Abstract
Introduction:
Menopausal symptoms experienced by women are known to affect their quality-of-life. The symptoms experienced at menopause are quite variable and their etiology is found to be multifactorial. This study was hence done to assess the pattern and severity of menopausal symptoms and to find out the factors associated with these symptoms.
Materials and Methods:
This cross-sectional study was conducted in various outreach clinics of Kasturba Medical College, Mangalore. Women in the age group of 40-65 years were included in the study by convenient sampling method. Data regarding menopausal symptom was obtained by interviewing each participant using the menopause rating scale questionnaire.
Results:
Mean age of the participants were 54.2 ± 7.2 years and mean age of attainment of menopause was 48.4 ± 4.5 years. Mean duration of menopause was found to be 7.5 ± 5.3 years. Commonest symptom reported was joint and muscular discomfort and physical and mental exhaustion seen in 94 (85.4%) participants. The mean number of symptoms reported by participants was 7.6 ± 2.8. Educated women reported significantly more symptoms (F = 2.218, P = 0.047). Somatic and urogenital symptoms were more among perimenopausal women and somatic symptoms were more among postmenopausal women. Fifty-eight (52.7%) participants had one or more severe symptoms. Severe symptoms were most among premenopausal women.
Conclusion:
The high proportion and severity of menopausal symptoms observed in this study group proves that menopausal symptoms are common and cannot be ignored. More of menopausal clinics are needed for awareness generation, early recognition and treatment of related morbidities.
Keywords: Perimenopausal women, postmenopausal women, premenopausal women, psychological symptoms, somatic symptoms, urogenital symptoms
INTRODUCTION
Menopausal symptoms result from depletion of oestrogen level as women approaches menopausal stage and some of these women begin to experiences these menopausal symptoms early in the perimenopausal phase.[1] Owing to lack of estrogen more than 80% of women experience decrease physical and mental well-being in the year approaching menopause and hence postmenopausal woman can be considered a risk population.[2]
It is well-documented that menopausal symptoms experienced by women affect their quality-of-life.[3] Unfortunately, majority of these women are not aware of the changes brought about by menopause.[2,4]
With the increasing life expectancy women spends almost a third of her life in menopause.[5] Health issues of postmenopausal women therefore would pose a significant challenge to public health also considering the fact that there hasn’t been a specific health program for such women in the country. The current geriatric health care services is largely based on the general health problems of the elderly and not directed specifically to the postmenopausal health problems.[6]
To compound the problems, the menopause symptoms are quite variable with multifactorial etiology. Studies on menopausal issues and health demand priority in Indian scenario due to the growing population of menopausal women and due to varying presentation following influence of varied social and cultural pattern. Moreover by such studies, we can make women aware of menopausal symptoms leading to reduction in discomfort and fears. This also helps in its early recognition and seeking appropriate medical care if necessary.
With this background, this study was done to assess the pattern and severity of menopausal symptoms and to find out the factors associated among women in South Canara District of Karnataka State of south India.
MATERIALS AND METHODS
This cross-sectional study was conducted in three urban and one rural outreach clinic affiliated to Kasturba Medical College in Mangalore in the month of March 2011. The study protocol was approved by the Ethics Committee of this institution. Sample size of 110 was calculated by the assuming the proportion of women with menopausal symptoms to be 50% with relative precision of 20% and nonresponse rate of 10%. Women in the age group of 40-65 years were included in the study by convenient sampling method.
Exclusion criteria at baseline included any serious illness that might compromise ovarian or hormonal and current use of exogenous sex hormones. Patients with amenorrhea secondary to ovarian surgery, hysterectomy or chemo radiotherapy were also excluded.
Each patient was explained the nature and purpose of this study and their written informed consent was obtained. Data regarding menopausal symptom was also obtained by interviewing each participant using the standard menopause rating scale (MRS) questionnaire[7] after translating it into the local language Kannada. MRS is an 11 item questionnaire on commonly associated symptoms of menopause with a scoring scale from zero (no complaints) to four (very severe symptoms). Each participant was asked if they had experienced these symptoms in the previous 1-month period and to grade its severity.
Somatic domain comprised of symptoms such as hot flushes and sweating, heart discomfort, sleep problems and joint and muscular discomfort. Psychological domain comprised of symptoms such as depressive mood, irritability, anxiety and physical and mental exhaustion. Urogenital domain comprised of symptoms like sexual problems, bladder problems and dryness of vagina.[1]
The menopausal status was classified according to Stages of Reproductive Ageing Workshop classification, which divided menopause staging into, postmenopausal as no menstrual bleeding in the previous 12 months, perimenopausal as those who did not have menstruation in the previous 2 months or those who experienced increasing irregularity of menses and premenopausal as minor changes in cycle length.[8]
Analysis was performed using Statistical Package for Social Sciences software package SPSS software version 11.0 (SPSS Inc., Chicago, IL). Chi-square test, unpaired t-test, ANOVA and Pearson co-efficient of correlation were used for statistical analysis. P ≤ 0.05 was considered as significant association.
RESULTS
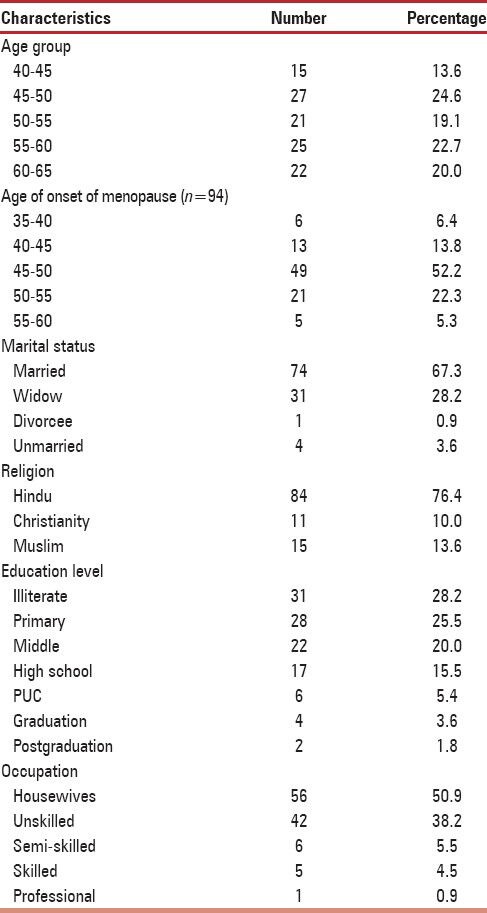
Mean age of the participants were 54.2 ± 7.2 years. The mean age of attainment of menopause was 48.4 ± 4.5 years and mean duration of menopause was 7.5 ± 5.3 years [Table 1]. Most of the participants were postmenopausal women 80 (72.7%) followed by perimenopausal 17 (15.5%) and premenopausal women 13 (11.8%). Mean age of premenopausal women was 44 ± 2.5 years, perimenopausal women was 48.5 ± 2.8 years and postmenopausal women was 57.1 ± 5.9 years.
Table 1.
Sociodemographic characteristic of participants (n=110)
The most common symptom reported was joint and muscular discomfort and physical and mental exhaustion seen in 94 (85.4%) participants [Table 2]. 84 (76.4%) women reported more than five symptoms. One woman who was in premenopausal group did not suffer from any symptoms of menopause. The mean number of symptoms reported by participants was 7.6 ± 2.8. There was no significant correlation between the number of menopausal symptoms with age (r = 0.05, P = 0.623), age of onset of menopause (r = 0.115, P = 0.268) and no association with occupation of participants (F = 0.904, P = 0.465). However a significant association was found between the number of menopausal symptoms and educational status of participants with the mean number of symptoms increasing with increasing educational status (F = 2.218, P = 0.047).
Table 2.
Distribution of menopausal symptoms among participants (n=110)
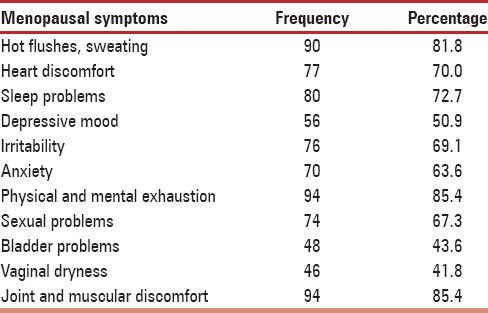
Common symptoms among premenopausal women were joint and muscle ache and physical and mental exhaustion 11 (84.6%). In perimenopausal women, it was hot flushes and physical and mental exhaustion 15 (88.2%). In postmenopausal women, it was joint and muscle ache 69 (86.2%). The mean number of reported symptoms was 7.1 ± 3.1 among premenopausal women, 7.6 ± 2.9 among perimenopausal women, and 7.7 ± 2.8 among postmenopausal women (F = 0.181, P = 0.834).
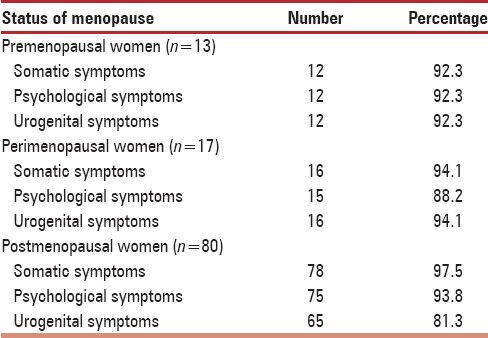
Somatic problems were present among 106 (96.4%), psychological problems among 102 (92.7%) and urogenital problems among 93 (84.5%) participants.
Mean age of participants without urogenital symptoms (n = 17) was 57.6 ± 6.5 years compared to 53.6 ± 7.1 years among participants with these symptoms (n = 93) (t = 2.133, P = 0.035).
Similarly, mean age of onset of menopause among participants without urogenital symptoms (n = 16) was 50.4 ± 3.6 years compared to 48 ± 4.6 years among participants with these symptoms (n = 78) (t = 2.006, P = 0.048). No other sociodemographic variables were found to be associated with the presence of somatic, psychological or urogenital symptoms among study participants.
No significant association of somatic symptoms (P = 0.563), psychological symptoms (P = 0.728) and urogenital symptoms (P = 0.293) was seen with menopausal status [Table 3]. The vasomotor symptoms like hot flushes and sweating were reported by 10 (76.9%) premenopausal, 15 (88.2%) perimenopausal and 65 (81.2%) postmenopausal women (P = 0.706).
Table 3.
Distribution of menopausal symptoms based on status of menopause
Most common severe or very severe problems experienced by participants were joint and muscle discomfort 37 (33.6%) [Table 4].
Table 4.
Distribution of menopausal symptoms based on severity of the condition
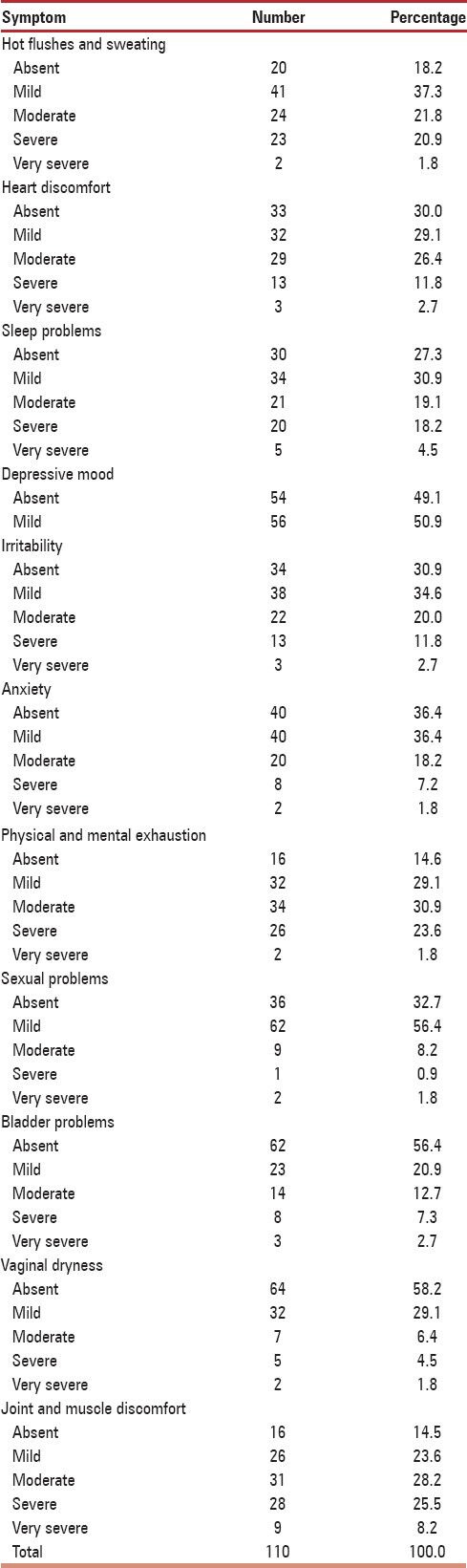
Fifty eight (52.7%) participants had one or more severe or very severe symptoms of menopause. There was no correlation between severity of menopausal symptoms with age of participant (r = 0.084, P = 0.381) or with duration of menopausal symptoms (r = 0.110, P = 0.290). There was no association of severity of menopausal symptoms with educational status (F = 0.279, P = 0.946), occupational status (F = 2.194, P = 0.075) and marital status (t = 1.038, P = 0.302). Severe or very severe symptoms were reported by 56 (52.8%) women with somatic symptoms, 23 (22.6%) women with psychological symptoms and 15 (16.1%) women with urogenital symptoms. Severe or very severe symptoms were most in the premenopausal women 8 (61.5%) followed by postmenopausal women 43 (53.8%) and perimenopausal women 7 (41.2%) (χ2 = 1.35, df = 2, P = 0.51). The mean number of severe symptoms among premenopausal women was 1.9, perimenopausal was 1.0 and postmenopausal was 1.7 (F = 1.012, P = 0.367).
DISCUSSION
Menopause though a universal phenomenon has a varied presentation due to influence of different biological, environmental and cultural factors like beliefs and attitudes.
The mean age of attainment of menopause which was 48.4 years in this study was similar to the findings of 48.3 years made in a study done in Kannur[9] and 48.7 years made in a study done in Manipal.[10] In other studies done in India and outside India, the mean age of onset of menopause ranged between 44.5 and 51.3 years.[1,3,6,11,12,13]
The most common symptoms of menopause seen in this study were physical and mental exhaustion and joint and muscle aches, which was similar to the findings of another regional study.[10] Several studies have reported joint and muscle pains as the commonest menopausal symptom.[11,12,14] There are also studies which have reported feeling of tiredness and easy fatigability as the commonest symptom of menopause.[4,13] On the other hand, a study done in Iran[15] reported night sweats, a study done in Malaysia[16] reported hot flushes, a study done in Bolivia[17] reported loss of libido and a study done in Manipal[18] reported poor memory as the commonest menopausal symptom. Overall musculoskeletal symptoms being reported as the commonest menopausal symptom has been proved to be related to hormonal changes.
The mean number of symptoms reported by participants in our study was 7.6 when compared to 12.5 reported in a study done in Malaysia. In the latter study, two participants were also found to have no menopausal symptoms at all.[3] A study done in Kannur found mean number of symptoms to be 4.9, which was lower than our findings.[9]
In this study, educated women had significantly more menopausal symptoms compared to less educated women which was similar to the findings of a study done in Taiwan.[19] This could be because of greater health consciousness among the educated than less educated women. However, other studies found women with higher education having a lower prevalence and intensity of menopausal symptoms.[20,21] A study done in Singapore also demonstrated no association between education and menopausal symptoms.[11]
The study done in Malaysia found a significant positive correlation between total score of menopausal symptoms and age which was not found in our study.[3] A study done in Nigeria reported a significant association of symptom based scores with socio demographic variable like age, menopausal status and occupation, which was again different from our observations.[22]
There was no association with the number of symptoms with menopausal status in this study, which was in contrast to findings of a study done in USA where perimenopausal and postmenopausal women reported significantly more menopausal complaints than premenopausal women.[23]
The commonest symptom among perimenopausal women in a study done in Brazil was joint and muscle aches and fatigue and among postmenopausal women was joint and muscle aches, which was similar to our observations.[24] However in a study done in Mumbai, mastalgia followed by mood changes were the commonest symptom reported among perimenopausal women, which was different from ours.[25] In another study done in Bangladesh, fatigue and tiredness followed by headache were the commonest symptoms among the three groups and was significantly more in perimenopausal women.[12]
The most common type of symptom in the present study was somatic (which includes vasomotor symptoms), which was different from the findings of another regional study where vasomotor symptoms were less frequently reported.[10] Furthermore, somatic problems reported among 96.4% participants in our study was higher than the proportion of 88.4% reported in a study done in Gujarat.[6]
The frequency of psychological problems observed in this study was lesser than the observations of 96% reported in a study done in Pakistan[14] but higher than the findings of a study done in China[26] where it was reported in 90% participants. With respect to psychological problems, it is possible that the normal aging process could be influencing its occurrence.[3] Increase in psychological symptoms may also be associated with current life events and difficulties particularly those experienced in family life.
The frequency of urogenital problems in this study was more than the proportion of 41.5% reported in a study done in Malaysia.[3] The reasons for different frequencies in type of symptoms could be due to effects of environmental and socio-cultural factors such as diet, exercise and other lifestyle modifications.[3] Furthermore, the different methodologies used by different studies could also be an influencing factor.
In this study, mean age and mean age of onset of menopause was found to be significantly less among participants with urogenital symptoms. In the study done in Nigeria, age of the respondent and menopausal status was found to be significantly associated with scores of somatic and urogenital subscales. The above mentioned study also found a significant association between occupational status of participants with psychological subscale which was not observed in our study.[22]
In our observations, no association was noticed between type of symptoms and menopausal status. Here somatic followed psychological symptoms were seen more among postmenopausal women while somatic and urogenital symptoms were more among perimenopausal women. In other studies, perimenopausal women experienced higher prevalence of somatic and psychological symptoms compared to pre and postmenopausal women. Also these studies found urogenital symptoms to occur more among postmenopausal women.[1,27] A study done in Singapore found urogenital symptoms to be more among perimenopausal women and no association between somatic symptoms and menopausal status similar to our findings.[11] A study done in Thailand found somatic symptoms to be significantly more in postmenopausal group.[28]
In this study, perimenopausal women were noted to experience more of vasomotor symptoms when compared to other menopausal group of women, but this was not statistically significant. However, several other studies have found a significant association and reported as high as 75% of perimenopausal women experiencing bothersome vasomotor symptoms at some point of their transitional period.[1,11,23] This can be explained by the fact that in these group of women, estrogen fluctuation during this phase occurs the most, hence they will experienced the most vasomotor symptoms.[1] However a study done in Sydney[4] and another done in Manipal[18] found postmenopausal women suffered significantly more vasomotor symptoms than pre and perimenopausal women. The decreased estrogen theory thus fails to explain why some regularly menstruating women experience hot flashes or why hot flashes are not experienced by all perimenopausal or postmenopausal women.[29]
In the study done in Malaysia, severe or very severe symptoms in joint and muscle discomfort was reported by 22.9%, depressive mood by 18.6%, sleep problems by 17.1%, irritability or anxiety by 14.3%, hot flushes and physical and mental exhaustion by 12.9%, bladder problems and vaginal dryness by 5.7% and sexual problems by 1.4% subjects, which were lower than our observations, but for the proportion of cases with anxiety.[3]
In this study, there was no association of severity of menopausal symptoms with any of the socio demographic variables, menopausal status or duration of menopause, which was similar to the findings of a study done in Malaysia.[3] Other studies have observed that women with a longer duration of menopause reported a lower severity of symptoms probably because they had more time to adapt to the menopausal changes.[20,21,30] May be this was the reason behind greater number of severe symptoms among premenopausal women in this study compared with other menopausal groups, however this difference was not statistically significant.
A study done in Iran found severity of menopausal symptoms to be significantly less among employed women and women with higher educational level.[30] Similarly, another study done in Sydney found that better educated women reported fewer and less severe symptoms.[4] A study done in Brazil reported severity of symptoms to be more in postmenopausal women.[24] All these observations were different from our findings.
CONCLUSION
The commonest menopausal symptoms were joint and muscular discomfort and physical and mental exhaustion. Most women suffered from somatic symptoms followed by psychological and urogenital symptoms. Somatic symptoms were more among postmenopausal women, while somatic and urogenital symptoms were more among perimenopausal women. The total number of symptoms was most among postmenopausal. More than half of participants had at least one severe complaint. Severe symptoms were most among premenopausal women. Educated women were found to report significantly more symptom than less educated. The high proportion and severity of the menopausal symptoms observed in this study group proves that menopausal symptoms are common and cannot be ignored. It is therefore suggested that menopausal clinics needs to be established within the current primary health care system so as to focus attention to menopausal women and their needs. Such clinics need to also create awareness among women who are approaching their menopause regarding early identification of common menopausal symptoms and its prompt management so that the severity of such symptoms could be minimized.
Limitations
This being a clinic and not a population based study might not reveal the real magnitude of menopausal symptoms as mild complaints are often not reported to health facilities. Furthermore, a cross-sectional study of this nature cannot exclude the role of other confounding effects of the natural aging process that may influence the experience of these symptoms. In collecting data, women were asked to provide some retrospective information, such as menopausal symptoms experienced in the preceding weeks, regularity of menstruation and last menstrual period, hence recall bias is unavoidable especially in some elderly women. A final limitation of this study being unavailability of information of daily physical activity and anthropometric measurements of study participants due to time constraints in a busy outpatient clinic setting.
ACKNOWLEDGMENTS
Our authors would like to thank MBBS students Mr. Sanal, Mr. Akshaj, Ms. Ashika, Mr. Adhish and Ms. Mareeka of KMC Mangalore for their help in data collection.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Rahman SA, Zainudin SR, Mun VL. Assessment of menopausal symptoms using modified Menopause Rating Scale (MRS) among middle age women in Kuching, Sarawak, Malaysia. Asia Pac Fam Med. 2010;9:5. doi: 10.1186/1447-056X-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fuh JL, Wang SJ, Lee SJ, Lu SR, Juang KD. Quality of life and menopausal transition for middle-aged women on Kinmen island. Qual Life Res. 2003;12:53–61. doi: 10.1023/a:1022074602928. [DOI] [PubMed] [Google Scholar]
- 3.Jahanfar SH, Abdul Rahim BA, Shah Reza BK. Age at menopause and menopausal symptoms among Malaysian women who were referred to a health clinic in Malaysia. Shiraz E-Med J. 2006;7:3. [Google Scholar]
- 4.Lu J, Liu J, Eden J. The experience of menopausal symptoms by Arabic women in Sydney. Climacteric. 2007;10:72–9. doi: 10.1080/13697130601159649. [DOI] [PubMed] [Google Scholar]
- 5.Vaze N, Joshi S. Yoga and menopausal transition. J Midlife Health. 2010;1:56–8. doi: 10.4103/0976-7800.76212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christian DS, Kathad M, Bhavsar B. A clinico-epidemiological study on health problems of post-menopausal women in rural area of Vadodara District, Gujarat. Natl J Med Res. 2012;2:478–80. [Google Scholar]
- 7.Menopause Rating Scale. [Last cited on 2011 Jan 23]. Available from: http://www.hqlo.com/content/supplementary/1477-7525-1-28-s3.pdf .
- 8.Soules MR, Sherman S, Parrott E, Rebar R, Santoro N, Utian W, Woods N. Stages of Reproductive Aging Workshop (STRAW) J Womens Health Gend Based Med. 2001;10:843–8. doi: 10.1089/152460901753285732. [DOI] [PubMed] [Google Scholar]
- 9.Borker SA, Venugopalan PP, Bhat SN. Study of menopausal symptoms, and perceptions about menopause among women at a rural community in Kerala. J Midlife Health. 2013;4:182–7. doi: 10.4103/0976-7800.118997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bairy L, Adiga S, Bhat P, Bhat R. Prevalence of menopausal symptoms and quality of life after menopause in women from South India. Aust N Z J Obstet Gynaecol. 2009;49:106–9. doi: 10.1111/j.1479-828X.2009.00955.x. [DOI] [PubMed] [Google Scholar]
- 11.Chim H, Tan BH, Ang CC, Chew EM, Chong YS, Saw SM. The prevalence of menopausal symptoms in a community in Singapore. Maturitas. 2002;41:275–82. doi: 10.1016/s0378-5122(01)00299-7. [DOI] [PubMed] [Google Scholar]
- 12.Rahman S, Salehin F, Iqbal A. Menopausal symptoms assessment among middle age women in Kushtia, Bangladesh. BMC Res Notes. 2011;4:188. doi: 10.1186/1756-0500-4-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mahajan N, Aggarwal M, Bagga A. Health issues of menopausal women in North India. J Midlife Health. 2012;3:84–7. doi: 10.4103/0976-7800.104467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nisar N, Sohoo NA. Frequency of menopausal symptoms and their impact on the quality of life of women: A hospital based survey. J Pak Med Assoc. 2009;59:752–6. [PubMed] [Google Scholar]
- 15.Ashrafi M, Ashtiani SK, Malekzadeh F, Amirchaghmaghi E, Kashfi F, Eshrati B. Factors associated with age at natural menopause in Iranian women living in Tehran. Int J Gynaecol Obstet. 2008;102:175–6. doi: 10.1016/j.ijgo.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 16.Kronenberg F. Hot flashes: Epidemiology and physiology. Ann N Y Acad Sci. 1990;592:52–86. doi: 10.1111/j.1749-6632.1990.tb30316.x. [DOI] [PubMed] [Google Scholar]
- 17.Castelo-Branco C, Palacios S, Mostajo D, Tobar C, von Helde S. Menopausal transition in Movima women, a Bolivian Native-American. Maturitas. 2005;51:380–5. doi: 10.1016/j.maturitas.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 18.Nayak G, Kamath A, Kumar P, Rao A. A study of quality of life among perimenopausal women in selected coastal areas of Karnataka, India. J Midlife Health. 2012;3:71–5. doi: 10.4103/0976-7800.104456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheng MH, Wang SJ, Wang PH, Fuh JL. Attitudes toward menopause among middle-aged women: A community survey in an island of Taiwan. Maturitas. 2005;52:348–55. doi: 10.1016/j.maturitas.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 20.Gharaibeh M, Al-Obeisat S, Hattab J. Severity of menopausal symptoms of Jordanian women. Climacteric. 2010;13:385–94. doi: 10.3109/13697130903050009. [DOI] [PubMed] [Google Scholar]
- 21.Lee Y, Kim H. Relationships between menopausal symptoms, depression, and exercise in middle-aged women: A cross-sectional survey. Int J Nurs Stud. 2008;45:1816–22. doi: 10.1016/j.ijnurstu.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 22.Olaolorun FM, Lawoyin TO. Experience of menopausal symptoms by women in an urban community in Ibadan, Nigeria. Menopause. 2009;16:822–30. doi: 10.1097/gme.0b013e318198d6e7. [DOI] [PubMed] [Google Scholar]
- 23.Xu J, Bartoces M, Neale AV, Dailey RK, Northrup J, Schwartz KL. Natural history of menopause symptoms in primary care patients: A MetroNet study. J Am Board Fam Pract. 2005;18:374–82. doi: 10.3122/jabfm.18.5.374. [DOI] [PubMed] [Google Scholar]
- 24.Guimarães AC, Baptista F. Relationship between physical activity and menopausal symptoms. J Phys Act Health. 2011;16:144–9. [Google Scholar]
- 25.Joshi JV, Pandey SN, Galvankar P, Gogate JA. Prevalence of premenstrual symptoms: Preliminary analysis and brief review of management strategies. J Midlife Health. 2010;1:30–4. doi: 10.4103/0976-7800.66995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen Y, Lin SQ, Wei Y, Gao HL, Wu ZL. Menopause-specific quality of life satisfaction in community-dwelling menopausal women in China. Gynecol Endocrinol. 2007;23:166–72. doi: 10.1080/09513590701228034. [DOI] [PubMed] [Google Scholar]
- 27.Peeyananjarassri K, Cheewadhanaraks S, Hubbard M, Zoa Manga R, Manocha R, Eden J. Menopausal symptoms in a hospital-based sample of women in southern Thailand. Climacteric. 2006;9:23–9. doi: 10.1080/13697130500487422. [DOI] [PubMed] [Google Scholar]
- 28.Punyahotra S, Dennerstein L, Lehert P. Menopausal experiences of Thai women. Part 1: Symptoms and their correlates. Maturitas. 1997;26:1–7. doi: 10.1016/s0378-5122(96)01058-4. [DOI] [PubMed] [Google Scholar]
- 29.Hahn PM, Wong J, Reid RL. Menopausal-like hot flashes reported in women of reproductive age. Fertil Steril. 1998;70:913–8. doi: 10.1016/s0015-0282(98)00281-7. [DOI] [PubMed] [Google Scholar]
- 30.Abedzadeh-Kalahroudi M, Taebi M, Sadat Z, Saberi F, Karimian Z. Prevalence and severity of menopausal symptoms and related factors among women 40-60 years in Kashan, Iran. Nurs Midwifery Stud. 2012;1:88–93. [Google Scholar]


