Abstract
STUDY DESIGN
Prospective analysis of a longitudinal cohort with an embedded comparison group at a single time point.
OBJECTIVES
To determine the feasibility and effectiveness of an outpatient rehabilitation protocol that includes movement symmetry biofeedback on functional and biomechanical outcomes after total knee arthroplasty (TKA).
BACKGROUND
TKA reduces pain and improves functional ability, but many patients experience strength deficits and movement abnormalities in the operated limb, despite outpatient rehabilitation. These asymmetries increase load on the nonoperated limb, and greater asymmetry is related to worse functional outcomes.
METHODS
Biomechanical and functional metrics were assessed 2 to 3 weeks prior to TKA, at discharge from outpatient physical therapy, and 6 months after TKA in 11 patients (9 men, 2 women; mean ± SD age, 61.4 ± 5.8 years; body mass index, 33.1 ± 5.4 kg/m2) who received 6 to 8 weeks of outpatient physical therapy that included specialized symmetry training. Six-month outcomes were compared to a control group, matched by age, body mass index, and sex (9 men, 2 women; mean ± SD age, 61.8 ± 5 years; body mass index, 34.3 ± 5.1 kg/m2), that did not receive specialized symmetry retraining.
RESULTS
Of the 11 patients who received added symmetry training, 9 demonstrated clinically meaningful improvements that exceeded the minimal detectable change for all performance-based functional tests at 6 months post-TKA compared to pre-TKA. Six months after TKA, when walking, patients who underwent symmetry retraining had greater knee extension during midstance and had mean sagittal knee moments that were more symmetrical, biphasic, and more representative of normal knee kinetics compared to patients who did not undergo symmetry training. No patients experienced adverse events as the result of the protocol.
CONCLUSION
Adding symmetry retraining to postoperative protocols is clinically viable, safe, and may have additional benefits compared to rehabilitation protocols that focus on range of motion, strength, and return to independence.
Keywords: biomechanics, gait, joint replacement, sit-to-stand
Total knee arthroplasty (TKA) has become the surgical standard for the management of pain and disability associated with knee osteoarthritis (OA). More than 500 000 TKAs are performed annually in the United States,27 and this is expected to increase 6-fold over the next 20 years.13 Although this procedure typically reduces joint pain and improves functional performance,21 most patients continue to demonstrate residual strength impairments and functional deficits up to 1 year after TKA.8,28 Rehabilitation is an important component of postoperative management. Patients who receive early, progressive strengthening interventions demonstrate larger improvements in functional performance21 and quicker strength gains23 compared to individuals who receive lower-intensity postoperative rehabilitation.4
Despite improvements in strength and functional performance, patients who undergo progressive outpatient rehabilitation after TKA continue to demonstrate persistent movement asymmetries that increase the load on the nonoperated knee.2 These movement asymmetries are related to interlimb discrepancies in quadriceps strength17; however, unilateral quadriceps weakness does not account for all of the variability in movement asymmetries. Although few longitudinal studies have evaluated movement patterns before and after TKA, some evidence suggests that asymmetries that reduce reliance on the operated limb are adopted in the presence of pain and weakness before TKA and persist after surgery, despite traditional rehabilitation.15 This finding is not isolated to individuals post-TKA; Kneiss et al12 reported that patients post–hip fracture demonstrated interlimb asymmetrical loading patterns during a sit-to-stand (STS) task, even after discharge from rehabilitation.22 In addition to the potential negative consequences of movement asymmetries on contralateral joint loading, greater asymmetry is also related to worse functional performance.6 Therefore, correcting asymmetrical and abnormal movement patterns should be a focus of postoperative rehabilitation.
We recently developed an outpatient rehabilitation strategy to counteract persistent movement asymmetries after TKA.16 This rehabilitation paradigm includes biofeedback to promote symmetrical weight bearing during functional retraining and strengthening exercises, in addition to a progressive strengthening protocol. The purpose of this research project was to test the feasibility and effectiveness of integrating this symmetry protocol into postoperative outpatient rehabilitation following TKA. We hypothesized that patients who underwent TKA for primary unilateral knee OA would demonstrate clinically meaningful improvements in functional and biomechanical variables after 6 to 8 weeks of rehabilitation that included symmetry retraining. We also hypothesized that patients who participated in symmetry retraining would have 6-month functional and biomechanical outcomes equivalent to or exceeding those of a control group, matched by age, body mass index (BMI), and sex, that did not receive symmetry training.
METHODS
Patients
Eleven patients participated in the symmetry retraining intervention after TKA for OA (9 men, 2 women; mean ± SD age, 61.4 ± 5.8 years; BMI, 33.1 ± 5.4 kg/m2). Biomechanical and functional metrics were assessed 2 to 3 weeks prior to TKA, at discharge from outpatient physical therapy, 3 months after TKA, and 6 months after TKA. Outcomes at 6 months after TKA were compared to those of an age-, sex-, and BMI-matched group of 11 patients (9 men, 2 women; mean ± SD age, 61.8 ± 5 years; BMI, 34.3 ± 5.1 kg/m2) who also underwent TKA 6 months prior. These individuals, referred to as the standard-of-care group, were selected from a concurrent cross-sectional study in which rehabilitation after TKA did not specifically include symmetry-retraining components. For all patients, the surgical procedure was performed by 1 of 2 surgeons. All patients had primarily unilateral pain prior to surgery and were excluded if maximal pain in the nonoperated limb prior to surgery was greater than or equal to 4/10 on a visual analog scale. The testing and intervention protocols were approved by the University of Delaware Human Subjects Review Board, and all subjects signed informed consent forms before participating in testing or the intervention.
Rehabilitation Protocol
The rehabilitation regimen in both groups consisted of outpatient physical therapy that began 2 to 4 weeks after TKA. Patients were treated 2 to 3 times per week for 6 to 10 weeks, depending on their progress toward clinical goals. Standard of care included progressive strengthening, functional retraining, stretching to maximize range of motion, and modalities to reduce pain and swelling.21 The symmetry training consisted of the same protocol, but also included a progressive symmetry-retraining program. Symmetry retraining consisted of visual, auditory, and tactile feedback provided to improve kinetic and kinematic symmetry between limbs.16 Feedback during quadriceps strengthening exercises was provided using the SymSlide (customKYnetics, Inc, Versailles, KY), a leg-press device that monitors the magnitude of force under each limb. When the force between limbs was symmetrical, a visual tracing on a computer monitor remained in the center of the screen. Patients were asked to keep the tracing centered in the screen by applying equal force to both limbs during the task. The amount of allowable error could be reduced as the subject progressed, and resistance could be increased. Furthermore, during STS retraining exercises and wall slides, a Wii Balance Board (Nintendo of America Inc, Redmond, WA) was used to monitor weight distribution between limbs. Visual feedback consisted of 2 cylinders on a computer screen that represented the relative load under each limb as a percentage of total body weight. Patients were cued to maintain symmetrical load under each foot during the exercises. In the symmetry group, patients were progressed from simple symmetrical loading and weight shifting during standing to symmetrical loading during an STS movement performed on a progressively lower surface, and wall slides and squats with progressively lower end points. The allowable error for asymmetry was reduced as milestones were achieved (APPENDIX). The symmetry protocol encouraged and reinforced symmetrical movement patterns for all daily activities, with the intention of promoting symmetrical movement outside the clinic and after discharge from outpatient physical therapy.
Although the exact data were not available, the duration of each therapy session in the standard-of-care group was typically 60 to 75 minutes. Symmetry retraining exercises took approximately 30 minutes to complete. However, this protocol only extended the duration of treatment by 15 minutes. This is attributed to the fact that some exercises were identical between groups—except the symmetry group received visual, auditory, or tactile feedback during the task (treadmill walking, STS exercises, wall slides, step-ups). Symmetry retraining with direct oversight from the physical therapist was considered to consist of neuromuscular re-education of movement, balance, coordination, kinesthetic sense, posture, and proprioception. Patients in the symmetry retraining group averaged 24 treatment sessions, and patients in the standard-of-care group averaged 23 visits (data obtained from 8 of 11 subjects in the standard-of-care group).
Functional Metrics
To gauge functional ability, patients completed a comprehensive battery of functional measures and performance-based tests. For patients in the symmetry group, this was performed 2 to 4 weeks prior to TKA, at initial outpatient physical therapy evaluation (2-3 weeks after TKA), at discharge from physical therapy (3 months after TKA), and at a 6-month follow-up. Patients in the standard-of-care group were only tested 6 months after TKA.
Patients completed the Knee Outcome Survey activities of daily living subscale, a 14-item questionnaire in which patients rate their ability to perform typical functional tasks on a 0-to-5 scale, where 0 represents “inability to perform the task” or “symptom prevents me from completing the task” and 5 represents “no limitations performing the task” or “I don’t have the symptom.” The total score, represented as a percentage, ranges from 0% to 100%, with greater percentages indicating greater perception of functional performance. The Knee Outcome Survey is a responsive measure of function, with excellent test-retest reliability (intraclass correlation coefficient = 0.93) and a minimal detectable change (MDC) of 11.4% on an individual level,9 and has been used to test large groups of individuals before and after TKA.21
Active knee flexion angle was measured using a goniometer, with the patient in a supine position. During this test, patients were asked to pull their heel toward their buttocks as far as possible.
Patients also completed 3 performance-based tests: the timed up-and-go test (TUG), stair-climbing test (SCT), and 6-minute walk test (6MW). For the TUG, patients were asked to stand up from a chair, walk 3 m as fast as possible, turn around, walk back to the chair, and sit down. Minimal detectable change for the TUG is 2.49 seconds in patients with lower extremity OA.19 For the SCT, patients climbed and descended a set of 21 steps as fast as possible, using a handrail if needed. Similar tests show excellent reliability (intraclass correlation coefficient = 0.93),22 are appropriate for this population, and have an MDC of 2.6 seconds.1 For the 6MW, patients were asked to walk as fast as possible for 6 minutes along a 30-m squared hallway. This test is responsive20 and has an MDC of 61 m.11
Quadriceps isometric strength was measured using an electromechanical dynamometer (Kin-Com 500 H; Isokinetic International, Harrison, TN). Patients were seated with the knee flexed at a 75° angle. After a warm-up session of 2 sub-maximal (50% and 75%) and 1 maximal quadriceps contractions, patients performed 3 maximal isometric contractions with 1 minute of rest between trials. The uninvolved limb was tested first, followed by the involved limb. The quadriceps index (QI) was then calculated by dividing the maximal force output of the involved limb by that of the uninvolved limb. The outcome was represented as a percentage of perfect symmetry (100%), with values less than 100% representing weakness of the operated limb compared to the nonoperated limb.
Motion Analysis
Patients were asked to wear low-top sneakers that fit comfortably. A 3-D, 8-camera motion-capture system (Vicon; OMG plc, Oxford, UK), synchronized with 2 force platforms (Bertec Corporation, Columbus, OH), was used for motion analysis. On each patient, 16-mm spherical retroreflective markers were placed bilaterally on the iliac crest, greater trochanter, lateral femoral condyle, lateral malleolus, and the head of the fifth metatarsal, and 2 markers were placed on the heel. Rigid thermoplastic shells with 4 markers were secured bilaterally on the lower legs and thighs. Pelvic motion was tracked using a rigid thermoplastic shell, with 3 markers placed below the line between the 2 posterior superior iliac spines. Marker data were sampled at 120 Hz, and the force-platform data were collected at 1080 Hz.
A standing calibration was first obtained to identify joint centers and to create a segment coordinate system. Kinematics and kinetics calculations were performed using Visual3D software (C-Motion, Inc, Germantown, MD). Marker trajectories were low-pass filtered at 6 Hz, and force-platform data were filtered at 40 Hz using a second-order, phase-corrected Butterworth filter. Joint angles were calculated using the Euler x-y-z sequence corresponding to flexion/extension, abduction/adduction, and rotation sequences. Calculations for joint moments were performed with 3-D inverse dynamics and expressed as external moments normalized to body mass and height (Nm/kg·m). The external knee flexion moment represents the rotational force applied by external forces (ground reaction force) and inertial properties that act to flex the knee in the sagittal plane. This moment must be balanced by an internal extension moment produced by quadriceps muscle and/or connective tissue. Therefore, the external knee flexion moment is a surrogate measure of quadriceps function, particularly during the loading-response phase of gait.
For the symmetry group, motion analysis was performed before surgery, 3 months postsurgery, and 6 months postsurgery. The standard-of-care group only participated in motion analysis 6 months after surgery.
Chair Rise
Patients performed the chair-rise task on an armless and backless chair. The height of the chair was set to ensure that the patient’s knees were positioned at 90° of flexion when sitting. Chair rise was performed at a self-selected pace and with a self-selected foot position. Patients were instructed to hold their arms across their chest, not to use their arms to assist with rising from the chair, and not to look at the chair when sitting down. Data were collected from 5 trials for each subject. In each trial, the subject stood from the seated position (STS), stood still for 1 second (standing portion), and returned to a seated position (return-to-sit [RTS]). The symmetry ratio, calculated as the value for the operated limb divided by the value for the nonoperated limb, was determined for the mean vertical ground reaction force (VGRF) during the STS, standing, and RTS portions of the chair rise. The symmetry ratio was also calculated for the peak external knee flexion moment (PEKFM) during the STS portion.
Gait
Five walking trials were collected for each patient, with acceptable trials requiring a clean foot strike for each force plate and a walking speed of ±5% of predetermined self-selected walking speed. Knee flexion angle and external knee flexion moment were analyzed during the stance phase of gait. Data were time normalized as a percentage of stance phase, with 0% representing initial contact and 100% representing toe-off. Gait events were detected using a 20-N threshold of VGRF.
Data Analysis
Functional Data
Descriptive statistics of all clinical metrics were calculated (mean and standard deviation) before surgery, at initial outpatient physical therapy evaluation post-TKA, at discharge 3 months post-TKA, and at 6 months post-TKA for the symmetry group. The mean and standard deviation were also calculated for the standard-of-care group, but only at the 6-month time point. Effect sizes were calculated between the symmetry group and the standard-of-care group at the 6-month post-TKA time point. Percent change was calculated over time for the symmetry group, and percent difference was calculated between the symmetry and standard-of-care groups at the 6-month time point. The number of patients whose improvement exceeded the MDC for each metric between the preoperative time point and discharge from physical therapy was also quantified.
Biomechanical Data
Symmetry ratios were calculated for mean VGRF and PEKFM during the chair-rise task. This ratio was calculated as the value on the operated side divided by the value on the nonoperated side. A value equal to 1 represents perfect symmetry, values greater than 1 represent higher values on the operated side, and values less than 1 represent lower values on the operated side. Mean and standard deviation for symmetry ratios were calculated at the preoperative, 3-month, and 6-month post-TKA time points for the symmetry group and only at the 6-month time point for the standard-of-care group. Descriptive statistics (percent improvement) were calculated over time for the symmetry group, and descriptive comparisons (percent difference) were calculated for between-group comparisons at the 6-month time point. To better describe distribution of symmetry ratios within each group, we calculated the percent of individuals with symmetry ratios greater than or equal to 0.90 and less than 0.90 at all time points for the symmetry group and at 6 months for the standard-of-care group. It has been suggested that most healthy individuals have symmetry ratios between 0.90 and 1.10.14,25 During gait, ensemble time-series curves for sagittal plane knee moments were calculated for both limbs of patients in the symmetry group prior to TKA and at the 3-month time point. Ensemble curves for sagittal plane knee moment and angle were also created for both limbs of patients in the standard-of-care and symmetry groups at the 6-month time point for qualitative comparison. Visual inspection of these time-series curves was performed to detect obvious differences between time and group.
RESULTS
Functional Outcomes
Longitudinal Analysis for Symmetry Group
At the initial physical therapy evaluation 2 to 3 weeks after TKA, there was notable worsening in self-perceived functional ability, functional performance scores, range of motion, and quadriceps strength symmetry compared to preoperative status (TABLE 1). However, at discharge from physical therapy (average, 3 months after TKA), the mean Knee Outcome Survey scores increased by 83% and 110% relative to preoperative and initial-evaluation values, respectively. Additionally, all clinical metrics were as good as or better than preoperative values, and all patients had TUG, SCT, and 6MW scores greater than the MDC, except for 2 patients for the TUG. Between 3 months and 6 months after TKA, mean 6MW distance increased by 96 m, and there was a 4.2-second decrease in mean SCT scores. There was also an increase of 9.5% in the QI between 3 months and 6 months.
TABLE 1.
Functional Data for the Symmetry-Training and Standard-of-Care Groups*
| Symmetry Training (n = 11) | Standard of Care (n = 11) | |||||
|---|---|---|---|---|---|---|
| Presurgery | Initial Postoperative Outpatient PT Evaluation |
3 mo Postsurgery | 6 mo Postsurgery | 6 mo Postsurgery | Effect Size† | |
| KOS, % | 46 ± 20 | 40 ± 14 | 84 ± 9 | 84 ± 10 | 86 ± 10 | 0.20 |
| Flexion ROM, deg | 122 ± 23 | 89 ± 12 | 123 ± 6 | 125 ± 9 | 119 ± 7 | 0.78 |
| TUG, s | 8.7 ± 2.3 | 13.8 ± 5.2 | 8.5 ± 2.2 | 8.1 ± 2.1 | 7.6 ± 1.8 | 0.26 |
| SCT, s | 18.3 ± 8.8 | 34.1 ± 15.7 | 16.7 ± 5.6 | 12.4 ± 4.6 | 12.1 ± 3.3 | 0.08 |
| 6MW, m | 500 ± 142 | 341 ± 100 | 531 ± 90 | 627 ± 141 | 564 ± 85 | 0.54 |
| Quadriceps index, % | 81 ± 22 | 24 ± 14 | 81 ± 17 | 85 ± 20 | 79 ± 20 | 0.30 |
Abbreviations: 6MW, 6-minute walk test; KOS, Knee Outcome Survey; PT, physical therapy; ROM, range of motion; SCT, stair-climbing test; TUG, timed up-and-go test.
Values are mean ± SD except for effect size.
Calculated between the symmetry group and the standard-of-care group at the 6-mo post–total knee arthroplasty time point.
Between-Group Analysis 6 Months Post-TKA
Six months after TKA, patients in the symmetry group had similar or greater clinical scores, particularly for knee strength side-to-side symmetry (85% versus 79%), knee flexion range of motion (125° versus 119°), and the 6MW (627 m versus 564 m), compared to the standard-of-care group. The effect sizes for knee flexion and the 6MW were moderate (0.78 and 0.54, respectively), and the effect size for the QI was small (0.30) (TABLE 1).
Chair-Rise Biomechanics
Longitudinal Analysis for Symmetry Group
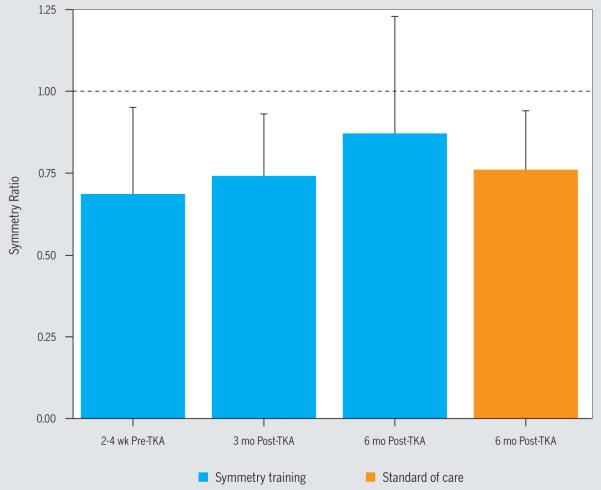
Patients in the symmetry group improved interlimb symmetry across time for all outcome variables. Mean ± SD VGRF symmetry ratios during STS were 0.86 ± 0.15, 0.93 ± 0.17, and 1.02 ± 0.15 before surgery, 3 months postsurgery, and 6 months postsurgery, respectively. For standing, mean ± SD VGRF symmetry ratios were 0.86 ± 0.11, 0.98 ± 0.21, and 1.01 ± 0.19, respectively. During RTS, mean ± SD VGRF symmetry ratios were 0.86 ± 0.11, 1.02 ± 0.12, and 1.06 ± 0.11 for each time point, respectively (FIGURE 1). For PEKFM, mean ± SD symmetry ratios were 0.67 ± 0.28, 0.74 ± 0.19, and 0.87 ± 0.36, respectively (FIGURE 2). The symmetry ratio of VGRF from before surgery to 3 months after surgery improved 8% during STS, 18% while standing, and 14% during RTS. The PEKFM symmetry ratio, which was evaluated during the STS portion, improved 10% compared to preoperative values. From 3-month to 6-month follow-up, the interlimb symmetry ratio of VGRF improved 10% during STS, 4% during standing, and 3% during RTS. The PEKFM symmetry ratio also improved 18% over these 3 months.
FIGURE 1.
Mean ± SD interlimb symmetry ratio of vertical ground reaction force for the symmetry-training (pre-TKA, 3 months post-TKA, and 6 months post-TKA; n = 11) and standard-of-care (6 months post-TKA; n = 11) groups during the sit-to-stand, standing, and return-to-sit portions of the chair-rise task. Symmetry ratio was calculated as the mean vertical ground reaction force on the surgical limb divided by the mean vertical ground reaction force on the nonsurgical limb. Abbreviation: TKA, total knee arthroplasty.
FIGURE 2.
Mean ± SD interlimb symmetry ratio of peak external knee flexion moment, reflective of knee extensor torque requirements, during sit-to-stand for the symmetry group (pre-TKA, 3 months post-TKA, and 6 months post-TKA; n = 11) and standard-of-care group (6 months post-TKA; n = 11). Symmetry ratio was calculated as the peak external knee flexion moment on the surgical limb divided by the peak external knee flexion moment on the nonsurgical limb. Abbreviation: TKA, total knee arthroplasty.
Between-Group Analysis 6 Months Post-TKA
Individuals in the symmetry group demonstrated greater interlimb symmetry compared to the standard-of-care group 6 months after TKA (FIGURES 1 and 2). A greater percentage of patients in the symmetry group also had symmetry ratios greater than 90% (TABLE 2). The mean differences in symmetry ratios of VGRF during STS, standing, and RTS were 7%, 8%, and 10% between groups, with the symmetry group having greater values. The symmetry group also had 14% greater symmetry in PEKFM 6 months after TKA compared to the standard-of-care group.
TABLE 2.
Percentage of Patients With Symmetry Ratios* Greater Than or Equal to 0.90 and Less Than 0.90 During the Chair-Rise Task
| VGRF Sit-to-Stand Portion, % | VGRF Standing Portion, % | VGRF Return-to-Sit Portion, % | PEKFM During Sit-to-Stand, % | |||||
|---|---|---|---|---|---|---|---|---|
| Group/Time Point | ≥0.90 | <0.90 | ≥0.90 | <0.90 | ≥0.90 | <0.90 | ≥0.90 | <0.90 |
| Symmetry | ||||||||
| Pre-TKA | 56 | 44 | 44 | 56 | 44 | 56 | 11 | 89 |
| 3 mo post-TKA | 44 | 56 | 67 | 33 | 67 | 33 | 22 | 78 |
| 6 mo post-TKA | 91 | 9 | 82 | 18 | 82 | 18 | 27 | 73 |
| Standard of care | ||||||||
| 6 mo post-TKA | 64 | 36 | 64 | 36 | 64 | 36 | 18 | 82 |
Abbreviations: PEKFM, peak external knee flexion moment; TKA, total knee arthroplasty; VGRF, vertical ground reaction force.
Symmetry ratio was calculated as the surgical limb divided by the nonsurgical limb.
Gait Biomechanics
Longitudinal Analysis for Symmetry Group
Prior to TKA, patients in the symmetry group demonstrated asymmetrical external knee flexion moments during walking. These asymmetries were mostly resolved at discharge from physical therapy (FIGURE 3).
FIGURE 3.
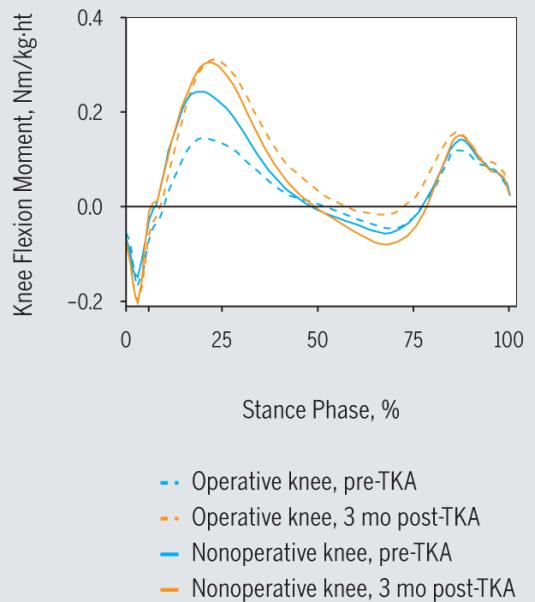
Average external knee flexion moment (positive values are external flexion moment) during the stance phase of gait for the operated knee and nonoperated knee for the symmetry-training group. Abbreviations: ht, height; TKA, total knee arthroplasty.
Between-Group Analysis 6 Months Post-TKA
Compared to the standard-of-care group, patients who received symmetry training demonstrated more symmetrical knee flexion angles and more symmetrical external knee flexion moments, particularly at the end of midstance (FIGURES 4 and 5). The ensemble average of the external sagittal plane knee moment on the operated limb of the symmetry group demonstrated a biphasic pattern 6 months after TKA, whereas that moment in the standard-of-care group remained positive, which represents persistent external knee flexion moment throughout midstance (FIGURE 5).
FIGURE 4.
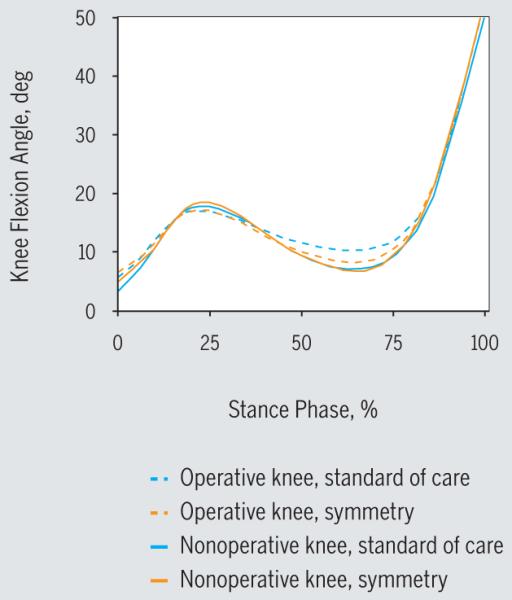
Average knee flexion angle during the stance phase of gait 6 months post–total knee arthroplasty for the operated knee and nonoperated knee.
FIGURE 5.
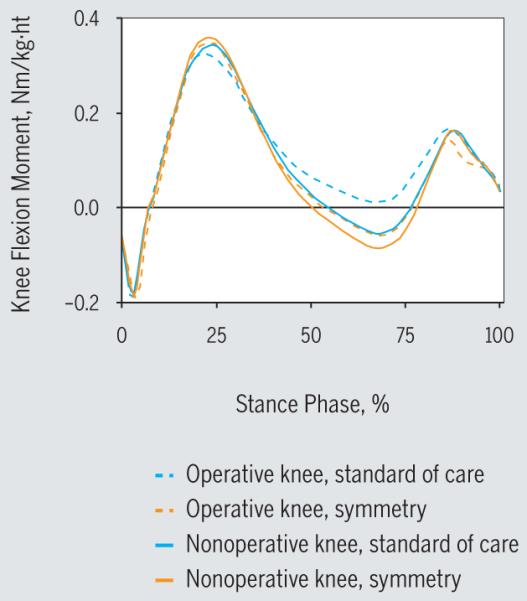
Average external sagittal knee moment (positive values are external flexion moment) during the stance phase of gait for the operated knee and nonoperated knee 6 months after total knee arthroplasty. Abbreviation: ht, height.
DISCUSSION
The symmetry rehabilitation protocol was well tolerated by patients, produced functional outcomes that were equivalent or superior to a progressive strengthening protocol, and was easily implemented by our outpatient physical therapy facility. No patients experienced adverse events that were attributable to the protocol. Our hypotheses were supported, and patients who underwent the symmetry retraining protocol demonstrated improved kinetic and kinematic symmetry during gait and a chair-rise task compared to preoperative status. These preliminary results suggest that including symmetry retraining may also improve interlimb kinematic and kinetic symmetry to a greater extent than progressive strengthening alone.
The functional performance of patients who received symmetry training was on the upper end of what has been previously reported for these metrics.3,6,24 In this study, TUG time, SCT time, and 6MW distance at 3 months and 6 months after TKA were consistent with or surpassed previously reported outcomes (TABLES 1 and 3).3,24 TUG time was slightly longer for the symmetry group than for the standard-of-care group at 6 months, although the mean difference (0.5 seconds) was less than the MDC for this measure and would likely not be clinically meaningful.1 At the 6-month time point, patients in the symmetry group required similar time to the standard-of-care group to perform the SCT, but walked 63 m farther than the standard-of-care group, which exceeded the MDC for this measure.11 The patients who participated in the symmetry protocol had more symmetrical quadriceps strength than the standard-of-care group (higher QI), as well as active knee flexion range of motion that was 6° greater than the standard-of-care group and 12° to 26° greater than previously reported normal values 6 months after TKA.3,10
TABLE 3.
Functional Data From Previous and Current Studies*
| TUG, s | SCT, s | 6MW, m | |||||
|---|---|---|---|---|---|---|---|
| Study | n | 3 mo Post-TKA | 6 mo Post-TKA | 3 mo Post-TKA | 6 mo Post-TKA | 3 mo Post-TKA | 6 mo Post-TKA |
| Bade et al3 | 24 | 9.7 ± 2.7 | 9.1 ± 2.4 | 18.8 ± 8.4 | 18.2 ± 10.1 | 412.9 ± 110 | 432.6 ± 107 |
| Stevens-Lapsley et al24 | 39 | 8.46 ± 0.5 | 7.92 ± 0.41 | 16.05 ± 1.5 | 14.25 ± 1.3 | 459 ± 18 | 473 ± 18 |
| Present study | 11 | 8.5 ± 2.2 | 8.1 ± 2.1 | 16.7 ± 5.6 | 12.4 ± 4.6 | 531 ± 90 | 627 ± 141 |
Abbreviations: 6MW, 6-minute walk test; SCT, stair-climbing test; TKA, total knee arthroplasty; TUG, timed up-and-go test.
Values are mean ± SD.
Compared to preoperative values, patients in the symmetry group demonstrated clinically meaningful improvements in kinematic and kinetic symmetry during walking, standing, and rising from a chair. These improvements were apparent at discharge from physical therapy and persisted 6 months after TKA. During walking, patients who underwent symmetry retraining demonstrated sagittal plane knee moments that were not only more symmetrical but were also similar to the typical biphasic sagittal knee moments observed in individuals without lower extremity pathology. Patients in the standard-of-care group did not demonstrate an external knee extension moment at the end of midstance, which may be attributed to the lack of knee extension motion in the operated limb during this phase. During midstance, patients in the standard-of-care group maintained their knee in a more flexed position (10.8°) compared to the symmetry group (6.8°). It should also be noted that for biomechanical symmetry during STS (FIGURES 1 and 2, TABLE 2), the standard-of-care group at 6 months after TKA was similar to the symmetry group 3 months after TKA. The symmetry group showed improvements between 3 and 6 months, which may reflect carryover into daily life after discharge from therapy. This would be consistent with a treatment approach that encouraged and reinforced symmetrical movement patterns for all daily activities, with the intention of promoting symmetrical movement outside the clinic and after discharge from outpatient physical therapy, as described in the Methods section. Future analyses should include a longer-term follow-up.
Despite biomechanical improvements, asymmetries persisted in the sagittal plane knee moment during the chair-rise task for both groups. Although the patients in the symmetry group had a 14% better symmetry ratio for the PEKFM during STS compared to the standard-of-care group, they still had an average value that was lower than 1.0, suggesting a disuse of the operated limb during this dynamic task. The STS task requires greater joint excursions in the knee and greater vertical translation of the center of mass. Because it is a challenging but bilateral task, there is greater likelihood that patients may compensate by using the nonoperated limb. This may explain the higher asymmetry in knee flexion moment in all groups during this task. While it is likely that the biofeedback contributed to the improvements in movement symmetry, there was a large amount of variability, suggesting that some individuals responded better to the protocol than others. Identifying patient characteristics that may increase response to symmetry training may lead to improved outcomes and allow for patient-specific rehabilitation protocols.
Several limitations exist in this preliminary study. Although we compared 6-month outcomes in our symmetry group to a cross-sectional sample, we are not able to draw conclusions about differences between groups with respect to change over time. In addition, our standard-of-care group might have included higher-functioning patients who were willing to travel to the laboratory to participate in the functional and motion analysis testing. Although we evaluated the biomechanics of rising from a chair and walking, there are many other challenging dynamic tasks that patients perform on a daily basis. Future outcomes should include additional variables, such as stair climbing or curb descent, to capture unilateral stance activities that require a larger vertical displacement of the center of mass and therefore place greater demands on the lower extremity. We were also not able to assess rate of progression in the program and factors that influenced how fast patients were able to meet symmetry or strength milestones. These important factors should be considered in future longitudinal studies.
Although we demonstrated preliminary success with this program, some methodological improvements could be made in this rehabilitation paradigm. Although the biofeedback used during the leg-press exercise (SymSlide) was beneficial, it required expensive, customized equipment. It may be possible to reduce equipment costs by equipping existing leg-press devices with the pressure sensor (Wii Balance Board) to monitor force during this activity. Improved, objective feedback during gait symmetry retraining would be beneficial and may have better transfer to symmetrical walking activity outside the clinic. Although the therapist cued the patients to walk more symmetrically and patients walked on a treadmill in front of a mirror, the use of a metronome or other auditory device to synchronize temporospatial values may prove valuable during this task.26 Feedback throughout this program consisted of constant feedback on performance. We did not include a faded-feedback design, which has been successful in retraining normal movement and lower extremity loading patterns during running.5,7,18 These methodological changes may improve subsequent retraining programs and should be tested using a long-term follow-up to determine if such a program can fully restore movement symmetry and truly reduce symptomatic or radiographic progression of OA in the contralateral joints.
CONCLUSION
The functional and biomechanical recovery seen in patients who participated in the symmetry paradigm is encouraging. Adding symmetry retraining to postoperative protocols is clinically viable, safe, and may provide additional benefits beyond those provided by rehabilitation protocols that focus on range of motion, strength, and return to independence. Future randomized controlled trials are needed to determine if symmetry retraining can better restore normal symmetrical movement patterns, reduce reliance on the nonoperated limb, and ultimately reduce the risk for contralateral knee OA or TKA. Based on the preliminary data from this study, we plan to conduct a randomized control trial to test this protocol in a larger sample, using commercially available equipment, as well as to make the custom software available for clinical use. Identifying effective, low-cost, and generalizable rehabilitation paradigms will be critical to ensure that the rapidly increasing number of individuals who undergo TKA receive optimal postoperative care.
KEY POINTS.
FINDINGS
The results of this study suggest that the addition of tasks focusing on interlimb symmetry to a standard-of-care program following TKA may lead to improved biomechanical symmetry during functional tasks.
IMPLICATIONS
Clinicians may want to consider incorporating a similar protocol to improve biomechanical outcomes in a variety of patient populations.
CAUTION
Based on study design, we cannot draw definitive conclusions pertaining to effectiveness until randomized clinical trials are completed.
Acknowledgments
Funding for this work was supported by the National Institutes of Health: P20RR16458-S1 and K12HD055931. All interventions and testing procedures were approved by the Human Subjects Review Board at the University of Delaware. The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article.
APPENDIX. PHYSICAL THERAPY TREATMENT REGIMEN: SYMMETRY-TRAINING PROTOCOL
| Stage | Focus of Treatment |
Treatment | Milestones |
|---|---|---|---|
| 1 (typically visits 1-6; 3-6 weeks post-TKA) |
ROM |
|
|
| NMES |
|
|
|
| Volitional strength |
|
|
|
| Gait retraining |
|
|
|
| SymSlide | Exercise 1: targets
Exercise 2: balanced knee extension
|
|
|
| Standing balance |
|
|
|
| 2 (typically visits 7-12; 5-8 weeks post-TKA) |
ROM |
|
|
| NMES |
|
||
| Volitional strength |
|
|
|
| Gait retraining |
|
|
|
| Sit-to-stand |
|
|
|
| Squats on bal- ance board |
|
|
|
| Stair ascent |
|
|
|
| Stair descent |
|
|
|
| 3 (typically visits 13-18; 7-10 weeks post-TKA) |
ROM |
|
|
| NMES |
|
|
|
| Volitional strength |
|
|
|
| Sit-to-stand |
|
|
|
| Stair ascent |
|
|
|
| Stair descent |
|
|
- Pain and swelling: ice, compression, and elevation daily after exercises
- Incision mobility: soft tissue mobilizations to entire length of incision, with greater emphasis on distal one third of incision until incision moves freely over subcutaneous tissue
- Vital signs: monitored during each session
- NMES protocol guidelines: electrodes placed over proximal lateral quadriceps and distal medial quadriceps and knee flexed to 75°. Parameters: 2500 Hz, 75 bursts, 2-second ramp, 12 seconds on, 50 seconds off, intensity to maximum tolerable or at least 30% of the MVIC, 10 contractions (active plus NMES) per session until quadriceps index is 70%.
Abbreviations: MVIC, maximal voluntary isometric contraction; NMES, neuromuscular electrical stimulation; RM, repetition maximum; ROM, range of motion; SAQ, short-arc quadriceps exercise; SLR, straight leg raise; TKA, total knee arthroplasty.
REFERENCES
- 1.Almeida GJ, Schroeder CA, Gil AB, Fitzgerald GK, Piva SR. Interrater reliability and validity of the stair ascend/descend test in subjects with total knee arthroplasty. Arch Phys Med Rehabil. 2010;91:932–938. doi: 10.1016/j.apmr.2010.02.003. http://dx.doi.org/10.1016/j.apmr.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alnahdi AH, Zeni JA, Snyder-Mackler L. Gait after unilateral total knee arthroplasty: frontal plane analysis. J Orthop Res. 2011;29:647–652. doi: 10.1002/jor.21323. http://dx.doi.org/10.1002/jor.21323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes before and after total knee arthroplasty compared to healthy adults. J Orthop Sports Phys Ther. 2010;40:559–567. doi: 10.2519/jospt.2010.3317. http://dx.doi.org/10.2519/jospt.2010.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bade MJ, Stevens-Lapsley JE. Early high-intensity rehabilitation following total knee arthroplasty improves outcomes. J Orthop Sports Phys Ther. 2011;41:932–941. doi: 10.2519/jospt.2011.3734. http://dx.doi.org/10.2519/jospt.2011.3734. [DOI] [PubMed] [Google Scholar]
- 5.Barrios JA, Crossley KM, Davis IS. Gait retraining to reduce the knee adduction moment through real-time visual feedback of dynamic knee alignment. J Biomech. 2010;43:2208–2213. doi: 10.1016/j.jbiomech.2010.03.040. http://dx.doi.org/10.1016/j.jbiomech.2010.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christiansen CL, Bade MJ, Judd DL, Stevens-Lapsley JE. Weight-bearing asymmetry during sit-stand transitions related to impairment and functional mobility after total knee arthroplasty. Arch Phys Med Rehabil. 2011;92:1624–1629. doi: 10.1016/j.apmr.2011.05.010. http://dx.doi.org/10.1016/j.apmr.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crowell HP, Davis IS. Gait retraining to reduce lower extremity loading in runners. Clin Biomech (Bristol, Avon) 2011;26:78–83. doi: 10.1016/j.clinbiomech.2010.09.003. http://dx.doi.org/10.1016/j.clinbiomech.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Finch E, Walsh M, Thomas SG, Woodhouse LJ. Functional ability perceived by individuals following total knee arthroplasty compared to age-matched individuals without knee disability. J Orthop Sports Phys Ther. 1998;27:255–263. doi: 10.2519/jospt.1998.27.4.255. [DOI] [PubMed] [Google Scholar]
- 9.Impellizzeri FM, Mannion AF, Leunig M, Bizzini M, Naal FD. Comparison of the reliability, responsiveness, and construct validity of 4 different questionnaires for evaluating outcomes after total knee arthroplasty. J Arthroplasty. 2011;26:861–869. doi: 10.1016/j.arth.2010.07.027. http://dx.doi.org/10.1016/j.arth.2010.07.027. [DOI] [PubMed] [Google Scholar]
- 10.Jones CA, Voaklander DC, Suarez-Alma ME. Determinants of function after total knee arthroplasty. Phys Ther. 2003;83:696–706. [PubMed] [Google Scholar]
- 11.Kennedy DM, Stratford PW, Wessel J, Gollish JD, Penney D. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord. 2005;6:3. doi: 10.1186/1471-2474-6-3. http://dx.doi.org/10.1186/1471-2474-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kneiss JA, Houck JR, Bukata SV, Puzas JE. Influence of upper extremity assistance on lower extremity force application symmetry in individuals post-hip fracture during the sit-to-stand task. J Orthop Sports Phys Ther. 2012;42:474–481. doi: 10.2519/jospt.2012.3562. http://dx.doi.org/10.2519/jospt.2012.3562. [DOI] [PubMed] [Google Scholar]
- 13.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. http://dx.doi.org/10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 14.Lugade V, Wu A, Jewett B, Collis D, Chou LS. Gait asymmetry following an anterior and anterolateral approach to total hip arthroplasty. Clin Biomech (Bristol, Avon) 2010;25:675–680. doi: 10.1016/j.clinbiomech.2010.05.003. http://dx.doi.org/10.1016/j.clinbiomech.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 15.Mandeville D, Osternig LR, Chou LS. The effect of total knee replacement on dynamic support of the body during walking and stair ascent. Clin Biomech (Bristol, Avon) 2007;22:787–794. doi: 10.1016/j.clinbiomech.2007.04.002. http://dx.doi.org/10.1016/j.clinbiomech.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 16.McClelland J, Zeni J, Haley RM, Snyder-Mackler L. Functional and biomechanical outcomes after using biofeedback for retraining symmetrical movement patterns after total knee arthroplasty: a case report. J Orthop Sports Phys Ther. 2012;42:135–144. doi: 10.2519/jospt.2012.3773. http://dx.doi.org/10.2519/jospt.2012.3773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mizner RL, Snyder-Mackler L. Altered loading during walking and sit-to-stand is affected by quadriceps weakness after total knee arthroplasty. J Orthop Res. 2005;23:1083–1090. doi: 10.1016/j.orthres.2005.01.021. http://dx.doi.org/10.1016/j.orthres.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 18.Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2011;45:691–696. doi: 10.1136/bjsm.2009.069112. http://dx.doi.org/10.1136/bjsm.2009.069112. [DOI] [PubMed] [Google Scholar]
- 19.Norén AM, Bogren U, Bolin J, Stenström C. Balance assessment in patients with peripheral arthritis: applicability and reliability of some clinical assessments. Physiother Res Int. 2001;6:193–204. doi: 10.1002/pri.228. [DOI] [PubMed] [Google Scholar]
- 20.Parent E, Moffet H. Comparative responsiveness of locomotor tests and questionnaires used to follow early recovery after total knee arthroplasty. Arch Phys Med Rehabil. 2002;83:70–80. doi: 10.1053/apmr.2002.27337. [DOI] [PubMed] [Google Scholar]
- 21.Petterson SC, Mizner RL, Stevens JE, et al. Improved function from progressive strengthening interventions after total knee arthroplasty: a randomized clinical trial with an imbedded prospective cohort. Arthritis Rheum. 2009;61:174–183. doi: 10.1002/art.24167. http://dx.doi.org/10.1002/art.24167. [DOI] [PubMed] [Google Scholar]
- 22.Rejeski WJ, Ettinger WH, Jr., Schumaker S, James P, Burns R, Elam JT. Assessing performance-related disability in patients with knee osteoarthritis. Osteoarthritis Cartilage. 1995;3:157–167. doi: 10.1016/s1063-4584(05)80050-0. [DOI] [PubMed] [Google Scholar]
- 23.Stevens-Lapsley JE, Balter JE, Wolfe P, Eckhoff DG, Kohrt WM. Early neuromuscular electrical stimulation to improve quadriceps muscle strength after total knee arthroplasty: a randomized controlled trial. Phys Ther. 2012;92:210–226. doi: 10.2522/ptj.20110124. http://dx.doi.org/10.2522/ptj.20110124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stevens-Lapsley JE, Schenkman ML, Dayton MR. Comparison of self-reported knee injury and osteoarthritis outcome score to performance measures in patients after total knee arthroplasty. PM R. 2011;3:541–549. doi: 10.1016/j.pmrj.2011.03.002. quiz 549. http://dx.doi.org/10.1016/j.pmrj.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Talis VL, Grishin AA, Solopova IA, Oskanyan TL, Belenky VE, Ivanenko YP. Asymmetric leg loading during sit-to-stand, walking and quiet standing in patients after unilateral total hip replacement surgery. Clin Biomech (Bristol, Avon) 2008;23:424–433. doi: 10.1016/j.clinbiomech.2007.11.010. http://dx.doi.org/10.1016/j.clinbiomech.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 26.Thielman G. Rehabilitation of reaching post-stroke: a randomized pilot investigation of tactile versus auditory feedback for trunk control. J Neurol Phys Ther. 2010;34:138–144. doi: 10.1097/NPT.0b013e3181efa1e8. http://dx.doi.org/10.1097/NPT.0b013e3181efa1e8. [DOI] [PubMed] [Google Scholar]
- 27.United States Bone and Joint Decade . The Burden of Musculoskeletal Diseases in the United States: Executive Summary. American Academy of Orthopaedic Surgeons; Rosemont, IL: 2008. [Google Scholar]
- 28.Walsh M, Woodhouse LJ, Thomas SG, Finch E. Physical impairments and functional limitations: a comparison of individuals 1 year after total knee arthroplasty with control subjects. Phys Ther. 1998;78:248–258. doi: 10.1093/ptj/78.3.248. [DOI] [PubMed] [Google Scholar]