Abstract
Background and Purpose
Improving actionable stroke knowledge of a witness or bystander, which in some cases are children, may improve response to an acute stroke event.
Methods
We used a quasi-experimental pretest (PT) post-test design to evaluate actionable stroke knowledge of 210 children aged 9–10 years in response to a single 15-minute exposure to a stroke education video game conducted in the school computer lab. Following immediate post-testing (IP) we provided remote password-protected online video game access, and encouraged children play at their leisure from home. An unannounced delayed post-test (DP) occurred seven weeks later.
Results
Two hundred ten children completed PT, 205 completed IP, while 198 completed DP. 156 (74%) children had home Internet access, and 41 (26%), mostly girls, played the video game remotely. There was significant improvement of stroke symptom composite scores, calling 911 and all individual stroke knowledge items, including a distractor across the testing sequence (p<0.05). Children who played the video game remotely demonstrated significant improvement in knowledge of one symptom (sudden imbalance) compared to children who did not (p<0.05), although overall composite scores showed no difference.
Conclusions
Stroke education video games may represent novel means for improving and sustaining actionable stroke knowledge of children.
Keywords: health education, health disparities, stroke, stroke prevention
Introduction
Since the average 8–12 year-old child plays approximately 13 hours of video games every week,1 supplementing the content of these media with stroke education may represent a powerful way to improve stroke knowledge.
Stroke treatment is time dependent, and activation of the emergency medical service plays a critical role.2 Knowledge of stroke symptoms and the importance of calling 911 (collectively termed “actionable stroke knowledge”) is low among adults and children living in high stroke risk communities.3,4 Although stroke knowledge does not necessarily imply rapid action in all lay-public,5 there may be a sex-specific impact among women.6 Moreover, bystanders and family members may play an important role in calling 911 for suspected stroke, and some of these individuals may include young children.4,7
We previously showed that increasing stroke knowledge of children may lead to increased knowledge in their parents (most of whom were women).8 As part of that program we developed a “clotbuster” stroke video game for the purpose of improving actionable stroke knowledge of children, which in this study we explored as an independent tool. We hypothesized that: 1) the stroke video game will improve stroke knowledge of children after a single 15-minute game round; 2) children will access an online version of the game as a leisurely activity; and, 3) children who access the online game will demonstrate greater stroke knowledge during delayed testing than those who do not.
Methods
Setting and study population
We enrolled a convenience sample of 210 fourth and fifth grade children from one elementary school in Bronx, New York, located in a low-income high stroke risk community. Student ages ranged from 9–12 years (mean age 10) and 52% were female. School level demographic data revealed a student body comprising 65% Hispanic, 18% Asian, 13% Black, 2% White and 2% Native American/Alaska Native. The Columbia University Institutional Review Board approved this study.
Design
We used a quasi-experimental pretest post-test design in which we compared individual’s scores between pretest (PT), immediate post-test (IP), and an unannounced and unanticipated delayed post-test (DP) of gamers using instruments that assess actionable stroke knowledge.
Intervention
Development of the stroke video game (Figure 1) was influenced by social cognitive theory.9 The video game involves navigating a clot-busting spaceship intra-arterially, shooting down clots that occlude the passage of blood to the brain, while avoiding large ‘atherosclerotic’ plaques on the arterial wall. When clotbuster medicine runs out, the gamer must answer stroke knowledge questions in order to refill it and continue playing. Correct answers are provided for incorrect responses, and the game is synced to a hip-hop song with educational lyrics around stroke that also contain the correct answers. This incentive-reward circuit is designed to motivate gamers to learn, creating a loop that increases the gamers’ confidence in his or her mastery or self-efficacy of the stroke information being taught.
Figure 1. Screen shots from Clotbuster stroke video game.
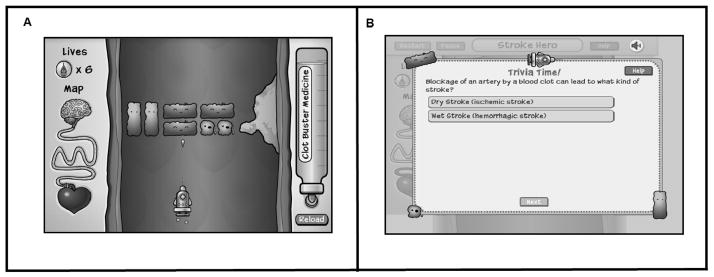
The video game can be played at: http://hiphoppublichealth.org/#!/check-this/
(Registration required)
Gaming Protocol
Children were assembled in a school computer lab and were informed that test scores will not affect their class grades. Following a baseline survey (PT), all children played the video game for a pre-specified 15 minute duration (a single game round), immediately after which they were given an immediate post-test (IP). Following IP, each child was given a “Hip Hop Stroke Hero” card, which contained a unique identifier access code (“secret code”) for logging onto our website to play the stroke video game at home as a leisurely activity. The children were then encouraged to play the game for fun at home. An unannounced delayed post-test was administered seven weeks later.
Assessments
Stroke action (calling 911) was assessed using hypothetical stroke scenarios in which the diagnosis is not revealed such as; “You are eating lunch with a friend and suddenly pieces of his sandwich start falling out if the right side of his mouth and you notice that the right side of his face is drooping down. What should you do?”10 Knowledge of symptoms was assessed using a multiple-choice format, which included the five “suddens” stroke symptoms (except that facial droop was taught in the context of unilateral face, arm, and leg weakness; facial droop was selected on the basis that it is a specific component of the face-arm-speech test, and slurred speech was used a surrogate for speech disturbance in general which includes incomprehensible speech), and a distracter (chest pain). A composite score was created by counting the number of correct multiple-choice responses to the five “suddens” stroke symptoms and the distracter was included make the test consistent with the Behavioral Risk Factor Surveillance System survey.11 The maximum score that could be achieved was six. A second composite score was computed using all of the elements of the first composite score with the addition of calling 911. The maximum score that could be achieved was seven. We also assessed knowledge of stroke localization in the brain, and the term, “brain attack” (a stroke alias).
Statistical Analysis
Chi-square analyses were used for group-wise comparisons for each stroke knowledge question relative to test sequence. Wilcoxon signed-rank tests were used to compare improvement among individual subjects across the testing sequence for overall composite scores of stroke symptom knowledge. Multinomial logistic regression was used to study the effect of website access on composite knowledge scores. All tests were two-sided, with p<0.05 considered statistically significant. All analyses were conducted using IBM SPSS Version 20.
Results
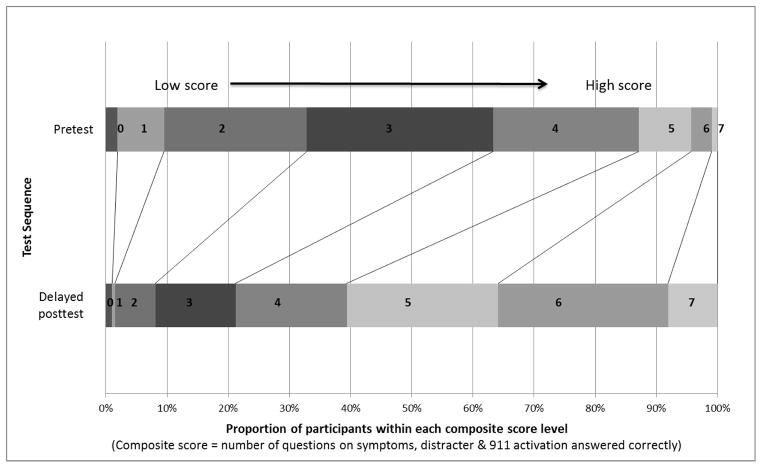
Two hundred and ten children completed PT, 205 completed IP, and 198 completed DP (94% retention). Twenty-five percent of children had a personal experience with stroke victims. Ninety percent of children reported liking the game while 6% did not like the game (4% did not respond). There was significant improvement of stroke symptom composite scores, calling 911, and all individual stroke knowledge items across the testing sequence (all p values <0.05) (Figure 2 & 3). Interestingly, we observed further increases in knowledge of three of five stroke symptoms from IP to DP (sudden imbalance, sudden facial droop, and sudden headache). There were no significant gender differences in post-test stroke knowledge composite scores (p = 0.98). Post hoc we explored the possibility of whether accessing our game online after initial exposure improved stroke knowledge scores. Of 156 children (74%) who reported having home Internet access, 67% reported that they were “confident or very confident” that they would play the game at home. However, only 41 children (26%) (25 of who were girls) played the game remotely between IP and DP. Composite stroke knowledge scores were not significantly different between children who played remotely and those who did not (p = 0.71), although we found a significant increase in knowledge of one symptom (sudden imbalance), favoring children who were exposed at home (p = 0.03), while most other stroke symptoms showed non-significant trends that favored increased knowledge among remote players.
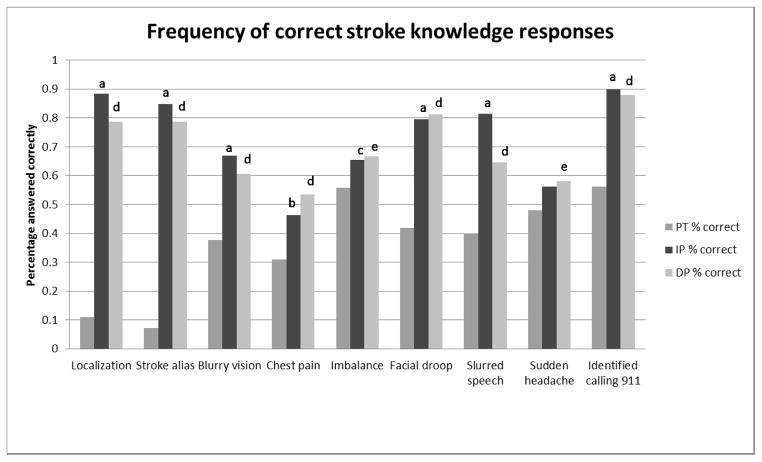
Figure 2. Frequency of correct stroke knowledge responses.
Pretest (PT) vs immediate posttest (IP): ap<0.001, bp<0.01, cp<0.05; PT vs delayed posttest (DP, 7 weeks): dp<0.001, ep<0.05, PT vs IP and PT vs DP: p values are based on χ2 tests.
Localization, stroke alias, and calling 911 were all multiple choice questions with four possible answers (expected correct=25% if subjects had no knowledge), while all others were Yes/No (expected correct=50% if subjects had no knowledge). The localization question regarded which organ in the body a stroke occurs, the stroke alias question targeted the term “brain attack”, and the calling 911 question offered four options for stroke action).
Figure 3. Stroke knowledge before and 7 weeks after video game exposure.
Discussion
Our results show that playing a stroke video game for 15-minutes may improve actionable stroke knowledge of children, which may be retained for up to seven weeks. In addition, we found that one quarter of children (mostly girls) accessed the video game from home as a leisurely activity, and that these children demonstrated some additional improvement in stroke knowledge compared to those who did not.
Although novel to stroke information, incorporating health information into video games is in itself not new. Indeed, educational video games have led to increased nutritional knowledge and eating behaviors,12,13 reduced diabetes-related emergency department visits by children and adolescents with type 1 diabetes,14 and improved adherence to chemotherapy and treatment plans by adolescent patients with cancer.15
Our study has several limitations. We used a quasi-experimental pretest post-test design with a relatively small convenience sample size, and our study did not have a control group. We instead compared test performance with baseline measures in order to minimize disruption of classroom activity by a control program without anticipated educational gain as evidenced by the eighth grade control subjects in another study16 where only slight improvement or worse performance was found for stroke education outcome measures. We used identical measures at each assessment, which is vulnerable to priming effects. Despite 67% of children reporting confidence that they would play the video game at home, only 26% actually did. We did not quantify the frequency and duration of each remote video game encounter in our analysis nor did we explore reasons for the discrepancy between children who said they would play remotely and those who actually did. In addition, we did not account for possible contamination of our sample by other local stroke programs and campaigns during our study period, although we were not aware of any. Finally, we did not perform a cost-benefit analysis of the stroke video game.
Overall, our findings demonstrate that a stroke video game may be an innovative method for improving and sustaining actionable stroke knowledge among young children.
Acknowledgments
The authors would like to thank our Hip Hop Public Health Team.
Sources of Funding. NIH/NINDS 1 R01 NS067443-01A1 (Olajide Williams. PI).
Footnotes
Conflict of Interest Disclosures. None.
References
- 1.Gentile D. Pathological Video-Game Use Among Youth Ages 8 to 18 A National Study. Psychological Science. 2009;20:594–602. doi: 10.1111/j.1467-9280.2009.02340.x. [DOI] [PubMed] [Google Scholar]
- 2.Adams HP, Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. Guidelines for the early management of adults with ischemic stroke. Circulation. 2007;115:e478–e534. doi: 10.1161/CIRCULATIONAHA.107.181486. [DOI] [PubMed] [Google Scholar]
- 3.Willey JZ, Williams O, Boden-Albala B. Stroke literacy in Central Harlem. Neurology. 2009;73:1950–1956. doi: 10.1212/WNL.0b013e3181c51a7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams O, Noble JM. Hip-Hop Stroke. Stroke. 2008;39:2809–2816. doi: 10.1161/STROKEAHA.107.513143. [DOI] [PubMed] [Google Scholar]
- 5.Teuschl Y, Brainin M. Stroke education: discrepancies among factors influencing prehospital delay and stroke knowledge. International Journal of Stroke. 2010;5:187–208. doi: 10.1111/j.1747-4949.2010.00428.x. [DOI] [PubMed] [Google Scholar]
- 6.Muller-Nordhorn J, Wegscheider K, Nolte CH, Jungelhusing GJ, Rossnagel K, Reich A, et al. Population-based intervention to reduce prehospital delays in patients with cerebrovascular events. Archives of Internal Medicine. 2009;169:1484. doi: 10.1001/archinternmed.2009.232. [DOI] [PubMed] [Google Scholar]
- 7.Wein TH, Staub L, Felberg R, Hickenbottom SL, Chan W, Grotta JC, et al. Activation of Emergency Medical Services for Acute Stroke in a Nonurban Population The TLL Temple Foundation Stroke Project. Stroke. 2000;31:1925–1928. doi: 10.1161/01.str.31.8.1925. [DOI] [PubMed] [Google Scholar]
- 8.Williams O, DeSorbo A, Noble J, Gerin W. Child-Mediated Stroke Communication. Stroke. 2012;43:163–169. doi: 10.1161/STROKEAHA.111.621029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allen NA. Social cognitive theory in diabetes exercise research: an integrative literature review. The Diabetes Educator. 2004;30:805–819. doi: 10.1177/014572170403000516. [DOI] [PubMed] [Google Scholar]
- 10.Billings-Gagliardi S, Mazor KM. Development and validation of the stroke action test. Stroke. 2005;36:1035–1039. doi: 10.1161/01.STR.0000162716.82295.ac. [DOI] [PubMed] [Google Scholar]
- 11.Greenlund KJ, Neff LJ, Zheng Z-J, Keene NL, Giles WH, Ayala CA, et al. Low public recognition of major stroke symptoms. American Journal of Preventive Medicine. 2003;25:315–319. doi: 10.1016/s0749-3797(03)00206-x. [DOI] [PubMed] [Google Scholar]
- 12.Turnin M, Tauber M, Couvaras O, Jouret B, Bolzonella C, Bourgeois O, et al. Evaluation of microcomputer nutritional teaching games in 1,876 children at school. Diabetes and Metabolism. 2001;27:459–464. [PubMed] [Google Scholar]
- 13.Baranowski T, Baranowski J, Cullen KW, Marsh T, Islam M, Zakeri I, et al. Squire’s Quest!: dietary outcome evaluation of a multimedia game. American Journal of Preventive Medicine. 2003;24:52–61. doi: 10.1016/s0749-3797(02)00570-6. [DOI] [PubMed] [Google Scholar]
- 14.Brown S, Lieberman DA, Gemeny B, Fan Y, Wilson D, Pasta D. Educational video game for juvenile diabetes: results of a controlled trial. Informatics for Health and Social Care. 1997;22:77–89. doi: 10.3109/14639239709089835. [DOI] [PubMed] [Google Scholar]
- 15.Kato PM, Cole SW, Bradlyn AS, Pollock BH. A video game improves behavioral outcomes in adolescents and young adults with cancer: A randomized trial. Pediatrics. 2008;122:e305–e317. doi: 10.1542/peds.2007-3134. [DOI] [PubMed] [Google Scholar]
- 16.Morgenstern LB, Gonzales NR, Maddox KE, Brown DL, Karim AP, Espinosa N, et al. A Randomized, Controlled Trial to Teach Middle School Children to Recognize Stroke and Call 911 The Kids Identifying and Defeating Stroke Project. Stroke. 2007;38:2972–2978. doi: 10.1161/STROKEAHA.107.490078. [DOI] [PubMed] [Google Scholar]