18]. However, navigation systems are not yet routinely used in pelvic tumour surgery, as they prolong operative time and require sufficient user experience and training to prevent technical errors in the registration process or the tracking system. In this study, we describe a technically easy-to-use alternative to computer-assisted navigated periacetabular tumour resection by introducing patient-specific templates that make a guided osteotomy feasible and facilitate the prosthesis implantation process.
The few existing studies describing the outcome of 3D planning and patient-specific endoprosthetic reconstruction for periacetabular tumours have mostly been in the form of retrospective studies assessing a heterogeneous patient population diagnosed with different tumour entities [5, 12, 24–26]. This makes it difficult to directly compare study results. Nevertheless, the overall clinical and oncological outcome described in our study seems to be comparable with results of other studies [23, 27]. In our study, good results were obtained in patients with primary sarcomas of the pelvis with a five year survival rate of 73.7 %; other studies reported five year survival rates between 41 % and 65 % for similar patient groups [5, 27–29]. As expected, survival was significantly affected by tumour stage. From an oncological point of view, outcomes differed significantly between primary and secondary tumours. Therefore, in the future we would recommend this procedure only in patients with single metastatic lesions from tumor entities with a relatively long median survival after diagnosis of bone metastasis such as breast, prostate or thyroid cancer. As known from other series [5, 23], survival was significantly influenced by resection status and significantly better after wide and marginal than intralesional resection. Whether a guided or navigated osteotomy results in an increase of negative resection margins in pelvic tumour surgery must be proven in future studies comparing these techniques with nonguided procedures.
The most common reported failure mode of pelvic tumour resection and reconstruction with megaprostheses is infection [23] due to the large wound cavity, relatively long operative time and limited intrinsic regenerative potential of tissue after neoadjuvant therapy. This was also observed in our series, with an infection rate of 25 % resulting in septic implant removal in 10.7 % of patients. These numbers are similar to those reported in other series with infection rates between 13 % and 32 % and implant removal rates between 3.6 % and 25 % (reviewed in detail in [23]). In the future, this problem has to be approached from the perspective of the nature of the implant material the surgeon works with [30]. In orthopaedic tumour surgery, in particular, a paradigm shift is needed from surgical concepts to replace tissues with inert metallic implants to more biological approaches that focus on repair and reconstitution of tissue structure and function [31].
Given the complexity of the surgical procedures required to treat patients with periacetabular tumours, we obtained acceptable clinical and oncological outcomes. When using the described surgical approach, good oncological results can be expected in patients with primary tumours. Pre-operatively, the high complication rate associated with endoprosthetic reconstruction after periacetabular tumour resection must be discussed in detail, and patients must be informed about alternative reconstruction strategies. Importantly, the customised osteotomy guides presented here simplify the process of tumour resection and the later prosthesis implantation. This treatment concept is already used in maxillofacial surgery to transfer insights of the preoperative 3D planning process to the operating field [32]. However, to our knowledge, this technique has not been described for pelvic tumour surgery. It is to be expected that navigation technologies which have already displayed their clinical utility in conventional hip and knee replacements improve the outcome of pelvic tumor surgery in the future. However, the easy-to-use surgical protocol described in this study might be a treatment alternative, especially when it might be possible to simplify the production workflow of the osteotomy guides by implementing novel 3D printing technologies in-house in order to reduce treatment costs and production time.
Acknowledgements
This work was funded by the Wilhelm-Sander Foundation (project no. 94.086.1/2). BMH is a fellow of the German Research Foundation (DFG HO 5068/1-1). DWH is supported by a Hans Fischer Senior Fellowship of the Institute for Advanced Study, Technical University Munich, funded by the German Excellence Initiative.
Conflict of interest statement
None.
References
- 1.Yuen A, Ek ET, Choong PF. Research: Is resection of tumours involving the pelvic ring justified? : A review of 49 consecutive cases. Int Semin Surg Oncol. 2005;2:9. doi: 10.1186/1477-7800-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kawai A, Healey JH, Boland PJ, Lin PP, Huvos AG, Meyers PA. Prognostic factors for patients with sarcomas of the pelvic bones. Cancer. 1998;82:851–859. doi: 10.1002/(SICI)1097-0142(19980301)82:5<851::AID-CNCR8>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 3.Ham SJ, Schraffordt KH, Veth RP, van Horn JR, Eisma WH, Hoekstra HJ. External and internal hemipelvectomy for sarcomas of the pelvic girdle: consequences of limb-salvage treatment. Eur J Surg Oncol. 1997;23:540–546. doi: 10.1016/S0748-7983(97)93173-5. [DOI] [PubMed] [Google Scholar]
- 4.Hoffmann C, Gosheger G, Gebert C, Jurgens H, Winkelmann W. Functional results and quality of life after treatment of pelvic sarcomas involving the acetabulum. J Bone Joint Surg Am. 2006;88:575–582. doi: 10.2106/JBJS.D.02488. [DOI] [PubMed] [Google Scholar]
- 5.Jaiswal PK, Aston WJ, Grimer RJ, Abudu A, Carter S, Blunn G, Briggs TW, Cannon S. Peri-acetabular resection and endoprosthetic reconstruction for tumours of the acetabulum. J Bone Joint Surg (Br) 2008;90:1222–1227. doi: 10.1302/0301-620X.90B9.20758. [DOI] [PubMed] [Google Scholar]
- 6.Davidson AW, Hong A, McCarthy SW, Stalley PD. En-bloc resection, extracorporeal irradiation, and re-implantation in limb salvage for bony malignancies. J Bone Joint Surg (Br) 2005;87:851–857. doi: 10.1302/0301-620X.87B6.15950. [DOI] [PubMed] [Google Scholar]
- 7.Delloye C, Banse X, Brichard B, Docquier PL, Cornu O. Pelvic reconstruction with a structural pelvic allograft after resection of a malignant bone tumor. J Bone Joint Surg Am. 2007;89:579–587. doi: 10.2106/JBJS.E.00943. [DOI] [PubMed] [Google Scholar]
- 8.Schwameis E, Dominkus M, Krepler P, Dorotka R, Lang S, Windhager R, Kotz R (2002) Reconstruction of the pelvis after tumor resection in children and adolescents. Clin Orthop Relat Res 220–235 [DOI] [PubMed]
- 9.Uchida A, Myoui A, Araki N, Yoshikawa H, Ueda T, Aoki Y (1996) Prosthetic reconstruction for periacetabular malignant tumors. Clin Orthop Relat Res 238–245 [DOI] [PubMed]
- 10.Windhager R, Karner J, Kutschera HP, Polterauer P, Salzer-Kuntschik M, Kotz R (1996) Limb salvage in periacetabular sarcomas: review of 21 consecutive cases. Clin Orthop Relat Res 265–276 [PubMed]
- 11.Pilge H, Gradl G, von Eisenhart-Rothe R, Gollwitzer H. Incidence and outcome after infection of megaprostheses. Hip Int. 2012;22(Suppl 8):S83–S90. doi: 10.5301/HIP.2012.9576. [DOI] [PubMed] [Google Scholar]
- 12.Dai KR, Yan MN, Zhu ZA, Sun YH. Computer-aided custom-made hemipelvic prosthesis used in extensive pelvic lesions. J Arthroplasty. 2007;22:981–986. doi: 10.1016/j.arth.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 13.Sun W, Li J, Li Q, Li G, Cai Z. Clinical effectiveness of hemipelvic reconstruction using computer-aided custom-made prostheses after resection of malignant pelvic tumors. J Arthroplasty. 2011;26:1508–1513. doi: 10.1016/j.arth.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 14.Bruns J, Habermann CR, Ruther W, Delling D. The use of CT derived solid modelling of the pelvis in planning cancer resections. Eur J Surg Oncol. 2010;36:594–598. doi: 10.1016/j.ejso.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Bastian L, Hufner T, Mossinger E, Geerling J, Goesling T, Busche M, Kendoff D, Bading S, Rosenthal H, Krettek C. Integration of modern technologies in therapy of sarcomas of the pelvis. Computer-assisted hemipelvectomy and implantation of a "custom-made" Bonit gentamycin coated partial pelvic prosthesis. Unfallchirurg. 2003;106:956–962. doi: 10.1007/s00113-003-0680-z. [DOI] [PubMed] [Google Scholar]
- 16.Docquier PL, Paul L, Cartiaux O, Delloye C, Banse X. Computer-assisted resection and reconstruction of pelvic tumor sarcoma. Sarcoma. 2010;2010:125162. doi: 10.1155/2010/125162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho HS, Oh JH, Han I, Kim HS. The outcomes of navigation-assisted bone tumour surgery: minimum three-year follow-up. J Bone Joint Surg (Br) 2012;94:1414–1420. doi: 10.1302/0301-620X.94B10.28638. [DOI] [PubMed] [Google Scholar]
- 18.Wong KC, Kumta SM, Chiu KH, Antonio GE, Unwin P, Leung KS. Precision tumour resection and reconstruction using image-guided computer navigation. J Bone Joint Surg (Br) 2007;89:943–947. doi: 10.1302/0301-620X.89B7.19067. [DOI] [PubMed] [Google Scholar]
- 19.Rudert M, Holzapfel BM, Pilge H, Rechl H, Gradinger R. Partial pelvic resection (internal hemipelvectomy) and endoprosthetic replacement in periacetabular tumors. Oper Orthop Traumatol. 2012;24:196–214. doi: 10.1007/s00064-012-0161-z. [DOI] [PubMed] [Google Scholar]
- 20.Tumormanual des Tumorzentrums München. München: W. Zuckschwerdt Verlag; 2004. [Google Scholar]
- 21.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–246. [PubMed] [Google Scholar]
- 22.Gradinger R, Rechl H, Hipp E. Pelvic osteosarcoma. Resection, reconstruction, local control, and survival statistics. Clin Orthop Relat Res. 1991;270:149–158. [PubMed] [Google Scholar]
- 23.Witte D, Bernd L, Bruns J, Gosheger G, Hardes J, Hartwig E, Lehner B, Melcher I, Mutschler W, Schulte M, Tunn PU, Wozniak W, Zahlten-Hinguranage A, Zeifang F. Limb-salvage reconstruction with MUTARS hemipelvic endoprosthesis: a prospective multicenter study. Eur J Surg Oncol. 2009;35:1318–1325. doi: 10.1016/j.ejso.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 24.Abudu A, Grimer RJ, Cannon SR, Carter SR, Sneath RS. Reconstruction of the hemipelvis after the excision of malignant tumours. Complications and functional outcome of prostheses. J Bone Joint Surg Br. 1997;79:773–779. doi: 10.1302/0301-620X.79B5.6749. [DOI] [PubMed] [Google Scholar]
- 25.Guo W, Li D, Tang X, Yang Y, Ji T. Reconstruction with modular hemipelvic prostheses for periacetabular tumor. Clin Orthop Relat Res. 2007;461:180–188. doi: 10.1097/BLO.0b013e31806165d5. [DOI] [PubMed] [Google Scholar]
- 26.Muller PE, Durr HR, Wegener B, Pellengahr C, Refior HJ, Jansson V. Internal hemipelvectomy and reconstruction with a megaprosthesis. Int Orthop. 2002;26:76–79. doi: 10.1007/s00264-001-0322-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ueda T, Kakunaga S, Takenaka S, Araki N, Yoshikawa H. Constrained total hip megaprosthesis for primary periacetabular tumors. Clin Orthop Relat Res. 2013;471:741–749. doi: 10.1007/s11999-012-2625-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grimer RJ, Carter SR, Tillman RM, Spooner D, Mangham DC, Kabukcuoglu Y. Osteosarcoma of the pelvis. J Bone Joint Surg (Br) 1999;81:796–802. doi: 10.1302/0301-620X.81B5.9241. [DOI] [PubMed] [Google Scholar]
- 29.Ozaki T, Hillmann A, Lindner N, Blasius S, Winkelmann W. Chondrosarcoma of the pelvis. Clin Orthop Relat Res. 1997;337:226–239. doi: 10.1097/00003086-199704000-00025. [DOI] [PubMed] [Google Scholar]
- 30.Holzapfel BM, Chhaya MP, Melchels FP, Holzapfel NP, Prodinger PM, von Eisenhart-Rothe R, van Griensven M, Schantz JT, Rudert M, Hutmacher DW. Can bone tissue engineering contribute to therapy concepts after resection of musculoskeletal sarcoma? Sarcoma. 2013;2013:153640. doi: 10.1155/2013/153640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Holzapfel BM, Reichert JC, Schantz JT, Gbureck U, Rackwitz L, Noth U, Jakob F, Rudert M, Groll J, Hutmacher DW. How smart do biomaterials need to be? A translational science and clinical point of view. Adv Drug Deliv Rev. 2013;65:581–603. doi: 10.1016/j.addr.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 32.Polley JW, Figueroa AA. Orthognathic positioning system: intraoperative system to transfer virtual surgical plan to operating field during orthognathic surgery. J Oral Maxillofac Surg. 2013;71:911–920. doi: 10.1016/j.joms.2012.11.004. [DOI] [PubMed] [Google Scholar]