Abstract
Background
Current 30-day readmission models used by the Center for Medicare and Medicaid Services for the purpose of hospital-level comparisons lack measures of socioeconomic status (SES). We examined whether the inclusion of a SES measure in 30-day congestive heart failure (CHF) readmission models changed hospital risk standardized readmission rates (RSRR) in New York City (NYC) hospitals.
Methods and Results
Using a Centers for Medicare & Medicaid Services (CMS)-like model we estimated 30-day hospital-level RSRR by adjusting for age, gender and comorbid conditions. Next, we examined how hospital RSRRs changed relative to the New York City mean with inclusion of the Agency for Healthcare Research and Quality (AHRQ) validated SES index score. In a secondary analysis, we examined whether inclusion of the AHRQ SES Index score in 30-day readmission models disproportionately impacted the RSRR of minority-serving hospitals.
Higher AHRQ SES scores, indicators of higher socioeconomic status, were associated with lower odds, 0.99, of 30-day readmission (p< 0.019). The addition of the AHRQ SES index did not change the model’s C statistic (0.63). After adjustment for the AHRQ SES index, one hospital changed status from “worse than the NYC average” to “no different than the NYC average”. After adjustment for the AHRQ SES index, one NYC minority-serving hospital was re-classified from “worse” to “no different than average”.
Conclusions
While patients with higher SES were less likely to be admitted, the impact of SES on readmission was very small. In NYC, inclusion of the AHRQ SES score in a CMS based model did not impact hospital-level profiling based on 30-day readmission.
Keywords: Congestive heart failure, readmission, socioeconomic status, CMS profiling
INTRODUCTION
The high prevalence of congestive heart failure (CHF)1, 2 imposes a large burden on patients, their families, and the health care system. For example, CHF is the most common cause of hospital readmissions among Medicare beneficiaries, costing the Medicare program $15 billion annually, of which $12 billion may be preventable.3 In 2005, the Deficit Reduction Act mandated that hospital performance measurements be made publicly available and that these should include CHF readmission rates. To assess hospital performance, the Centers for Medicare & Medicaid Services (CMS), developed a model to create hospital-level CHF risk standardized readmission rates (RSRR).4 The model accounts only for patient co-morbid health conditions and age and gender. Hospital-level 30-day CHF readmission rates based on this risk-standardized model became publicly available in 2005 through the Hospital Compare website.5
Under the Hospital Readmissions Reduction program, hospitals with “excessive” readmissions (i.e. when the number of patients readmitted to a hospital is more than expected) began losing a percentage of their Medicare reimbursement as of October, 2012. In fiscal year 2013, the decrease reached one percent of reimbursement, rising to two percent in 2014 and three percent in 2015.6 A total of 2,217 hospitals were penalized up to 1% of Medicare reimbursements in the first year of the program, and from those 307 will be penalized the maximum 1%.7
Readmission penalties potentially pose a tremendous financial threat to hospitals that serve vulnerable populations because the CMS’ risk model does not adjust for socioeconomic status (SES). Policymakers at CMS excluded SES from their model because of the belief that all hospitals should provide the same quality of care regardless of the resources of the people they serve.8 However, socioeconomic and social risk factors such as poverty, low educational attainment, and limited social support result in worse health care outcomes.9, 10 For example, black residents of New York City’s (NYC) poorest neighborhoods have nearly 50% higher mortality rates than black residents living in wealthier neighborhoods.11 Similarly, white residents in poor communities also have higher mortality rates than whites in the wealthiest (771 vs. 552 per 100,000).12
Recent research has demonstrated that the predictive ability of models to predict CHF readmissions are improved with the addition of socioeconomic factors that represent the degree of chaos and social risk in a patient’s life.10 Therefore it is possible that hospitals are being held accountable and potentially penalized for factors that are beyond a hospitals control (e.g. social isolation, substance abuse). Patients that are socially disadvantage may require more investment in targeted interventions such as supported discharge transitions, care coordination, health coaching, home visits, same day appointments, and greater education efforts. Hospitals that care for disadvantaged populations may need more resources to support disadvantaged populations not less. In other words, current readmission models, which are based on age, gender and co-morbid conditions, might penalize hospitals, that serve a high-risk, disadvantaged population that need more supportive services in care transitions. Though Medicare administrative data are limited in the types of information collected, it captures home zip code; this can help delineate the average SES of a community. In this study we examined whether adjustment for the average SES of a community in NYC, where neighborhoods diverge considerably in terms of resources and wealth, could have an impact on hospital profiling.
Methods
Data Sources
We extracted data from the 2005-2008 Medicare Inpatient Files that included complete information on heart failure hospitalizations for Medicare fee-for-service enrollees. We also accessed the 2005-2008 Beneficiary Annual Summary Files that provided data on chronic conditions, date of death, beneficiary residency zip code, and number of months of enrollment in a health maintenance organization.
Study Population
The study population included Medicare fee-for-service patients aged 65 years and older hospitalized with a primary discharge diagnosis of CHF between December 1, 2006, and December 1, 2009. We identified index hospitalizations for patients with heart failure according to the CMS inclusion criteria used to calculate a CHF readmission measure and included patients with any of the following International Classification of Diseases, Ninth Revision codes as a primary diagnose: 402.01, 402.11, 402.91, 402.01, 404.03, 404.11, 404.13, 404.91, 404.93, 428.0, 428.1, 428.2, 428.21, 428.22, 428.23, 428.3, 428.31, 428.32, 428.33, 428.4, 428.41, 428.42, 428.43, 428.9.4
We excluded patients less than 65 years old, those who died in the hospital, left against medical advice, and those with incomplete data.4 In addition, we limited our hospital-level analysis to acute or critical care hospitals and, similar to methods outlined by CMS, excluded all rehabilitation, psychiatric, and chronic care facilities.4
Main Outcome variable
Our dependent variable was 30-day hospital all-cause readmission following index admission for CHF. We used the established CMS methodology in identifying 30-day readmissions.6
Independent variables
The CMS CHF readmission model uses age, gender, and comorbid conditions to estimate the RSRR. To test our hypothesis that SES would affect hospital profiles, we added to the RSRR model a proxy measure for SES-- the Agency for Healthcare Research and Quality (AHRQ) SES index. AHRQ developed the SES index specifically for use with Medicare data because Medicare files lack person-level SES data. The index is based on the beneficiary’s ZIP code of residence and includes the following seven Census variables: percentage of persons in the labor force who are unemployed; percentage of persons living below poverty level; median household income; median value of owner-occupied dwellings; percentage of persons 25 years of age or older with less than a 12th grade education; the percentage of persons 25 years of age or older completing four or more years of college; and the percentage of households that average one or more persons per room.13-15 ENREF 16 Higher index scores indicate higher SES. Our calculations of the AHRQ SES index were based on 2006-2010 American Community Survey data because this database contained the needed SES variables and were done on the census block group level. We used a 9-digit zip codes; the linkage between US Postal service ZIP codes and census block data was performed using Maponics commercial cross walk file. (Maponics, LLC, 15 Railroad Row, White River Junction, VT 05001)
Data on date of death were extracted from the Beneficiary Annual Summary File. In our analysis we used the complete set of chronic conditions defined by CMS for readmission rate assessment after index hospitalization with heart failure.16
Statistical Analysis
We examined whether inclusion of a measure of SES in the 30-day CHF RSRR models influenced hospital-level profiling in New York City. Because of the natural clustering of observations within hospitals, we used hierarchical generalized linear models to estimate the log odds of 30-day readmission. We built 2 models of readmission in sequence: (1) the first (base) model included baseline patient age, gender, comorbidities, and hospital; (2) the second model included the baseline characteristics plus the AHRQ SES index. The baseline model was a CMS-like model that modeled the log-odds of readmission within 30 days of discharge from an index CHF admission as a function of age, gender, clinical characteristics, and a random hospital-specific intercept.6 The incremental discriminative performance of the models was assessed using the C statistic.
Next we calculated hospital 30-day RSRRs. These rates were obtained as the ratio of predicted to expected readmissions, multiplied by the NYC mean unadjusted readmission rate. The expected number of readmissions in each hospital was estimated using its patient mix and the average hospital-specific intercept.4 The profiling of hospitals was based on the CMS methodology and compared the hospital RSRR value (with confidence interval obtained using a bootstrapping procedure) and the overall average readmission rate calculated for all NYC hospitals.4 Hospitals with 30-day readmission rates and associated 95% confidence intervals above average were deemed “worse than expected” and those with 30-day readmission rates below average were considered “better than expected.”
In a secondary analysis, we examined the impact of the AHRQ SES index on the profiling of minority serving hospitals (defined in the literature as top 10% of hospitals with the highest proportion of black patients).17 ENREF 20 Out of 479 minority-serving hospitals across the country, 21 are located in New York City.
All confidence intervals were computed at the 95% level. Analyses were conducted using SAS statistical software (SAS Institute Inc., Version 9.2, Cary, NC). IRB approval was obtained, according to the Circulation: Cardiovascular Quality and Outcomes guidelines.
Results
Study Population
The sample included 48 New York City hospitals and 17,767 patients who had 25,962 hospitalizations between 2006 and 2009. The majority of patients were female. The most frequent conditions for hospitalizations were coronary atherosclerosis or angina, CHF, and renal failure (Table 1).
TABLE 1.
Characteristics of Patients Admitted to New York City Hospitals
| Variable | All Hospitals |
Minority Serving Hospitals |
Non- Minority serving Hospitals |
P |
|---|---|---|---|---|
| Number of Hospitals | 48 | 21 | 27 | - |
| Number of Patients | 17767 | 3737 | 14517 | - |
| Admissions with Heart Failure | 25962 | 5376 | 20586 | - |
| Crude readmission rate | 30.15% | 32.98% | 29.41% | <0.001 |
| Age, mean (SD) | 81.29(8.28) | 79.53(8.31) | 81.75(8.21) | <0.001 |
| Male | 38.95% | 34.11% | 40.21% | <0.001 |
| Black | 23.12% | 54.22% | 15.00% | <0.001 |
| Hispanic | 8.07% | 10.23% | 7.51% | <0.001 |
| History of CABG | 14.09% | 12.20% | 14.58% | <0.001 |
| History of PCI | 10.78% | 10.70% | 10.81% | 0.81 |
| Cardio-respiratory failure or shock | 10.80% | 11.01% | 10.75% | 0.57 |
| Congestive heart failure | 57.02% | 59.43% | 56.39% | <0.001 |
| Acute coronary syndrome | 14.94% | 17.30% | 14.32% | <0.001 |
| Coronary atherosclerosis or angina | 66.19% | 62.50% | 67.15% | <0.001 |
| Valvular or rheumatic heart disease | 8.53% | 5.67% | 9.27% | <0.001 |
| Specified arrhythmias | 39.45% | 35.94% | 40.37% | <0.001 |
| Other on unspecified heart disease | 3.09% | 3.57% | 2.97% | 0.03 |
| Vascular or circulatory disease | 17.73% | 17.93% | 17.68% | 0.66 |
| Metastatic cancer or acute leukemia | 1.54% | 1.26% | 1.61% | 0.07 |
| Cancer | 8.40% | 7.51% | 8.63% | 0.01 |
| Diabetes or DM complications | 46.29% | 53.07% | 44.53% | <0.001 |
| Protein-calorie malnutrition | 4.44% | 3.44% | 4.71% | <0.001 |
| Disorders of fluid, electrolyte, acid-base | 29.81% | 31.36% | 29.41% | 0.005 |
| Liver or biliary disease | 4.80% | 6.03% | 4.48% | <0.001 |
| Peptic ulcer, hemorrhage, other gastrointestinal disorders |
10.44% | 11.20% | 10.24% | 0.04 |
| Other gastrointestinal disorders | 26.79% | 29.71% | 26.03% | <0.001 |
| Severe hematological disorders | 2.02% | 1.75% | 2.09% | 0.11 |
| Anemias and blood disease | 33.34% | 37.70% | 32.20% | <0.001 |
| Dementia or other specified brain disorders | 14.90% | 15.90% | 14.64% | 0.02 |
| Drug and alcohol abuse/ dependence | 4.62% | 6.88% | 4.03% | <0.001 |
| Major psychiatric disorders | 2.99% | 3.76% | 2.78% | 0.0006 |
| Depression | 9.09% | 7.96% | 9.39% | 0.001 |
| Other psychiatric disorders | 3.94% | 3.52% | 4.06% | 0.06 |
| Hemiplegia, paraplegia, paralysis | 5.21% | 7.46% | 4.62% | <0.001 |
| Stroke | 2.74% | 3.11% | 2.64% | 0.06 |
| Chronic obstructive pulmonary disease | 33.25% | 34.32% | 32.97% | 0.06 |
| Fibrosis of lung or other chronic lung disorders | 3.15% | 3.13% | 3.16% | 0.89 |
| Asthma | 9.15% | 13.67% | 7.97% | <0.001 |
| Pneumonia | 28.18% | 28.11% | 28.20% | 0.89 |
| End stage renal disease or dialysis | 3.47% | 5.23% | 3.01% | <0.001 |
| Renal failure | 33.51% | 36.07% | 32.84% | <0.001 |
| Nephritis | 2.06% | 2.34% | 1.99% | 0.11 |
| Other urinary tract disorders | 8.89% | 9.15% | 8.82% | 0.44 |
| Decubitus ulcer or chronic skin ulcer | 9.42% | 9.51% | 9.39% | 0.81 |
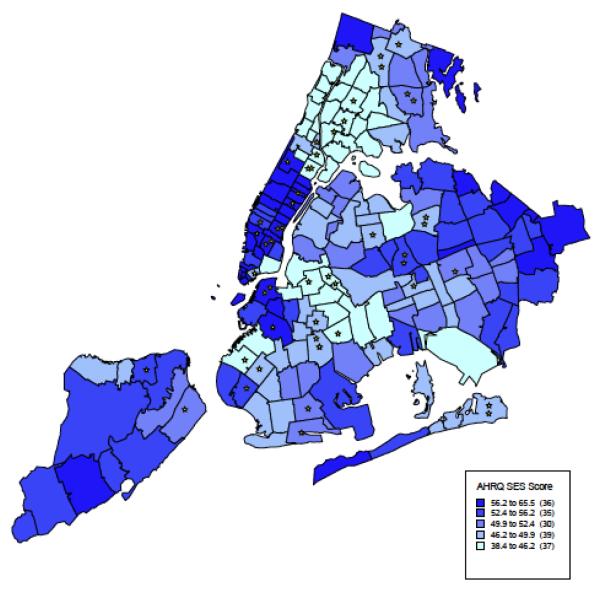
The median patient-level AHRQ SES index was 55, with a range of 33 to 76 (lower quartile 52, median 55, upper quartile 58). Figure 1 shows the mean SES Index scores in all ZIP Code areas of metropolitan New York City. The South Bronx neighborhood had the lowest SES score and the Upper East Side neighborhood in Manhattan had the highest. St. Barnabas Hospital in central Bronx served the population with the lowest average AHRQ SES score (47.3) and Lenox Hill Hospital on the Upper East Side had the patient population with the highest average score (59.9).
Figure 1.
New York City Distribution of the AHRQ SES index by ZIP code.
* = New York City Hospitals
The median observed 30-day readmission rate in New York City hospitals was 30.3% (Interquartile range, 28.6% −31.6%). Twenty-one of the 48 New York City hospitals were classified as minority-serving (Table 1). In the minority-serving hospitals of New York City, the proportion of heart failure admissions by black patients ranged between 30.95% and 95.88% (lower quartile 40.66%, median 52.78%, upper quartile 77.32%).
Impact of SES on 30-day readmission
After accounting for age, gender and comorbid conditions, the AHRQ SES Index was significantly associated with 30-day readmission risk (Table 2). Individuals with higher SES Index scores were less likely to experience a 30-day hospital readmission (estimate=−0.0057, p<0.019, or odds ratio= 0.99 with 95% CI 0.9968 and 0.9996). In other words, an increase of the SES score by 1 unit decreased the odds of readmission by 0.6% (an increase by 5 units decreased the odds by 2.6%). Adjustment for the AHRQ SES score had no appreciable effect on the C statistic (0.6347 adjusted to 0.6353). The following comorbid conditions which were covariates in the model had the strongest association with 30-day readmission after adjusting for other variables: history of end stage renal disease on dialysis 1.34 (95% CI 1.16-1.55); other psychiatric disorders 1.31 (95% CI 1.14-1.49); and decubitus or chronic skin ulcer 1.28 (95% CI 1.17-1.41).
TABLE 2.
Impact of AHRQ Index on 30-day CHF Readmissions
| Variable | Estimate | Standard Error |
P-Value | OR (95% CI) |
|---|---|---|---|---|
| Age (per 1 year) | 0.0000 | 0.0019 | 0.99 | 1.00(1.00,1.00) |
| Male | 0.0403 | 0.0303 | 0.18 | 1.04(0.98,1.10) |
| AHRQ SES score (per 1 unit) | −0.0057 | 0.0024 | 0.019 | 0.99(0.99,0.99) |
| History of CABG | 0.0600 | 0.0411 | 0.14 | 1.06(0.98,1.15) |
| Cardio-respiratory failure or shock | 0.1112 | 0.0454 | 0.014 | 1.12(1.02,1.22) |
| Congestive heart failure | 0.1396 | 0.0370 | 0.0002 | 1.15(1.07,1.24) |
| Acute coronary syndrome | 0.0457 | 0.0400 | 0.25 | 1.05(0.97,1.13) |
| Coronary atherosclerosis or angina | 0.0646 | 0.0329 | 0.05 | 1.07(1.00,1.14) |
| Valvular or rheumatic heart disease | 0.1576 | 0.0493 | 0.001 | 1.17(1.06,1.29) |
| Specified arrhythmias | 0.0702 | 0.0321 | 0.029 | 1.07(1.01,1.14) |
| Other on unspecified heart disease | 0.1182 | 0.0781 | 0.13 | 1.13(0.97,1.31) |
| Vascular or circulatory disease | 0.1547 | 0.0373 | <0.001 | 1.17(1.09,1.26) |
| Metastatic cancer or acute leukemia | 0.0208 | 0.1149 | 0.86 | 1.02(0.82,1.28) |
| Cancer | 0.1064 | 0.0514 | 0.039 | 1.11(1.01,1.23) |
| Diabetes or DM complications | 0.0645 | 0.0300 | 0.033 | 1.07(1.01,1.13) |
| Protein-calorie malnutrition | 0.2957 | 0.0648 | <0.0001 | 1.34(1.18,1.53) |
| Disorders of fluid, electrolyte, acid-base | 0.1773 | 0.0337 | <0.0001 | 1.19(1.12,1.28) |
| Liver or biliary disease | 0.0915 | 0.0630 | 0.15 | 1.10(0.97,1.24) |
| Other gastrointestinal disorders | 0.1757 | 0.0456 | 0.0001 | 1.19(1.09,1.30) |
| Gastrointestinal disorders | 0.0258 | 0.0327 | 0.43 | 1.03(0.96,1.09) |
| Severe hematological disorders | 0.2324 | 0.0938 | 0.013 | 1.26(1.05,1.52) |
| Anemias and blood disease | 0.1513 | 0.0313 | <0.001 | 1.16(1.09,1.24) |
| Dementia or other specified brain disorders | 0.1472 | 0.0399 | 0.0002 | 1.16(1.07,1.25) |
| Drug/alcohol abuse/ dependence | 0.0441 | 0.0659 | 0.5 | 1.05(0.92,1.19) |
| Major psychiatric disorders | 0.0958 | 0.0800 | 0.23 | 1.10(0.94,1.29) |
| Depression | −0.0108 | 0.0487 | 0.83 | 0.99(0.90,1.09) |
| Other psychiatric disorders | 0.2671 | 0.0687 | 0.0001 | 1.31(1.14,1.49) |
| Hemiplegia, paraplegia, paralysis | −0.0407 | 0.0630 | 0.52 | 0.96(0.85,1.09) |
| Stroke | 0.0271 | 0.0847 | 0.75 | 1.03(0.87,1.21) |
| Chronic obstructive pulmonary disease | 0.1493 | 0.0309 | <0.0001 | 1.16(1.09,1.23) |
| Fibrosis of lung or other chronic lung disorders |
0.0850 | 0.0771 | 0.27 | 1.09(0.94,1.27) |
| Asthma | 0.1299 | 0.0478 | 0.007 | 1.14(1.04,1.25) |
| Pneumonia | 0.1571 | 0.0323 | <0.0001 | 1.17(1.10,1.25) |
| End stage renal disease or dialysis | 0.2904 | 0.0739 | 0.0001 | 1.34(1.16,1.55) |
| Renal failure | 0.1663 | 0.0346 | <0.0001 | 1.18(1.10,1.26) |
| Nephritis | 0.0586 | 0.0937 | 0.53 | 1.06(0.88,1.27) |
| Other urinary tract disorders | 0.0975 | 0.0478 | 0.041 | 1.10(1.00,1.21) |
| Decubitus ulcer or chronic skin ulcer | 0.2477 | 0.0473 | <0.0001 | 1.28(1.17,1.41) |
Changes in Hospital Profiling After Inclusion of the AHRQ SES Index
The mean hospital-level AHRQ Index score was 54.6. The median and inter-quartile range (IQR) for the RSRR estimated based on the CMS model was 30.3 (28.6- 31.6)] and similar to the model which included the AHRQ SES Index 30.2 (28.5, 31.6). The agreement between the RSRR from the two models was very high (kappa=0.88). After adjustment for the SES index, the quality rating changed for one hospital, from worse than average to average. The ratings of no other hospitals change with adjustment for the SES index score.
In the secondary analysis of minority-serving hospitals, the median RSRR and IQR was 30.7 (29.8, 31.7) in minority serving hospitals and 29.6 (28, 30.6) in non-minority serving hospitals (Table 3). Among minority serving hospitals, 19 out of 21 were categorized as “no different than NYC average” and 2 hospitals as “worse than NYC average”. After inclusion of SES index in the model, the RSRR and IQR were 30.6 (30.0, 31.6) in minority serving hospitals and 29.5 (28.1, 30.6) in non-minority serving hospitals (Table 3). One minority hospital improved their status from “worse than NYC average” to “no different than NYC average”. This was the same hospital that changed ranking in the primary analysis. Among the non-minority-serving hospitals, 24 were “no different than NYC average”, one hospital was “worse than NYC average”, and 2 were “better than NYC average.” No hospitals changed status after adjustment for the AHRQ SES Index score.
Table 3.
Hospital RSRRs with and without adjusting for the AHRQ SES Index
| Hospital Characteristics | All Hospitals | Minority Serving Hospitals |
Non-Minority Serving Hospital |
|---|---|---|---|
| No. Hospitals | 48 | 21 | 27 |
| Median (range) patients per hospital |
541(56, 2636) | 256(56, 897) | 762(57, 2636) |
| Mean AHRQ Index Score | 54.6 | 53.1 | 55.8 |
| Median and Range Hospital Mean AHRQ Index Score |
54.3(47.2, 60.7) | 52.8(47.5, 60.6) | 56.2(47.2, 60.7) |
| RSRR Based on CMS model | |||
| Median and (IQR, 25%, 75%) (%) |
30.3(28.6, 31.6) | 30.7(29.8, 31.7) | 29.6(28.0, 30.6) |
| Range (min-max) (%) | 25.7-35.3 | 27.7-35.3 | 25.7-33.4 |
|
RSRR with Inclusion of
AHRQ Index Score in CMS Model |
|||
| Median and (IQR, 25%, 75%) (%) |
30.2(28.5,31.6) | 30.6(30.0,31.6) | 29.5(28.1, 30.6) |
| Range (min-max) (%) | 25.8-35.2 | 27.8-35.2 | 25.8-33.3 |
Discussion
There is a large variation in wealth, education, and income in NYC neighborhoods. We examined whether inclusion of a measure of community SES, in NYC, in the 30-day CHF models impacted hospital-level profiling. The impact of the community-level measure of SES on 30-day CHF readmission models was small. As such, even in NYC where differences in SES status are stark, inclusion of this measure had minimal impact on hospital-level RSRRs.
The lack of impact of SES on RSRR could be because community level SES, represented by the AHRQ SES Index, was an inadequate indicator for individual patient-level socioeconomic and social risk. Better measures may be needed to assess the impact of socioeconomic factors on hospital profiling based on 30-day readmission. Recent research has demonstrated that social risk factors such as cocaine use, missed clinic visits, multiple address changes, and excessive emergency department use is associated with higher risk of 30-day readmission.10 These factors are more prevalent in low SES populations, but are also not available in Medicare administrative data and not available for hospital profiling.
The importance of including data on socioeconomic and social risk factors in assessing health care outcomes was highlighted by an editorial featured by the Centers for Disease Control. 18 The editorial lamented the inadequacy of current data systems to examine health outcomes because they “do not include economic and social factors that influence the health of individuals and communities as a whole.” Hospitals that serve the poor may require more resources because vulnerable patients have higher admission rates and longer hospital admissions. 19, 20 ENREF 26 In other countries, for example, hospitals that cater to the poor are given more, not less, resources. In England’s National Health Service system, until 2004, primary care general practitioner payments were partially based on the poverty of their patient population, as measured by percent unemployment.21 ENREF 28 In the United States, hospitals that cared for the uninsured poor had been given increased resources through disproportionate share hospital payments but with the number of uninsured to be greatly reduced, starting in 2014, the Affordable Care Act allows CMS to phase out these supplemental payments. CMS’s new readmission penalization policy, and CMS’s Hospital Value-Based Purchasing program, may further diminish resources to hospitals that serve poor vulnerable patients.22 As evidenced by emerging data from the Value-Based Purchasing Program, some hospitals with significant resources have been able to move from a CMS penalty to bonus while some resource poor hospitals have been penalized.22 More research to fully explore the impact of CMS’s new policies on hospital profiling is clearly needed.
Our study has several key strengths and limitations that deserve comment. This study focused on hospitals in New York City which limits the generalizability of the findings. We chose New York City because of the vast differences in health and socioeconomic status between different neighborhoods. For example, East Harlem is the poorest neighborhood in Manhattan (median income in 1999 was $22,000) and is immediately adjacent to the Upper East Side, which is the wealthiest (median income in 1999 was $77,000).23 ENREF 22 East Harlem has the city’s highest rates of obesity and diabetes, and the Upper East Side has the lowest rates.24 Even though the local nature of this study limits its generalizability; as we did not see an impact of SES represented by ZIP code on hospital profiling in New York City, it is doubtful, that SES would impact hospital profiling in areas with a less extreme gradient in wealth and health. In addition, we used a validated measure of SES designed for Medicare25 and used ZIP code as a proxy for neighborhood because this was a practical and readily available demographic variable available for all Medicare patients. However the use ZIP code level data may be an inadequate measure of SES status. Past research has demonstrated the socioeconomic and social risk factors are associated with 30- readmission in a largely uninsured population. ENREF 1010 Future research should examine the link between SES and 30-day readmission in the Medicare program. Finally, we followed the publicly available CMS methodology with a limitation. We had access to the Inpatient and Beneficiary Annual Summary Files (BASF) and could correctly identify index hospitalizations and readmissions. We used hierarchical models for prediction of 30-day readmissions and bootstrapping technique for estimation of 95% CL. We also categorized the comorbidities using CMS’ list for CHF patients. However, we did not have access to the outpatient hospital and Part B physician data. Comorbidities in the BASF file were developed by CMS using both Part A and Part B data. Therefore it is possible that we underestimated the prevalence of comorbid conditions among patients. However, we performed sensitivity analysis using comorbid conditions available in the Medicare BASF file and obtained a similar result.
In conclusion, we found that the measure of SES available in Medicare did not appreciably impact risk of readmission or RSRR for hospitals in NYC. Community level SES, represented by the AHRQ SES Index may be an inadequate indicator for individual patient-level socioeconomic and social risk. More research examining the impact of SES on 30-day CHF readmission is needed to determine the link between SES and hospital readmissions in the Medicare program.
Supplementary Material
Acknowledgments
Funding Sources: This project was not directly supported by any external grants or funds. Dr. Blum was supported through a National Research Service Award from the Health Resources & Administration at Mount Sinai School of Medicine (T32HP10262). Dr. Keyhani was supported by a VA HSR&D Career Development Award and an NHLBI R01HL116522-01A1.
Abbreviations
- CHF
Congestive Heart Failure
- ACA
Patient Protection Affordable Care Act
- RSRR
risk standardized readmission rate
- NYC
New York City
Footnotes
Disclosures: None
REFERENCES
- 1.Schocken DD, Arrieta MI, Leaverton PE, Ross EA. Prevalence and mortality rate of congestive heart failure in the united states. J Am Coll Cardiol. 1992;20:301–306. doi: 10.1016/0735-1097(92)90094-4. [DOI] [PubMed] [Google Scholar]
- 2.Ho KK, Anderson KM, Kannel WB, Grossman W, Levy D. Survival after the onset of congestive heart failure in framingham heart study subjects. Circulation. 1993;88:107–115. doi: 10.1161/01.cir.88.1.107. [DOI] [PubMed] [Google Scholar]
- 3.Report to congress: Promoting greater efficiency in medicare. 2007;2010 [Google Scholar]
- 4.Krumholz H, Normand S-L, Keenan P, Lin Z, Drye E, Bhat K, Wang Y, Ross J, Schuur J, Stauffer B, Bernheim S, Epstein A, Herrin J, Federer J, Mattera J, Wang Y, Mulvey G, Schreiner G. Hospital 30-day heart failure readmission measure methodology. 2008.
- 5.Halasyamani LK, Davis MM. Conflicting measures of hospital quality: Ratings from “hospital compare” versus “best hospitals”. Journal of hospital medicine : an official publication of the Society of Hospital Medicine. 2007;2:128–134. doi: 10.1002/jhm.176. [DOI] [PubMed] [Google Scholar]
- 6.Federal Register Medicare program; proposed changes to the hospital inpatient prospective payment systems for acute care hospitals and the long-term care hospital prospective payment system and fiscal year 2012 rates; proposed rule. 2011;Vol. 76(No. 87) [Google Scholar]
- 7.Rau J. Medicare revises hospitals’ readmissions penalties. Kaiser Health News. 2012 [Google Scholar]
- 8.Federal Register Fy12 hospital readmissions reduction program. 2011;160:51660–51676. [Google Scholar]
- 9.Marmot M. Social determinants of health inequalities. Lancet. 2005;365:1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 10.Amarasingham R, Moore BJ, Tabak YP, Drazner MH, Clark CA, Zhang S, Reed WG, Swanson TS, Ma Y, Halm EA. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Med Care. 2010;48:981–988. doi: 10.1097/MLR.0b013e3181ef60d9. [DOI] [PubMed] [Google Scholar]
- 11.Muennig P, Franks P, Jia H, Lubetkin E, Gold MR. The income-associated burden of disease in the united states. Social science & medicine. 2005;61:2018–2026. doi: 10.1016/j.socscimed.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Hygiene NYCDoHaM Health disparities in new york city. 2010.
- 13.Bonito AJBC, Eicheldinger C, Carpenter L. Creation of new race-ethnicity codes and socioeconomic status (ses) indicators for medicare beneficiaries. 2008.
- 14.Lentine KL, Schnitzler MA, Xiao H, Saab G, Salvalaggio PR, Axelrod D, Davis CL, Abbott KC, Brennan DC. Racial variation in medical outcomes among living kidney donors. The New England journal of medicine. 2010;363:724–732. doi: 10.1056/NEJMoa1000950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moy E, Greenberg LG, Borsky AE. Community variation: Disparities in health care quality between asian and white medicare beneficiaries. Health affairs. 2008;27:538–549. doi: 10.1377/hlthaff.27.2.538. [DOI] [PubMed] [Google Scholar]
- 16.Qualitynet.org Heart failure icd 9 to chronic conditions. 2012;2013 [Google Scholar]
- 17.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for medicare beneficiaries by race and site of care. JAMA : the journal of the American Medical Association. 2011;305:675–681. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harrison K, Dean H. Use of data systems to address social determinants of health: A need to do more. 2011;126 doi: 10.1177/00333549111260S301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Epstein AM, Stern RS, Weissman JS. Do the poor cost more? A multihospital study of patients’ socioeconomic status and use of hospital resources. The New England journal of medicine. 1990;322:1122–1128. doi: 10.1056/NEJM199004193221606. [DOI] [PubMed] [Google Scholar]
- 20.Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in new york city. Health affairs. 1993;12:162–173. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- 21.Goddard M, Gravelle H, Hole A, Marini G. Where did all the gps go? Increasing supply and geographical equity in england and scotland. Journal of health services research & policy. 2010;15:28–35. doi: 10.1258/jhsrp.2009.009003. [DOI] [PubMed] [Google Scholar]
- 22.Rau J. Nearly 1,500 hospitals penalized under medicare program rating quality. Kaiser Health News. 2013 [Google Scholar]
- 23.FactFinder A Income charecteristics. 2000.
- 24.Karpati ALX, Mostashari F, et al. The health of east harlem. Nyc commun health profiles. 2003:1–12. [Google Scholar]
- 25.Quality AfHRa Creation of new race-ethnicity codes and socioeconomic status (ses) indicators for medicare beneficiaries: Final report. 2008. AHRQ publication no. 08-0029.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.