Abstract
Purpose of review
Advances in medical care have led to an increasing elderly population. Elderly individuals should be able to participate in society as long as possible. However, with an increasing age their adaptive capacity gradually decreases, specially before and after major life events (like hospitalization and surgery) making them vulnerable to reduced functioning and societal participation. Therapeutic exercise before and after surgery might augment the postoperative outcomes by improving functional status and reducing the complication and mortality rate.
Recent findings
There is high quality evidence that preoperative exercise in patients scheduled for cardiovascular surgery is well tolerated and effective. Moreover, there is circumstantial evidence suggesting preoperative exercise for thoracic, abdominal and major joint replacement surgery is effective, provided that this is offered to the high-risk patients. Postoperative exercise should be initiated as soon as possible after surgery according to fast-track or enhanced recovery after surgery principles.
Summary
The perioperative exercise training protocol known under the name ‘Better in, Better out’ could be implemented in clinical care for the vulnerable group of patients scheduled for major elective surgery who are at risk for prolonged hospitalization, complications and/or death. Future research should aim to include this at-risk group, evaluate perioperative high-intensity exercise interventions and conduct adequately powered trials.
Keywords: exercise therapy, functional status, postoperative, preoperative, surgery
INTRODUCTION
The successes of society in terms of education, urbanization, industrialization and innovation, not in the least in healthcare, have led to an increasing elderly population [1]. This still expanding generation of the elderly should be able to participate in society for as long as possible. However, with an increasing age their adaptive capacity gradually decreases [2], which makes the elderly vulnerable to reduced functioning and societal participation [3] due to gradually diminishing physical activity [4,5], stereotypical ‘to be old is to be ill’ and ‘let it be’ beliefs [6, 7]. Major life events like hospitalization and surgery can further compromise their functional status and activities of daily living [8]. This decrease in adaptive capacity of (vulnerable) elderly can be reduced by recent medical innovations and can be reduced more or possibly even prevented by therapeutic physical exercise training and maintaining physical activity in the course of an event; enabling the elderly to remain independent and live independently for a longer period of time after the event [4,9,10].
In case of elective surgery, exercise therapy could be initiated preoperatively in patients at risk for unsatisfactory surgical outcomes [11], and be continued during the early and late postoperative period [12] until maximal recovery of physical function and societal participation is achieved. This article provides the latest insights and evidence into pre and postoperative therapeutic exercise training to counterbalance the detrimental effects of hospitalization combined with either cardiovascular, abdominal, thoracic, or orthopedic surgery.
Box 1.
no caption available
EFFECTS OF HOSPITALIZATION AND SURGERY IN OLDER PATIENTS
Temporary functional decline among the elderly as a result of decreased physical activity is a common side-effect before, during, and after hospitalization and major surgery [13,14▪▪]. Already before admission, up to 50% of the elderly patients experience loss of functioning [14▪▪]. Some hospitalized patients spend around 80% of the hospital stay lying in bed, generally without medical reason [15▪]. This bed rest leads to a marked and rapid loss of lower extremity strength, power and aerobic capacity [16], particularly in those with distinct risk profiles [17]. Surgery is known to augment this muscle wasting due to surgical stress [18], which may even lead to more serious or even life-threatening conditions as is the case with patients undergoing surgical manipulations close to the diaphragm. Here, the muscular component of the diaphragm suffers an additional degradation by reflex inhibition of phrenic nerve output and/or mechanical ventilation, further compromising the diaphragmatic function thereby increasing the risk of serious pulmonary complications [16]. Apart from decreased inpatient physical activity and temporary sedentary behavior, the so-called, surgical stress syndrome, is a physiological contributor to functional decline. This surgical stress response includes a wide range of physiological effects that directly impair cardiopulmonary, muscle and neurological function [19], and contribute to an accelerated loss of lean tissue [20]. Aforementioned consequences of hospitalization and surgery lead to protracted functional decline, which can be considered an iatrogenic process in elderly patients, as it leads to a higher risk of postoperative complications and mortality, a prolonged hospital stay and/or readmissions, and/or a prolonged and sometimes even permanent loss of mobility and activities of daily living.
We depicted these phenomena in Fig. 1, in which preoperative functional status plays a key role in the adaptive responses from hospitalization and surgery [21]. We define functional status as part of patients’ health and consider health a dynamic property [22]. Thus, a physically healthy person has the capacity to cope with physiological stress (including surgical stress) and to restore the body's physiological balance, a process called allostasis [2].
FIGURE 1.
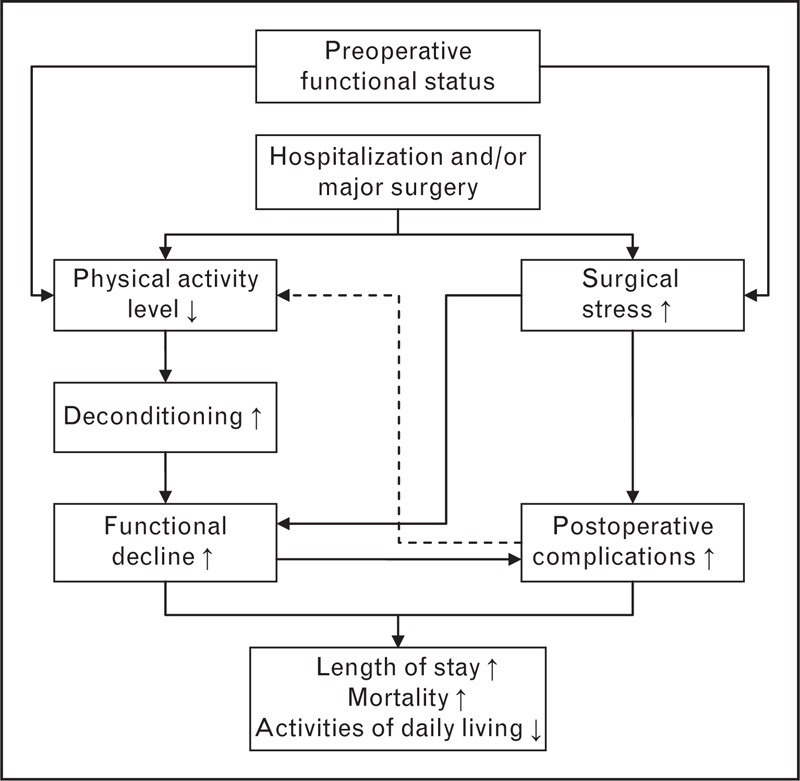
Depiction of possible effects of surgery and hospitalization in older patients and the role of preoperative functional status [21].
MODIFIABLE COURSE OF FUNCTIONAL STATUS BEFORE AND AFTER SURGERY
After major surgery functional status thus dips immediately and substantially, with a recovery of functional status during the postoperative period [23,24]. The majority of patients demonstrate an adequate surgical stress response and most patients regain prehospitalization level of functioning [2,23]. However, patients with a poorer preoperative physical condition might not be able to respond to the detrimental effects of hospitalization and surgery, which may hamper postoperative recovery, increasing hospitalization times and operative mortality.
Knowing the detrimental impact of surgical interventions it is important to determine whether the risk of surgery is personally acceptable for each individual patient. Therefore, health professionals need to screen and monitor for known risk factors. They need to determine physical fitness and activity factors in each patient to ascertain whether and when surgery is an appropriate intervention, and identify patients who may need additional necessary preventive care. Functional status can be improved by high-quality therapeutic exercise, even in the (very) old and frail [25] and even in a short timeframe like the waiting for surgery [26]. Therapeutic exercise training should be considered to improve perioperative outcomes and functional status [24].
Risk stratification enables one to identify patients who are eligible for preoperative training, to optimize their physical status prior to elective surgery, so that they can withstand the negative consequences of surgery and minimize decrease in their perioperative functional status. The latter could be amplified with timely mobilization and, again, training after surgery an intervention. This is known as ‘Better in, Better out’. In the following paragraphs, we discuss the merits of screening for risks, preoperative and postoperative exercise therapy in the physically frail patients in respectively cardiovascular, thorax, abdominal and major joint replacement surgery.
THERAPEUTIC PHYSICAL EXERCISE TRAINING IN CARDIOVASCULAR SURGERY
Undergoing cardiac surgery is a significant life event and has an important psychoemotional impact on patients and their families. Most patients report fear and anxiety and many report that uncertainty about the future is more disturbing than their chest pain. The longer a patient stays on the waiting list for cardiac surgery, the more likely they are to reduce their leisure activities, causing them to experience anxiety, reduced physical and social functioning, poorer vitality and general health [27].
In cardiac surgery, short-term mortality is frequently used as a measure of performance, whereas postoperative pulmonary complications (PPCs) are recognized as being a major determinant of hospital costs and quality of life after heart surgery [28]. PPCs can lead to postoperative morbidity and mortality, increased use of medical resources, length of hospital stay and healthcare costs [29]. Preoperative identification of patients at high risk of developing functional decline and/or PPCs (e.g. pneumonia) after cardiac surgery can help clinicians to direct their interventions toward these patients. A six-factor model (age ≥ 70 years, productive cough, smoking, diabetes mellitus, inspiratory vital capacity and maximum expiratory mouth pressure lower than 75% of the predicted value) is a useful tool to predict the risk of developing PPCs in patients undergoing elective cardiac surgery [30].
Evidence demonstrates that preoperative physical therapy reduces PPCs (i.e. atelectasis and pneumonia) and length of hospital stay in patients undergoing elective cardiac surgery [26]. In particular, preoperative inspiratory muscle training has positive effects in patients with a high risk of developing PPCs awaiting cardiac surgery [31], while its effects in relatively healthy patients are likely negligible [11]. Maximal inspiratory muscle strength is a clinically relevant indicator of respiratory fitness that can be improved by training the inspiratory muscle before surgery; thus improving the preoperative respiratory condition of patients. A reference chart is developed to monitor the maximal inspiratory muscle strength and to provide feedback for both patient and their therapist [32▪]. Feedback given to patients may improve their motivation, and thus contribute further to lower the risk of PPCs.
Exercise therapy after cardiac surgery is generally used for the prevention and/or treatment of PPCs and motor complications in an attempt to accelerate the recovery of (lung) function and functional status. In a literature review on the different techniques used in chest physiotherapy after cardiac surgery, there is no consensus regarding the superiority of one technique over the other [33]. Regarding the recovery of function, evidence suggests that postoperative fast-track mobilization reduces the time to extubation and shortens the length of stay in the ICU after cardiac surgery [34].
THERAPEUTIC PHYSICAL EXERCISE TRAINING IN MAJOR ABDOMINAL AND THORACIC SURGERY
As in open heart surgery, successful postoperative recovery from abdominal and thoracic surgery also depends on the ability of patients to cope with impaired cardiopulmonary and (respiratory) muscle function. An insufficient adaptive capacity may compromise postoperative functional recovery, potentially leading to postoperative complications, death, and protracted and sometimes permanent loss of mobility [8]. Conventional risk factors in abdominal surgery are generally related to demographics, such as age and smoking habits, and comorbidities, such as diabetes, chronic obstructive pulmonary disease and heart disease [35]. More recently, the relationship between postoperative outcomes and measures of physical fitness and activity like cardiorespiratory fitness and muscle function was demonstrated [36,37]. For instance, cardiorespiratory fitness is a strong independent predictor of survival after lung surgery for nonsmall cell lung cancer [38]. Moreover, in older patients undergoing abdominal surgery, physical fitness and activity are significantly and strongly associated with the postoperative outcomes such as mortality, length of stay and recovery of functional. The addition of these variables to prediction models involving conventional factors significantly improved the prediction of mortality, discharge destination and length of stay [36].
Apart from a predictive factor, physical fitness is also a modifiable and treatable factor during the preoperative phase. If there is a cause–effect relationship with the postoperative course, patients will benefit from preoperative interventions to improve their physical fitness. Evidence is accumulating that inspiratory muscle training decreases the incidence of PPCs after abdominal and thoracic surgery [39]. Moreover, preoperative aerobic exercise training is associated with improved physical fitness of patients before [40▪] and improved functional recovery after abdominal and thoracic surgery [41]. Evidence for the prevention of postoperative complications is still weak [40▪,42–44], as most studies lack statistical power to demonstrate an effect on postoperative complications. Therefore, in order to determine the effectiveness of this intervention, it is recommended to include patients at high risk for postoperative complications. Personalized and well monitored and titrated high-intensity training is necessary to achieve improvements, given the often short time available before surgery [45].
In the postoperative period, recovery of patients’ physical fitness and activity is also of importance as immobilization in this period is associated with postoperative complications and poor functional outcome [12]. Studies investigating early physical training demonstrated improvements on physical fitness and on disability measures at discharge and a reduction in the number of transfers to a nursing home [12,46]. Physical training is often part of a multi(parallel) or inter(integrated) disciplinary rehabilitation approach, known under the names as fast-track or enhanced recovery after surgery. These programs also include dietary guidance and adequate analgesia to enable physical activity. The merits of these programs have been proven, demonstrating a decrease in the length of hospital stay and postoperative complications [47].
THERAPEUTIC PHYSICAL EXERCISE TRAINING IN HIP (THR) AND KNEE REPLACEMENT (TKR)
Elective major joint replacement is generally advocated as a highly successful operation for relieving symptoms in people suffering from hip or knee osteoarthritis. Such claims are often made from a medical and biomechanical perspective (i.e. in terms of low rates of complications and prosthesis failure), rather than the perspective of the patient (i.e. pain, functional status and societal participation). Hawker et al.[48] demonstrated that nearly half of the people had poor outcomes on pain and functioning; these were mostly the elderly patients with additional comorbidities. Pre and postoperative exercise therapy might augment the postoperative functional recovery of patients undergoing total hip replacement (THR) or total knee replacement (TKR). To date, several reviews are available that systematically synthesized the literature on preoperative exercise in individuals awaiting major joint replacement; concluding that preoperative exercise has little worth on postoperative outcomes [49]. However, most of the included studies investigated the effectiveness of preoperative exercise in generally healthy adults, whereas in essence eligible people with comorbidities and/or higher age were excluded [50]; yielding at best small effect sizes [51]. The inclusion of the fit elderly distorts results, as patients of higher age with comorbidities are the ones with a significant risk of disappointing surgery outcomes [48]. Therefore to understand and appreciate the true potential of preoperative therapeutic exercise, we need to evaluate studies that did include individuals with a higher risk for disappointing outcomes after surgery.
To date two studies are available that investigated the merits of preoperative exercise in patients with an increased risk for delayed functional recovery or increased length of hospital stay in a typical Western care setting [52,53]. Topp et al.[52] investigated the effectiveness of therapeutic exercise in patients with low preoperative functional level awaiting TKR. They found that after 3 months the functional performance level and strength of the people in the preoperative exercise group was better restored than in the control group. Hansen et al.[53] demonstrated that, in the context of fast-track rehabilitation, preoperative therapeutic exercise of individuals with an increased risk of delayed recovery, can further shorten the hospital stay by one additional day after THR or TKR. The previous study suggests that an adequate selection of high-risk patients before surgery is essential for the success of preoperative exercise in THR and TKR. Considering that preoperative exercise is fairly cheap, well tolerated and clinically relevant, it needs to be considered an intervention of choice in aiding the recovery after total joint replacement [54].
For postoperative exercise therapy, evidence suggests that the retraining of functional abilities should be initiated within 4 h after surgery [55]. However, the effectiveness of postdischarge exercise is still under debate [55,56]. Experts in the field conclude that therapeutic exercise training is often of limited intensity and/or offered too late after surgery [57,58]. The latter is confirmed by the study of Pozzi et al.[56] who recommend strength and functional exercise therapy highly tailored to the needs of the patient to improve postoperative recovery. To do so, supervision by a trained physical therapist is essential. Low intensity, unsupervised exercise should be avoided.
RECOMMENDATIONS FOR FUTURE RESEARCH
The current evidence for perioperative exercise therapy is currently skewed toward small RCTs with relatively fit elderly patients, testing mostly generalized (‘one size fits all’) low-to-moderate intensity general exercise programs, which is neither cost-effective nor a targeted approach. Instead, research should identify which aspects of (preventive) exercise training programmes [strength, (an) aerobic capacity or functional mobility] are appropriate and tolerable for individual or specific groups of patients [50]. Moreover, exercise training-related research should also incorporate monitoring principles to establish the optimum in training parameters for each individual patient [32▪]. High-intensity training is necessary to achieve improvements given the often short time available before surgery. Fortunately, frail and older patients can tolerate the programs [25].
CONCLUSION
There is high quality evidence that perioperative exercise in patients scheduled for cardiac surgery is well tolerated and effective. Moreover, there is circumstantial evidence suggesting the same for thorax, abdominal and major joint replacement surgery provided that this is offered to the high-risk patients. We conclude that this participatory, preventive, predictive and preferably personalized perioperative exercise training intervention might be a valuable asset to concepts like ‘strong for surgery’ [59] as a component of an elderly friendly healthcare system as a whole [60]. Implementation should be guided by proper monitoring of the effects in the real-life context of the care system.
Acknowledgements
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Gehem M, Diaz PS. Shades of graying: research tackling the grand challenges of aging for Europe. The Hague:The Hague Centre for Strategic Studies and TNO; 2013 [Google Scholar]
- 2.McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev 2007; 87:873–904 [DOI] [PubMed] [Google Scholar]
- 3.Smith AK, Walter LC, Miao Y, et al. Disability during the last two years of life. JAMA Intern Med 2013; 173:1506–1513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown CJ, Flood KL. Mobility limitation in the older patient: a clinical review. JAMA 2013; 310:1168–1177 [DOI] [PubMed] [Google Scholar]
- 5.Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012; 380:247–257 [DOI] [PubMed] [Google Scholar]
- 6.Stewart TL, Chipperfield JG, Perry RP, Weiner B. Attributing illness to ‘old age:’ consequences of a self-directed stereotype for health and mortality. Psychol Health 2012; 27:881–897 [DOI] [PubMed] [Google Scholar]
- 7.Levy B. Stereotype embodiment: a psychosocial approach to aging. Curr Dir Psychol Sci 2009; 18:332–336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boyd CM, Landefeld CS, Counsell SR, et al. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc 2008; 56:2171–2179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rimmer JH, Marques AC. Physical activity for people with disabilities. Lancet 2012; 380:193–195 [DOI] [PubMed] [Google Scholar]
- 10.Tak E, Kuiper R, Chorus A, Hopman-Rock M. Prevention of onset and progression of basic ADL disability by physical activity in community dwelling older adults: a meta-analysis. Ageing Res Rev 2012; 12:329–338 [DOI] [PubMed] [Google Scholar]
- 11.Lemanu DP, Singh PP, MacCormick AD, et al. Effect of preoperative exercise on cardiorespiratory function and recovery after surgery: a systematic review. World J Surg 2013; 37:711–720 [DOI] [PubMed] [Google Scholar]
- 12.Patel BK, Hall JB. Perioperative physiotherapy. Curr Opin Anaesthesiol 2013; 26:152–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gill TM, Gahbauer EA, Murphy TE, et al. Risk factors and precipitants of long-term disability in community mobility: a cohort study of older persons. Ann Intern Med 2012; 156:131–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14▪▪.Palleschi L, Fimognari FL, Pierantozzi A, et al. Acute functional decline before hospitalization in older patients. Geriatr Gerontol Int 2013; [Epub ahead of print] [DOI] [PubMed] [Google Scholar]; The detrimental effects of waiting for surgery generally remain unrecognized. Up to 50% of the patients, especially those who are vulnerable, fall victim to further functional decline; putting them at greater risk for unwelcome surgical outcomes like complications, disability or even mortality.
- 15▪.Brown CJ, Redden DT, Flood KL, Allman RM. The underrecognized epidemic of low mobility during hospitalization of older adults. J Am Geriatr Soc 2009; 57:1660–1665 [DOI] [PubMed] [Google Scholar]; To adapt and self-manage is by some proposed as a new definition for health. Clearly, this way of thinking has not been adopted in our hospital systems as this is still very much characterized by passive and inactive care.
- 16.Welvaart WN, Paul MA, Stienen GJM, et al. Selective diaphragm muscle weakness after contractile inactivity during thoracic surgery. Ann Surg 2011; 254:1044–1049 [DOI] [PubMed] [Google Scholar]
- 17.Buurman BM, Hoogerduijn JG, van Gemert EA, et al. Clinical characteristics and outcomes of hospitalized older patients with distinct risk profiles for functional decline: a prospective cohort study. PLoS One 2012; 7:e29621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paddon-Jones D, Sheffield-Moore M, Cree MG, et al. Atrophy and impaired muscle protein synthesis during prolonged inactivity and stress. J Clin Endocrinol Metab 2006; 91:4836–4841 [DOI] [PubMed] [Google Scholar]
- 19.Desborough JP. The stress response to trauma and surgery. Br J Anaesth 2000; 85:109–117 [DOI] [PubMed] [Google Scholar]
- 20.Bautmans I, Njemini R, De Backer J, et al. Surgery-induced inflammation in relation to age, muscle endurance, and self-perceived fatigue. J Gerontol A Biol Sci Med Sci 2010; 65:266–273 [DOI] [PubMed] [Google Scholar]
- 21.Dronkers JJ. Preoperative physical fitness in older patients. [thesis]. 2013 [Google Scholar]
- 22.Huber M, Knottnerus JA, Green L, et al. How should we define health? BMJ 2011; 343:d4163. [DOI] [PubMed] [Google Scholar]
- 23.Brown CJ, Roth DL, Allman RM, et al. Trajectories of life-space mobility after hospitalization. Ann Intern Med 2009; 150:372–378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Topp R, Ditmyer M, King K, et al. The effect of bed rest and potential of prehabilitation on patients in the intensive care unit. AACN Clin Issues 2002; 13:263–276 [DOI] [PubMed] [Google Scholar]
- 25.Chou C-H, Hwang C-L, Wu Y-T. Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: a meta-analysis. Arch Phys Med Rehabil 2012; 93:237–244 [DOI] [PubMed] [Google Scholar]
- 26.Hulzebos EHJ, Smit Y, Helders PPJM, van Meeteren NLU. Preoperative physical therapy for elective cardiac surgery patients. Cochrane database Syst Rev 2012; 11:CD010118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosenfeldt F, Braun L, Spitzer O, et al. Physical conditioning and mental stress reduction: a randomised trial in patients undergoing cardiac surgery. BMC Complement Altern Med 2011; 11:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hannan EL, Wu C, Bennett EV, et al. Risk stratification of in-hospital mortality for coronary artery bypass graft surgery. J Am Coll Cardiol 2006; 47:661–668 [DOI] [PubMed] [Google Scholar]
- 29.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics: 2013 update – a report from the American Heart Association. Circulation 2013; 127:e6–e245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hulzebos EHJ, van Meeteren NLU, De Bie RA, et al. Prediction of postoperative pulmonary complications on the basis of preoperative risk factors in patients who had undergone coronary artery bypass graft surgery. Phys Ther 2003; 83:8–16 [PubMed] [Google Scholar]
- 31.Hulzebos EHJ, Helders PJM, Favié NJ, et al. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. JAMA 2006; 296:1851–1857 [DOI] [PubMed] [Google Scholar]
- 32▪.van Buuren S, Hulzebos EHJ, Valkenet K, et al. Reference chart of inspiratory muscle strength: a new tool to monitor the effect of preoperative training. Physiotherapy 2013; 10.1016/j.physio.2013.08.007 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]; The authors introduce a new method for physiotherapists that enables them to monitor patients’ progress (and when necessary titrate) during an intervention episode. An approach worth being followed by other (physiotherapy) researchers.
- 33.Cavenaghi S, Ferreira LL, Marino LHC, Lamari NM. Respiratory physiotherapy in the pre and postoperative myocardial revascularization surgery. Rev Bras Cir Cardiovasc 2011; 26:455–461 [DOI] [PubMed] [Google Scholar]
- 34.Zhu F, Lee A, Chee YE. Fast-track cardiac care for adult cardiac surgical patients. Cochrane database Syst Rev 2012; 10:CD003587. [DOI] [PubMed] [Google Scholar]
- 35.Kennedy GD, Rajamanickam V, O’connor ES, et al. Optimizing surgical care of colon cancer in the older adult population. Ann Surg 2011; 253:508–514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dronkers JJ, Chorus AMJ, van Meeteren NLU, Hopman-Rock M. The association of preoperative physical fitness and physical activity with outcome after scheduled major abdominal surgery. Anaesthesia 2013; 68:67–73 [DOI] [PubMed] [Google Scholar]
- 37.Revenig LM, Canter DJ, Taylor MD, et al. Too frail for surgery? Initial results of a large multidisciplinary prospective study examining preoperative variables predictive of poor surgical outcomes. J Am Coll Surg 2013; 217:665–670e1 [DOI] [PubMed] [Google Scholar]
- 38.Jones LW, Watson D, Herndon JE, et al. Peak oxygen consumption and long-term all-cause mortality in nonsmall cell lung cancer. Cancer 2010; 116:4825–4832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Valkenet K, van de Port IGL, Dronkers JJ, et al. The effects of preoperative exercise therapy on postoperative outcome: a systematic review. Clin Rehabil 2011; 25:99–111 [DOI] [PubMed] [Google Scholar]
- 40▪.O’Doherty AF, West M, Jack S, Grocott MPW. Preoperative aerobic exercise training in elective intra-cavity surgery: a systematic review. Br J Anaesth 2013; 110:679–689 [DOI] [PubMed] [Google Scholar]; In this review, the authors present a clear overview of effect and importance of the aerobic component of preoperative training on relevant postoperative outcome measures after intracavity surgery.
- 41.Nagarajan K, Bennett A, Agostini P, Naidu B. Is preoperative physiotherapy/pulmonary rehabilitation beneficial in lung resection patients? Interact Cardiovasc Thorac Surg 2011; 13:300–302 [DOI] [PubMed] [Google Scholar]
- 42.Morano MT, Araújo AS, Nascimento FB, et al. Preoperative pulmonary rehabilitation versus chest physical therapy in patients undergoing lung cancer resection: a pilot randomized controlled trial. Arch Phys Med Rehabil 2013; 94:53–58 [DOI] [PubMed] [Google Scholar]
- 43.Dronkers JJ, Lamberts H, Reutelingsperger IMMD, et al. Preoperative therapeutic programme for elderly patients scheduled for elective abdominal oncological surgery: a randomized controlled pilot study. Clin Rehabil 2010; 24:614–622 [DOI] [PubMed] [Google Scholar]
- 44.Jack S, West M, Grocott MPW. Perioperative exercise training in elderly subjects. Best Pract Res Clin Anaesthesiol 2011; 25:461–472 [DOI] [PubMed] [Google Scholar]
- 45.Lindelöf N, Rosendahl E, Gustafsson S, et al. Perceptions of participating in high-intensity functional exercise among older people dependent in activities of daily living (ADL). Arch Gerontol Geriatr 2013; 57:369–376 [DOI] [PubMed] [Google Scholar]
- 46.Kosse NM, Dutmer AL, Dasenbrock L, et al. Effectiveness and feasibility of early physical rehabilitation programs for geriatric hospitalized patients: a systematic review. BMC Geriatr 2013; 13:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhuang C-L, Ye X-Z, Zhang X-D, et al. Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum 2013; 56:667–678 [DOI] [PubMed] [Google Scholar]
- 48.Hawker GA, Badley EM, Borkhoff CM, et al. Which patients are most likely to benefit from total joint arthroplasty? Arthritis Rheum 2013; 65:1243–1252 [DOI] [PubMed] [Google Scholar]
- 49.Mak JCS, Fransen M, Jennings M, et al. Evidence-based review for patients undergoing elective hip and knee replacement. ANZ J Surg 2013; 10.1111/ans.12109 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 50.Hoogeboom TJ, Oosting E, Vriezekolk JE, et al. Therapeutic validity and effectiveness of preoperative exercise on functional recovery after joint replacement: a systematic review and meta-analysis. PLoS One 2012; 7:e38031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Villadsen A, Overgaard S, Holsgaard-Larsen A, et al. Postoperative effects of neuromuscular exercise prior to hip or knee arthroplasty: a randomised controlled trial. Ann Rheum Dis 2013; [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 52.Topp R, Swank AM, Quesada PM, et al. The effect of prehabilitation exercise on strength and functioning after total knee arthroplasty. PM R 2009; 1:729–735 [DOI] [PubMed] [Google Scholar]
- 53.Hansen TB, Bredtoft HK, Larsen K. Preoperative physical optimization in fast-track hip and knee arthroplasty. Dan Med J 2012; 59:A4381. [PubMed] [Google Scholar]
- 54.Oosting E, Jans MP, Dronkers JJ, et al. Preoperative home-based physical therapy versus usual care to improve functional health of frail older adults scheduled for elective total hip arthroplasty: a pilot randomized controlled trial. Arch Phys Med Rehabil 2012; 93:610–616 [DOI] [PubMed] [Google Scholar]
- 55.Ibrahim MS, Khan MA, Nizam I, Haddad FS. Peri-operative interventions producing better functional outcomes and enhanced recovery following total hip and knee arthroplasty: an evidence-based review. BMC Med 2013; 11:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pozzi F, Snyder-Mackler L, Zeni J. Physical exercise after knee arthroplasty: a systematic review of controlled trials. Eur J Phys Rehabil Med 2013; [Epub ahead of print] [PMC free article] [PubMed] [Google Scholar]
- 57.Bandholm T, Kehlet H. Physiotherapy exercise after fast-track total hip and knee arthroplasty: time for reconsideration? Arch Phys Med Rehabil 2012; 93:1292–1294 [DOI] [PubMed] [Google Scholar]
- 58.Bade MJ, Stevens-Lapsley JE. Restoration of physical function in patients following total knee arthroplasty: an update on rehabilitation practices. Curr Opin Rheumatol 2012; 24:208–214 [DOI] [PubMed] [Google Scholar]
- 59.Strong for Surgery: CERTAIN. http://www.becertain.org/strong_for_surgery [Accessed 12 October 2013] [Google Scholar]
- 60.Hood L, Flores M. A personal view on systems medicine and the emergence of proactive P4 medicine: predictive, preventive, personalized and participatory. N Biotechnol 2012; 29:613–624 [DOI] [PubMed] [Google Scholar]


