Abstract
Purpose
Stem version is not always equivalent to femoral neck version (native version) in cementless total hip arthroplasty (THA). We therefore examined the discrepancy of version between the native femoral neck and stem using pre- and postoperative computed tomography (CT), the level of the femur where the canal version most closely fit the stem version, and the factors influencing version discrepancy between the native femoral neck and stem.
Methods
A total of 122 hips in 122 patients who underwent primary THA using a metaphyseal-fit stem through the postero-lateral approach were included. Pre- and postoperative CT images were utilized to measure native and stem version, and the version of the femoral canal at four levels relative to the lesser trochanter.
Results
The mean native and stem versions were 28.1 ± 11.0° and 38.0 ± 11.2°, respectively, revealing increased stem version with a mean difference of 9.8° (p < 0.0001). A total of 84 hips (68.9 %) revealed an increase in version greater than 5°. Femoral canal version at the level of the lesser trochanter most closely approximated that of stem version. Among the factors analysed, both univariate and multivariate analysis showed that greater degrees of native version and anterior stem tilt significantly reduced the version discrepancy between the native femoral neck and stem version.
Conclusions
Since a cementless stem has little version adjustability in the femoral canal, these findings are useful for surgeons in preoperative planning and to achieve proper component placement in THA.
Keywords: Stem version, Femoral neck version, Total hip arthroplasty, Implant placement
Introduction
Accurate component placement is considered a necessity in successful total hip arthroplasty (THA) [1, 2], as implant malposition directly influences postoperative stability, wear, and aseptic loosening [3, 4]. The generally accepted combined anteversion has been reported to be from 30° to 60° to avoid impingement and maximize hip range of motion [5, 6]. The risk of dislocation is reportedly 6.9 times greater if the combined anteversion falls outside the range of 40° to 60° [7].
Femoral and stem version has a wide variability. Femoral version was reported to range from −15° to 35° in normal hips [8, 9]. Stem version was also reported to have a wide range: 30° retroversion to 45° anteversion [10, 11]. Therefore, surgeons should understand precise version pre- or intra-operatively as well as cup version in order to achieve the proper component placement in THA. It is important to note that stem version is not always equal to femoral neck version. A review of the literature revealed some discrepancy in the version between the femoral neck and stem. These studies were limited in that they used fluoroscopy and the contralateral side as a reference [12–14]. The accuracy of version measurement was questionable compared to that of computed tomography (CT), thought to be the most accurate method currently available [9].
In this study, we examined the discrepancy of version between the native femoral neck and stem, the level of the femur where the canal version most closely fit the stem version, and the factors influencing version discrepancy using pre- and postoperative CT.
Patients and methods
This study was approved by the institutional review board. This study includes 122 hips in 122 patients who underwent primary cementless THA between April 2010 and May 2013. Indications for THA included osteoarthritis (OA) of the hip in 110 hips, rheumatoid arthritis (RA) in four hips, and osteonecrosis of the femoral head (ONFH) in eight hips. The mean age at operation was 65.8 ± 8.5 years (range, 42–79 years). There were 99 women (99 hips) and 23 men (23 hips); there were 110 hips with OA (Table 1).
Table 1.
Patient characteristics and radiographic data
| Patient characteristics | Value |
|---|---|
| Total number of hips | 122 hips |
| Age (years) | 65.8 ± 8.5 (42–79)a |
| Male | 23 hips (18.9 %) |
| Female | 99 hips (81.1 %) |
| Body mass index (kg/m2) | 24.4 ± 3.7 (15.1–36.9)a |
| Osteoarthritis (DDH/non-DDH) | 110 hips (90.2 %) |
| DDH | 86 hips (70.5 %) |
| Non-DDH | 24 hips (19.7 %) |
| Rheumatoid arthritis (RA) | 4 hips (3.3 %) |
| Osteonecrosis of the femoral head (ONFH) | 8 hips (6.6 %) |
| Radiographic and CT data | |
| Native version | 28.1 ± 11.0° (0.7–61.6)a |
| Stem version | 38.0 ± 11.2° (14–63.2)a |
| Acetabular version | 17.5 ± 10.4° (−5.4–36.8)a |
| Combined anteversion | 55.7 ± 11.4° (26.8–86.1)a |
| Height of the stem (mm) | 30.7 ± 6.4 (18.7–58.5)a |
| Sagittal tilt | 0.3 ± 1.7° (−3.4–3.8)a |
| Coronal tilt | 0.1 ± 0.9° (−1.9–2.1)a |
aMean ± SD (range)
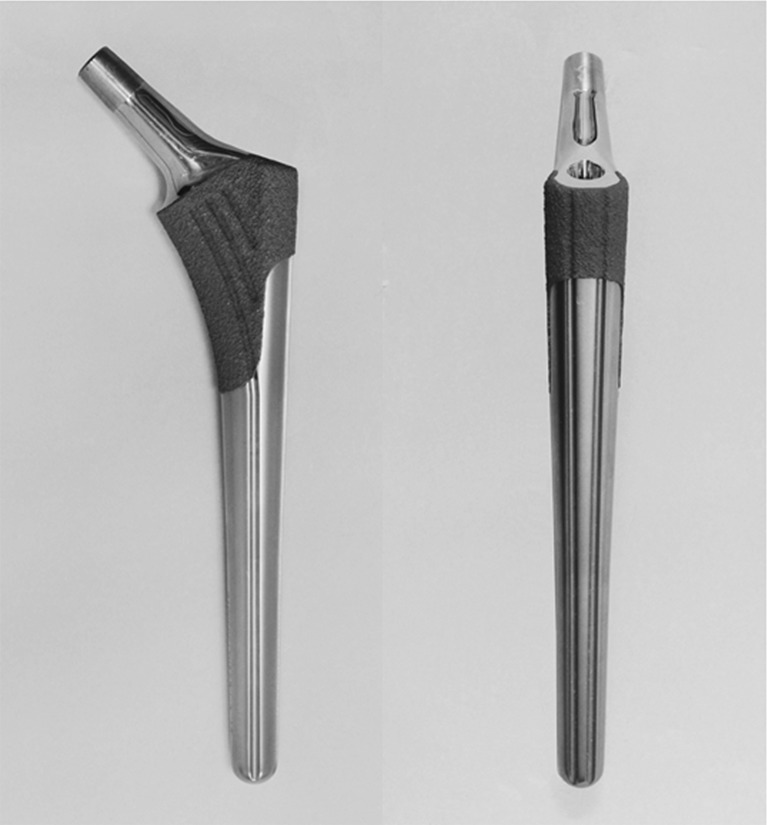
Each operation was performed using a posterolateral approach. A cementless hemispherical press fit cup and a straight metaphyseal fit stem (AMS & PerFix HA; Kyocera Medical, Osaka, Japan) were used in all cases (Fig. 1) [15, 16]. Two or three screws were inserted to augment cup fixation in most cases.
Fig. 1.
Coronal (left) and sagittal (right) views of the cementless metaphyseal fit femoral stem (PerFix HA, JMM)
All CT scans were performed with every patient supine and symmetrically positioned in the scanner as shown by the scout views. After downloading the scan data in the Digital Imaging and Communications in Medicine format (DICOM; NEMA [National Electrical Manufacturers Association], Rosslyn, Virginia) onto a personal computer, each measurement was performed using image processing and analysis software (3D Template; Kyocera Medical) [17, 18]. The scans included the pelvis, proximal femur, and knee.
Measurement of each parameter
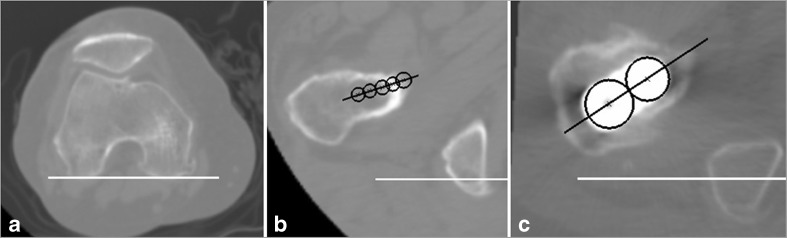
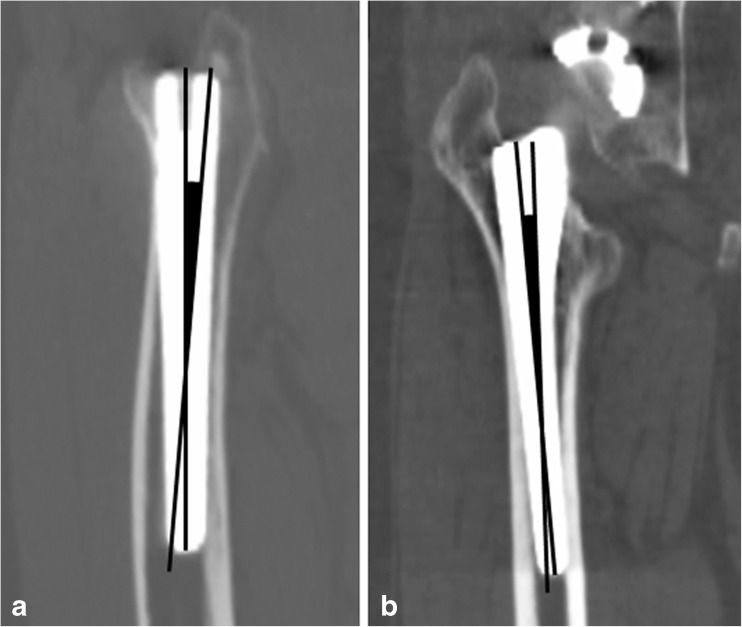
Native version was defined as the angle between the axis of the femoral neck and a line connecting the posterior aspect of the medial and lateral femoral condyles (posterior condylar line) (Fig. 2a and b) [19]. The femoral neck axis was calculated as a best-fit line connecting slices taken through a central segment of the neck. Stem version was calculated as the angle of the prosthetic femoral neck relative to the posterior condylar line (Fig. 2a and c) [20]. When the native or stem version indicated a superior position in reference to the posterior condylar line, it was defined as positive version. Cup version was defined as the operative anteversion following the method of Murray [21]. The discrepancy between native and stem version was calculated as the value subtracting the native version from the stem version (Sv–Nv). The version of the femoral canal was measured at four levels: the 35 % level (35 % of the head center height above the center of the lesser trochanter [CLT]), the CLT level, the −35 % level (35 % of the head centre height below the CLT), and at the level of the canal isthmus [22]. We compared stem version to canal version and estimated the level where the value of canal version most closely approximated the stem version. The height of the stem was defined as the distance from the stem neck–shoulder junction to the center of the lesser trochanter. Sagittal stem alignment was calculated from the angle between the stem axis and the proximal femoral axis in the sagittal plane (Fig. 3a) [23]. When the stem axis was anteriorly tilted compared to the proximal femoral axis, sagittal stem alignment was defined as having an anterior tilt. Anterior sagittal tilt was defined to be positive. Similarly, coronal stem alignment was calculated from the angle between the stem axis and the proximal femoral axis in the coronal plane (Fig. 3b). When the stem axis was varus or valgus compared to the proximal axis, valgus tilt was defined to be positive.
Fig. 2.
Measurement of the native and stem version. The axis of the femoral neck was calculated as the best-fit line in slices taken through a central segment of the neck. Native femoral version was defined as the angle formed between the axis of the neck and a line connecting the posterior aspect of the medial and lateral femoral condyles (a, b). A base line was defined as a line connecting the posterior aspect of the medial and lateral femoral condyles. Stem version was calculated as the angle of the prosthetic femoral neck relative to the posterior condyles of the knee (a, c)
Fig. 3.
Measurement of the stem alignment. Sagittal stem alignment (a). Coronal stem alignment (b). Sagittal stem alignment was calculated from the angle between the stem axis and the proximal femoral axis in the sagittal plane (a). Coronal stem alignment was calculated from the angle between the stem axis and the proximal femoral axis in the coronal plane (b)
All measurements using CT images were performed by one observer (MH) and were repeated in a blind manner during the course of two sessions at least one month apart. Intra-observer reliabilities, evaluated using intraclass correlation coefficients, were excellent (range, 0.980–0.994). Two observers (MH and DH) independently made CT measurements on the scans of the 20 randomly selected hips, and interobserver reliabilities, evaluated using interclass correlation coefficients, were also excellent (range, 0.886–0.968).
Statistical analysis
Descriptive statistics used means, standard deviation, and ranges. We determined the difference between the native and stem version using the paired t-test for paired samples assuming equal variance. The Student’s t-test was used to compare the discrepancy between males and females. The analysis of variance (ANOVA) was utilized for primary diagnoses. The simple linear regression analysis was used to compare the discrepancy between the other continuous parameters. The multivariable regression analysis was used to compare the discrepancy among every parameter. A significant difference was defined as a p-value < 0.05. Statistical analyses were performed using JMP Software (Version 9.0; SAS Institute, Cary, North Carolina).
Results
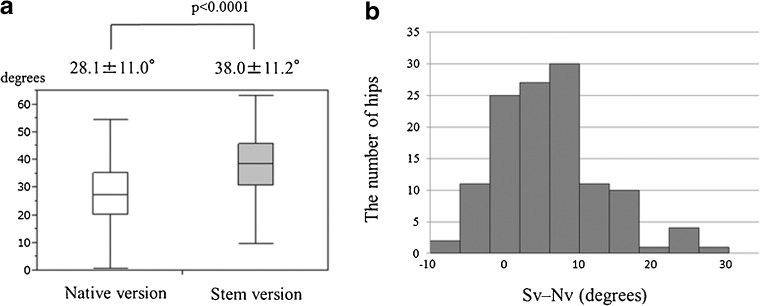
The mean native version was 28.1 ± 11.0° (range, 1–62°). The mean stem version was 38.0 ± 11.2° (range, 14–63°). The degree of stem version was significantly increased compared to the degree of native version with a mean difference (Sv–Nv) of 9.8 ± 8.8° (p < 0.0001) (Table 1) (Fig. 4a). Stem version was increased in 108 hips (88.5 %) by 1° or more, and in 84 hips (68.9 %) by 5° or more. Stem version was decreased in nine hips (7.4 %) by 1° or more, and in two hips (1.6 %) by more than 5° (Fig. 4b).
Fig. 4.
Comparison of native and stem version (a). The angle of stem version was significantly larger than the native version with a mean difference (Sv–Nv) of 9.0 ± 8.8° (p < 0.001). The bar line shows standard deviation. Distribution of the version discrepancy (Sv–Nv) (b). The discrepancy between native and stem version was calculated as the value subtracting the native version from the stem version
Femoral canal version at 35 % above the CLT, at the CLT, at 35 % below the CLT, and at the isthmus was 26.4 ± 10.5°, 37.9 ± 9.9°, 51.9 ± 9.8°, and 75.1 ± 5.7°, respectively, revealing posterior torsion of the canal from the distal isthmus towards the proximal metaphyseal level. Compared to stem version, there was a significant difference in version between the stem and femoral canal except at the CLT level. In other words, stem version most closely approximated canal version at the level of the CLT, with a mean difference of 0.1° (p = 0.8845) (Table 2).
Table 2.
Comparison of the version angle between the stem and femoral canal at each level
| Location | The mean major axis angle in the femoral canal | Stem version | Difference from mean stem version | p-value |
|---|---|---|---|---|
| At 35 % above CLT | 26.4 ± 10.5° | −11.6 ± 8.2° | < 0.0001 | |
| At CLT | 37.9 ± 9.9° | 38.0 ± 11.2° | −0.1 ± 8.4° | 0.8845 |
| At 35 % below CLT | 51.9 ± 9.8° | 13.9 ± 10.2° | < 0.0001 | |
| At the isthmus | 75.1 ± 5.7° | 36.8 ± 11.4° | < 0.0001 |
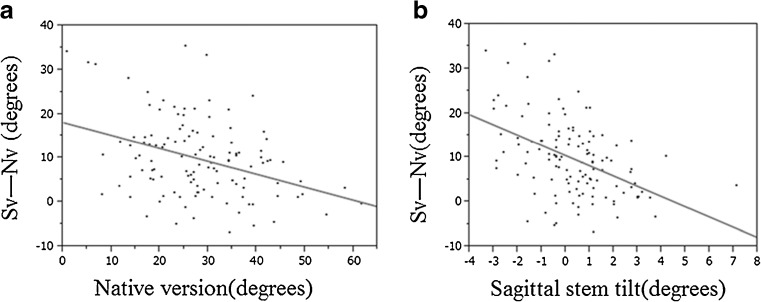
Among the factors analyzed, the native version and sagittal stem tilt significantly influenced the value of Sv–Nv using both univariate and multivariate analysis (Table 3). Increased native version resulted in decreased Sv–Nv (p < 0.0001). When native version increased by 1°, Sv–Nv decreased by 0.29° (Fig. 5a). Likewise, increased anterior stem tilt in the sagittal plane resulted in a decreased Sv–Nv (p < 0.0001). When the stem was tilted anteriorly in the sagittal plane by 1°, the Sv–Nv decreased by 2.3° (Fig. 5b). Although the mean degree of the Sv–Nv varied among the subgroups, no significant differences in Sv–Nv were noted among the individual primary diagnoses (Table 3).
Table 3.
Influencing factors for the Sv–Nv
| Parameter | p-value (univariate analysis) |
p-value (multivariate analysis) |
|---|---|---|
| Age | 0.9633 | 0.1796 |
| Sex | 0.5070 | 0.2382 |
| BMI | 0.5226 | 0.2077 |
| Primary diagnosis | 0.5983 | 0.6844 |
| DDH vs the other groups | 0.0512 | |
| DDH vs non-DDH | 0.1000 | |
| Crowe classification | 0.1468 | |
| (grade I/II vs III/IV) | ||
| Native version | < 0.0001a | < 0.0001a |
| Stem height | 0.8034 | 0.1634 |
| Sagittal stem tilt | < 0.0001a | < 0.0001a |
| Coronal stem tilt | 0.0219a | 0.2515 |
Fig. 5.
Correlation between Sv–Nv and native anteversion (a) and sagittal stem tilt (b)
The mean cup version was 17.5 ± 10.4° (range, −5–37°) and the mean combined anteversion was 55.7 ± 11.4° (range, 27–86°) (Table 1). No dislocations were observed during the study period.
Discussion
As native femoral version has a wide variability [8, 9, 24], surgeons need to place the components to optimize the combined anteversion of cup and stem [5–7]. Stem version is not always equivalent to femoral neck version. Therefore, we evaluated the degree of femoral neck version (native version) and stem (stem version) using pre- and postoperative CT in THA with a metaphyseal fit cementless stem, the level where the value of canal version most closely approximates stem version, and factors influencing version discrepancy.
In this study, the discrepancy between native version and stem version was found and stem version was, on average, generally larger than native version by 9.8°. Several authors have described the discrepancy between native and stem version ranging from 3° to 8° [12–14]. Suh et al. reported 3.8° using CT through estimations of the discrepancy between the contralateral native femoral version and stem version [13]. Emerson, using fluoroscopy, reported that stem version was greater than native version by 8.2° [14]. Although measurement methods and patient characteristics varied, the common finding was that the amount of stem version was greater than the amount of native version. This is in accordance with our results where an increase in version by greater than 5° was observed in about 70 % of hips compared to native version using pre- and postoperative CT. Only two hips (1.6 %) revealed a decrease in stem version greater than 5°.
Our results agree with previous studies in measuring gradual posterior torsion from the isthmus towards the femoral neck in the proximal femoral canal. Sugano et al. reported a difference of 12.6° on average between the CLT and femoral neck in the normal femur [22]. Therefore, stem version varied according to the level of the femur where the stem was located. In this study using a metaphyseal fit stem, the stem version most closely approximated canal version near the level of the CLT. These results indicate that version discrepancy may depend on the degree of version between the lesser trochanter and the femoral neck.
Native version was significantly and inversely correlated with version discrepancy (Table 3). When native version increased by 1°, the Sv–Nv decreased by 0.29° (Fig. 5a). Greater native version is accompanied with a smaller gradual posterior torsion from the isthmus towards the femoral neck in the proximal femoral canal [22]. Therefore, greater native version resulted in a smaller difference in version between the lesser trochanter and the femoral neck as mentioned above.
Sagittal stem alignment also significantly influenced version discrepancy. An anteriorly tilted stem was significantly and inversely correlated with the degree of the Sv–Nv (Table 3). When sagittal stem alignment was tilted anteriorly by 1°, the Sv–Nv decreased by 2.3° (Fig. 5b). This suggests that when the stem is inserted at the anterior femoral neck, the anterior wall of the neck possibly interferes with stem rotation. This could explain why stem version tended to be smaller than what would be expected based on native version. Although it is unclear whether the sagittal tilt of a cementless stem has an effect on dislocation rate or long-term results, surgeons should notice that it alters stem version against the native version of the femoral canal.
Stem version is influenced by several factors such as sagittal stem tilt and native version. These results might lead to the importance of intra-operative measurement of stem version prior to the cup placement. To achieve an appropriate CA for each case, the method to adjust cup anteversion according to stem anteversion, the so-called CA technique, has been recommended by Dorr et al. in cementless THA as a cementless stem has less adjustability in the femoral canal compared to the cemented stem [16, 25].
There are several limitations to this study. First, this study analyzed only one design, a metaphyseal fit stem. Although the design is similar to many other stems currently available and a cementless stem usually has little adjustability of version, our findings may not be applied to other stem designs. Future studies could address if other stems display similar characteristics. Secondly, we grouped OA, ONFH, and RA together into a category of primary diagnoses. However, the number of ONFH and RA hips was small compared to the number of OA hips, therefore potentially decreasing statistical power in terms of influence of the primary diagnosis. Thirdly, our study had a high proportion of DDH hips (86 hips, 70.5 %). The proportion of hips with primary OA was usually larger than that in our study [20, 25]. Based on the results of this study, as DDH has usually large femoral anteversion, it was expected that the Sv–Nv in primary OA hips would be larger. The value of the discrepancy between native and stem version might change if the patient characteristics changed. Finally, all operations were carried out using a posterolateral approach. Compared to an average of 0.3° sagittal stem tilt in this study, an anterior or lateral approach seemed to result in an increased stem tilt. One study reported 5.2° of sagittal stem tilt using a direct lateral or anterolateral surgical approach [23]. As sagittal stem tilt significantly influenced version discrepancy, an analysis utilizing additional surgical approaches may alter the tendencies found in this study.
In conclusion, the degree of stem version was consistently greater than native version by 9.8° on average utilizing a cementless metaphyseal fit stem. Increased native version and an anteriorly oriented sagittal stem tilt resulted in a decreased discrepancy. Stem version most closely approximated femoral canal version at the level of the CLT, therefore the found discrepancy reflected the difference in version between the lesser trochanter and the femoral neck. These findings are useful for surgeons in preoperative planning and to achieve the proper combined anteversion.
Acknowledgments
This work was supported by Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (No. 24592268). We thank Junji Kishimoto, a statistician from the Digital Medicine Initiative, Kyushu University, for his valuable comments and suggestions in regards to the statistical analysis.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 2.Barsoum WK, Patterson RW, Hiquera C, Klika AK, Krebs VE, Molloy R. A computer model of the position of the combined component in the prevention of impingement in total hip replacement. J Bone Joint Surg Br. 2007;89:839–845. doi: 10.1302/0301-620X.89B6.18644. [DOI] [PubMed] [Google Scholar]
- 3.Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. J Bone Joint Surg Am. 2007;89:1832–1842. doi: 10.2106/JBJS.F.01313. [DOI] [PubMed] [Google Scholar]
- 4.Ji WT, Tao K, Wang CT. A three-dimensional parameterized and visually kinematic simulation module for the theoretical range of motion of total hip arthroplasty. Clin Biomech. 2010;25:427–432. doi: 10.1016/j.clinbiomech.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 5.McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970;52:148–159. [PubMed] [Google Scholar]
- 6.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–821. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17:282–288. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 8.Maruyama M, Feinberg JR, Capello WN, D’Antonio JA. The Frank Stinchfield Award: Morphologic features of the acetabulum and femur: anteversion angle and implant positioning. Clin Orthop Relat Res. 2001;393:52–65. doi: 10.1097/00003086-200112000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Botser IB, Ozoude GC, Martin DE, Siddiqi AJ, Kuppuswami S, Domb BG. Femoral anteversion in the hip: comparison of measurement by computed tomography, magnetic response imaging, and physical examination. Arthroscopy. 2012;28:619–627. doi: 10.1016/j.arthro.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 10.Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006;21:696–701. doi: 10.1016/j.arth.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Sendtner E, Müller M, Winkler R, Wӧrner M, Grifka J, Renkawitz T. Femur first in hip arthroplasty—the concept of combined anteversion. Z Orthop Unfall. 2010;148:185–190. doi: 10.1055/s-0029-1240969. [DOI] [PubMed] [Google Scholar]
- 12.Eckrich SG, Noble PC, Tullos HS. Effect of rotation on the radiographic appearance of the femoral canal. J Arthroplasty. 1994;9:419–426. doi: 10.1016/0883-5403(94)90053-1. [DOI] [PubMed] [Google Scholar]
- 13.Suh KT, Kang JH, Roh HL, Moon KP, Kim HJ. True femoral anteversion during primary total hip arthroplasty: use of postoperative computed tomography-based sections. J Arthroplasty. 2006;21:599–605. doi: 10.1016/j.arth.2005.04.042. [DOI] [PubMed] [Google Scholar]
- 14.Emerson RH., Jr Increased anteversion of press-fit femoral stems compared with anatomic femur. Clin Orthop Relat Res. 2012;470:477–481. doi: 10.1007/s11999-011-1993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Itokawa K, Nakashima Y, Yamamoto T, Motomura G, Ohishi M, Hamai S, Akiyama M, Hirata M, Hara D, Iwamoto Y. Late dislocation is associated with recurrence after total hip arthroplasty. Int Orthop. 2013;37:1457–1463. doi: 10.1007/s00264-013-1921-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nakashima Y, Hirata M, Akiyama M, Itokawa T, Yamamoto T, Motomura G, Ohishi M, Hamai S, Iwamoto Y. Combined anteversion technique reduced the dislocation in cementless total hip arthroplasty. Int Orthop. 2014;38:27–32. doi: 10.1007/s00264-013-2091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fujii M, Nakashima Y, Yamamoto T, Yamamoto T, Mawatari T, Motomura G, Matsushita A, Matsuda S, Jingushi S, Iwamoto Y. Acetabular retroversion in developmental dysplasia of the hip. J Bone Joint Surg Am. 2010;92:895–903. doi: 10.2106/JBJS.I.00046. [DOI] [PubMed] [Google Scholar]
- 18.Fujii M, Nakashima Y, Sato T, Akiyama M, Iwamoto Y. Acetabular tilt correlates with acetabular version and coverage in hip dysplasia. Clin Orthop Relat Res. 2010;470:2827–2835. doi: 10.1007/s11999-012-2370-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sugano N, Noble PC, Kamaric E. A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr. 1998;22:610–614. doi: 10.1097/00004728-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Bargar WL, Jamali AA, Nejad AH. Femoral anteversion in THA and its lack of correlation with native acetabular anteversion. Clin Orthop Relat Res. 2010;468:527–532. doi: 10.1007/s11999-009-1040-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 22.Sugano N, Noble PC, Kamaric E, Salama JK, Ochi T, Tullos HS. The morphology of the femur in developmental dysplasia of the hip. J Bone Joint Surg Br. 1998;80:711–719. doi: 10.1302/0301-620X.80B4.8319. [DOI] [PubMed] [Google Scholar]
- 23.Müller M, Crucius D, Perka C, Tohtz S. The association between the sagittal femoral stem alignment and the resulting femoral head centre in total hip arthroplasty. Int Orthop. 2011;35:981–987. doi: 10.1007/s00264-010-1047-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akiyama M, Nakashima Y, Fujii M, Sato T, Yamamoto T, Mawatari T, Motomura G, Matsuda S, Iwamoto Y. Femoral anteversion is correlated with acetabular version and coverage in Asian women with anterior and global deficient subgroups of hip dysplasia: a CT study. Skelet Radiol. 2012;41:1411–1418. doi: 10.1007/s00256-012-1368-7. [DOI] [PubMed] [Google Scholar]
- 25.Dorr LD, Wan Z, Malik A, Zhu J, Dastane M, Deshmane P. A comparison of surgeon estimation and computed tomographic measurement of femoral component anteversion in cementless total hip arthroplasty. J Bone Joint Surg Am. 2009;91:2598–2604. doi: 10.2106/JBJS.H.01225. [DOI] [PubMed] [Google Scholar]