Abstract
Transfusion associated circulatory overload (TACO) is an established, but grossly under diagnosed and underreported complication of blood transfusion. We present the case of a 46-year-old diabetic and hypertensive patient admitted to our hospital for recurrent episodes of urinary retention. Over initial 3 days of the admission, the patient received multiple units of packed red blood cells (RBC) and fresh frozen plasma, uneventfully. However, the patient developed signs and symptoms suggestive of TACO with only small amount of the 4th unit of RBC. The patient had to be shifted to the Intensive Care Unit for further management of this complication. Etiology of TACO is more complex than a mere circulatory overload and is still not completely understood. TACO leads to a prolonged hospital stay and morbidity in the patients developing this complication. TACO thus needs to be suspected in patients at risk for this complication.
Keywords: Blood transfusion, blood transfusion reaction, risk factors, transfusion associated circulatory overload
Introduction
Transfusion associated circulatory overload (TACO) is an established, but grossly under diagnosed and underreported complication of blood transfusion (BT).[1,2,3] This may be due to the lack of awareness about its diagnostic criteria, dependence of the blood banks on a passive reporting system[2] and masking of this complication by the preexisting patient factors. TACO occurs independently of the patient's underlying condition or other known causes, that may involve the respiratory system. Like transfusion related acute lung injury (TRALI), TACO also is known to be associated with a prolonged Intensive Care Unit (ICU) and hospital stay. However, the short- and long-term mortality remains unaffected in TACO as against TRALI where it is reported to be higher.[4]
Transfusion associated circulatory overload includes any four of the following occurring within 6 h of a BT[3] - acute respiratory distress, tachycardia, increased blood pressure (BP), acute or worsening pulmonary edema and evidence of a positive fluid balance.
Case Report
We present here the case of a 46-year-old known diabetic and hypertensive male admitted with the complaints of recurrent episodes of urinary retention for the past 4 months. Patient had multiple problems in the form of benign prostatic hyperplasia, urinary tract infection, diabetic nephropathy with a creatinine level of 6.1 mg/dL, electrolyte imbalances, small subdural hematoma with organized clot, and a perianal abscess. On the day of the admission, the patient was hemodynamically stable with a clear chest on physical as well as X-ray examination. For low hemoglobin (5.9 g/dL) and a deranged coagulogram, patient received a total of 3 units of red blood cells (RBC) and 5 units of fresh frozen plasma (FFP) over the subsequent 3 days, respectively. All the BTs were given slowly, under a diuretic cover and were uneventful.
However, patient had a reaction to the 4th unit of RBC on day 4 of the admission. After approximately 100 ml of RBC transfusion, patient developed chills, tachypnea (respiratory rate of 46/min), tachycardia (heart rate of 119/min), hypertension (BP increase from a baseline of 120/80-170/90 mm of Hg) and acute dyspnea with hypoxemia (oxygen saturation dropped to 60% on room air).
The patient was afebrile and his chest auscultation revealed the presence of bilateral rhonchi and basal crepts. The chest X-ray done after the BT reaction showed confluent air space opacities and obscured costophrenic angle in the bilateral lung fields [Figure 1]. Diagnosis of an acute respiratory distress syndrome was made on the basis of patient's clinical and X-ray findings. The blood bank was asked to investigate the reaction as a possible anaphylactic or hemolytic transfusion reaction.
Figure 1.
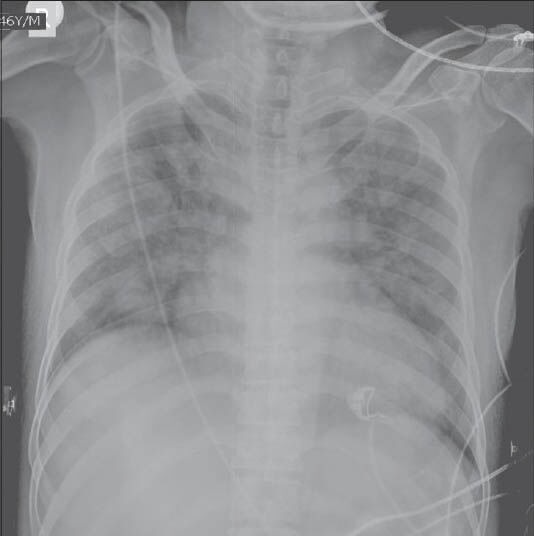
Chest X-ray after transfusion associated circulatory overload
Patient was shifted to the ICU for further management of his condition. He was given intravenous diuretics and oxygen besides other symptomatic support. His oxygen saturation improved to 97% on 4 L of oxygen administered by mask. Patient underwent one cycle of hemodialysis and 2.5 L of fluid was removed from his circulation. Echocardiography revealed a left ventricular ejection fraction of 45%, which was considered as normal for this patient.
Hemolytic reaction was ruled out by the clerical and the serological workup in the blood bank. Although both TACO and TRALI present with similar conditions (pulmonary edema, hypoxemia, and infiltrates on chest X-ray), possibility of a TRALI was ruled out because of several reasons: TRALI is an immune reaction most commonly occurring due to antibodies in donor plasma (coming from parous female or transfused blood donors) reacting with transfused patient's leukocytes. However, all the blood units given to our patient were donated by un-transfused, male donors. Hypotension, one of the typical characteristics of TRALI was absent,[5] instead our patient presented with hypertension – a sign suggestive of circulatory overload as seen in TACO. Facility for testing (elevated) plasma B-type natriuretic peptide levels – a nonspecific marker for TACO was not available at our center.
However, the patient had all other features suggestive of TACO and a thus a diagnosis of TACO was made.
Patient improved symptomatically and O2 saturation improved to 99% the next day. BP was still high at 170/86 mm of Hg. The lung infiltrates and BP improved gradually over the next 5-7 days [Figures 2] and the patient was shifted out of ICU. During his stay in the ward, patient was transfused 1 more unit of RBC and 2 units of FFP uneventfully. Patient improved gradually and after a prolonged stay in the hospital, was discharged on day 17th of the admission.
Figure 2.

Resolved transfusion associated circulatory overload
Discussion
Our patient had three out of the six known risk factors for TACO, viz. renal impairment, hypoalbuminemia (albumin of 2.5 g/dL) and plasma transfusion (received 1400 ml of FFP). The other known risk factors for the TACO are - cardiac impairment, extremes of age and fluid overload.[6,7] Although these factors are known as risk factors, they do not predict the occurrence of a TACO. Our patient had the same risk factors before each BT, but TACO occurred with only one episode of RBC transfusion. It has been suggested that the etiology of TACO may be much more complex than just an excessive blood volume. Exact mechanism leading to TACO has not yet been elucidated and TACO can occur even with small volume of the RBC transfusion, say of 1 unit or less.[4] Blumberg et al., in a retrospective study done at single center, reported substantial reduction in the incidence of TACO after leukodepletion of the blood.[3] However, this hypothesis still needs to be verified by larger studies. Nonetheless, all the RBC units at our center are routinely leukodepleted before storage and this patient also received leukodepleted RBC units.
Clinical assessment of patients before a BT is recommended to identify those at an increased risk for TACO.[5,6]. Particular attention should be given to the appropriateness and rate of the transfusion, diuretic cover and the fluid balance. All the high-risk patients receiving a BT must be carefully observed during and after the BT is over.
Our case highlights the need to correctly identify TACO and differentiate it from other BT reactions. This correct identification in turn can directly influence the treatment, prevention, future BT management and prognosis of the patients experiencing a TACO.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Pandey S, Vyas GN. Adverse effects of plasma transfusion. Transfusion. 2012;52(Suppl 1):65S–79. doi: 10.1111/j.1537-2995.2012.03663.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Narick C, Triulzi DJ, Yazer MH. Transfusion-associated circulatory overload after plasma transfusion. Transfusion. 2012;52:160–5. doi: 10.1111/j.1537-2995.2011.03247.x. [DOI] [PubMed] [Google Scholar]
- 3.Blumberg N, Heal JM, Gettings KF, Phipps RP, Masel D, Refaai MA, et al. An association between decreased cardiopulmonary complications transfusion-related acute lung injury and transfusion-associated circulatory overload and implementation of universal leukoreduction of blood transfusions. Transfusion. 2010;50:2738–44. doi: 10.1111/j.1537-2995.2010.02748.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li G, Kojicic M, Reriani MK, Fernández Pérez ER, Thakur L, Kashyap R, et al. Long-term survival and quality of life after transfusion-associated pulmonary edema in critically ill medical patients. Chest. 2010;137:783–9. doi: 10.1378/chest.09-0841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bux J, Sachs UJ. Pulmonary transfusion reactions. Transfus Med Hemother. 2008;35:337–45. doi: 10.1159/000151349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bolton-Maggs PH, Cohen H On Behalf of the Serious Hazards of Transfusion (SHOT) Steering Group. The 2011 Annual SHOT Report. 2012. [Last accessed on 2013 May 01]. Available from: http://www.shotuk.org/wp-content/uploads/2012/07/shot-annual-report_FinalWebVersionBookmarked_2012_06_22.pdf .
- 7.Alam A, Lin Y, Lima A, Hansen M, Callum JL. The prevention of transfusion-associated circulatory overload. Transfus Med Rev. 2013;27:105–12. doi: 10.1016/j.tmrv.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Popovsky MA, Robillard P, Schipperus M, Stainsby D, Tissot JD, Wiersum J. ISBT Working Party on Hemovigilance. Proposed standard definitions for surveillance of noninfectious adverse transfusion reactions. 2006. [Last accessed on 2013 May 01]. Available from: http://www.ihn-org.com/wp-content/uploads/2011/06/ISBT-definitions-for-non-infectious-transfusion-reactions.pdf .


