Abstract
The aim of this paper is to review the current literature on allergy in orthodontics and to identify the predisposing factors and the implications of the allergic reaction in the management of patients during orthodontic treatment. A computerized literature search was conducted in PubMed for articles published on allergy in relation to orthodontics. The MeSH term used was allergy and orthodontics. Allergic response to alloys in orthodontics, particularly nickel, has been extensively studied and several case reports of nickel-induced contact dermatitis have been documented. Current evidence suggests that the most common allergic reaction reported in orthodontics is related to nickel in orthodontic appliances and allergic response is more common in women due to a previous sensitizing exposure from nickel in jewellery. Studies have implicated allergy in the etiology of hypo-dontia. It has also been considered as a high-risk factor for development of extensive root resorption during the course of orthodontic treatment. This review discusses the relationship and implications of allergy in orthodontics.
Keywords: Allergy, nickel, orthodontics
INTRODUCTION
Allergic reactions are of increasing concern to practitioners in health-related fields. As patient susceptibility increases, the need for basic understanding and successful management of these conditions are of primary importance. An allergic response is one in which certain components of the immune system react excessively to a foreign substance. Allergy in patients undergoing orthodontic treatment can be seen due to several reasons and these include nickel allergy, allergy to the acrylic resins that are used during treatment, latex products, etc.[1] A large variety of metallic alloys are routinely used in dentistry. Allergy as a possible factor has also been implicated in root resorption and hypo-dontia.
Gold was used in orthodontics for fabrication of accessories until the 1930s and 1940s. In 1929, stainless steel was used for the first time to replace gold. Several metallic alloys are used in orthodontics, such as cobalt-chromium, nickel-titanium, β-titanium, among others; the majority of these alloys have nickel as one of their components. The percentage of this metal in the alloys varies from 8%, as in stainless steel, up to more than 50%, as in nickel-titanium alloys. The aim of this paper is to review and analyze critically the current available literature in the field of allergy in orthodontics and to provide clinical implications based on scientific evidence on the topic.
SEARCH STRATEGY
A search was conducted on PubMed to retrieve all available literature on allergy and orthodontics. The search revealed a total of 114 articles on the topic. A total of 106 articles were retrieved in nickel allergy and orthodontics. Of these, 14 articles were reviews on nickel allergy and 92 were case reports. Four reviews were in languages other than English. These articles were eliminated and 10 articles were studied. Five articles were in relation to allergy and root resorption, and three were in relation to allergy and hypo-dontia.
NICKEL ALLERGY IN ORTHODONTICS
Nickel is a powerful sensitizer metal and a common allergen. Dermatitis due to contact with nickel was first reported among workers in the nickel plating industry and was recognized as an allergic response in 1925.[2,3] Nickel has often been pointed out as a biological sensitizer capable of causing short- and long-term sensitivity reactions. An increased risk of nickle sensitization in potential orthodontic patients could possibly be due to wearing Ni-containing jewellery at an early age.[4]
SALIVARY NICKEL RELEASE FROM FIXED APPLIANCES
Park and Shearer[5] reported an average release of 40 μg of nickel and 36 μg of chromium from a simulated orthodontic appliance. The release of nickel is not necessarily related to the alloy's nickel content.[6] The amount of nickel release can increase during stress. The quantities released may be negligible from a toxicological point of view, but might conceivably be of significance for patients with a high degree of hypersensitivity to nickel. Fors and Persson[7] found significantly higher content of nickel in the plaque and saliva of patients with orthodontic appliances compared with non-orthodontic patients. Moreover, in orthodontic patients, significantly higher nickel content was found in plaque from metal surfaces (band and brackets) than from enamel surfaces.
BIOLOGY OF NICKEL ALLERGY
Elicitation of an allergic reaction to nickel depends on the conditions of nickel exposure—for example, hapten concentration on the contact area, open or occluded exposure, presence of an irritant, and degree of contact allergy. The elicitation threshold varies between patients and also individually over time.[8,9] Nickel elicits contact dermatitis, which is a type-IV delayed hypersensitivity immune response. This process has two interrelated, distinct phases:[10] A sensitization phase occurs from the moment the allergen enters the body, is recognized, and a response occurs. The elicitation phase occurs after re-exposure to the allergen to appearance of the full clinical reaction. There may have been no symptoms at the initial exposure, but subsequent exposure leads to a more visible reaction.[11]
CLINICAL FEATURES ASSOCIATED WITH ALLERGY
Clinical abnormalities, such as gingivitis, gingival hyperplasia, lip desquamation, multiform erythema, burning sensation in the mouth, metallic taste, angular cheilitis, and periodontitis, may be associated with release of nickel from orthodontic appliances.[12,13,14,15,16] These reactions are associated with an inflammatory response induced by corrosion of orthodontic appliances and subsequent release of nickel. It is manifested as Nickel Allergic Contact Stomatitis (NiACS). A burning sensation is the most frequent symptom. The aspect of the affected mucosa is also variable, from slight erythema to shiny lesions, with or without edema. Vesicles are rarely observed, but when they are present, they quickly rupture, forming erosion areas. In chronic cases, the affected mucosa is typically in contact with the causal agent and appears erythematous or hyper-keratotic to ulcerated.[17] Other symptoms can also be present, such as peri-oral dermatitis and, rarely, orolingual paresthesia.
PREVALENCE OF NICKEL ALLERGY
The incidence of Ni-induced side effects from orthodontic materials in non-sensitized people is not known. It has also been suggested that the risk of sensitization from orthodontically derived Ni in these patients is extremely low. Nickel allergy is the most common contact allergy in industrialized countries; patch test verified data of general populations in several studies have shown that this allergy affects 10%-30% of females and 1-3% of males.[18,19,20,21,22] Two recent surveys from Europe estimated incidence of adverse patient reactions in orthodontic practice to be approximately 0.3%-0.4%.[23,24] Kerosuo et al.[25] found prevalence of nickel allergy in Finnish adolescents to be 30% in girls and 3% in boys. This is thought to be due to ear piercing being a major cause of sensitization to nickel, as prevalence in subjects with pierced ears was 31% and those without pierced ears was 2%.[25]
People with cutaneous piercing were considered a significant risk factor for Ni allergy.[26] Scientific evidence suggests that orthodontic treatment is not associated with increase of Ni hypersensitivity, unless patients have a history of previous cutaneous piercing exposure to Ni, usually ear piercing. Previous allergic history has been significantly associated by several authors to a hypersensitivity response to nickel released from orthodontic appliances.
NICKEL ALLERGY AND PERIODONTAL STATUS
Placement of orthodontic brackets influences the accumulation of biofilm and colonization of bacteria, thereby making a patient more prone to inflammation and bleeding.[27] Pazzini et al. found that nickel can influence inflammatory reactions throughout orthodontic treatment. Such reactions are characterized by gingival hyperplasia, changes in color and gingival bleeding upon probing. More than a direct sensitizing agent of skin and mucosa, nickel appears to alter the periodontal status, acting as a modifying factor of periodontal disease in sensitive patients. Results suggest a cumulative effect of nickel throughout orthodontic treatment and that this effect is associated with clinically significant periodontal abnormalities.[28]
Gursoy et al.[29] in 2007 found that low-dose continuing nickel release from orthodontic appliances might be the initiating factor for gingival overgrowth, as it has the capability of increasing epithelial cell proliferation. Pazzini et al. in 2011 found that patients treated with conventional braces exhibited greater periodontal alterations than those treated with nickel-free braces. Individuals with an allergy to nickel exhibit better periodontal health when treated with nickel-free braces than with conventional braces.[30] Pazzini et al.[31] found that nickel can influence the condition of the periodontal and blood cells of allergic orthodontic patients, but with reactions of an inflammatory, rather than allergic nature.
DIAGNOSIS
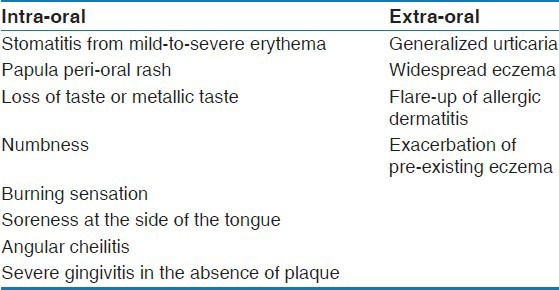
Sensitivity to nickel has been evaluated through biocompatibility tests,[32] including cutaneous sensitivity (patch) tests,[33] and reactivity to nickel has been evaluated with in vitro cell proliferation assays.[34] It is important to make correct diagnosis of nickel allergy, symptoms of which may occur either within or remote to the oral environment. The signs and symptoms of nickel allergy are presented in Table 1. The following patient history would suggest a diagnosis of nickel allergy.[11]
Table 1.
Signs and symptoms of nickel allergy[11]
Previous allergic response after wearing earrings or a metal watchstrap;
Appearance of allergy symptoms shortly after initial insertion of orthodontic components containing nickel;
Confined extra-oral rash adjacent to headgear studs.
A dermatologist should confirm the diagnosis by patch testing using 5% nickel sulfate in petroleum jelly.
MANAGEMENT OF NICKEL ALLERGY
The majority of investigations have found that nickel-sensitive patients are able to tolerate stainless steel without any noticeable reaction.[35] Most research concludes that stainless steel is a safe material to use for all intra-oral orthodontic components for nickel-sensitive patients.
Alternatives to Nickel-Titanium Wires
Alternatives to Ni-Ti include twistflex stainless steel and fiber-reinforced composite archwires. Wires such as TMA, pure titanium, and gold-plated wires may also be used without risk. Altered nickel-titanium archwires also exist and include plastic/resin-coated nickel-titanium archwires.[36] Ion-implanted nickel-titanium archwires have their surface bombarded with nitrogen ions, which forms an amorphous surface layer, conferring corrosion resistance and displacing nickel atoms, and decreasing the risk of an allergic response.
Brackets
Stainless steel brackets are generally considered safe. However, nickel-free alternative brackets to stainless steel include:
Ceramic brackets produced using polycrystalline alumina, single-crystal sapphire, and zirconia;
Polycarbonate brackets that are produced from plastic polymers;
Titanium brackets;
Gold-plated brackets.
Extra-oral metal components, including metal studs in headgear, are of greatest concern due to greater sensitivity of skin. Plastic-coated headgear studs may be a better alternative for such patients.
ALLERGY AND ROOT RESORPTION
Root resorption is a common sequel to orthodontic treatment and has been recorded in 93% of treated adolescents.[37] Davidovitch et al.[38] hypothesized that individuals who have medical conditions that affect the immune system may be at a high level of risk for developing excessive root resorption during the course of orthodontic treatment. In reviewing orthodontic patient records at the University of Oklahoma, they discovered that the incidence of asthma, allergies and signs indicative of psychological stress were significantly higher in patients who had experienced excessive root resorption during orthodontic treatment as compared with the group of orthodontic patients who had completed their course of treatment without suffering this unfortunate outcome.
McNab et al.[39] reported that the incidence of external apical root resorption was elevated in patients with asthma. However, both asthmatics and healthy patients exhibited similar amounts of moderate and severe resorption. Nishioka et al.[40] found that allergy and asthma might be an etiological factor in excessive root resorption. The same association was found in earlier studies.[37,38,39,40,41] Owman-Moll and Kurol[41] also suggested that there might be a link between allergy and the extent of root resorption, but no statistically significant difference was found. Nishioka et al.[40] strongly supported the hypothesis that allergy and asthma may be high-risk factors for development of excessive root resorption during orthodontic treatment. They concluded that allergy, root morphology abnormalities and asthma may be considered high-risk factors for development of excessive root resorption during the course of orthodontic treatment in a Japanese population.
ALLERGY AND HYPODONTIA
Three articles were retrieved in the search and only one article dealt with allergy in relation to hypo-dontia. Third molars are the most commonly missing teeth followed by the second premolars and the maxillary lateral incisors.[42] The etiology of hypo-dontia is considered to be multifactorial, with genetics and environmental factors playing an important role.[43] Yamaguchi et al.[44] in 2008 studied 3683 Japanese orthodontic patients and found positive correlation between allergy and hypo-dontia. They concluded that health problems, especially those related to allergy, are of importance and could be strongly related to hypo-dontia.
CONCLUSION
Safe and effective practice depends on identifying patients with allergy along with knowledge of materials that can potentially cause them. It is imperative for a practitioner to not only know the physical and mechanical properties of the materials being used, but also of the biologic compatibility of the material. Knowledge of alternatives to allergy-causing materials is also of prime importance in efficient management of patients in routine clinical practice.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hensten-Pettersen A, Jacobsen N. Disintegration of orthodontic appliances in vivo. In: Eliades G, Eliades T, Brantley WA, Watts DC, editors. In Vivo Aging of Dental Biomaterials. Chicago: Quintessence; 2003. pp. 290–296. [Google Scholar]
- 2.Namikoshi T, Yoshimatsu T, Suga K, Fujii H, Yasuda K. The prevalence of sensitivity to constituents of dental alloys. J Oral Rehabil. 1990;17:377–81. doi: 10.1111/j.1365-2842.1990.tb00022.x. [DOI] [PubMed] [Google Scholar]
- 3.Counts AL, Miller MA, Khakhria ML, Strange S. Nickel allergy associated with a transpalatal arch appliance. J Orofac Orthop. 2002;63:509–15. doi: 10.1007/s00056-002-0128-z. [DOI] [PubMed] [Google Scholar]
- 4.McDonagh AJ, Wright AL, Cork MJ, Gawkrodger DJ. Nickel sensitivity: The influence of ear piercing and atopy. Br J Dermatol. 1992;126:16–8. doi: 10.1111/j.1365-2133.1992.tb08396.x. [DOI] [PubMed] [Google Scholar]
- 5.Park HY, Shearer TR. In vitro release of nickel and chromium from simulated orthodontic appliances. Am J Orthod. 1983;84:156–9. doi: 10.1016/0002-9416(83)90180-x. [DOI] [PubMed] [Google Scholar]
- 6.Grimsdottir MR, Gjerget NR, Hensten-Pettersen A. Composition and in vitro corrosion of orthodontic appliances. Am J Orthod Dentofac Orthop. 1992;101:525–32. doi: 10.1016/0889-5406(92)70127-V. [DOI] [PubMed] [Google Scholar]
- 7.Fors R, Persson M. Nickel in dental plaque and saliva in patients with and without orthodontic appliances. Eur J Orthod. 2006;28:292–7. doi: 10.1093/ejo/cji091. [DOI] [PubMed] [Google Scholar]
- 8.Fischer LA, Menne T, Johansen JD. Experimental nickel elicitation thresholds—a review focusing on occluded nickel exposure. Contact Dermatitis. 2005;52:57–64. doi: 10.1111/j.0105-1873.2005.00523.x. [DOI] [PubMed] [Google Scholar]
- 9.Emmett EA, Risby TH, Jiang L, Ng SK, Feinman S. Allergic contact dermatitis to nickel: Bioavailability from consumer products and provocation threshold. J Am Acad Dermatol. 1988;19:314–22. doi: 10.1016/s0190-9622(88)70178-4. [DOI] [PubMed] [Google Scholar]
- 10.van Loon LA, van Elsas PW, Bos JD, ten Harkel-Hagenaar HC, Krieg SR, Davidson CL. T-lymphocyte and Langerhans cell distribution in normal and allergically-induced oral mucosa in contact with nickel-containing dental alloys. J Oral Path. 1988;17:129–37. doi: 10.1111/j.1600-0714.1988.tb01899.x. [DOI] [PubMed] [Google Scholar]
- 11.Rahilly G, Price N. Nickel allergy and orthodontics. J Orthod. 2003;30:171–4. doi: 10.1093/ortho/30.2.171. [DOI] [PubMed] [Google Scholar]
- 12.Janson GR, Dainesi EA, Consolaro A, Woodside DG, Freitas MR. Nickel hypersensitivity reaction before, during, and after orthodontic therapy. Am J Orthod Dentofacial Orthop. 1998;113:655–60. doi: 10.1016/s0889-5406(98)70226-4. [DOI] [PubMed] [Google Scholar]
- 13.Lindsten R, Kurol J. Orthodontic appliances in relation to nickel hypersensitivity: A review. J Orofac Orthop. 1997;58:100–8. [PubMed] [Google Scholar]
- 14.Starkjaer L, Menné T. Nickel allergy and orthodontic treatment. Eur J Orthod. 1990;12:284–9. doi: 10.1093/ejo/12.3.284. [DOI] [PubMed] [Google Scholar]
- 15.Lamster IB, Kalfus DI, Steigerwald PJ, Chasens AI. Rapid loss of alveolar bone association with nonprecious alloy crowns in two patients with nickel hypersensitivity. J Periodontol. 1987;58:486–92. doi: 10.1902/jop.1987.58.7.486. [DOI] [PubMed] [Google Scholar]
- 16.Bishara SE, Barrett RD, Selim M. Biodegradation of orthodontic appliances. Part II. Changes in the blood level of nickel. Am J Orthod Dentofacial Orthop. 1993;103:115–9. doi: 10.1016/S0889-5406(05)81760-3. [DOI] [PubMed] [Google Scholar]
- 17.Genelhu MC, Marigo M, Alves-Oliveira LF, Malaquias LC, Gomez RS. Characterisation of nickel induced allergic contact stomatitis associated with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2005;128:378–81. doi: 10.1016/j.ajodo.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Smith-Sivertsen T, Dotterud LK, Lund E. Nickel allergy and its relationship with local nickel pollution, ear piercing, and atopic dermatitis: A population based study from Norway. J Am Acad Dermatol. 1999;40:726–35. doi: 10.1016/s0190-9622(99)70154-4. [DOI] [PubMed] [Google Scholar]
- 19.Mattila L, Kilpeläinen M, Terho EO, Koskenvuo M, Helenius H, Kalimo K. Prevalence of nickel allergy among Finnish university students in 1995. Contact Dermatitis. 2001;44:218–23. doi: 10.1034/j.1600-0536.2001.044004218.x. [DOI] [PubMed] [Google Scholar]
- 20.Schafer T, Bohler E, Ruhdorfer S, Weigl L, Wessner D, Filipiak B, et al. Epidemiology of contact allergy in adults. Allergy. 2001;56:1192–6. doi: 10.1034/j.1398-9995.2001.00086.x. [DOI] [PubMed] [Google Scholar]
- 21.Blanco-Dalmau L, Carrasquillo-Alberty H, Silva-parra J. A study of nickel allergy. J Prosth Dent. 1984;52:116–9. doi: 10.1016/0022-3913(84)90193-8. [DOI] [PubMed] [Google Scholar]
- 22.Janson GR, Dainesi EA, Pereira AC, Pinzan A. Clinical evaluation of nickel hypersensitivity reaction in patients under orthodontic treatment. Ortodontia. 1994;27:31–7. [Google Scholar]
- 23.Jacobsen N, Hensten-Pettersen A. Changes in occupational health problems and adverse patient reactions in orthodontics from 1987 to 2000. Eur J Orthod. 2003;25:591–8. doi: 10.1093/ejo/25.6.591. [DOI] [PubMed] [Google Scholar]
- 24.Schuster G, Reichle R, Bauer RR, Schopf PM. Allergies induced by orthodontic alloys: Incidence and impact on treatment. J Orofac Orthop. 2004;65:48–59. doi: 10.1007/s00056-004-0312-4. [DOI] [PubMed] [Google Scholar]
- 25.Kerosuo H, Kullaa A, Kerosuo E, Kanerva L, Hensten-Pettersen A. Nickel allergy in adolescents in relation to orthodontic treatment and piercing of ears. Am J Orthod Dentofac Orthop. 1996;109:148–54. doi: 10.1016/s0889-5406(96)70175-0. [DOI] [PubMed] [Google Scholar]
- 26.Thyssen JP, Linneberg A, Menne T, Johansen JD. The epidemiology of contact allergy in the general population—prevalence and main findings. Contact Dermatitis. 2007;57:287–99. doi: 10.1111/j.1600-0536.2007.01220.x. [DOI] [PubMed] [Google Scholar]
- 27.Naranjo AA, Trivino ML, Jaramillo A, Betancourth M, Botero JE. Changes in the subgingival microbiota and periodontal parameters before and 3 months after bracket placement. Am J Orthod Dentofacial Orthop. 2006;130:17–22. doi: 10.1016/j.ajodo.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 28.Pazzini CA, Junior GO, Marques LS, Pereira CV, Pereira LJ. Prevalence of nickel allergy and longitudinal evaluation of periodontal abnormalities in orthodontic allergic patients. Angle Orthod. 2009;79:922–7. doi: 10.2319/081408-430.1. [DOI] [PubMed] [Google Scholar]
- 29.Gursoy UK, Sokucu O, Uitto VJ, Aydin A, Demirer S, Toker H, et al. The role of nickel accumulation and epithelial cell proliferation in orthodontic treatment-induced gingival overgrowth. Eur J Orthod. 2007;29:555–8. doi: 10.1093/ejo/cjm074. [DOI] [PubMed] [Google Scholar]
- 30.Pazzini CA, Pereira LJ, Carlos RG, de Melo GE, Zampini MA, Marques LS. Nickel: Periodontal status and blood parameters in allergic orthodontic patients. Am J Orthod Dentofacial Orthop. 2011;139:55–9. doi: 10.1016/j.ajodo.2009.02.036. [DOI] [PubMed] [Google Scholar]
- 31.Pazzini CA, Marques LS, Ramos-Jorge ML, Júnior GO, Pereira LJ, Paiva SM. Longitudinal assessment of periodontal status in patients with nickel allergy treated with conventional and nickel-free braces. Angle Orthod. 2012;82:653–7. doi: 10.2319/080211-487.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wataha JC. Biocompatibilty of dental casting alloys: A review. J Prosthet Dent. 2000;83:223–34. doi: 10.1016/s0022-3913(00)80016-5. [DOI] [PubMed] [Google Scholar]
- 33.Menné T, Brandup F, Thestrup-Pedersen K, Veien NK, Andersen JR, Yding F, et al. Patch test reactivity to nickel alloys. Contact Dermatitis. 1987;16:255–9. doi: 10.1111/j.1600-0536.1987.tb01448.x. [DOI] [PubMed] [Google Scholar]
- 34.Marigo M, Nouer DF, Genelhu MC, Malaquias LC, Pizziolo VR, Costa AS, et al. Evaluation of immunologic profile in patients with nickel sensitivity due to use of fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2003;124:46–52. doi: 10.1016/s0889-5406(03)00239-7. [DOI] [PubMed] [Google Scholar]
- 35.Toms AP. The corrosion of orthodontic wire. Eur J Orthod. 1988;10:87–97. doi: 10.1093/ejo/10.2.87. [DOI] [PubMed] [Google Scholar]
- 36.Kim H, Johnson J. Corrosion of stainless steel, nickel titanium, coated nickel-titanium, and titanium orthodontic wire. Angle Orthod. 1999;69:39–44. doi: 10.1043/0003-3219(1999)069<0039:COSSNT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 37.Kurol J, Owman-Moll P, Lundgren D. Time related root resorptions after application of a controlled continuous orthodontic force. Am J Orthod Dentofac Orthop. 1996;110:303–10. doi: 10.1016/s0889-5406(96)80015-1. [DOI] [PubMed] [Google Scholar]
- 38.Davidovitch Z, Lee YJ, Counts AL, Park YG, Bursac Z. The immune system possibly modulates orthodontic root resorption. In: Davidovitch Z, Mah J, editors. Biological Mechanisms of Tooth Movement and Craniofacial Adaptation. Boston, MA: Harvard Society for the Advancement of Orthodontics; 2000. pp. 207–17. [Google Scholar]
- 39.McNab S, Battistutta D, Taverne A, Symons AL. External apical root resorption of posterior teeth in asthmatics after orthodontic treatment. Am J Orthod Dentofacial Orthop. 1999;116:545–51. doi: 10.1016/s0889-5406(99)70187-3. [DOI] [PubMed] [Google Scholar]
- 40.Nishioka M, Ioi H, Nakata S, Nakasima A, Counts A. Root resorption and immune system factors in the Japanese. Angle Orthod. 2006;76:103–8. doi: 10.1043/0003-3219(2006)076[0103:RRAISF]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 41.Owman-Moll P, Kurol J. Root resorption after orthodontic treatment in high- and low-risk patients: Analysis of allergy as a possible predisposing factor. Eur J Orthod. 2000;22:657–63. doi: 10.1093/ejo/22.6.657. [DOI] [PubMed] [Google Scholar]
- 42.Symons AL, Stritzel F, Stamation J. Anomalies associated with hypodontia of the permanent lateral incisors and second premolars. J Clin Pediatr Dent. 1993;17:109–11. [PubMed] [Google Scholar]
- 43.Larmour CJ, Mossey PA, Thind BS, Forgie AH, Stirrups DR. Hypodontia–a retrospective review of prevalence and etiology. Part I. Quintessence Int. 2005;36:263–70. [PubMed] [Google Scholar]
- 44.Yamaguchi T, Tomoyasu Y, Nakadate T, Oguchi K, Maki K. Allergy as a possible predisposing factor for hypodontia. Eur J Orthod. 2008;30:641–4. doi: 10.1093/ejo/cjn043. [DOI] [PubMed] [Google Scholar]


