Abstract
Background:
Inhaled foreign bodies are common paediatric emergencies and a major cause of accidental deaths at home among Nigerian children especially among children below the age of 5 years. Different types of foreign bodies have been reported from the ordinary to the most bizarre. We evaluated the types of foreign bodies and sites of possible impaction of these foreign bodies along the tracheobronchial tree.
Materials and Methods:
A 6-year case record of 35 patients with foreign body inhalation was reviewed from January 2005 to December 2010 at the Otorhinolaryngology Department of Bayero University/Aminu Kano Teaching Hospital, Kano — North-western Nigeria. Basic information such as date of birth, age groups, gender, indication for bronchoscopy, type of foreign bodies, sites of foreign body impaction and surgical outcome were extracted and analysed.
Results:
Thirty-five patients [18 (51.4%) males and 17 (48.6%) females, aged 6 months-10 years] with a mean age of 5.1 years and median of 5 years (+/- 3.0 Standard Deviation). The most affected age group with 31.4% is 3-5 years. Groundnuts and whistles were the most frequently inhaled foreign bodies with an equal frequency of 25.7%, respectively. Foreign bodies were preferentially lodged in the left main bronchus in 8 (22.9%) patients compared to the right main bronchus in 6 (17.1%) patients.
Conclusion:
Public enlightenment both in the news/print media on the risk of foreign body aspiration especially among the under-five's is highly advocated. The left main bronchus may be a common site for impaction as well.
Keywords: Bronchus, foreign bodies, impaction site, inhalation, public enlightenment, types, whistles
INTRODUCTION
Inhaled foreign bodies (FBs) are a common paediatric emergency and perhaps among the greatest cause of accidental death at home among Nigerian children, although the exact incidence is not known because many are not recognised especially in rural communities.1 It is equally a major source of morbidity and mortality in even the most sophisticated of centres. This is particularly so in the paediatric age group especially the under-fives.2 This is said to be due to their inquisitiveness, adventurous nature, lack of molars for proper mastication, playing and running with food in the mouth with consequent incoordination in swallowing and glottic closure.3 With the advent of the ventilating bronchoscope, skilled personnel and better anaesthetic techniques, the mortality rate is said to have reduced from 24 to 3% or even less in developed countries.4
This, however, is not the case in developing countries especially sub-Saharan Africa, where the mortality rate is variable but reported cases range from 2.7 to 8.3%5,6,7 with majority probably under reported as most die before getting to a definitive point of care. The classical symptoms during FB inhalation are a sudden onset of paroxysms of cough, stridor and dyspnoea and occasionally this history is unavailable. The commoner signs are respiratory difficulty, reduced air entry in an affected lung, wheezing and/or crepitations. Therefore, a high index of suspicion is usually required to make a diagnosis.
Different types of foreign bodies (FBs) have been reported from the ordinary to the most bizarre. These range from inorganic materials such as needles, nails, whistles, toy parts and beads/rosary to organic substances such as groundnuts, maize seeds, water melon seeds, beans, variety of grains, etc. Nonetheless, one thing is sure they are all a major source of anxiety and fear to the patient, caregiver and perhaps the attending physician as well. This broad classification becomes important when considering obstruction to airflow, amount of mucosal reaction, inflammation/infection and abscess formation akin to organic foreign bodies in the tracheobronchial tree. On the other hand, inorganic FBs may cause total or partial obstruction which may be tolerated for some time with mild signs and symptoms leading to formation of granulation tissue after a period of time.8
The clinical course and outcome of inhaled foreign bodies largely depends on the nature/type of foreign body, the site of arrest or impaction along the tracheobronchial tree and perhaps availability of skilled manpower especially in developing countries. Foreign bodies can get impacted at any point from the laryngeal inlet to the terminal bronchioles, but more often these FBs get lodged in the right main bronchus. This is due to the right main stem bronchus being more in line with the trachea, thereby, creating a relatively straight path from the larynx to bronchus.
Despite this anatomical arrangement some controversies exist to suggest that more FBs are lodged in the left main bronchus compared to the right bronchus. In the same vain, some studies also posit that the site of election for impaction has an almost equal incidence in children, while others claim that this arrangement becomes relevant only after 15 years of age.1,9,10 However, the site of impaction of FBs may ultimately depend on the position of the patient at the time of inhalation. The right main bronchus is commoner in the erect position and right lateral position while FBs which are small enough preferentially lodge in the left main bronchus in the left lateral position. This may also account for the difference in distribution of site of lodgment between adults/adolescent and children.1
MATERIALS AND METHODS
This is a 6-year retrospective review of case notes of patients who have had bronchoscopies performed for foreign body inhalation at the Otorhinolaryngology Department of Aminu Kano Teaching Hospital, Kano from January 2005 to December 2010. All the cases were referrals from the accidents and emergency unit, Emergency paediatric unit and direct referrals from peripheral hospitals as well. The hospital is the main tertiary centre serving a population of over 10 million Nigerians with three other states as catchment areas (Katsina, Jigawa and Bauchi states).
A total of 39 patient case notes were retrieved for the study and only 35 were included for analysis, one case note had incomplete information/missing pages, two case notes revealed a failed/negative bronchoscopy, with one recorded mortality due to cardiac arrest intra-operatively. Basic information such as date of birth, age groups, gender, indication for bronchoscopy, type of FB, sites of FB impaction, and surgical outcome were recorded and analysed. In our centre, only the rigid bronchoscopy is carried out for foreign body inhalation extraction.
Data analysis
IBM SPSS (for windows, version 21) software was used to analyse this data and for ease of interpretation presented in the form of tables and charts. Statistically significant association between variables was explored using a two-tailed chi-square test and a confidence interval of 95.0%.
RESULTS
Thirty-five patient case notes were reviewed. The patient's ages ranged from 6 months to 10 years. The mean age was 5.1 years (+/- 3.0 Standard Deviation) and median age of 5 years. There were 18 (51.4%) males and 17 (48.6%) females with a male: Female ratio of 1.1:1. The most affected age group is 3-5 years (31.4%), followed by 0-2 years (25.7%) old age group [Table 1 and Figure 1].
Table 1.
Age group by sex distribution of foreign bodies among our patient groups
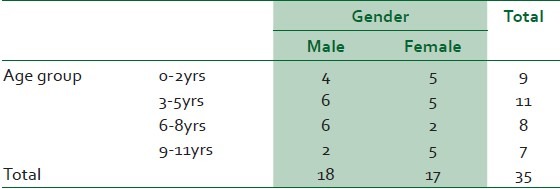
Figure 1.
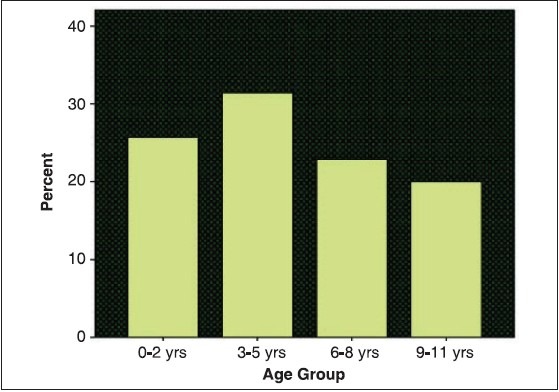
Chart depicting percentage of foreign body inhalation by age groups with highest among the under-five's
Groundnuts and whistles were the most frequently inhaled FBs in our series with 9 (25.7%) each [Figure 2 and Table 2]. Subdivision of types of FBs into two broad groups revealed organic 18 (51.4%) foreign bodies and 17(48.6%) inorganic foreign bodies [Figures 3 and 4, respectively].
Figure 2.
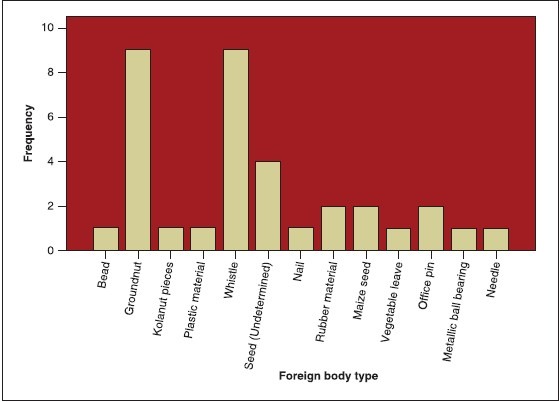
Chart to show the frequency of foreign body types as seen in our patient population
Table 2.
Variety of foreign bodies removed at bronchoscopy during the period under review
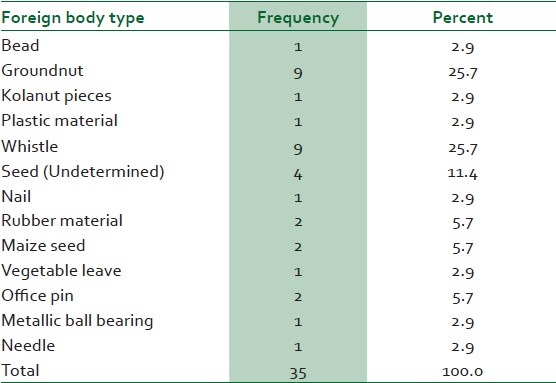
Figure 3.
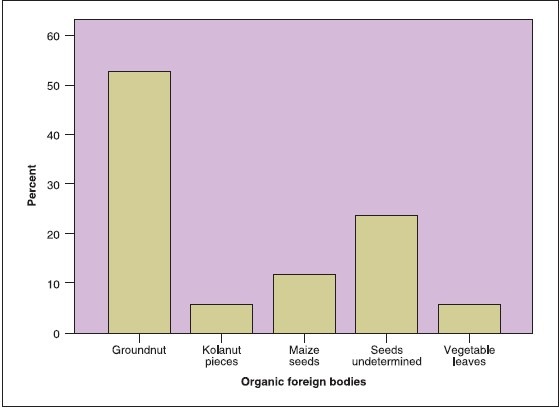
Distribution of organic foreign bodies by (groundnut with highest) percentage
Figure 4.
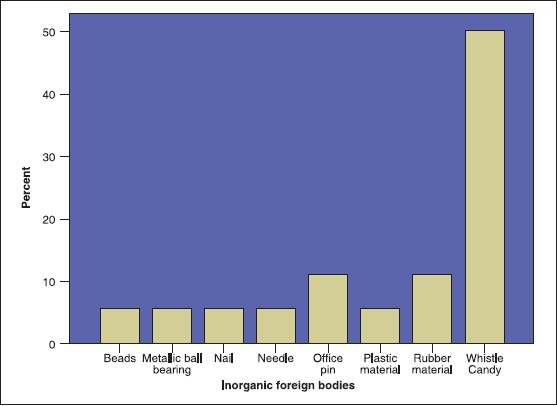
Distribution of inorganic foreign bodies by (whistles with highest) percentage
With regard to the bronchus, overall FBs were more preferentially lodged in the left main bronchus in 8 (22.9%) patient against the right main bronchus in 6 (17.1%) patients. The 9-11-year and 3-5-year-old age groups were especially noted to have FB impaction involving the left main bronchus 3 (42.9) and right main bronchus 2 (18.2%) (P = 0.592), respectively. However, the majority of extracted FBs from the airways had no label for the specific site of impaction 15 (42.9%). [Figures 5 and 6]
Figure 5.
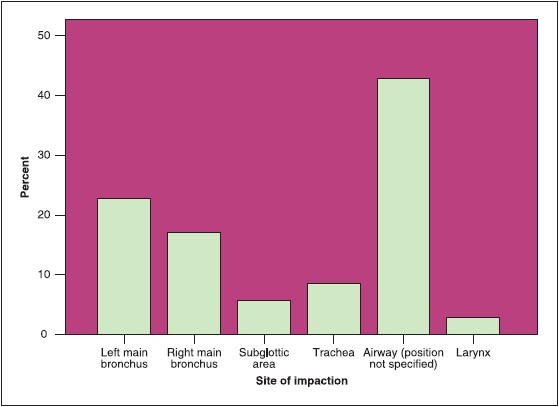
Distribution of impaction sites by percentages for foreign bodies in the tracheobronchial tree in our patient population
Figure 6.
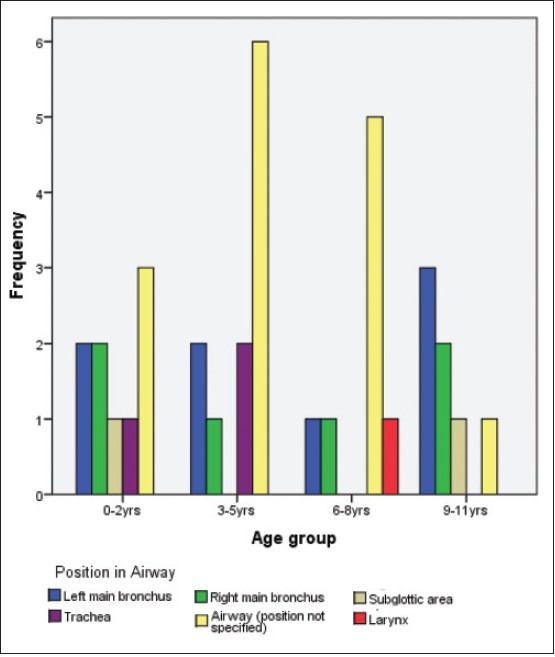
Frequency of impaction site by age group cluster bar chart
Analysis to determine relationship between age groups of these patients and types of inhaled foreign bodies revealed a strong association between these variables [Exact test P = 0.001; Phi and Cramer's V = 1.255 and 0.725, respectively, and contingency coefficient 0.782]
Further attempts to find relationships within variables such as sex of patients and nature of inhaled FBs, age groups and site of impaction, organic and inorganic FBs did not reveal any significant associations (P > 0.05) including the effect of age and gender in this study.
DISCUSSION
Our study clearly revealed that children below 5 years of age were most susceptible with a slight male preponderance. This was also the finding by Gulshan et al., and is probably due to the over active nature of male children compared to their female counterparts.11 A higher male preponderance ratio of atleast 2:1 or more, has been reported by several authors this may be due to variations in sample size when compared to ours.6,11,12,13 In contrast, from available literature we did not find a higher female preponderance.
Moreover, with regard to variety of FB's, groundnuts and whistles were the most common FB's accidently inhaled with equal frequencies in our series [Table 2]. To our knowledge, no recent study has reported an equal frequency of these FBs, much less reporting whistles as high as 25.7%. A study in Pakistan showed that whistles were the commonest inhaled foreign body with a frequency of 57.7%.14 However, two recent studies show a frequency of 5.26% and 17.3%, respectively,10,11 which is still less than findings from our series.
Children under 5 years are said to be generally more susceptible to FB inhalation due to their oral tendency, playing or running around with food pieces in the oral cavity and also parental nonchalance with regard to close supervision. Many studies allude to this same finding.1,15,16 Children between the ages of 3 and 5years were the highest in our series [Figure 1], this was also the finding of Onotai et al; however, other studies report a higher incidence in children less than or equal to 3 years.2,12,17,18 These periods coincide with the periods of inquisitiveness, adventure and exploration in a child's developmental milestone, and by implication require closer attention and supervision from parents/caregivers.
By and large organic FBs are commoner than inorganic FBs; our study revealed 51.4% and 48.6% respectively and this was the finding by other authors.19,20 The commonest organic FB inhaled in children is the groundnut and this concurs with our finding (25.7%) and is corroborated by other studies as well.10,11,16,21,22 In contrast, a recent study in Kenya revealed that the commonest organic FB in their series was beans while the second were peanuts/groundnuts.6
This was closely followed by seeds, although the particular type of seed was not documented in some instances due to its fragmented nature, but in addition to maize seeds, these still made up a large portion of inhaled organic FBs [Figure 3].16,18 Kolanut and vegetable matter were the least (<10%) but what we found, however, was the feeding, in some cases, of kolanut to children either by older siblings or accidently inhaled by the child while the parents were looking away or were not around. Kolanut is a commonly chewed nut by adults in Nigeria especially in the North, and requires molars to adequately grind them enough to be swallowed, but how they end up in the mouths of children since they lack molars says a lot about their care, or perhaps due to careless storage by the parents. Other studies have revealed fishbone as the commonest type of FB seen especially in South-south Nigeria.12
Generally, inorganic FBs portend grave danger with acute asphyxiation from total obstruction or respiratory difficulty from partial obstruction. With regard to whistles, in our part of the country during festivities or ceremonies sweet candies are frequently giving to children. However, a variety of ‘sweet candy’ is now available which is made combined with a whistle embedded within the sweet candy and after sucking out the candy bit, the children then go ahead to indulge in the reward by blowing the whistle as part of the fun. And as such, older children with whistles as FBs (25.7%) accounted for a greater portion of this group and this coincided with the Islamic festive periods of Eid-el-fitr or -Kabir and in the wet season [Figure 4]. Adegboye et al., reported the same observation during the wet season in Ibadan south-eastern Nigeria,1 a similar Turkish study also reported similar findings highlighting an association between FBs with seasonal, geographic locality and sociocultural environment of affected patients.23 The seasonal significance of this finding at this time is unclear and may require further observations. The finding of whistles as part of other toys or snacks is, however, not uncommon, as this was also reported in Abbottabad, where they mostly accounted for (17.3%) second highest after groundnuts.10 In one study in Saudi Arabia, the whistle could not be removed transglottically and tracheostomy with tracheal slit had to be performed, in our series all the whistle were successfully extracted transglottically via a rigid bronchoscope. This further emphasises the danger posed by these ‘toys of sweetness’.
Other varieties of FBs are more straightforward in terms of extraction with the appropriate forceps at hand. Ball bearings in particular, had to be removed with a ventilating bronchoscope via the tracheostome. This obviously requires cooperation between the anaesthetist and endoscopist in addition to relevant skill and experience. By and large, most studies show organic FBs to be most prevalent in comparison to inorganic FBs1,16 and this was our finding as well [Figures 3 and 4].
With regard to site of impaction or lodgment of foreign bodies, most studies have reported the preferential lodgment of FBs in children and adults to the right main bronchus as compared to the left main bronchus.15,16,24,25 However, in this review we did not record FB in both bronchi at the same seating as reported by a previous study.16
Location of impacted FB is somewhat contentious; most authors have argued that there is a preferential lodgment of FB in the right main bronchus than to the left main bronchus. This is said to be dependent on the patient's age and relative physical position at the onset of inhalation. Up until 15 years of age the angle made by the bronchi with the trachea is about the same, by implication an equal frequency is thereby recorded. However, after this age with continued growth and development, the left main bronchus assumes a more acute angle than the right and as such, the right bronchus is therefore more in line with the trachea. This may account for the relative higher frequency of FBs in the right main bronchus than in left as alluded to by many authors.4,10,21 Conversely, a recent study using tracheobronchial widths and angles from a large database of paediatric radiographs tested this hypothesis using standardised techniques with good reproducibility, and they concluded that an inhaled foreign body is more likely to enter the right bronchial tree than the left in children of ‘all’ ages. However, in another recent study the authors claim that variability in the position of the carina with respect to the mid-trachea may explain why this right-sided preference is less marked in children compared to adults. This is because, in most children, the carina was positioned to the left of the mid-trachea, but in 34% of cases (40% of infants), it was to the right of the mid-trachea.24 In another related study the authors posit that aspirated foreign bodies are equally distributed between the left and right main bronchus ‘only’ in children younger than 3 years. And that in children aged 3 and older foreign bodies were more commonly found in the right main bronchus.18,26
In our review of these paediatric cases, we found a preferential lodgement of FBs in the left bronchus than the right with 22.9% and 17.1%, respectively [Figures 5 and 6]. This was also the finding of Yeh et al., as well.27 Although, as previously highlighted, the lack of specific labelling for site of impaction might have affected this result inadvertently. However, it is not uncommon.27 It suffices to say then that the bronchi, irrespective of laterality are the commonest areas of impaction along the tracheobronchial tree. Our study showed a combined frequency of 40% (right and left) of bronchi involvement [Figure 5] and this was the finding of some authors as well.17,23,28 With regard to the rest of the tracheobronchial tree, the larynx and trachea have the lowest prevalence except in children less than 1 year,17 [Figure 5] this was our finding as well. Finally, our finding of left bronchial lodgment of FBs in specific age groups of 9-11 and 3-5 years was not statistical significant and as such no reliable comment can be made at this time.
Limitations
It suffices to say that proper and/or specific identification of extracted seeds and accurate delineation of impaction sites may have affected significantly the overall outcome measures in this study. Possible biases may have existed in the recorded information, and some patient information was missing or not reported by the attending surgeon. We also recognise that perhaps the sample size may be too small to make population-based conclusions.
CONCLUSIONS
Children particularly infants will always be curious leading to accidents and as such parents/caregivers have a fundamental role to play by providing constant supervision. The government must organise regular campaigns and proper education of the public both in the news/print media on the risk of foreign body aspiration especially among the under-five's. Parents must be advised to desist from giving infants and toddlers groundnuts/peanuts. Furthermore, the left main bronchus is a common area for impaction of FBs as well, although this may ultimately depend on the position of the patient at the time of inhalation. We suggest that a strong legislation be put in place to regulate sweet and/or toy-producing companies on whistles (toys) manufactured with candies/sweets, and if possible be totally withdrawn from the market.
ACKNOWLEDGEMENT
We want to thank our records department for their support in the compilation and retrieval of the case records for this study. Similarly, we would like to thank the other consultants who graciously gave valuable advice and agreed for their patient's records to be used for the study and of course the entire ENT department.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Adegboye VO, Adebo OA. Epidemiology of tracheobronchial foreign bodies in Ibadan. Niger J Clin Pract. 2001;4:51–3. [Google Scholar]
- 2.Orji FT, Akpeh JO. Tracheobronchial foreign body aspiration in children: How reliable are clinical and radiological signs in the diagnosis? Clin Otolaryngol. 2010;35:479–85. doi: 10.1111/j.1749-4486.2010.02214.x. [DOI] [PubMed] [Google Scholar]
- 3.Onotai LO, Ebong ME. The pattern of foreign body impactions in the tracheobronchial tree in University of Port Harcourt Teaching Hospital. Port Harcourt Med J. 2011;5:130–5. [Google Scholar]
- 4.Evans JNG. Foreign bodies in larynx and trachea. In: Kerr, editor. Scott-Brown's Otolaryngology. London: Butterworth - Heinemann; 1997. [Google Scholar]
- 5.Gilyoma J, Chalya P. Endoscopic procedures for removal of foreign bodies of the aerodigestive tract: The Bugando Medical Centre experience. BMC Ear Nose Throat Disord. 2011;11:1–5. doi: 10.1186/1472-6815-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oburra HO, Ngumi ZW, Mugwe P, Masinde PW, Maina AW, Irungu C. Bronchoscopy for removal of aspirated tracheobronchial foreign bodies at Kenyatta National Hospital, in Kenya. East Cent Afr J Surg. 2013;18:48–57. [Google Scholar]
- 7.Falase B, Sanusi M, Majekodunmi A, Ajose I, Oke D. Preliminary experience in the management of tracheobronchial foreign bodies in Lagos, Nigeria. Pan Afr Med J. 2013;15:31. doi: 10.11604/pamj.2013.15.31.2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muhammad A, Tahir H, Waqar-ur-Rehman Q, Muhammad J, Sohail M, Rehman G. Correlation of operative findings with pre-operative clinical signs and analysis of x-rays in patients with airway foreign bodies. J Ayub Med Coll Abbottabad. 2010;22:32–4. [PubMed] [Google Scholar]
- 9.Karatzanis AD, Vardouniotis A, Moschandreas J, Prokopakis EP, Michailidou E, Papadakis C, et al. The risk of foreign body aspiration in children can be reduced with proper education of the general population. Int J Pediatr Otorhinolaryngol. 2007;71:311–5. doi: 10.1016/j.ijporl.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 10.Muhammad A, Shahid AS, Farida K, Rehman G. Analysis of tracheobronchial foreign bodies with respect to sex, age, type and presentation. J Ayub Med Coll Abbottabad. 2007;19:13–5. [PubMed] [Google Scholar]
- 11.Gulshan H, Mahid I, Sharafat AK, Muhamad I, Javed Z. An experience of 42 cases of bronchoscopy at Saidu group of teaching hospitals, Swat. J Ayub Med Coll Abbottabad. 2006;18:59–62. [PubMed] [Google Scholar]
- 12.Onotai LO, Ibekwe MU, George IO. Impacted foreign bodies in the larynx of Nigerian children. J Med Med Sci. 2012;3:217–21. [Google Scholar]
- 13.Narasimhan KL, Chowdhary SK, Suri S, Mahajan JK, Samujh R, Rao KL. Foreign body airway obstruction in children. J Indian Assoc Pediatr Surg. 2002;7:184–9. [Google Scholar]
- 14.Farooqi T, Hussain M, Pasha HK, Bokhari K, Hassan S. Foreign body aspiration in children: An experience at Nishtar Hospital Multan. Pakistan J Paed Surg. 1999;1-2:16–24. [Google Scholar]
- 15.Amer JH, Kareemullah C, Amer MH, Shembish A. Tracheobronchial foreign bodies in children. Saudi Med J. 2000;21:672–4. [PubMed] [Google Scholar]
- 16.Salisu AD, Abubakar MY. Clinical presentation and management of tracheobronchial foreign bodies in Kano. Niger J Basic Clin Sci. 2010;7:1–7. [Google Scholar]
- 17.Rodríguez H, Passali GC, Gregori D, Chinski A, Tiscornia C, Botto H, et al. Management of foreign bodies in the airway and oesophagus. Int J Pediatr Otorhinolaryngol. 2012;76(Suppl 1):S84–91. doi: 10.1016/j.ijporl.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 18.Pan H, Lu Y, Shi L, Pan X, Li L, Wu Z. Similarities and differences in aspirated tracheobronchial foreign bodies in patients under the age of 3 years. Int J Pediatr Otorhinolaryngol. 2012;76:911–4. doi: 10.1016/j.ijporl.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 19.Huankang Z, Kuanlin X, Xiaolin H, Witt D. Comparison between tracheal foreign body and bronchial foreign body: A review of 1,007 cases. Int J Pediatr Otorhinolaryngol. 2012;76:1719–25. doi: 10.1016/j.ijporl.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 20.Sersar SI, Rizk WH, Bilal M, El Diasty MM, Eltantawy TA, Abdelhakam BB, et al. Inhaled Foreign Bodies: Presentation, management and value of history and plain chest radiography in delayed presentation. Otolaryngol Head Neck Surg. 2006;134:92–9. doi: 10.1016/j.otohns.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 21.Kitcher ED. Foreign Body Inhalation: A review of patients at the Korle Bu Teaching Hospital, Accra, Ghana. West Afr J Med. 2009;28:368–70. doi: 10.4314/wajm.v28i6.55026. [DOI] [PubMed] [Google Scholar]
- 22.Oncel M, Sunam GS, Ceran S. Tracheobronchial aspiration of foreign bodies and rigid bronchoscopy in children. Pediatr Int. 2012;54:532–5. doi: 10.1111/j.1442-200X.2012.03610.x. [DOI] [PubMed] [Google Scholar]
- 23.Sahin A, Meteroglu F, Eren S, Celik Y. Inhalation of foreign bodies in children: Experience of 22 years. J Trauma Acute Care Surg. 2013;74:658–63. doi: 10.1097/TA.0b013e3182789520. [DOI] [PubMed] [Google Scholar]
- 24.Tahir N, Ramsden WH, Stringer MD. Tracheobronchial anatomy and the distribution of inhaled foreign bodies in children. Eur J Pediatr. 2009;168:289–95. doi: 10.1007/s00431-008-0751-9. [DOI] [PubMed] [Google Scholar]
- 25.Oviawe O, Abhulimhen-Iyoha BI, Obaseki DE. Migrating foreign body in the tracheobronchial tree of childen: Report of two cases. Niger Postgrad Med J. 2011;18:154–7. [PubMed] [Google Scholar]
- 26.Van Looij MA, Rood PP, Hoeve LJ, Borgstein JA. Aspirated foreign bodies in children: Why are they more commonly found on the left? Clin Otolaryngol Allied Sci. 2003;28:364–7. doi: 10.1046/j.1365-2273.2003.00725.x. [DOI] [PubMed] [Google Scholar]
- 27.Yeh LC, Li HY, Huang TS. Foreign bodies in tracheobronchial tree in children: A review of cases over a twenty-year period. Changgeng Yi Xue Za Zhi. 1998;21:44–9. [PubMed] [Google Scholar]
- 28.Pinzoni F, Boniotti C, Molinaro SM, Baraldi A, Berlucchi M. Inhaled foreign bodies in pediatric patients: Review of personal experience. Int J Pediatr Otorhinolaryngol. 2007;71:1897–903. doi: 10.1016/j.ijporl.2007.09.002. [DOI] [PubMed] [Google Scholar]


