Abstract
BACKGROUND:
Despite a high prevalence of complementary alternative medicine (CAM) use among inflammatory bowel disease (IBD) patients, there is a dearth of information about the attitudes and perceptions of CAM among the gastroenterologists who treat these patients.
OBJECTIVE:
To characterize the beliefs, perceptions and practices of gastroenterologists toward CAM use in patients with IBD.
METHODS:
A web-based survey was sent to member gastroenterologists of the Canadian Association of Gastroenterology. The survey included multiple-choice and Likert scale questions that queried physician knowledge and perceptions of CAM and their willingness to discuss CAM with patients.
RESULTS:
Fifty-three per cent of respondents considered themselves to be IBD subspecialists. The majority (86%) of gastroenterologists reported that less than one-half of their patient population had mentioned the use of CAM. Only 8% of physicians reported initiating a conversation about CAM in the majority of their patient encounters. Approximately one-half (51%) of respondents were comfortable with discussing CAM with their patients, with lack of knowledge being cited as the most common reason for discomfort with the topic. Most gastroenterologists (79%) reported no formal education in CAM. While there was uncertainty as to whether CAM interfered with conventional medications, most gastroenterologists believed it could be effective as an adjunct treatment.
CONCLUSION:
Our findings demonstrate that gastroenterologists were hesitant to initiate discussions about CAM with patients. Nearly one-half were uncomfortable or only somewhat comfortable with the topic, and most may benefit from CAM educational programs. Interestingly, most respondents appeared to be receptive to CAM as adjunct therapy alongside conventional IBD treatment.
Keywords: CAM, Complementary alternative medicine, Crohn disease, IBD, Inflammatory bowel disease, Ulcerative colitis
Abstract
HISTORIQUE :
Malgré la forte prévalence de la médecine complémentaire et parallèle (MCP) chez les patients ayant une maladie inflammatoire de l’intestin (MII), il y a pénurie d’information sur les attitudes et perceptions de la MCP chez les gastroentérologues qui traitent ces patients.
OBJECTIF :
Caractériser les croyances, les perceptions et les pratiques des gastroentérologues envers l’utilisation de la MCP chez les patients atteints d’une MII.
MÉTHODOLOGIE :
Les gastroentérologues membres de l’Association canadienne de gastroentérologie ont reçu un sondage virtuel. Ce sondage contenait des questions à choix multiples et des questions sur l’échelle de Likert pour s’informer de leurs connaissances et perceptions de la MCP et de leur volonté à parler de MCP avec leurs patients.
RÉSULTATS :
Cinquante-trois pour cent des répondants se considéraient comme des surspécialistes des MII. Selon la majorité (86 %) des gastroentérologues, moins de la moitié de leur population de patients indiquait utiliser la MCP. Seulement 8 % des médecins ont affirmé lancer une conversation sur la MCP lors de la majorité de leurs rencontres avec les patients. Environ la moitié (51 %) des répondants était à l’aise de discuter de MCP avec les patients, le manque de connaissances étant cité comme la principale raison d’être mal à l’aise d’aborder le sujet. La plupart des gastroentérologues (79 %) ont indiqué ne pas posséder de formation officielle sur la MCP. Même s’ils n’étaient pas certains de la possibilité d’interaction de la MCP avec les médicaments classiques, la plupart des gastroentérologues croyaient qu’elle pouvait être efficace comme traitement d’appoint.
CONCLUSION :
Nos observations démontrent que les gastroentérologues hésitaient à lancer des discussions sur la MCP avec leurs patients. Près de la moitié n’était pas à l’aise ou plutôt mal à l’aise de parler de ce sujet, et la plupart pourraient profiter de programmes de formation sur la MCP. Fait intéressant, la plupart des répondants semblent réceptifs à la MCP comme traitement d’appoint à la thérapie classique des MII.
Patients with inflammatory bowel disease (IBD), including ulcerative colitis (UC) and Crohn disease, use complementary alternative medicine (CAM) more frequently than the general population (1,2). The popularity of CAM among IBD patients is due, in part, to the chronicity and severity of these diseases, resulting in patients seeking alternative treatments. Furthermore, patients with IBD comprise a well-educated population with a desire to gain control over their illness (3,4). CAM can serve as a coping mechanism through which patients can retain a sense of influence and independence in their treatment course. In addition, adverse effects experienced while taking some IBD medications may prompt patients to seek alternative treatments. Given the correlation between steroid use and CAM use among IBD patients, it is speculated that the adverse effects of these commonly used drugs drives the use of CAM (5,6). Due to the increasing use of information technology, along with a more informed and educated patient population, it can be expected that CAM will continue to play a prominent role in the holistic care of patients with IBD.
CAM may provide IBD patients with a greater sense of control over their disease treatment; however, its use remains controversial among gastroenterologists (7,8). CAM has traditionally been difficult to study for multiple reasons including: a universally accepted definition of CAM does not exist; studies investigating CAM have significant limitations including a lack of randomized controlled trials, small sample sizes and selection biases; and an inability to study CAM methods without the use of concurrent conventional medications (3,9). There is also skepticism of CAM because of its potential to cause harm. Herbal therapies – the most common form of CAM used by IBD patients – have contributed to liver and renal failure (1,10,11). Other dangers include the addition of prescription medications in ‘natural’ products, along with the transmission of infectious diseases through contamination of needles and other sharps (4,12). Despite the inconsistencies and potential harm, CAM use continues to rise among the general population (5,13–16).
A survey suggested that 47% of Canadian patients with IBD used CAM to treat their IBD at some point in time (7). Studies from other countries have found similar rates of CAM use among IBD patients (17). Interestingly, most patients do not receive information about CAM from their gastroenterologists (18,19), which is concerning for several reasons. For example, adverse interactions between CAM therapies and conventional medications have been documented (20). As a result, patients who withhold information about their CAM use from their gastroenterologists may be putting themselves at risk. Interestingly, one study found that 50% of patients with IBD who use CAM do not believe there is scientific evidence to support their practices (19). This apparent contradiction may further represent a lack of meaningful communication between patients and their gastroenterologists.
While many studies have investigated the patterns of CAM use among IBD patients, limited data regarding gastroenterologist perceptions and beliefs regarding CAM (6,7,20) exist. To address this gap in knowledge, a survey study was directed toward Canadian gastroenterologists. The present article reports findings on how gastroenterologists communicate with patients regarding CAM; their reactions to patient CAM use; and potential ways in which CAM can be incorporated into the treatment of IBD.
METHODS
A questionnaire was developed to assess gastroenterologist attitudes and opinions regarding CAM. Situational questions involving CAM use by patients, as well as questions regarding specific CAM modalities, were used. In the survey, CAM referred to ‘complementary alternative medicine’, which included but was not limited to meditation, acupuncture, traditional Chinese medicine, probiotics, massage and herbal diets. Multiple IBD specialists reviewed the survey and provided input to increase validity. Demographic data were solicited. The questionnaire was administered using an online survey engine (Novi-Survey).
The survey was sent to active members of the Canadian Association of Gastroenterology, who were medical doctors and not trainees, via their monthly e-mail invitation. Participants were encouraged to only complete the survey once. Surveys were sent in English only. After selecting the link to the survey site, participants were given an explanation of the study. Consent was implied if participants proceeded with the survey.
Before accessing the survey, participants were screened for suitability for the study. Participants were required to be practicing physicians, who in the past 12 months had participated in the care of patients with IBD, and had completed medical, specialty and/or subspecialty training. A combination of contingency, matrix and closed-ended questions were used in the questionnaire. All data were collected anonymously. Continuous variables are presented as means and SDs.
Some groups were collapsed for comparisons and analysis. IBD subspecialists and those with >50% of their practice including IBD patients were combined to categorize the comparison group ‘IBD subspecialist’. In classifying comfort level with CAM, ‘somewhat comfortable’ and ‘not comfortable’ were combined into a single category of ‘uncomfortable’, while ‘comfortable’ and ‘very comfortable’ were combined into the category ‘comfortable’. Certain categorical data of percentages were collapsed for comparison among groups. Comparisons of categorical variables between subgroups were performed using the χ2 test or Fisher’s exact test.
The study protocol was approved by the Research Ethics Board of Mount Sinai Hospital, Toronto, Ontario.
RESULTS
All active clinical, nontrainee members of the the Canadian Association of Gastroenterology were invited to participate in the survey via e-mail. There were 96 respondents to the survey, yielding a response rate of 22%. Among these, 87 met the inclusion criteria and completed the survey. The mean (± SD) length of time in practice was 13.5±9.0 years (Table 1). One-third of the respondents practiced primarily in a community setting, while the remaining two-thirds practiced in an academic setting or had an academic affiliation. The majority (69%) of respondents’ clinical practices were limited to adult gastroenterology, while 18% practiced both internal medicine and gastroenterology; and 13% practiced only pediatric gastroenterology. Slightly more than one-half (53%) identified themselves as IBD subspecialists. However, a majority (60%) reported that fewer than one-quarter of their practice comprised IBD patients (Table 1).
TABLE 1.
Practice characteristics of respondents
| Years in practice, mean ± SD | 13.5±9.0 |
| Primary practice setting | |
| Academic | 54 (62) |
| Community | 29 (33) |
| Both | 4 (5) |
| Scope of practice | |
| Limited to adult gastroenterology | 60 (69) |
| Gastroenterology and internal medicine | 16 (18) |
| Pediatric gastroenterology | 11 (12) |
| Surgery | 0 (0) |
| Other | 0 (0) |
| Gastroenterology practice patients with IBD, % | |
| <10 | 16 (18) |
| 10–25 | 36 (41) |
| 25–50 | 20 (23) |
| >50 | 15 (17) |
| Subspecialist in IBD | |
| Yes | 46 (53) |
| No | 41 (47) |
Data presented n (%) unless otherwise indicated. IBD Inflammatory bowel disease
The survey explored the nature of the patient-physician interaction with respect to CAM use. A vast majority (86%) of gastroenterologists reported that fewer than one-half of their patients mentioned the use of CAM in their discussion of IBD treatment. A minority (18%) of gastroenterologists reported that they initiated discussions about CAM in the majority of their patient encounters. IBD subspecialists were more inclined to do so than nonsubspecialists (28% versus 5%, respectively; P=0.02). However, academic gastroenterologists were not more likely to initiate discussions regarding CAM than their community counterparts (20% versus 14%; P=0.3). Only a minority (12%) of gastroenterologists believed that more than one-half of their patients used CAM without reporting it (Table 2). Physicians perceived the most common reason to not report CAM use was fear of physician disapproval (Figure 1).
TABLE 2.
Gastroenterologist perceptions and practices regarding complementary alternative medicine (CAM)
| <10% | 10% – 25% | >25% – 50% | >50% | |
|---|---|---|---|---|
| What percentage of your patients has mentioned the use of CAM as a part of their treatment of inflammatory bowel disease? | 18 (21) | 36 (41) | 21 (24) | 12 (14) |
| How often do you initiate a discussion with your patients about their use of CAM? | 34 (40) | 24 (28) | 11 (13) | 15 (18) |
| How often does a patient with IBD initiate a discussion about their use of CAM? | 20 (23) | 34 (39) | 26 (13) | 7 (8) |
| What percentage of your patients do you think use CAM and do not tell you about it? | 10 (12) | 33 (38) | 33 (38) | 10 (12) |
Data presented as n (%). IBD Inflammatory bowel disease
Figure 1).
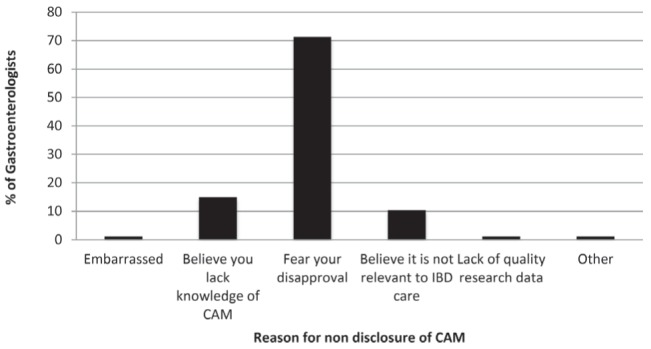
Perceived reasons by gastroenterologists that patients do not disclose their use of complementary alternative medicine (CAM). IBD Inflammatory bowel disease
Only one-half of respondents (51%) were comfortable or very comfortable discussing CAM with their patients (Figure 2A). There was no difference in comfort level between IBD subspecialists and nonsubspecialists (57% versus 43%, respectively; P=0.20) or between community and academic gastroenterologists (57% versus 38%, respectively; P=0.12). The most commonly cited reason for feeling uncomfortable or somewhat comfortable was a lack of knowledge on CAM (Figure 2B). Most gastroenterologists (79%) reported having never attended a formal education program on CAM, which included training in medical school, contnuing medical education (CME) sessions, hospital workshops or structured independent learning. Among the minority that received formal training in CAM, 72% gained exposure through CME activities. IBD subspecialists were no more likely to have undergone formal training in CAM than nonsubspecialists (28% versus 13%; P=0.11). Community and academic gastroenterologists also reported similar exposure to formal CAM education (22% versus 17%; P=0.78).
Figure 2).
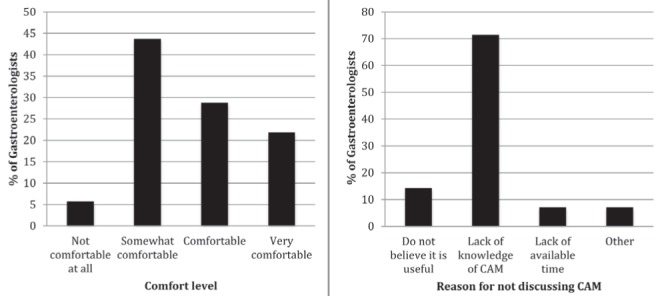
A Comfort levels of gastroenterologists when discussing complementary alternative medicine (CAM) with their patients. B Reason that respondents were not comfortable or only somewhat comfortable discussing CAM with patients
Nearly one-half of physicians (47%) reported that they did not have a systematic or standardized approach to the discussion of CAM, and that their conversations with patients on the topic of CAM varied from individual to individual. Nearly one-third (32%) of gastroenterologists were willing to at least participate in an initial discussion regarding CAM, while a minority (15%) were doubtful that they would be able to add to such a discussion due to lack of knowledge on the topic. Only two gastroenterologists outright dismissed CAM, and two referred patients to an alternative practitioner, while one actively recommended its use.
Overall, gastroenterologists reported broad familiarity with the types of CAM. The majority (77%) of respondents had heard of and recommended probiotics (Figure 3). More than three-quarters of respondents had heard of each of the following CAM modalities: probiotics, prebiotics, herbal remedies, aloe vera, marijuana, fish oil and acupuncture. However, none of these modalities were recommended by more than 30% of gastroenterologists (Figure 3). The vast majority (90%) of gastroenterologists had, at some point, recommended at least one form of CAM listed on the survey. IBD subspecialists were no more likely to recommend CAM than non-IBD subspecialists (87% versus 93%; P=0.5). Similarly, the proportion of academic and community gastroenterologists who recommended at least one form of CAM did not significantly differ (91% versus 86%; P=0.47).
Figure 3).
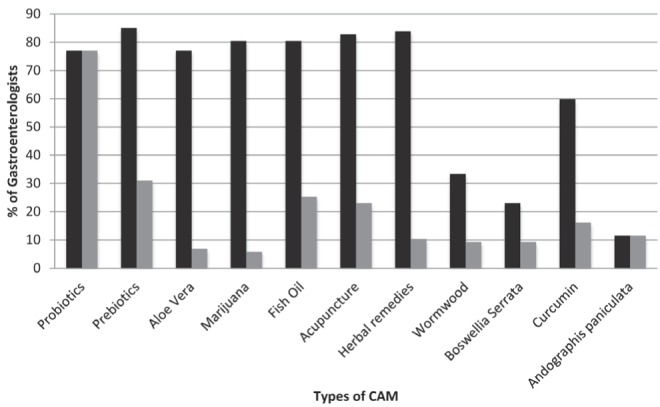
Gastroenterologists’ familiarity with and recommendation practices for specific modalities of complementary alternative medicine (CAM). Black bars represent the proportion of respondents who were familiar with a specific type of CAM and grey bars represent the proportion who recommended that specific modality
Table 3 summarizes gastroenterologists’ beliefs and attitudes toward CAM. Most respondents believed that patients who respond poorly to conventional therapy exhibited more willingness to use CAM. A vast majority believed that their patients would still use CAM irrespective of the physician’s recommendations. Most respondents affirmed that CAM should be subjected to strict regulations by health agencies and that research in CAM efficacy should be a high priority. There was moderate uncertainty as to whether CAM would interfere with adherence to conventional medical management of IBD. However, the majority (57%) of respondents posited that CAM could serve as an effective adjunct to conventional therapy.
TABLE 3.
Perceptions of complementary alternative medicine (CAM) efficacy, user characteristics and utility in patients who use CAM to treat inflammatory bowel disease
| Strongly disagree | Disagree | Somewhat disagree | Undecided | Somewhat agree | Agree | Strongly agree | |
|---|---|---|---|---|---|---|---|
| Patients that have poor response to conventional inflammatory bowel disease therapy tend to use more CAM | 0 (0) | 1 (1) | 9 (11) | 8 (10) | 37 (44) | 22 (26) | 7 (8) |
| My patients will pursue CAM despite my recommendations for or against it | 1 (1) | 1 (1) | 7 (8) | 13 (16) | 34 (45) | 24 (29) | 4 (5) |
| Women, high income and high education patients are more likely to use CAM | 0 (0) | 3 (4) | 10 (12) | 23 (28) | 26 (31) | 17 (21) | 4 (5) |
| My patients would benefit from a wellness centre at my institution that could provide access to CAM providers | 4 (5) | 9 (11) | 15 (18) | 21 (25) | 19 (23) | 11 (13) | 5 (6) |
| CAM can be an effective adjunct to the management of inflammatory bowel disease | 2 (2) | 7 (8) | 11 (13) | 16 (19) | 32 (38) | 13 (16) | 3 (4) |
| CAM should be subject to strict regulations by governing health agencies | 2 (2) | 1 (1) | 4 (5) | 11 (13) | 16 (19) | 24 (29) | 26 (31) |
| Research in the efficacy and safety of CAM should be a high priority | 1 (1) | 2 (2) | 4 (5) | 9 (11) | 24 (29) | 28 (34) | 15 (19) |
| CAM interferes with the adherence to medical management of inflammatory bowel disease | 1 (1) | 13 (16) | 25 (30) | 19 (23) | 21 (25) | 5 (6.0) | 0 (0) |
| When in doubt about potential drug-drug interactions of a CAM supplement, I call a pharmacist for clarification | 3 (4) | 18 (21) | 11 (13) | 10 (12) | 19 (23) | 14 (17) | 9 (11) |
Data presented as n (%)
DISCUSSION
The present survey reports data regarding the current practices and attitudes of Canadian gastroenterologists toward patients who use CAM to treat IBD. Considering the widespread and increasing use of CAM, we believe it is necessary to gain an understanding of physician opinions and comfort levels with CAM, along with how these attitudes influence their interaction with patients. This information may help enhance the overall patient-physician encounter by fostering increased opportunities for communication. To our knowledge, the present study was the first to assess Canadian gastroenterologists’ beliefs and practices related to CAM use.
Understanding the dynamics that surround the discussion of CAM can promote more open discussions between patients and their treating physicians. In our study, gastroenterologists perceived that patients most often instigate conversations regarding CAM. However, a majority of respondents believed that fewer than one-half of their patient population failed to disclose CAM use. Previous studies using patient self-report questionnaires have presented conflicting data regarding patient disclosure of CAM use. A survey sent to members of the Crohn’s and Colitis Foundation found that 71% of IBD patients had discussed CAM with their doctors, while only 13% were uncomfortable doing so (7). Ganguli et al (1) found that 43% of IBD patients had discussed CAM with their gastroenterologist. However, another study of IBD patients found that only 34% had consulted with their gastroenterologist before using CAM (3). The variations in findings likely reflect inherent differences in study populations, design and tools, but underscore the underlying gravity of the problem. Physicians in our study speculated that fear of physician disapproval was a major contributing factor for the lack of disclosure, which mirror concerns expressed by Hilsden (7). Thus, physicians may need to initiate discussions about CAM with their patients to assure them that they will not be judged negatively for discussing alternative therapies. Regardless of the physician’s initial beliefs regarding CAM, these conversations to ascertain whether a patient is using CAM for the treatment of IBD are important for assessing whether it is interfering with adherence to prescribed conventional therapies and the safety of the particular type of CAM being used. These discussions also provide an opportunity for physicians to disseminate accurate information, reliable sources of patient information and evidence-based recommendations regarding CAM.
Unfortunately, our study showed that fewer than one-quarter of physicians initiated discussions regarding CAM primarily because of discomfort with and lack of knowledge of the topic. Encouragingly, respondents appeared to be receptive to the role of CAM as adjunct therapy alongside conventional treatment. For more physicians to gain the confidence and comfort level to instigate conversations about CAM, more educational directives may be needed, either during training or CME programs, that address the topic. The vast majority of respondents had no formal education on CAM. Even guidance on a standardized approach to discussing CAM may facilitate these conversations because most physicians did not have one. One strategy is to routinely ask about CAM use during review of medications.
Given the high prevalence of CAM use, an increasingly important therapeutic consideration for gastroenterologists is the impact of alternative therapies on adherence to conventional IBD treatment; there was uncertainty among our respondents as to whether this was the case. A previous questionnaire-based study found that 24% of IBD patients agreed that CAM resulted in abandoning their use of conventional medicine (7). However, in a cross-sectional study conducted by Weizman et al (3), overall medication adherence did not significantly differ between CAM users and nonusers. A concerning finding from one survey on CAM use found that one in 12 patients reported being told by CAM practitioners to change their conventional medications prescribed by physicians (1). Similar data from the United Kingdom showed that CAM providers occasionally advised patients with celiac disease to adjust their prescribed medication dosage, without consulting the treating physicians (21).
Another reason gastroenterologists cited for not initiating discussions regarding CAM was lack of time. These concerns introduce the possible role of other health providers in educating patients about CAM – particularly pharmacists. In the current survey, there was also little consensus from gastroenterologists regarding the role of pharmacists in managing conventional medications and those prescribed by alternative practitioners. The role of the pharmacist in CAM has not been well elucidated in general. While pharmacists agree that they could serve an important role by performing medication reviews of patients who use CAM, they also report a need for additional formal and interprofessional training on CAM (13).
One unifying concern regarding CAM among gastroenterologists was the lack of evidence-based data. Numerous randomized controlled trials have tested the efficacy of certain CAM modalities on gastrointestinal symptoms and disease end points. However, design flaws and small sample sizes remain a reason for skepticism among gastroenterologists (14,16). The majority of gastroenterologists in the present survey agreed that research on the efficacy of CAM should remain a high priority. Herbal medications and probiotics are the most commonly used CAM for IBD (7,18,22). Results from our study showed that gastroenterologists frequently recommended probiotics for IBD, which may be attributable to evidence from clinical trials for pouchitis and UC (23). A meta-analysis from a Cochrane review (24) found limited evidence that probiotics added to standard therapy was modestly effective at inducing remission of disease activity in mild to moderate UC. A separate Cochrane review found insufficient evidence that probiotics were effective in the maintenance of remission of UC compared with placebo (25). Interestingly, most gastroenterologists surveyed did not recommend herbal remedies. Therefore, it is likely that the majority of IBD patients are being prescribed herbal supplements by nonphysicians.
There were several limitations to our survey, the first of which was the possiblity of response bias. Although the response rate (22%) was low, it is not unexpected for an e-mail-based survey that targeted all gastroenterologists throughout Canada. We could have increased the response rate by inviting only academic gastroenterologists, but we believed that it was also important to include representation from community gastroenterologists. We should note that our survey likely reflected under-representation from community gastroenterologists; however, there were no statistically significant different responses between academic and community gastroenterologists. An additional limitation was the lack of a unifying definition for CAM and, thus, the likelihood that the entire spectrum of CAM practices was not captured. The survey did provide an option to mention CAM modalities that we did not list. It does not appear that we omitted major forms of CAM because only eight gastroenterologists suggested additional forms of CAM.
CAM will continue to play a role in the physician-patient relationship. The use of CAM has risen steadily in the United Kingdom and Canada, and will likely continue to rise (5,15,26). As a result of the increasing use of CAM, the College of Physicians and Surgeons of Ontario recently revised a policy statement regarding how physicians should address patient use of CAM (27). Among other points, the policy recommends that “physicians inquire about patient use of CAM on a regular basis,” and document this in the medical record (27). It is recommended that physicians read these policies to gain a better understanding of the most productive way to engage and advise their patients. In the present study, there was a lack of consensus among gastroenterologists on how CAM use may influence the patient-physician relationship. Additional educational opportunities, along with a unifying training and CME approach, possibly mandated from specific subspecialty organizations, may guide physicians in effectively counselling and guiding patients.
REFERENCES
- 1.Ganguli SC, Cawdron R, Irvine EJ. Alternative medicine use by Canadian ambulatory gastroenterology patients: Secular trend or epidemic? Am J Gastroenterol. 2004;99:319–26. doi: 10.1111/j.1572-0241.2004.04046.x. [DOI] [PubMed] [Google Scholar]
- 2.Haas L, McClain C, Varilek G. Complementary and alternative medicine and gastrointestinal diseases. Curr Opin Gastroenterol. 2000;16:188–96. doi: 10.1097/00001574-200003000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Weizman AV, Ahn E, Thanabalan R, et al. Characterisation of complementary and alternative medicine use and its impact on medication adherence in inflammatory bowel disease. Aliment Pharmacol Ther. 2001;35:342–9. doi: 10.1111/j.1365-2036.2011.04956.x. [DOI] [PubMed] [Google Scholar]
- 4.Moser G, Tillinger W, Sachs G, et al. Relationship between the use of unconventional therapies and disease-related concerns: A study of patients with inflammatory bowel disease. J Psychoso Res. 1996;40:503–9. doi: 10.1016/0022-3999(95)00581-1. [DOI] [PubMed] [Google Scholar]
- 5.Li FX, Verhoef MJ, Best A, Otley A, Hilsden RJ. Why patients with inflammatory bowel disease use or do not use complementary and alternative medicine: A Canadian national survey. Can J Gastroenterol. 2005;19:567–73. doi: 10.1155/2005/943547. [DOI] [PubMed] [Google Scholar]
- 6.Langhorst J, Anthonisen IB, Steder-Neukamm U, et al. Amount of systemic steroid medication is a strong predictor for the use of complementary and alternative medicine in patients with inflammatory bowel disease: Results from a German national survey. Inflamm Bowel Dis. 2005;11:287–95. doi: 10.1097/01.mib.0000160771.71328.6c. [DOI] [PubMed] [Google Scholar]
- 7.Hilsden R. Complementary and alternative medicine use by Canadian patients with inflammatory bowel disease: Results from a national survey. Am J Gastroenterol. 2003;98:1563–8. doi: 10.1111/j.1572-0241.2003.07519.x. [DOI] [PubMed] [Google Scholar]
- 8.Hilsden RJ, Scott CM, Verhoef MJ. Complementary medicine use by patients with inflammatory bowel disease. Am J Gastroenterol. 1998;93:697–701. doi: 10.1111/j.1572-0241.1998.208_a.x. [DOI] [PubMed] [Google Scholar]
- 9.Bernstein CN. Complementary and alternative medicine use by patients with inflammatory bowel disease: Are Canadian physicians failing with conventional therapy, or not. Can J Gastroenterol. 2004;18:47–8. doi: 10.1155/2004/507410. [DOI] [PubMed] [Google Scholar]
- 10.Barnes J. Pharmacovigilance of herbal medicines. Drug Safety. 2003;26:829–51. doi: 10.2165/00002018-200326120-00001. [DOI] [PubMed] [Google Scholar]
- 11.Langmead L, Rampton D. Review article: Complementary and alternative therapies for inflammatory bowel disease. Aliment Pharmacol Ther. 2006;23:341–9. doi: 10.1111/j.1365-2036.2006.02761.x. [DOI] [PubMed] [Google Scholar]
- 12.Ernst E, Sherman KJ. Is acupuncture a risk factor for hepatitis? Systematic review of epidemiological studies. J Gastroenterol Hepatol. 2003;18:1231–6. doi: 10.1046/j.1440-1746.2003.03135.x. [DOI] [PubMed] [Google Scholar]
- 13.Koh H-L, Teo H-H, Ng H-L. Pharmacists’ patterns of use, knowledge, and attitudes toward complementary and alternative medicine. J Altern Complement Med. 2003;9:51–63. doi: 10.1089/107555303321222946. [DOI] [PubMed] [Google Scholar]
- 14.Koretz RL, Rotblatt M. Complementary and alternative medicine in gastroenterology: The good, the bad, and the ugly. Clin Gastroenterol Hepatol. 2004;2:957–67. doi: 10.1016/s1542-3565(04)00461-6. [DOI] [PubMed] [Google Scholar]
- 15.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: Results of a follow-up national survey. JAMA. 1998;280:1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 16.Hilsden RJ, Verhoef MJ. Complementary and alternative medicine: Evaluating its effectiveness in inflammatory bowel disease. Inflamm Bowel Dis. 1998;4:318–23. doi: 10.1002/ibd.3780040411. [DOI] [PubMed] [Google Scholar]
- 17.Burgmann T, Rawsthorne P, Bernstein CN. Predictors of alternative and complementary medicine use in inflammatory bowel disease: Do measures of conventional health care utilization relate to use? Am J Gastroenterol. 2004;99:889–93. doi: 10.1111/j.1572-0241.2004.30033.x. [DOI] [PubMed] [Google Scholar]
- 18.Limdi JK, Butcher RO. Complementary and alternative medicine use in inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:E86–8. doi: 10.1002/ibd.21748. [DOI] [PubMed] [Google Scholar]
- 19.Gangl A. Alternative and complementary therapies for inflammatory bowel disease. Nat Clin Pract Gastroenterol Hepatol. 2006;3:180–1. doi: 10.1038/ncpgasthep0445. [DOI] [PubMed] [Google Scholar]
- 20.Kong SC, Hurlstone DP, Pocock CY, et al. The incidence of self-prescribed oral complementary and alternative medicine use by patients with gastrointestinal diseases. J Clin Gastroenterol. 2005;39:138–41. [PubMed] [Google Scholar]
- 21.Moody GA, Eaden JA, Bhakta P, Sher K, Mayberry JF. The role of complementary medicine in European and Asian patients with inflammatory bowel disease. Public Health. 1998;112:269–71. doi: 10.1038/sj.ph.1900469. [DOI] [PubMed] [Google Scholar]
- 22.Tillisch K. Complementary and alternative medicine for gastrointestinal disorders. Clin Med. 2007;7:224–7. doi: 10.7861/clinmedicine.7-3-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holubar SD, Cima R, Sandborn WJ, et al. Treatment and prevention of pouchitis after ileal pouch-anal anastomosis for chronic ulcerative colitis. Cochrane Database Syst Rev. 2010;(6):CD001176. doi: 10.1002/14651858.CD001176.pub2. [DOI] [PubMed] [Google Scholar]
- 24.Naidoo K, Gordon M, Fagbemi O, Thomas G, Akobeng A. Probiotics for maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev. 2011;(12):CD007443. doi: 10.1002/14651858.CD007443.pub2. [DOI] [PubMed] [Google Scholar]
- 25.Mallon P, McKay D, Kirk S, Gardiner K. Probiotics for induction of remission in ulcerative colitis. Cochrane Database Syst Rev. 2007;(4):CD005573. doi: 10.1002/14651858.CD005573.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Maha N, Shaw A. Academic doctors’ views of complementary and alternative medicine (CAM) and its role within the NHS: An exploratory qualitative study. BMC Complement Altern Med. 2007;7:17. doi: 10.1186/1472-6882-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.College of Physicians and Surgeons of Ontario Policy Statement #3–11. Dialogue. 2011;1:4. [Google Scholar]


