Abstract
Purpose
The Humerusblock is a minimally invasive device allowing fixation of proximal humeral fractures. A drawback of the device is possible K-wire perforation of the head with the need for early removal of the implant. We assessed the amount of humeral head impaction and its role in the postoperative varus/valgus deviation of the humeral head in fractures of the upper humerus treated with Humerusblock.
Methods
Fractures were classified according to the Codman-Lego system. The length of the posteromedial metaphyseal extension and integrity of medial hinge were measured; metaphyseal comminution was assessed. Accuracy of fracture reduction was classified as excellent to poor. An original method of measurement of amount of postoperative impaction of the humeral head was developed. The impaction and varus/valgus inclination of the heads were measured comparing postoperative and three-month follow-up radiographs. Constant score and its relation to sintering was calculated at 12-month follow-up.
Results
Forty-three fractures were available for follow-up. The amount of humeral head impaction was 3.9 mm on average and was directly correlated with patient’s age, sex, Codman-Lego classification, varus inclination and mataphyseal comminution. The postoperative cervico-diaphyseal angle was restored in 35 cases, with 81 % good results. The Humerusblock was removed in 41 % of cases because of K-wire perforation of the humeral head. A negative correlation was found between impaction and Constant score.
Conclusions
The amount of humeral head impaction is related to patients’ age, sex, and fracture patterns, being the most prone to compaction those with metaphyseal comminution. Humeral head impaction negatively affects final Constant score.
Electronic supplementary material
The online version of this article (doi:10.1007/s00264-014-2327-9) contains supplementary material, which is available to authorized users.
Keywords: Proximal humerus fractures, Humeral head impaction, Sintering, Humerusblock, Metaphyseal comminution, Calculation of head impaction, Complications
Introduction
It has recently been reported that surgical management is needed in 21 % of proximal humeral fractures [1]. However, fixation of these fractures remains challenging, particularly in the presence of multiple fragments, metaphyseal comminution, and severe osteoporosis. Angular stable implants with rigid or semi-rigid fixation of head and shaft were introduced to treat displaced, comminuted fractures, specifically aiming to improve the osteosynthesis in the osteoporotic proximal humerus [2–6]. However, there is a lack of consensus on the optimal management of these fractures, since the mean reported rate of postoperative complications is 36 % [7–10]. A survey carried out at 348 hospitals in Germany, Austria and Switzerland has shown that one of the most common complications of the surgical treatment of proximal humerus fractures is perforation of the articular surface of the humeral head by fixation means or components of the implant, which occurred in 73 % of cases [11].
The Humerusblock device (Synthes, Oberdorf, Switzerland) enables percutaneous Kirschner-wire (K-wire) fixation of displaced fractures of the proximal humerus [12]. The peculiar features of the device are two 2.5-mm K-wires that are fixed in a cylindrical device applied on the lateral cortex of the humeral diaphysis. The wires are introduced through the cylinder and the lateral cortical bone of the humerus shaft into the humeral head. They are inserted, in the sagittal plane, in divergent directions, very similar to the directions of the humeral load peaks described by Bergmann et al. [13]. According to the latter study, in fact, the load peaks on the humeral head occur in a superomedial direction in the frontal plane and a superoposterior direction in the sagittal plane within a very small range of direction [13].
Good clinical and radiolographic results were obtained with the Humerusblock in different trauma centres [5, 12, 14, 15], with limited cases of fixation failure. However, one of the drawbacks of the implant is that perforation of the humeral head by K-wires requires early removal of the implant in 20–40 % of cases [5, 14, 15]. Head perforation is the result of a phenomenon called “controlled impaction” [16], which is a sintering effect of the fractured humeral head that consistently occurs in the first few weeks after surgery. A similar effect was found also in the factures of the upper humerus treated with locking plates and head screws, which may undergo postoperative impaction resulting in subsidence of the humeral head [17, 18].
Although several authors have described the impaction phenomenon of the humeral head in fractures of the proximal humerus treated with the Humerusblock, in no study was the amount of sintering measured and, thus, no mean, or range of values, are known. However, this information is important since the knowledge of a safe distance between the tip of the hardware and the surface of the humeral head might avoid most perforations of the head.
This study was aimed at assessing the rate and amount of the humeral head impaction, and its influence on the maintenance of the cervico-diaphyseal angle obtained at surgery, and on clinical results in a consecutive series of proximal humerus fractures treated with the Humerusblock device.
Materials and methods
Between March 2011 and January 2013, 46 consecutive displaced proximal humerus fractures were treated with closed or minimally-invasive reduction and ostheosynthesis using the Humerusblock system. The diagnosis and classification of fractures was based on anteroposterior, transthoracic and axillary (when possible) radiographs of the involved shoulder. CT scans were obtained in all cases to better evaluate the fracture pattern and to plan surgery. Fractures were classified according to the Hertel et al. Codman-Lego system (Fig. 1) [19], while the varus/valgus of the upper humerus, and impaction/distraction angulation was assessed as described by Resch [20]. On the basis of the Codman-Lego system, we measured the length of the posteromedial metaphyseal extension (length of calcar attached to the head < or > 8 mm) and the integrity of the medial hinge (calcar dislocation with respect to the diaphysis < or > 2 mm). Metaphyseal comminution was also assessed.
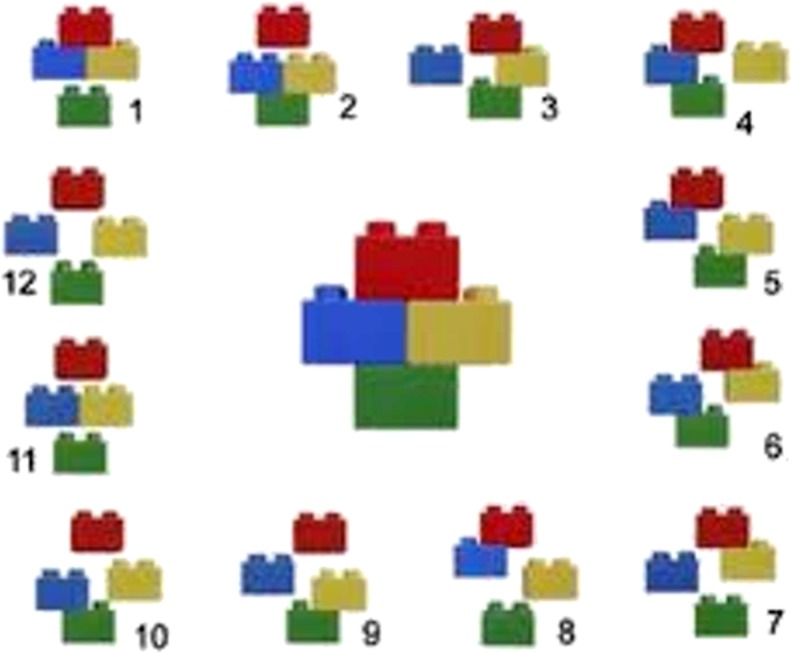
Fig. 1.
The binary system (LEGO system) developed by Hertel et al. [19] represents the four parts of the proximal humerus (head, greater tuberosity, lesser tuberosity, shaft) using the LEGO blocks. The absence of a bond between any of the four parts locates the fracture plane. A number is then assigned to each fracture pattern (Reprinted with permission from Hertel R, Hempfing A, Stiehler M, Leunig M (2004). Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg.; 13: 427–33. doi:10.1016/j.jse.2004.01.034)
Postoperatively, a perpendicular anteroposterior (1.2-m distance from X-ray source from the shoulder with a beam magnification of 10 %) and an axillary radiograph (10 % of beam magnification) were obtained. Fracture stability at the end of surgery was consistently evaluated by testing abduction with external and internal rotation of the arm under fluoroscopy (Video). On radiographs, the accuracy of fracture reduction was assessed following the criteria of Bahrs et al. [21], i.e. (i) greater tuberosity with a side-to-side difference distance <5 mm, (ii) no excessive varus or valgus (±15°) of the head fragment on the anteroposterior view and (iii) no increased retro- or antetorsion (±15°) on the axillary view. To evaluate the quality of the reduction, a score 0 was assigned if all three criteria were satisfied (excellent) and a score 1 was given if two of the three criteria were met (good), while a score 2 (fair) or 3 (poor) were assigned if one or no criteria, respectively, were satisfied. The same criteria were used to classify the accuracy of reduction at the final follow-up (12 months).
Operative and postoperative treatment
After applying the Humerusblock according to the technique of Resch [12], reduction of displaced fractures by manipulation was consistently attempted. When we did not succeed, the varus/valgus deviation of the humeral head was corrected using a blunt elevator introduced percutaneously to push the head as much as possible laterally or medially (Fig. 2). Reduction of the greater tuberosity was carried out with a hook to grasp the cuff tendons and relocate the tuberosity in the correct position. Fixation of tuberosity, when necessary, was achieved with one cannulated screw introduced with a craniocaudal and lateromedial direction as far as to transfix the uppermost medial cortex of the humeral diaphysis.
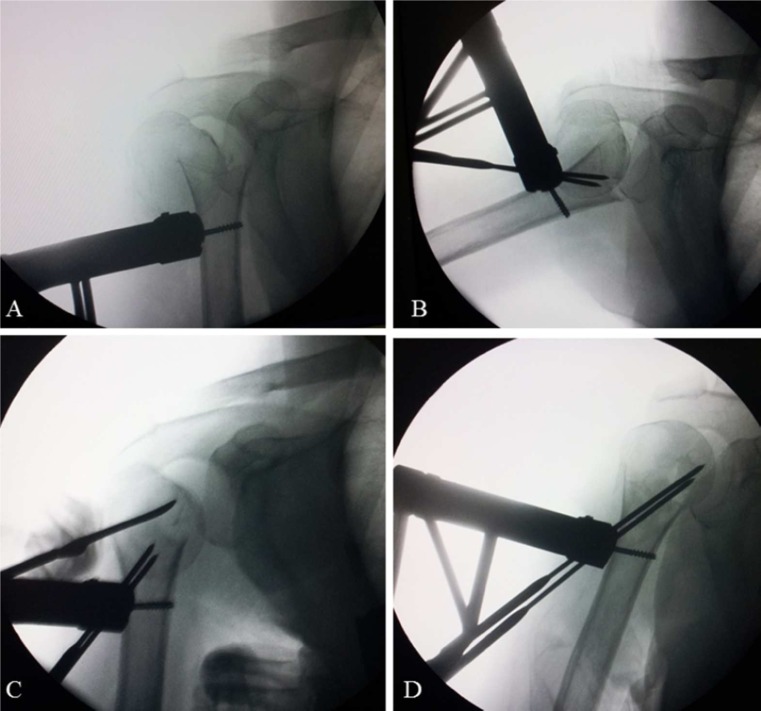
Fig. 2.
The operative steps to implant the Humerusblock. a The block is fixed to the proximal third of the humeral diaphysis with a cannulated 4-mm screw. b The two 2.5-mm K-wires passing through the block are pulled to the fracture line. c The varus/valgus deviation of the humeral head is corrected using a blunt elevator introduced percutaneously to push the head as much as possible laterally or medially. d The K-wires are pulled to the subchondral bone
After surgery, a sling was applied with the arm in internal rotation for two weeks. Then, pendulum exercises and passive assisted exercises were begun. Active exercises were allowed at four weeks after surgery.
Assessment of sintering and varus/valgus inclination of humeral head
All images were examined on diagnostic quality liquid crystal display monitors using DICOM (Digital Imaging and Communication in Medicine) compliant grading software (IMPACS Web 1000; Agfa, Mortsel, Belgium).
To evaluate the sintering, an accurate true perpendicular anteroposterior radiograph (1.2-m distance from X-ray source from the shoulder with a beam magnification of 10 %) of the shoulder was obtained in the operating room immediately after surgery with the patient still under general anaesthesia. On this radiograph, the distance between the tip of the most cranial K-wire and the humeral articular surface was calculated and noted by tracing a line in continuation with that K-wire (Fig. 3). Since the Humerusblock has a width (lateral-to-medial) of 12 mm, the following proportion was made: [Measured width of the Humerusblock (mm): 12 mm (real width of the Humerusblock in mm) = Measured distance (mm) of the K-wire tip from the articular surface: X]. We thus obtained the distance in millimetres (X) from the tip of the most cranial K-wire to the humeral articular surface on the anteroposterior view. The same measurement was performed three months after surgery or when we had to remove the Humerusblock, which was carried out when radiographs showed fracture healing and, in any case, never before eight weeks. By comparing the measurements made on the immediate postoperative and the three-month follow-up radiographs (carried out with the same technique by the same radiologist), the degree of head impaction was assessed.
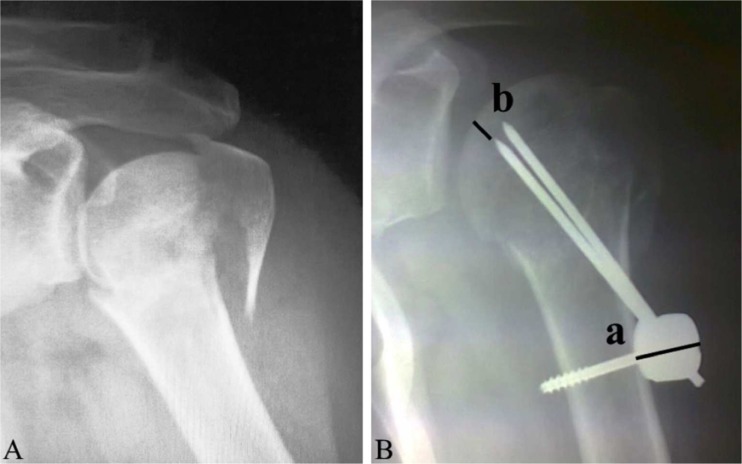
Fig. 3.
Measurement of the amount of humeral head impaction. Three-part fracture before (A) and after reduction (B). On the postoperative radiograph, the distance between the tip of the most cranial K-wire and the humeral articular surface is measured by a line that continues the direction of the K-wire. [Measured width of the Humerusblock (mm): 12 mm (real width of the Humerusblock) = Measured distance of the K-wire tip from the articular surface (mm): X]. a Width of the Humerusblock. b Distance of the K-wire tip from the articular surface
The cervico-diaphyseal angle was assessed according to Hertel et al. [22], by measuring, on the perpendicular anteroposterior radiograph, the angle formed by the intersection of the axis of the proximal humerus and the line perpendicular to the anatomic neck. An angle of 130–140° was considered to correspond to an adequate fracture reduction. Then, a radiograph at 12-month follow-up was done to assess final varus/valgus deviation.
Clinical evaluation of patients was done using the Constant score [23] method at six- and 12-month follow-up.
Statistical analysis
According to a minimal clinically important difference estimate of 10.4 points in patients undergoing rotator cuff surgery [24], the power calculation detected a significant difference in total Constant score of 60 at six months and 70.4 at 12-months follow-up with an SD of 12, assuming a two-tailed α value of 0.05 (sensitivity 95 %) and a β value of 0.95 (study power 95 %); we determined that at least 20 patients were required at follow-up evaluation (G power3 power analysis program).
A separate investigator collected the data, and the statistical analysis was then performed with SPSS software, version 16.0 (SPSS, Chicago, IL).
X-ray images were studied and interpreted by three orthopaedic surgeons with different skills in shoulder surgery (senior and expert surgeon; assistant to shoulder surgery; resident with particular interest in shoulder surgery) three times per examiner. The intra- and inter-observer agreement was determined using the κ statistic, with the level of significance set a priori at P < 0.01. Interpretation of the κ statistic was performed as described by Landis and Koch in 1977. Agreement was considered excellent if κ fell between 0.81 and 1.0, high if κ was between 0.61 and 0.80, moderate if κ was 0.41 to 0.60, fair if κ was 0.21 to 0.40, and poor if κ was 0.20 or less [25].
The Fisher’s exact test was used to compare the proportions and the Student t-test for average values. P-values <0.05 were deemed to be statistically significant.
Potential correlations between independent preoperative variables (age, sex, Codman-Lego classification, varus/valgus inclination, flexion/extension of the head with respect to the diaphysis, length of calcar attached to the head > or < of 8 mm, calcar dislocation with respect to the diaphysis < or > 2 mm, metaphyseal comminution), postoperative variable (additional screw beyond the Humerusblock, initial distance of the K-wire from the articular surface, accuracy of fracture reduction, Constant score) and amount of head impaction were calculated with the Spearman’s correlation coefficient. The ANOVA method was used to assess differences in the cervico-diaphyseal angle between immediate postoperative and final follow-up radiographs. The nominal and ordinal variables were summarized as percentages.
Results
Forty-three fractures were available for the study since three patients were lost at the final follow-up. There were 36 females and seven males, with a mean age of 69.9 years (range 29–88) at the time of injury. The dominant side was involved in 33 cases. Fracture patterns are reported in Table 1. A Humerusblock device without additional hardware was applied in 21 cases (48.9 %). In the remaining patients, fixation of the greater tuberosity was performed with one cannulated screw in 22 cases (51.1 %). The mean operative time was 50.2 minute (range, 20–120) and the mean fluoroscopy time was 40 second (range, 15–100).
Table 1.
Fracture details
| Characteristics | Patterns | Number of cases (%) |
|---|---|---|
| Codman Hertel (Lego System) | 1 | 8 (18.6 %) |
| 7 | 27 (62.79 %) | |
| 12 | 7 (16.27 %) | |
| Head split | 1 (2.3 %) | |
| Varus/valgus | Valgus | 18 (41.86 %) |
| Varus impacted | 16 (37.2 %) | |
| Varus disrupted | 9 (20.9 %) | |
| Flex/extension | Neutral | 34 (79.06 %) |
| Flexion | 3 (6.97 %) | |
| Extension | 6 (13.95 %) | |
| Metaphyseal extension | >8 mm | 12 (27.9 %) |
| <8 mm | 31 (72.09 %) | |
| Medial hinge dislocation | <2 mm | 23 (53.48 %) |
| >2 mm | 20 (46.51 %) | |
| Metaphyseal comminution | Yes | 6 (13.95 %) |
| No | 37 (86.04 %) |
Intra- and inter-tester agreement were 0.71 (CI, 0.663–0.778) and 0.62 (CI, 0.592–0.756), respectively. The results show that there is a high intra- and inter-tester agreement. Reported results are those obtained by the expert surgeon.
Fracture reduction was excellent in 22 cases (51.16 %) (Fig. 3), good in 13 (30.23 %) (Fig. 4), fair in five (11.62 %) (Fig. 5) and poor in three (6.97 %).
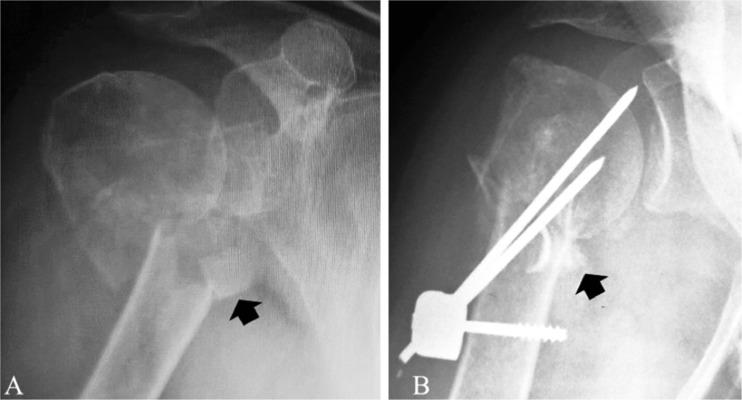
Fig. 4.
An 88-year-old female patient with a type 7 fracture (Codman-Lego classification) showing severe impaction, with perforation of the humeral head, without significant change in varus/valgus inclination. a Pre-operative radiograph. b Immediate postoperative radiograph showing an excellent reduction. c and d Anteroposterior and axial radiographs obtained one month after surgery. e Radiograph taken four months after surgery, after removal of the Humerusblock. The final radiographic result was rated as good
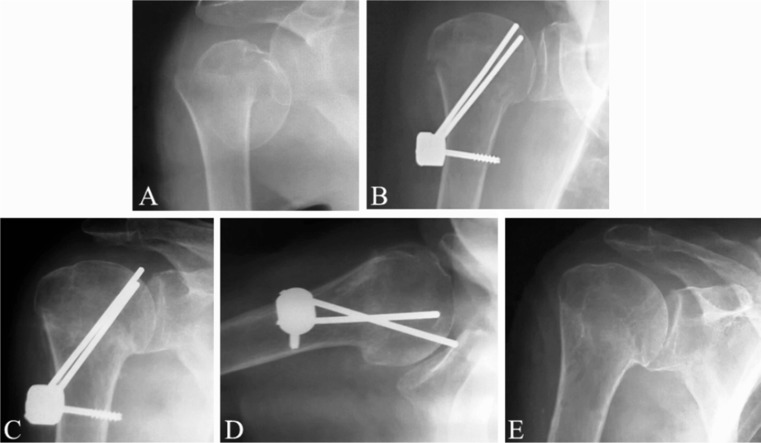
Fig. 5.
An 83-year-old female with a type 12 fracture (Codman-Lego classification) with metaphyseal comminution and complete calcar separation from head and diaphysis, indicated by the arrow (a). Two months after surgery (b) the head exhibits severe impaction, perforation of humeral articular surface by K-wires and varus angulation, with fair final result
The mean initial post-operative distance of the most cranial K-wire to the articular surface was 3.1 mm (range, 0–5, SD 2.8).
The mean sintering of the humeral head was 3.9 mm (range 0–8 mm, SD 3.5). The amount of impaction was correlated to the patient’s age (p = 0.02) and sex (p = 0.031), with the degree of sintering higher in patients older than 50 years and in females. A correlation was also found with the Codman-Lego classification [19], the greatest sintering being found in type 12 (p = 0.04) and type 7 (p = 0.049) fractures, with varus impacted (p = 0.048), and varus disrupted (p = 0.039) fractures and, particularly, with the fractures exhibiting metaphyseal comminution (six cases, 13.95 %) (Fig. 5), which showed by far the highest amount of sintering (with a mean of 6.5 mm, p < 0.001). Other fracture patterns did not reach statistically significant differences (Table 2). The use of additional screws beyond the Humerusblock, the initial distance of the K-wire from the articular surface (with a maximum of 5 mm) and accuracy of fracture reduction did not reach statistically significant differences.
Table 2.
Correlation between patients’ demographic data, fracture patterns and amount of impaction of the humeral head
| Patients’ demographic data | Amount of impaction (mean in mm) | p-value (correlation) | |
|---|---|---|---|
| Age | <50 years | 2.5 | 0.4 |
| >50 years | 4.8 | 0.02 | |
| Sex | M | 2.7 | 0.8 |
| F | 4.3 | 0.031 | |
| Fracture patterns | |||
| Codman-Lego | 1 | 2 | 0.65 |
| 7 | 4.7 | 0.049 | |
| 12 | 5.3 | 0.04 | |
| Varus/valgus | Valgus | 2.8 | 0.68 |
| Varus impacted | 4.1 | 0.048 | |
| Varus disrupted | 5.5 | 0.039 | |
| Flex/extension | Neutral | 3.8 | 0.1 |
| Flexion | 3.5 | 0.07 | |
| Extention | 4 | 0.07 | |
| Metaphyseal extension | >8 mm | 3.7 | 0.059 |
| <8 mm | 4.1 | 0.055 | |
| Medial hinge dislocation | <2 mm | 3.3 | 0.07 |
| >2 mm | 4.3 | 0.053 | |
| Metaphyseal comminution | Yes | 6.3 | <0.001 |
| No | 3.2 | 0.8 | |
The postoperative cervico-diaphyseal angle ranged from 130° to 140° in 35 cases (81.39 %), with residual valgus or varus inclination in five and three cases, respectively, the mean angle being 134° (range, 115–145°, SD 7). At 12-month follow-up, the cervico-diaphyseal angle was 130–140° in 31 cases (72.09 %, p = 0.058), with loss of reduction of less than 10° in four patients (9 %), in two of whom in varus and in the other two in valgus. Each of the four patients with loss of reduction had metaphyseal comminution.
The Humerusblock was removed in 18 cases (41.8 %) because of K-wires perforation of the humeral head. In only one case, the block of the device caused local discomfort and was removed. All fractures appeared to be healed after eight weeks of surgery. The radiographic result at the latest follow-up was excellent in 20 (46.5 %), good in 13 (30.2 %), fair in six (13.9 %), poor in four (9.3 %) cases.
At six-month follow-up, the mean Constant score was 60 (48–75, SD ±11), while at 12-month follow-up it was 73 (60–95, SD ±12) (p = 0.031). A negative statistically significant correlation was found between amount of sintering and Constant score both at six- (p = 0.032) and 12- (p = 0.047) month follow-up.
Discussion
Fractures of the proximal humerus may undergo proximo-distal impaction of the humeral head with possible loss of reduction after surgical fixation, particularly in osteoporotic patients. This has previously been described by Gardner et al. [17] and Soldberg et al. [18] in factures treated with locking plates and multiple humeral head screws. However, in contrast to locking plates, the K-wires locked into the Humerusblock follow the direction of the load peaks on the humeral head, thus allowing a controlled impaction while keeping the inclination of the head with respect to the diaphysis in a range of 132–142°, which is the anatomic range of the cervico-diaphyseal angle [22].
In our patients, the mean initial post-operative distance of the most cranial K-wire to the articular surface was 3.1 mm, with a maximum of 5 mm, and mean impaction of the humeral head was 3.9 mm. The satisfactory fracture reduction (excellent or good), obtained in 81 % of patients at surgery, was maintained in 90 % of those patients. Overall, only 9 % of cases had a loss of reduction, of less than 10°, and each of these cases showed metaphyseal comminution. These results demonstrate that the Humerusblock is a valuable device for fixing proximal humerus fractures, being also a minimally-invasive tool that requires a limited surgical and fluoroscopy time, but it is not able to control fracture impaction and reduction in case of metaphyseal comminution. The main drawback of the device is the so-called “sintering effect” [16], since a considerable fragment impaction may lead to early implant removal due to humeral head perforation by K-wires, a complication that occurred in 41 % of our cases. This figure is similar to those found in the previously reported studies. Bogner et al. [5], who operated on 48 patients aged 70 years or more, had K-wire perforation of the humeral head in 25 % of cases. Of the 34 patients of Vundenlinckx et al. [14], seven underwent early perforation by one or two K-wires (20.58 %). Brunner et al. [15] had to remove the implant prematurely in 40 % of cases. Recently, an alternative method has been proposed to avoid the need of implant removal, which does not provide the use of the block and of the K-wire [26]; on the other hand, we believe that the proposed method is not suitable for displaced fracture, as we had in our 46 cases. Pre-operatively, it is important to inform patients about the possible sintering, its negative effect on final result and about the possible need of a prompt removal, especially in those cases having the risk factors for sintering. Fracture exhibiting metaphyseal comminution should not be treated with the Humerusblock because of high sintering amount with secondary loss of reduction and fair final clinical results.
In no study reporting on the postoperative impaction in fractures of the upper humerus, a method of measuring the sintering effect has been described. Using DICOM imaging software, we conceived a method to determine the distance from the tip of the most cranial K-wire to the cortical bone of the humeral head, which may allow the safe distance for the introduction of the wire in the humeral head to be determined. However, the measurements are done on a perpendicular anteroposterior radiograph of a structure, such as the humeral head, that is semispherical and retroverted. Hence, to obtain the real distance from the tip of the K-wires to the articular surface, we would have to perform a CT scan immediately after surgery and at each follow-up, but this was not done due to ethical reasons. Nonetheless, the 12-mm width of the block represents a reference for a reliable measurement of impaction by means of a simple ratio. However, based on our measurements, it is conceivable that a maximum distance of 5 mm may be considered a safe distance between the tip of the K-wire and the surface of the humeral head. Assuming such maximum distance, it is likely that the majority of perforations of the head would not occur and it should be good enough to have a satisfactory grip on the subcondral bone of the humeral head. Unfortunately, it is not possible, at surgery, to measure exactly this safe distance on the screen of the amplioscope due to the magnification of the anatomical images. However, since 5 mm represent 41 % of the width of the metallic block fixed to the humeral diaphysis as seen on the anteroposterior view, such distance can be calculated with close approximation, using the block as a reference to adjust all measurements.
When using the Humerusblock (alone or with additional hardware) or other similar devices [27], reduction of the fracture is made with closed manoeuvres or minimally invasive tools. Thus, it may be even very difficult to restore the anatomy of the proximal humerus. The reported relative contraindications for closed reduction are severe osteoporosis, tuberosity comminution, medial calcar comminution or irreducible head-calcar displacement resulting in varus position of the head, displaced four-part fractures and non-acute fractures (>14 days) [28]. In this study, we report on 43 patients, most of whom had relative contraindications. Nevertheless, excellent or good reductions based on the criteria of Bahrs et al. [21] were obtained in 81 % of cases, a figure which compares well with the results of other authors [5]. The use of the screw for the tuberosity did not influence amount of impaction. The patients with the greatest sintering (up to 8 mm) and partial loss of reduction were females in older age and those with a high number of fragments, and, especially, with metaphyseal comminution. The latter condition was particularly challenging when the calcar appeared completely separated from the head and the diaphysis. This condition has been called “the fifth fragment”, and it should be considered as an additional unfavourable factor for reduction and fracture stability [29]. These cases, which were found to be the most unstable, more prone to severe sintering and with fair clinical results, should not be selected for minimally invasive fixation.
Humeral head post-traumatic avascular necrosis is a relevant issue in treatment of proximal humerus fracture. Due to the short time of follow-up of this study, we could not assess the rate of this complication. As Gerber et al. [30] stated, we believe that in case of avascular necrosis, it is the deformity rather than necrosis that causes disability. Therefore, the risk of avascular necrosis does not influence our decision making in terms of treatment. In addition, the minimally-invasive approach to implant the Humersublock device preserves the remaining vascular supply, with reported limited cases (5 %–10 %) of avascular necrosis in longer-term follow-up studies [5, 12, 14, 15]. This study has potential limitations that need to be assessed. First, the measurements are made on a plane antero-posterior radiograph with possible implant error positioning; also, there is possible unpredictable position of the K-wire from the articular surface in the antero-posterior view, due to implant positioning, to the semi-spherical anatomy of the proximal humerus and to the retrotorsion of the humeral head [22]. To obtain the real distance, we would have performed CT scans at each control, which is not possible in clinical and ethical practice. In any case, the width of the block of 12 mm represents a reference to adjust all measurements, with a reproducible quantification of the measured impaction by mean of a simple ratio. A further and related limitation is that it is difficult to obtain exactly the same antero-posterior view at different controls, even if obtained by the same technique and radiologist, and with three different researchers calculating the distances three times each, with possible modifications of the measurements. Again, it can be adjusted according to the use of the above reported ratio. Another limitation is the three-month follow-up for calculating sintering, because about 40 % of the Humerusblock was removed at that time. Anyway, varus/valgus deviation and clinical results were obtained at one-year of follow-up, which seems to be a reasonable time to correlate clinical results and impaction of the head, which occurs in the first weeks after surgery.
Conclusions
Postoperative impaction of the humeral head may allow the K-wires of the Humerusblock to perforate the cortex of the head, which occurred in 41 % of our patients, who needed prompt removal of the implant. An original method was used to calculate the amount of postoperative impaction of the head, which was 3.9 mm on average. A maximum distance of 5 mm between the tip of the most cranial K-wire and the cortex of the humeral head is probably safe enough as to avoid perforation of the head in most patients treated with the Humerusblock without predisposing to post-operative loss of reduction. The sintering effect varied considerably depending on the patient’s age and sex, fracture pattern according to the Codman-Lego classification system, varus/valgus deviation of the head and, particularly, metaphyseal comminution. Calcar separation from head and diaphysis should be carefully evaluated pre-operatively because it negatively affects fracture reduction and fixation, and it favours impaction of the humeral head with poorer clinical results. Pre-operatively, it is important to inform patients about the possible impaction of the head and about the possible need for a prompt removal, especially in those cases having the risk factors for sintering.
Electronic supplementary material
(WMV 5294 kb)
Acknowledgments
Conflict of interest
No support and disclaimer to declare.
Footnotes
IRB: In light of the Italian law, the authors are not required to have this type of study approved. However, each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Roux A, Decroocq L, El BAtti S, Bonnevialle N, Moineau G, Trojani C, Boileau P, de Peretti F. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res. 2012;98:715–719. doi: 10.1016/j.otsr.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 2.Fankhauser F, Boldin C, Schippinger G, Haunschmid C, Szyszkowitz R. A new locking plate for unstable fractures of the proximal humerus. Clin Orthop Relat Res. 2005;430:176–181. doi: 10.1097/01.blo.0000137554.91189.a9. [DOI] [PubMed] [Google Scholar]
- 3.Rouleau DM, Laflamme GY, Berry GK, Harvey EJ, Delisle J, Girard J. Proximal humerus fractures treated by percutaneous locking plate internal fixation. Orthop Traumatol Surg Res. 2009;95:56–62. doi: 10.1016/j.otsr.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 4.Spross C, Platz A, Erschbamer M, Lattmann T, Dietrich M. Surgical treatment of Neer Group VI proximal humeral fractures: retrospective comparison of PHILOS® and hemiarthroplasty. Clin Orthop Relat Res. 2012;470:2035–2042. doi: 10.1007/s11999-011-2207-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bogner R, Hubner C, Matis N, Auffarth A, Lederer S, Resch H. Minimally-invasive treatment of three- and four-part fractures of the proximal humerus in elderly patients. J Bone Joint Surg (Br) 2008;90:1602–1607. doi: 10.1302/0301-620X.90B12.20269. [DOI] [PubMed] [Google Scholar]
- 6.Resch H, Beck E, Bayley J. Reconstruction of valgus impacted humeral head fractures—indication, technique and long term results. J Shoulder Elbow Surg. 1995;4:73–80. doi: 10.1016/S1058-2746(05)80071-1. [DOI] [PubMed] [Google Scholar]
- 7.Owsley KC, Gorczyca JT. Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures [corrected] J Bone Joint Surg Am. 2008;90:233–240. doi: 10.2106/JBJS.F.01351. [DOI] [PubMed] [Google Scholar]
- 8.Südkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, Luo C, Plecko M, Wendt K, Köstler W, Konrad G. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am. 2009;91:1320–1328. doi: 10.2106/JBJS.H.00006. [DOI] [PubMed] [Google Scholar]
- 9.Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2011;22:542–549. doi: 10.1016/j.jse.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 10.Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011;42:1283–1288. doi: 10.1016/j.injury.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 11.Tepass A, Blumenstock G, Weise K, Rolauffs B, Bahrs C. Current strategies for the treatment of proximal humeral fractures: an analysis of a survey carried out at 348 hospitals in Germany, Austria, and Switzerland. J Shoulder Elbow Surg. 2013;22:e8–e14. doi: 10.1016/j.jse.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 12.Resch H, Hubner C, Schwaiger R. Minimally invasive reduction and osteosynthesis of articular fractures of the humeral head. Injury. 2001;32:25–32. doi: 10.1016/S0020-1383(01)00058-4. [DOI] [PubMed] [Google Scholar]
- 13.Bergmann G, Graichen F, Bender A, Kääb M, Rohlmann A, Westerhoff P. In vivo glenohumeral contact forces–measurements in the first patient 7 months postoperatively. J Biomech. 2007;40:2139–2149. doi: 10.1016/j.jbiomech.2006.10.037. [DOI] [PubMed] [Google Scholar]
- 14.Vundelinckx BJ, Dierickx CA, Bruckers L, Dierickx CH. Functional and radiographic medium-term outcome evaluation of the Humerus Block, a minimally invasive operative technique for proximal humeral fractures. J Shoulder Elbow Surg. 2012;21:1197–1206. doi: 10.1016/j.jse.2011.07.029. [DOI] [PubMed] [Google Scholar]
- 15.Brunner A, Weller K, Thormann S, Jöckel JA, Babst R. Closed reduction and minimally invasive percutaneous fixation of proximal humerus fractures using the Humerusblock. J Orthop Trauma. 2010;24:407–413. doi: 10.1097/BOT.0b013e3181c81b1c. [DOI] [PubMed] [Google Scholar]
- 16.Resch H. Proximal humeral fractures: current controversies. J Shoulder Elbow Surg. 2011;20:827–832. doi: 10.1016/j.jse.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 17.Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG. The importance of the medial support in locked plating of proximal humerus fracture. J Orthop Trauma. 2007;21:185–191. doi: 10.1097/BOT.0b013e3180333094. [DOI] [PubMed] [Google Scholar]
- 18.Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical treatment of three and four-part proximal humeral fractures. J Bone Joint Surg Am. 2009;91:1689–1697. doi: 10.2106/JBJS.H.00133. [DOI] [PubMed] [Google Scholar]
- 19.Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004;13:427–433. doi: 10.1016/j.jse.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 20.Majed A, Macleod I, Bull AM, Zyto K, Resch H, Hertel R, Reilly P, Emery RJ. Proximal humeral fracture classification systems revisited. J Shoulder Elbow Surg. 2011;20:1125–1132. doi: 10.1016/j.jse.2011.01.020. [DOI] [PubMed] [Google Scholar]
- 21.Bahrs C, Rolauffs B, Dietz K, Eingartner C, Weise K. Clinical and radiological evaluation of minimally displaced proximal humeral fractures. Arch Orthop Trauma Surg. 2010;130:673–679. doi: 10.1007/s00402-009-0975-9. [DOI] [PubMed] [Google Scholar]
- 22.Hertel R, Knothe U, Ballmer FT. Geometry of the proximal humerus and implications for prosthetic design. J Shoulder Elbow Surg. 2002;11:331–338. doi: 10.1067/mse.2002.124429. [DOI] [PubMed] [Google Scholar]
- 23.Constant CR, Murley AHG. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 24.Kukkonen J, Kauko T, Vahlberg T, Joukainen A, Aärimaa V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J Shoulder Elbow Surg. 2013;22:1650–1655. doi: 10.1016/j.jse.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Landis JR, Koch GC. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 26.Roberts VI, Komarasamy B, Pandey R. Modification of the Resch procedure: a new technique and its results in managing three- and four-part proximal humeral fractures. J Bone Joint Surg (Br) 2012;94:1409–1413. doi: 10.1302/0301-620X.94B10.28692. [DOI] [PubMed] [Google Scholar]
- 27.Carbone S, Tangari M, Gumina S, Postacchini R, Campi A, Postacchini F. Percutaneous pinning of 3-or 4-part fractures of proximal humerus in elderly patients in poor general conditions: MIROS® versus traditional pinning. Int Orthop. 2012;36:1267–1273. doi: 10.1007/s00264-011-1474-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Galatz LM, Kim HM. Minimally invasive techniques for proximal humerus fractures. In: Iannotti JP, Willams GR, editors. Disorders of the shoulder. 2. Philadelphia: Lippincott Willams & Wikkins; 2007. pp. 873–888. [Google Scholar]
- 29.Russo R, Cautiero F, Della Rotonda G. The classification of complex 4-part humeral fractures revisited: the missing fifth fragment and indications for surgery. Musculoskelet Surg. 2012;96(Suppl 1):S13–S19. doi: 10.1007/s12306-012-0195-2. [DOI] [PubMed] [Google Scholar]
- 30.Gerber C, Hersche O, Berberat C. The clinical relevance of posttraumatic avascular necrosis of the humeral head. J Shoulder Elbow Surg. 1998;7:586–590. doi: 10.1016/S1058-2746(98)90005-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(WMV 5294 kb)