Abstract
In 2012, it was estimated that 9180 people in the United States would die from melanoma and that more than 76,000 new cases would be diagnosed. Surgical resection is effective for early-stage melanoma, but outcomes are poor for patients with advanced disease. Expression of tumor-associated antigens by melanoma cells makes the disease a promising candidate for immunotherapy. The hematopoietic cytokine granulocyte–macrophage colony-stimulating factor (GM-CSF) has a variety of effects on the immune system including activation of T cells and maturation of dendritic cells, as well as an ability to promote humoral and cell-mediated responses. Given its immunobiology, there has been interest in strategies incorporating GM-CSF in the treatment of melanoma. Preclinical studies with GM-CSF have suggested that it has antitumor activity against melanoma and can enhance the activity of anti-melanoma vaccines. Numerous clinical studies have evaluated recombinant GM-CSF as a monotherapy, as adjuvant with or without cancer vaccines, or in combination with chemotherapy. Although there have been suggestions of clinical benefit in some studies, results have been inconsistent. More recently, novel approaches incorporating GM-CSF in the treatment of melanoma have been evaluated. These have included oncolytic immunotherapy with the GM-CSF–expressing engineered herpes simplex virus talimogene laherparepvec and administration of GM-CSF in combination with ipilimumab, both of which have improved patient outcomes in phase 3 studies. This review describes the diverse body of preclinical and clinical evidence regarding use of GM-CSF in the treatment of melanoma.
Keywords: Granulocyte macrophage-colony stimulating factor, GM-CSF, Melanoma, Cellular immunotherapy
Introduction
In 2012, it was estimated that 9180 people in the United States would die from melanoma and more than 76,000 new cases would be diagnosed [1]. The primary treatment for melanoma, excision of the malignancy, is highly effective in early-stage disease but is not a meaningful option for metastatic disease except in patients with solitary metastases or limited-volume disease [2]. For patients with advanced disease, cytotoxic chemotherapy has a limited role and curative potential in <1% of patients. For BRAF-mutant patients, treatment with vemurafenib, dabrafenib, and/or tremetinib have high rates of objective response, but median duration of response is typically ~6–8 months, after which rapid disease progression is common [2]. However, some patients with melanoma respond to immunotherapy with durable responses, and thus immunotherapy shows substantial promise for further improving durable control of advanced melanoma.
Expression of tumor-associated antigens by melanoma cells makes the disease a promising candidate for immunotherapy [3]. The potential for immunotherapy in melanoma has been demonstrated by improved outcomes among patients with stage III melanoma receiving interferon-α2b [4] and patients with metastatic melanoma receiving the anti-cytotoxic T-lymphocyte antigen 4 (CTLA-4) antibody ipilimumab alone or in combination with a gp100 peptide vaccine or dacarbazine [5,6], as well as by durable complete responses with high-dose interleukin-2 [7] and high response rates after adoptive T cell transfer therapies [8].
The hematopoietic cytokine granulocyte–macrophage colony-stimulating factor (GM-CSF) has been investigated as a monotherapy, and as a component of combination therapies for melanoma. Preclinical evidence has suggested that GM-CSF may have antitumor effects, but results from clinical trials evaluating GM-CSF present a complex picture. This review evaluates evidence regarding use of GM-CSF in melanoma and potential future strategies in this setting.
Review
Immunobiology of GM-CSF
GM-CSF was identified as a factor responsible for expansion and activation of granulocytes and macrophages, but has since been found to have many direct and indirect effects on multiple cell types, including cell proliferation, maturation, and survival (Figure 1A) [9]. GM-CSF plays a critical role in development and maturation of dendritic cells (DCs) and proliferation and activation of T cells, linking the innate and acquired immune response [10]. In mice, increased numbers of eosinophils, monocytes, macrophages, and lymphocytes were observed in the draining lymph node in response to treatment with irradiated melanoma cells expressing GM-CSF, resulting in a sustained antitumor response [11]. GM-CSF has also been shown to favor expansion of DC1 populations [12,13] and to increase DC-mediated responses to tumor cells (Figure 1B) [14]. In vitro studies using human myeloid leukemia cells suggest that, in addition to promoting antigen presentation, GM-CSF directs these cells toward a DC phenotype [15,16]. The role of GM-CSF in neutrophil proliferation and survival led to its use in amelioration of neutropenia following induction chemotherapy in elderly patients with acute myeloid leukemia [17].
Figure 1.
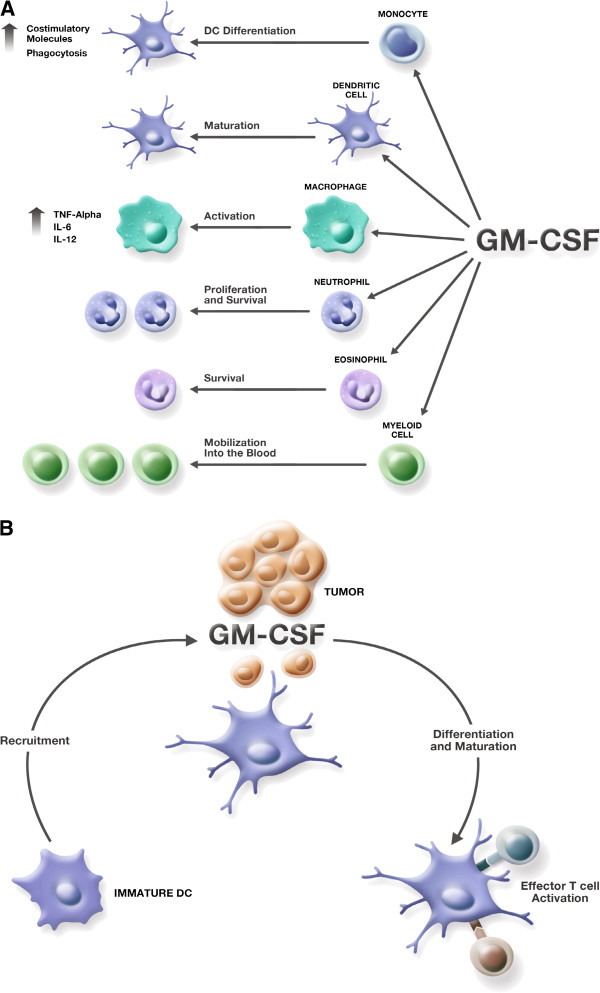
Immunobiologic effects of GM-CSF. (A) Effects of GM-CSF on cells of the immune system. (B) Effects of GM-CSF on dendritic cells and T cells in the tumor microenvironment.
Studies evaluating GM-CSF in preclinical models of melanoma
The immune adjuvant properties of GM-CSF led to numerous preclinical studies assessing the ability of GM-CSF to inhibit tumor growth and/or mediate tumor regression. In a seminal study, a panel of recombinant retroviral vectors expressing various cytokines, co-stimulatory molecules, or adhesion molecules were used to infect murine B16 melanoma cells. Infected cells were then irradiated and injected subcutaneously into immune-competent hosts, followed by a subsequent challenge with wild-type B16 cells [11]. The GM-CSF–secreting tumor vaccines conveyed 90% protection, whereas vaccines expressing interleukin-2 and interferon-γ failed to mediate antitumor protection [11]. Additionally, analysis of the vaccination site revealed an influx of dividing monocytes and granulocytes, with a coincident increase in lymphocytes in tumor-draining lymph nodes, suggesting direct augmentation of antigen presentation and T-cell priming against the tumor [11].
Exogenously administered GM-CSF has been shown to augment antitumor immunity Mice immunized with an HIV envelope peptide vaccine plus GM-CSF exhibited increased cytotoxic T lymphocyte (CTL) activity compared with vaccine alone or vaccine with interleukin-2 [18]. Studies using a tumor-associated antigen vaccine (neu), in combination with GM-CSF, produced increased neu-specific antibodies alongside an enhanced CTL response [19,20]. However, tumor protection was ultimately dependent on a cell-mediated response since depletion of CD8+ T cells abrogated tumor regression.
Genetically modified vaccines can generate protective anti-melanoma immune responses in animal models [21]. B16 tumor lines expressing bioactive levels of murine GM-CSF have been generated and assessed [11,21,22]. Levels of GM-CSF at the site of GM-CSF–expressing tumor transplantation remain elevated for days, whereas GM-CSF dissipated rapidly after injection of irradiated tumor with recombinant GM-CSF [22]. The pharmacokinetic longevity associated with the vaccine correlated with both increased DC infiltration and tumor protection against wild-type tumors [22].
Oncolytic immunotherapy with modified herpes simplex viruses (HSV) and vaccinia viruses expressing GM-CSF have also shown promise. These vectors have elicited tumor responses in mice when injected directly into tumor lesions [23-25]. In a murine melanoma model, a temperature-sensitive strain of HSV encoding murine GM-CSF significantly reduced Harding-Passey melanoma tumor growth and improved survival of tumor-bearing mice [25]. Similarly, preclinical studies demonstrated a potent lytic effect against lesions injected with the GM-CSF–expressing oncolytic HSV talimogene laherparepvec (T-VEC; formerly OncovexGM-CSF) [26]. Notably, when virus expressing GM-CSF was employed, regression of uninjected, distant lesions was enhanced compared with a regression observed with a control virus not expressing GM-CSF.
The combination of GM-CSF–secreting tumor vaccines with other immunotherapies is another potentially promising approach. Antibodies that block the co-inhibitory T-cell molecules CTLA-4 and PD-1 plus GM-CSF have boosted immune responses against melanomas [5,27-31]. Additionally, activation of co-stimulatory molecules (CD80, CD86, CD137), exogenous cytokine administration (interleukin-2, interferon-γ), and blockade of tumor angiogenesis can inhibit melanoma progression when combined with GM-CSF–expressing vaccines [32-36]. These preclinical studies strongly suggest that the combination of GM-CSF–based tumor vaccines with immunomodulatory agents has potential for clinical use.
Clinical trials evaluating exogenously administered GM-CSF in patients with melanoma
Given the evidence of antitumor activity in preclinical models of melanoma, there has been interest in using GM-CSF to improve outcomes in the clinical setting. Numerous studies have evaluated use of recombinant GM-CSF in completely resected stage III/IV melanoma patients. Data from these studies, however, have been inconsistent.
GM-CSF as an adjuvant therapy
GM-CSF has been evaluated as an adjuvant, systemic monotherapy following regional lymphadenectomy, to prevent or to delay recurrence in high-risk stage III patients (Table 1). In a phase 2 study, there were statistically significant improvements in survival among patients with stage III/IV disease (P = 0.04 and P < 0.001, respectively) receiving GM-CSF (125 μg/m2 daily for 14 consecutive days in 28-day cycles up to 1 year) compared with historical controls [37]. A subsequent single-arm study using the same dosing regimen evaluated treatment with GM-CSF over 3 years and reported a 5-year survival rate of 60%, with 5-year disease-free survival (DFS) of 67% and 40% for patients with stage III and IV disease, respectively [38]. The effect of GM-CSF on DC has been proposed as a mechanism for supporting antitumor immunity; consistent with this hypothesis, treatment with recombinant GM-CSF has increased mature DCs in melanoma patients [39]. A randomized study of recombinant GM-CSF (125 μg/m2 daily for 14 consecutive days in 28-day cycles) versus placebo in patients with completely resected stage IIIB/IIIC/IV or mucosal melanoma, there was a trend toward improvement in DFS although it did not reach statistical significance (11.5 vs 9.2 months; HR, 0.88; P = 0.14), and no improvement in overall survival (OS; 69.6 vs 62.4 months; HR, 0.96; P = 0.78) [40]. However, an improvement in DFS (HR, 0.74; P = 0.04) and a trend toward improved OS (HR, 0.72; P = 0.07) was observed in stage IV patients (n = 258) [40].
Table 1.
Clinical studies evaluating adjuvant GM-CSF in patients with surgically resected melanoma
| Citation | Evaluable patients | GM-CSF dose schedule | Control | Clinical response |
|---|---|---|---|---|
| Spitler et al. [37] |
48 |
125 μg/m2 for 14 d, 28-d cycles, for 1 y |
Historical |
OS: 37.5 mo |
| Markovic et al. [41] |
70 (Stage IV) 149 (Stage III) |
125 μg/m2 for 14 d, 28-d cycles, for 1 y 125 μg/m2 for 14 d, 28-d cycles, for 1 y |
Observation |
OS: 6.6 y (GM-CSF) vs 6.8 y (control) OS: 8.6 (GM-CSF) vs 5.2 y (control) |
| Isla et al. [42] |
24 |
150 mg/d for 2 y |
None |
DFS at 1 y: 88.8% |
| Elias et al. [43] |
45 |
125 μg/m2 for 14 d, then IL-2 9 × 106 IU/m2 for 4 d,/28-d cycle, ± autologous vaccine |
None |
DFS at 15.9 mo: 60% OS at 21 mo: 64% (21 mo follow-up) |
| Spitler et al. [38] |
98 |
125 μg/m2 for 14 d, 28-d cycles, for 3 y |
None |
DFS: 1.4 y 5-y survival: 60% |
| Lawson et al. [40] | 743 | 250 μg/m2 for 14 d, 28-d cycles, for 1 y | Placebo | OS: 62.4 mo for placebo vs. 69.6 mo for GM-CSF (HR, 0.96) DFS: 9.2 mo for placebo vs. 11.5 mo for GM-CSF (HR, 0.88) |
DFS = disease-free survival; GM-CSF = granulocyte-macrophage colony-stimulating factor; HR = hazard ratio; IL-2 = interleukin-2; OS = overall survival.
GM-CSF as intratumoral monotherapy
Several small studies have evaluated GM-CSF administered as a monotherapy by direct injection into metastatic lesions (Table 2). Clinical responses in two of these studies were modest, with only one partial response (PR) and no complete response (CR) reported [44,45]. In contrast, a study using perilesional injection of GM-CSF (400 μg/d over 5 days) to treat metastatic melanoma described reduced lesion size in 6/7 patients and a reduction in cutaneous metastases in 5/7 patients [46]. Three patients were still alive at 5-years follow-up; a fourth died tumor-free at age 93. In these studies, there was evidence of increases in DC and T-cell counts and infiltration at injected sites, and in some cases at uninjected sites, suggesting an immunologic effect of GM-CSF injection [44-46]. Other studies using novel methods (such as aerosolization and immunoembolization) to delivering GM-CSF to melanoma metastases at sites that are not readily injectable have met with mixed results (Table 2) [47-50].
Table 2.
Studies evaluating GM-CSF as a monotherapy in patients with advanced melanoma
| Citation | Evaluable patients | GM-CSF dose schedule | Route of administration | Clinical response | Observations |
|---|---|---|---|---|---|
| Si et al. [44] |
13 |
15–50 μg/lesion at 2 sites per patient |
Intralesional |
1 PR, 8 SD |
Responding patients had increased T-cell and Langerhans cell infiltration of the tumor |
| Site 1: 5 times daily | |||||
| Site 2: 5 times daily then once weekly for 6 mo | |||||
| Nasi et al. [45] |
16 |
10, 20, 40, or 80 μg/injection for 10 d |
Intralesional |
3 SD |
Significant increase in DCs and T cells at injection sites |
| Vaquerano et al. [51] |
1 |
500 μg/d for 4 d, monthly |
Intralesional |
1 PR |
Regression of melanoma cells |
| Hoeller et al. [46] |
7 |
400 μg/d for 5 d, 21-d cycle |
Perilesional |
6 with reduced lesion size |
Increased infiltration of monocytes and lymphocytes was observed in injected and systemic sites |
| Ridolfi et al. [52] |
14 |
150 μg/lesion plus IL-2 3 × 106 IU for 5 d, 21-day cycle |
Intralesional (GM-CSF) Perilesional (IL-2) |
2 PR, 2 MR, 7 SD |
Some evidence of systemic immune activation |
| Rao et al. [47] |
14 |
250 μg twice daily for 7 d on alternating weeks |
Aerosol delivery for lung metastases |
6 SD |
Upregulation of cytotoxic T lymphocytes was observed in peripheral blood |
| Markovic et al. [48] |
35 |
500–2000 μg (250-μg/dose increments) twice daily on days 1–7 and 15–21, over 28 d |
Aerosol delivery for lung metastases |
1 PR, 5 SD |
A trend toward increased immune response was observed with higher doses; MTD was not reached |
| Sato et al. [49] |
31 |
25–2000 μg every 4 wk |
Hepatic artery immunoembolization |
2 CR, 8 PR, 10 SD |
Prolonged PFS correlated with higher GM-CSF doses |
| Eschelman et al. [50] | 52 | 2000 μg every 4 wk | Hepatic artery immunoembolization | 5 PR, 12 SD | Trend toward increased OS with GM-CSF; prolonged OS with GM-CSF in patients with bulky metastases |
CR = complete response; DC = dendritic cell; GM-CSF = granulocyte-macrophage colony-stimulating factor; IL-2 = interleukin-2; MTD = maximum tolerated dose; MR = mixed response; OS = overall survival; PD = progressive disease; PFS = progression free survival; PR = partial response; SD = stable disease.
GM-CSF in combination with chemotherapy
A number of early-phase clinical studies have evaluated GM-CSF in conjunction with chemotherapy (Table 3). These studies were typically small with a single-arm design and used a variety of different drug regimens and dosing schedules; thus, as a whole, they are difficult to interpret. Clinical efficacy in studies varied widely, with response rates ranging from no response to >40% [53-58]. It is worth noting that several of the studies reporting high overall response rates also reported significant increases in T-cell, DC, macrophage, or natural killer–cell populations following treatment [53,55,58]. One study evaluating a chemotherapy regimen of dacarbazine, interferon-α2b, interleukin-2, and tamoxifen with three doses of GM-CSF reported a dose–response effect with increasing exposure to GM-CSF via administration over a greater number of days (P = 0.016) [59].
Table 3.
Studies evaluating GM-CSF in combination with chemotherapy in patients with advanced melanoma
| Citation | Evaluable patients | GM-CSF dose schedule | Other agents | Clinical response |
|---|---|---|---|---|
| Schacter et al. [53] |
40 |
20 μg/m2 once daily for 7 d every 3 wk |
BCNU, CDDP, DTIC, tamoxifen, IFN-α |
9 CR, 11 PR, 2 SD OS:14 mo |
| Gajewski et al. [60] |
7 |
5 μg/kg for 6 d |
DTIC, CDDP, IL-2, IFN-α |
1 CR, 1 PR, 2 MR |
| Gibbs et al. [61] |
60 |
250 μg/m2 for 20 d, 28-d cycle |
TMZ, CDDP, IL-2, IFN-α |
1 CR, 11 PR Median OS: 11 mo |
| Vaughan et al. [59] |
19 |
Arm 1: 450 μg/m2 on days 4, 5, 15, and 16 |
DTIC, CDDP, IL-2, IFN-α, TAM |
2 CR, 4 PR OS: 6.2 mo Trend toward increasing response with higher GM-CSF doses |
|
Arm 2: 450 μg/m2 on days 4, 5, 15, 16; 225 μg/m2 on days 6–10 and 17–21, 28-d cycle | ||||
|
Arm 3: 450 μg/m2 on days 4–10 and 15–21, 28-d cycle | ||||
| Gong et al. [62] |
30 |
5 μg/kg (first 25 patients) or 450 μg/m2 (last 8 patients) for 6 d |
DTIC, CDDP, IL-2, IFN-α |
3 CR, 4 PR, 6 MR, 7 SD Median OS: 15 mo |
| Groenewegen et al. [63] |
31 |
2.5 μg/kg for 10 d |
DTIC, IL-2, IFN-α |
4 CR, 6 PR Median OS: 8 mo 1-y survival: 22% |
| De Gast et al. [64] |
74 |
2.5 μg/kg for 12 d |
TMZ, IL-2, IFN-α |
4 CR, 19 PR, 13 SD OS: 8.3 mo 1-y survival: 41% |
| Smith et al. [65] |
8 |
125 and 250 μg/m2/d for 7 d every 2 wk, 28-d cycle |
IL-2 |
0 CR, 0 PR |
| Fruehauf et al. [54] |
10 |
250 μg/m2 for 11 d |
DOX, VIN |
0 CR, 5 PR Median time to progression: 8 mo |
| Lewis et al. [66] |
71 |
250 μg/m2 for 20 d, 28-d cycle |
TMZ, CDDP, IFN-α, IL-2 |
0 CR, 10 PR Median OS: 8.6 mo |
| Weber et al. [67] |
31 |
125 μg/m2 for 12 d, 28-d cycle |
TMZ, IL-2, IFN-α |
4 CR, 4 PR, 7 SD OS: 13.1 mo |
| Jin et al. [55] |
18 |
175 μg/m2 for 4 d, 21-d cycle |
DTIC, IL-2 |
4 CR, 8 PR |
| O’Day [56] |
131 |
Induction: 500 μg/d for 10 d or once daily until ANC >5000/μL |
Induction: VBL, CDDP, DTIC, IL-2, IFN-α |
10 CR, 47 PR, 38 SD Median OS: 13.5 mo 1-y survival: 57% |
|
Maintenance: 250 μg/d for 14 d |
Maintenance: IL-2 |
|||
| Gunturu et al. [68] |
18 |
250 μg/m2 from day 8 until AGC >5000 cells/μL on 2 consecutive days |
CTX, FLU, MESNA, IL-2 |
1 CR, 3 PR |
| Locke et al. [57] |
14 |
250 μg/m2 until WBC >30000/μL or for 10 d, 21-d cycle |
OX, DOX |
0 CR, 0 PR, 5 SD |
| Lutzky et al. [69] | 30 | 125 μg/m2 for 35 d | IL-2 | 0 CR, 4 PR, 8 SD Median OS: 10.7 mo 1-y survival: 32.5% |
AGC = absolute granulocyte count; ANC = absolute neutrophil count; BCNU = carmustine; CDDP = cisplatin; CR = complete response; CTX = cyclophosphamide; DOX = docetaxel; DTIC = dacarbazine; FLU = fludarabine; GM-CSF = granulocyte-macrophage colony-stimulating factor; IFN-α = interferon-α; IL-2 = interleukin-2; MESNA = sodium 2-mercaptoethanesulfonate; MR = mixed response; OS = overall survival; OX = oxaliplatin; PFS = progression-free survival; PR = partial response; SD = stable disease; TAM = tamoxifen; TMZ = temozolomide; VBL = vinblastine; VIN = vinorelbine.
GM-CSF as an adjuvant with cancer vaccines
Given the significant body of evidence from preclinical studies [11,18,20,21,70], GM-CSF has been evaluated as an adjuvant to cancer vaccines in a number of clinical studies. Several approaches to administering GM-CSF as an adjuvant have been employed, including coadministration with the vaccine [71-74], injection at the vaccination site [75,76] systemic administration [77,78], and administration of a plasmid/viral vector encoding GM-CSF [79,80]. The dose of GM-CSF administered as an adjuvant is typically less than the recommended overall weekly dose of 250 μg/m2/day for 21 days for use in myeloid reconstitution after autologous bone marrow transplantation [17].
In contrast to data from murine studies, the adjuvant effect of GM-CSF in human trials is inconsistent. In a study that evaluated coadministration of GM-CSF with multipeptide (including gp100 and tyrosinase peptides) melanoma vaccines incorporating GM-CSF and incomplete Freund’s adjuvant (IFA) in patients with advanced melanoma, there was a high T-cell response rate and a correlation between T-cell reactivity to the melanoma peptides and clinical outcome [72]. GM-CSF combined with IFA as an adjuvant for a vaccine containing 12 melanoma peptides resulted in a similar immunologic response in patients with resected stage III/IIIB/IV melanoma [74]. Similarly, systemic administration of GM-CSF following a peptide vaccination augmented T-cell response in three patients with advanced melanoma [77]. However, in a study that evaluated intradermal vaccination with tyrosinase peptides followed by intradermal GM-CSF, detectable T-cell responses were observed in only 4/15 (27%) evaluable patients [76].
Although results from these studies have suggested that administration of adjuvant GM-CSF might improve immune responses, none included control groups. Recently, clinical trials including controls have evaluated effects of GM-CSF administered locally at the vaccination site (Table 4). In a phase 1 study comparing different adjuvant strategies, vaccination with tyrosinase peptide plus GM-CSF or keyhole limpet hemocyanin (KLH) did not induce greater immune responses compared with vaccination with peptide alone, although combination with GM-CSF plus KLH had a moderate adjuvant effect [75]. Two recent randomized prospective trials suggested that addition of GM-CSF to melanoma vaccines did not improve cellular immune responses and, indeed, may have had negative effects [71,81]. Notably, both studies combined GM-CSF with another adjuvant (IFA or BCG) which may have influenced the immune response. The inconsistent effect of GM-CSF on immune responses to vaccines may be due in part to competing effects inducing dendritic cell maturation on one hand, and inducing myeloid suppressor cells on the other. A recent phase 2, randomized controlled trial (E1696) evaluated treatment of advanced melanoma with multipeptide vaccine alone or with subcutaneous interferon-α, GM-CSF, or interferon-α plus GM-CSF [78,82]. Consistent with results of studies evaluating administration of GM-CSF at the vaccine site, no significant improvement in T-cell or clinical response was observed with interferon-α and/or GM-CSF administration with vaccination [78,82].
Table 4.
Cancer vaccines testing the adjuvant effect of GM-CSF administered locally at the site of vaccination
| Citation | Design (Enrollment) | Ag (Route) | GM-CSF form (Route) | Coadmin-istration? | Study design | Effect of GM-CSF | Summary effect of GM-CSF |
|---|---|---|---|---|---|---|---|
| Scheibenbogen et al. [75] |
Sequential cohorts (n = 43) |
Tyrosinase peptides (ID/SC) |
Protein (ID/SC) 75 μg/d x 4 d/vaccine |
Yes |
Sequential: |
Minimal adjuvant effect Sequential trial cohorts |
Minimal adjuvant effect |
| 1. Peptides alone | |||||||
| 2. Peptides + GM-CSF | |||||||
| 3. Peptides + KLH | |||||||
| 4. Peptides + GM-CSF + KLH | |||||||
| Slingluff et al. [81] |
Randomized (n = 121) |
Melanoma peptides (ID/SC) |
Protein 110 μg (ID/SC) |
Yes |
Randomized: |
Negative on CD4 and CD8 T cells; too few events to differences in survival between groups |
Diminished, compared with IFA |
| 1. Peptides + IFA | |||||||
| 2. Peptides + IFA + GM-CSF | |||||||
| Faries et al. [71] |
Randomized (n = 97) |
Whole melanoma cell vaccine (ID) |
Protein 200 μg/m2/d x 5 days (ID) |
Yes |
Randomized: |
Better Ab, worse DTH; more Eos, Dec monocytes; more deaths |
Diminished compared with BCG |
| 1. Whole cell vaccine + BCG + GM-CSF | |||||||
| 2. Whole cell vaccine + BCG | |||||||
| Kirkwood et al. [78] |
2 × 2 (n = 120) |
MART-1, gp100, and tyrosinase peptides (SC) |
250 μg/d x 14 out of 28 days |
Yes |
2 × 2: |
No effect across treatment arms on best overall response |
Minimal adjuvant effect |
| |
|
|
|
|
Arm A: Peptide Vaccine Alone |
|
|
| |
|
|
|
|
Arm B: GM-CSF (250 μg/d x 14 out of 28 d) + vaccine |
|
|
| |
|
|
|
|
Arm C: IFN-α + vaccine |
|
|
| Arm D: GM-CSF + IFN-α + vaccine |
ID = intradermal; SC = subcutaneous; IFA = incomplete Freund’s adjuvant; BCG = Bacille Calmette-Guerin.
Results from clinical studies evaluating GM-CSF as an adjuvant to melanoma vaccines suggest the biologic effects of GM-CSF are complex and can be influenced by numerous factors. GM-CSF administered with a heat shock protein vaccine has been implicated in the induction of myeloid-derived suppressor cells (MDSC) in melanoma patients [83]. On the other hand, daily subcutaneous administration of GM-CSF (125 μg/m2 for 14 days in 28-day cycles) increased circulating mature DC but did not increase MDSC in melanoma patients [39]. It has been suggested that negative immunologic effects of GM-CSF may be associated primarily with high doses of GM-CSF (doses of 225 μg/d or higher in melanoma patients) [84]. In a trial of a multipeptide melanoma vaccine, immune responses were lower with GMCSF plus IFA than with IFA alone (the dose used in that trial was arguably less than 20 μg/day) [81]. Thus, even low doses of GM-CSF administered with a multipeptide vaccine may have negative immunologic effects. Additional studies are also needed to determine if GM-CSF alters the function of vaccine-induced T cells and whether inclusion of GM-CSF with the vaccine may affect clinical outcome.
Novel strategies incorporating GM-CSF
GM-CSF–expressing oncolytic immunotherapy
Preclinical studies have indicated an important role for GM-CSF in the tumor microenvironment and have suggested that increased expression of GM-CSF can inhibit tumor growth. However, administration of exogenous recombinant GM-CSF appears insufficient to mediate clinically meaningful improvements in outcomes in most instances. Consequently, there has been significant interest in novel treatment approaches incorporating GM-CSF.
Among the most extensively evaluated agents is the attenuated, oncolytic, herpes simplex virus, type 1 (HSV-1)–encoding human GM-CSF talimogene laherparepvec (T-VEC; formerly OncovexGM-CSF) [85-88]. The vector was generated from the HSV JS1 strain and was attenuated by functional deletion of the ICP34.5 and ICP47 viral genes, which renders the virus nonpathogenic in normal eukaryotic cells, promotes selective replication in tumor cells, and enhances immunogenicity [26] T-VEC has also been engineered to encode human GM-CSF, which further enhances the antitumor immune response. T-VEC is proposed to have a dual mechanism of action resulting in local tumor destruction by introduction of an oncolytic virus into tumor cells and induction of a systemic antitumor immune response.
In a phase 1 study, patients with subcutaneous or cutaneous metastases from breast, gastrointestinal, head and neck, or melanoma malignancies were treated with T-VEC. Clinically stable disease was noted in 3/26 patients administered intralesional T-VEC, with no patients having CR or PR during the study period [86]. However, follow-up biopsies in 14/19 patients showed necrosis, infiltration of T cells, and the presence of replicating virus [86]. Notably, there was evidence of expression of GM-CSF in injected lesions. In a subsequent phase 2 study among 50 patients with unresectable stage IIIC/IV melanoma administered intralesional T-VEC, the overall response rate was 26% (8 CR, 5 PR) [88]. Two additional patients were rendered disease-free by surgical resection following treatment. One-year survival was 58% for all patients and 40% among patients with stage IVM1c disease. Immunologic analysis of a subset of patients enrolled in the phase 2 study confirmed the presence of both local and distant antitumor immune responses following T-VEC administration. Biopsies performed on 11 patients after their sixth intratumoral injection were compared to nonstudy patients with metastatic melanoma [87]. In general, postvaccination tumors demonstrated extensive lymphocyte infiltration. Evaluation of both injected and noninjected lesions in T-VEC–treated patients revealed a significant increase in MART-1–specific T-cell response in both tumor and distant disease sites compared with unvaccinated controls. Regulatory CD4+FoxP3+ and suppressor CD8+FoxP3+ T cells and myeloid-derived suppressor cells were evaluated in injected tumor biopsies and found to be decreased when compared to unvaccinated control patients. When primary injected lesions were compared to distant noninjected lesions, the same general phenotypic pattern of effector T-cell and Treg infiltrates was seen; a greater number of CD4+FoxP3+ and CD8+FoxP3+ cells were present at the nontarget site than at the target sites. A randomized, phase 3 study, OPTiM, comparing intralesional T-VEC to subcutaneous GM-CSF demonstrated an improvement in durable response rate (16% vs 2%, respectively) and a trend toward improved OS at interim analysis (HR, 0.79 [95% CI, 0.61–1.02]) favoring the T-VEC arm [89]. The most frequently occurring adverse events were fatigue, chills, and pyrexia [89].
Systemic combination immunotherapy
GM-CSF has also been combined with ipilimumab, an anti-CTLA-4 monoclonal antibody. In a multicenter, phase 2 study, patients with metastatic melanoma were randomized to treatment with ipilimumab plus GM-CSF (250 μg/d subcutaneously for 14 days in 21-day cycles) or ipilimumab alone [90]. Patients receiving combination therapy experienced a significant improvement in 1-year OS. Although there were no significant differences in overall toxicity between the treatment arms, patients receiving combination therapy had a lower rate of serious adverse events.
Several other approaches utilizing GM-CSF are being developed. These include an oncolytic vaccinia virus encoding GM-CSF [91], autologous dendritic cells and allogeneic whole tumor cells encoding GM-CSF [92-94], adjuvant GM-CSF following vaccination with peptide or RNA encoding melanoma peptides [95,96] and autologous dendritic cell or whole tumor cell vaccines [97], and GM-CSF DNA vaccines [98].
Conclusions
GM-CSF has been studied extensively in murine models and in human clinical trials, alone and as adjuvant therapy for melanoma. There is evidence from numerous studies that GM-CSF can induce antitumor immunity when administered by a variety of different routes. Although there was initial enthusiasm for recombinant GM-CSF based on uncontrolled clinical trials in stage III/IV melanoma, therapeutic benefit has not been confirmed in larger, prospective, randomized trials. The adjuvant or combination use of GM-CSF has been more promising although results have been inconsistent and may depend on the potency of the immunotherapy regimen, GM-CSF dose, route and schedule of administration, and stage of disease. There is emerging evidence that GM-CSF may be a regulatory cytokine with the ability to promote both effector and regulatory/suppressor T cell populations. Thus, strategies that block suppressor T cell and myeloid-derived suppressor cell elements may enhance the antitumor activity of GM-CSF. GM-CSF has been particularly effective in studies of oncolytic HSV therapy of melanoma and in combination with ipilimumab. Further research into the basic biology of GM-CSF on effector and suppressor immune cells and expanded clinical studies of combination treatments will help define the full therapeutic potential of GM-CSF in treatment of melanoma.
Abbreviations
CTLA-4: Cytotoxic T-lymphocyte antigen 4; CR: Complete response; DC: Dendritic cells; DFS: Disease-free survival; GM-CSF: Granulocyte–macrophage colony-stimulating factor; HR: Hazard ratio; HSV: Herpes simplex viruses; IFA: Incomplete Freund’s adjuvant; KLH: Keyhole limpet hemocyanin; MDSC: Myeloid-derived suppressor cells; OS: Overall survival; PD-1: Programmed death 1; PR: Partial response; T-VEC: Talimogene laherparepvec.
Competing interests
HLK serves as a paid consultant and advisory board member for Amgen Inc. CLS is a scientific advisory board member for Immatics Biotechnologies and Polynoma LLC and a funded investigator for GlaxoSmithKline in the field of cancer vaccines; all funds from these activities are paid to the University of Virginia, not to Dr. Slingluff personally. Dr. Slingluff is an inventor on several patents for peptides used in cancer vaccines; the patents are held by the University of Virginia Licensing and Ventures Group. CER and TH have no conflicts to declare.
Authors’ contributions
All authors participated in critical analysis of the literature and drafting of the manuscript. All authors read and approved the final manuscript.
Contributor Information
Howard L Kaufman, Email: howard.kaufman@rutgers.edu.
Carl E Ruby, Email: carl_ruby@rush.edu.
Tasha Hughes, Email: tasha_hughes@rush.edu.
Craig L Slingluff, Jr, Email: cls8h@virginia.edu.
Acknowledgment
The authors would like to thank Erica S. Chevalier-Larsen, PhD (Complete Healthcare Communications, Inc., Chadds Ford, PA), for assistance in the preparation of this manuscript which was funded by Amgen Inc.
References
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- National Comprehensive Cancer Network. NCCN Guidelines® Version 2.2013 Melanoma. Fort Washington, PA; 2012. [Google Scholar]
- Pandolfi F, Cianci R, Pagliari D, Casciano F, Bagala C, Astone A, Landolfi R, Barone C. The immune response to tumors as a tool toward immunotherapy. Clin Dev Immunol. 2011;2011:894704. doi: 10.1155/2011/894704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggermont AM, Suciu S, Santinami M, Testori A, Kruit WH, Marsden J, Punt CJ, Sales F, Gore M, Mackie R, Kusic Z, Dummer R, Hauschild A, Musat E, Spatz A, Keilholz U, Group EM. Adjuvant therapy with pegylated interferon alfa-2b versus observation alone in resected stage III melanoma: final results of EORTC 18991, a randomised phase III trial. Lancet. 2008;372:117–126. doi: 10.1016/S0140-6736(08)61033-8. [DOI] [PubMed] [Google Scholar]
- Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, Akerley W, van den Eertwegh AJ, Lutzky J, Lorigan P, Vaubel JM, Linette GP, Hogg D, Ottensmeier CH, Lebbe C, Peschel C, Quirt I, Clark JI, Wolchok JD, Weber JS, Tian J, Yellin MJ, Nichol GM, Hoos A, Urba WJ. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert C, Thomas L, Bondarenko I, O’Day S, DJ M, Garbe C, Lebbe C, Baurain JF, Testori A, Grob JJ, Davidson N, Richards J, Maio M, Hauschild A, Miller WH Jr, Gascon P, Lotem M, Harmankaya K, Ibrahim R, Francis S, Chen TT, Humphrey R, Hoos A, Wolchok JD. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364:2517–2526. doi: 10.1056/NEJMoa1104621. [DOI] [PubMed] [Google Scholar]
- Atkins MB, Lotze MT, Dutcher JP, Fisher RI, Weiss G, Margolin K, Abrams J, Sznol M, Parkinson D, Hawkins M, Paradise C, Kunkel L, Rosenberg SA. High-dose recombinant interleukin 2 therapy for patients with metastatic melanoma: analysis of 270 patients treated between 1985 and 1993. J Clin Oncol. 1999;17:2105–2116. doi: 10.1200/JCO.1999.17.7.2105. [DOI] [PubMed] [Google Scholar]
- Rosenberg SA, Yang JC, Sherry RM, Kammula US, Hughes MS, Phan GQ, Citrin DE, Restifo NP, Robbins PF, Wunderlich JR, Morton KE, Laurencot CM, Steinberg SM, White DE, Dudley ME. Durable complete responses in heavily pretreated patients with metastatic melanoma using T-cell transfer immunotherapy. Clin Cancer Res. 2011;17:4550–4557. doi: 10.1158/1078-0432.CCR-11-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metcalf D. Hematopoietic cytokines. Blood. 2008;111:485–491. doi: 10.1182/blood-2007-03-079681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hercus TR, Thomas D, Guthridge MA, Ekert PG, King-Scott J, Parker MW, Lopez AF. The granulocyte-macrophage colony-stimulating factor receptor: linking its structure to cell signaling and its role in disease. Blood. 2009;114:1289–1298. doi: 10.1182/blood-2008-12-164004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dranoff G, Jaffee E, Lazenby A, Golumbek P, Levitsky H, Brose K, Jackson V, Hamada H, Pardoll D, Mulligan RC. Vaccination with irradiated tumor cells engineered to secrete murine granulocyte-macrophage colony-stimulating factor stimulates potent, specific, and long-lasting anti-tumor immunity. Proc Natl Acad Sci USA. 1993;90:3539–3543. doi: 10.1073/pnas.90.8.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonial S, Akhtari M, Kaufman J, Torre C, Lechowicz MJ, Flowers C, Sinha R, Khoury HJ, Langston AA, Waller EK. Mobilization of hematopoietic progenitors from normal donors using the combination of granulocyte-macrophage colony-stimulating factor and granulocyte colony-stimulating factor results in fewer plasmacytoid dendritic cells in the graft and enhanced donor T cell engraftment with Th1 polarization: results from a randomized clinical trial. Biol Blood Marrow Transplant. 2013;19:460–467. doi: 10.1016/j.bbmt.2012.11.017. [DOI] [PubMed] [Google Scholar]
- Lonial S, Hicks M, Rosenthal H, Langston A, Redei I, Torre C, Duenzl M, Feinstein B, Cherry J, Waller EK. A randomized trial comparing the combination of granulocyte-macrophage colony-stimulating factor plus granulocyte colony-stimulating factor versus granulocyte colony-stimulating factor for mobilization of dendritic cell subsets in hematopoietic progenitor cell products. Biol Blood Marrow Transplant. 2004;10:848–857. doi: 10.1016/j.bbmt.2004.07.008. [DOI] [PubMed] [Google Scholar]
- Mach N, Gillessen S, Wilson SB, Sheehan C, Mihm M, Dranoff G. Differences in dendritic cells stimulated in vivo by tumors engineered to secrete granulocyte-macrophage colony-stimulating factor or Flt3-ligand. Cancer Res. 2000;60:3239–3246. [PubMed] [Google Scholar]
- Choudhury BA, Liang JC, Thomas EK, Flores-Romo L, Xie QS, Agusala K, Sutaria S, Sinha I, Champlin RE, Claxton DF. Dendritic cells derived in vitro from acute myelogenous leukemia cells stimulate autologous, antileukemic T-cell responses. Blood. 1999;93:780–786. [PubMed] [Google Scholar]
- Boyer MW, Waller EK, Bray RA, Unangst T, Johnson TS, Phillips C, Jurickova I, Winton EF, Yeager AM. Cytokine upregulation of the antigen presenting function of acute myeloid leukemia cells. Leukemia. 2000;14:412–418. doi: 10.1038/sj.leu.2401685. [DOI] [PubMed] [Google Scholar]
- Leukine® (sargramostim) Full Prescribing Information. Cambridge, MA: Genzyme Corporation; 2009. [Google Scholar]
- Ahlers JD, Dunlop N, Alling DW, Nara PL, Berzofsky JA. Cytokine-in-adjuvant steering of the immune response phenotype to HIV-1 vaccine constructs: granulocyte-macrophage colony-stimulating factor and TNF-alpha synergize with IL-12 to enhance induction of cytotoxic T lymphocytes. J Immunol. 1997;158:3947–3958. [PubMed] [Google Scholar]
- Reilly RT, Gottlieb MB, Ercolini AM, Machiels JP, Kane CE, Okoye FI, Muller WJ, Dixon KH, Jaffee EM. HER-2/neu is a tumor rejection target in tolerized HER-2/neu transgenic mice. Cancer Res. 2000;60:3569–3576. [PubMed] [Google Scholar]
- Reilly RT, Machiels JP, Emens LA, Ercolini AM, Okoye FI, Lei RY, Weintraub D, Jaffee EM. The collaboration of both humoral and cellular HER-2/neu-targeted immune responses is required for the complete eradication of HER-2/neu-expressing tumors. Cancer Res. 2001;61:880–883. [PubMed] [Google Scholar]
- Borrello I, Pardoll D. GM-CSF-based cellular vaccines: a review of the clinical experience. Cytokine Growth Factor Rev. 2002;13:185–193. doi: 10.1016/S1359-6101(01)00034-X. [DOI] [PubMed] [Google Scholar]
- Simmons AD, Li B, Gonzalez-Edick M, Lin C, Moskalenko M, Du T, Creson J, VanRoey MJ, Jooss K. GM-CSF-secreting cancer immunotherapies: preclinical analysis of the mechanism of action. Cancer Immunol Immunother. 2007;56:1653–1665. doi: 10.1007/s00262-007-0315-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ju DW, Cao X, Acres B. Active specific immunotherapy of pulmonary metastasis with vaccinia melanoma oncolysate prepared from granulocyte/macrophage-colony-stimulating-factor-gene-encoded vaccinia virus. J Cancer Res Clin Oncol. 1996;122:716–722. doi: 10.1007/BF01209118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ju DW, Cao X, Acres B. Intratumoral injection of GM-CSF gene encoded recombinant vaccinia virus elicits potent antitumor response in a mixture melanoma model. Cancer Gene Ther. 1997;4:139–144. [PubMed] [Google Scholar]
- Toda M, Martuza RL, Rabkin SD. Tumor growth inhibition by intratumoral inoculation of defective herpes simplex virus vectors expressing granulocyte-macrophage colony-stimulating factor. Mol Ther. 2000;2:324–329. doi: 10.1006/mthe.2000.0130. [DOI] [PubMed] [Google Scholar]
- Liu BL, Robinson M, Han ZQ, Branston RH, English C, Reay P, McGrath Y, Thomas SK, Thornton M, Bullock P, Love CA, Coffin RS. ICP34.5 deleted herpes simplex virus with enhanced oncolytic, immune stimulating, and anti-tumour properties. Gene Ther. 2003;10:292–303. doi: 10.1038/sj.gt.3301885. [DOI] [PubMed] [Google Scholar]
- Li B, VanRoey M, Wang C, Chen TH, Korman A, Jooss K. Anti-programmed death-1 synergizes with granulocyte macrophage colony-stimulating factor–secreting tumor cell immunotherapy providing therapeutic benefit to mice with established tumors. Clin Cancer Res. 2009;15:1623–1634. doi: 10.1158/1078-0432.CCR-08-1825. [DOI] [PubMed] [Google Scholar]
- Quezada SA, Peggs KS, Curran MA, Allison JP. CTLA4 blockade and GM-CSF combination immunotherapy alters the intratumor balance of effector and regulatory T cells. J Clin Invest. 2006;116:1935–1945. doi: 10.1172/JCI27745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Powderly JD, Carvajal RD, Sosman JA, Atkins MB, Leming PD, Spigel DR, Antonia SJ, Horn L, Drake CG, Pardoll DM, Chen L, Sharfman WH, Anders RA, Taube JM, McMiller TL, Xu H, Korman AJ, Jure-Kunkel M, Agrawal S, McDonald D, Kollia GD, Gupta A, Wigginton JM, Sznol M. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Elsas A, Hurwitz AA, Allison JP. Combination immunotherapy of B16 melanoma using anti-cytotoxic T lymphocyte-associated antigen 4 (CTLA-4) and granulocyte/macrophage colony-stimulating factor (GM-CSF)-producing vaccines induces rejection of subcutaneous and metastatic tumors accompanied by autoimmune depigmentation. J Exp Med. 1999;190:355–366. doi: 10.1084/jem.190.3.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber J. Immune checkpoint proteins: a new therapeutic paradigm for cancer–preclinical background: CTLA-4 and PD-1 blockade. Semin Oncol. 2010;37:430–439. doi: 10.1053/j.seminoncol.2010.09.005. [DOI] [PubMed] [Google Scholar]
- Choi KJ, Kim JH, Lee YS, Kim J, Suh BS, Kim H, Cho S, Sohn JH, Kim GE, Yun CO. Concurrent delivery of GM-CSF and B7-1 using an oncolytic adenovirus elicits potent antitumor effect. Gene Ther. 2006;13:1010–1020. doi: 10.1038/sj.gt.3302759. [DOI] [PubMed] [Google Scholar]
- Li B, Lin J, Vanroey M, Jure-Kunkel M, Jooss K. Established B16 tumors are rejected following treatment with GM-CSF-secreting tumor cell immunotherapy in combination with anti-4-1BB mAb. Clin Immunol. 2007;125:76–87. doi: 10.1016/j.clim.2007.07.005. [DOI] [PubMed] [Google Scholar]
- Prell RA, Li B, Lin JM, VanRoey M, Jooss K. Administration of IFN-alpha enhances the efficacy of a granulocyte macrophage colony stimulating factor-secreting tumor cell vaccine. Cancer Res. 2005;65:2449–2456. doi: 10.1158/0008-5472.CAN-04-1975. [DOI] [PubMed] [Google Scholar]
- Stagg J, Wu JH, Bouganim N, Galipeau J. Granulocyte-macrophage colony-stimulating factor and interleukin-2 fusion cDNA for cancer gene immunotherapy. Cancer Res. 2004;64:8795–8799. doi: 10.1158/0008-5472.CAN-04-1776. [DOI] [PubMed] [Google Scholar]
- Li B, Lalani AS, Harding TC, Luan B, Koprivnikar K, Huan Tu G, Prell R, VanRoey MJ, Simmons AD, Jooss K. Vascular endothelial growth factor blockade reduces intratumoral regulatory T cells and enhances the efficacy of a GM-CSF-secreting cancer immunotherapy. Clin Cancer Res. 2006;12:6808–6816. doi: 10.1158/1078-0432.CCR-06-1558. [DOI] [PubMed] [Google Scholar]
- Spitler LE, Grossbard ML, Ernstoff MS, Silver G, Jacobs M, Hayes FA, Soong SJ. Adjuvant therapy of stage III and IV malignant melanoma using granulocyte-macrophage colony-stimulating factor. J Clin Oncol. 2000;18:1614–1621. doi: 10.1200/JCO.2000.18.8.1614. [DOI] [PubMed] [Google Scholar]
- Spitler LE, Weber RW, Allen RE, Meyer J, Cruickshank S, Garbe E, Lin HY, Soong SJ. Recombinant human granulocyte-macrophage colony-stimulating factor (GM-CSF, sargramostim) administered for 3 years as adjuvant therapy of stages II(T4), III, and IV melanoma. J Immunother. 2009;32:632–637. doi: 10.1097/CJI.0b013e3181a7d60d. [DOI] [PubMed] [Google Scholar]
- Daud AI, Mirza N, Lenox B, Andrews S, Urbas P, Gao GX, Lee JH, Sondak VK, Riker AI, Deconti RC, Gabrilovich D. Phenotypic and functional analysis of dendritic cells and clinical outcome in patients with high-risk melanoma treated with adjuvant granulocyte macrophage colony-stimulating factor. J Clin Oncol. 2008;26:3235–3241. doi: 10.1200/JCO.2007.13.9048. [DOI] [PubMed] [Google Scholar]
- Lawson DH, Lee SJ, Tarhini AA, Margolin KA, Ernstoff MS, Kirkwood JM. E4697: Phase III cooperative group study of yeast-derived granulocyte macrophage colonystimulating factor (GM-CSF) versus placebo as adjuvant treatment of patients with completely resected stage III-IV melanoma. J Clin Oncol. 2010;28:abstr 8504. [Google Scholar]
- Markovic S, Burch PA, LaPlant B, Heun JM, Bradshaw R. Adjuvant GM-CSF therapy for patients with resected stage III/IV melanoma: A retrospective review of a single-center experience. J Clin Oncol. 2011;29:abstr 8596. [Google Scholar]
- Isla D, Filipovich E, Mayordomo JI, Andres R, Puig S, Escudero MP, Gallego O, Trujillo R, Revenga F, Alvarez I, Saenz A, Polo E, Tres A. Daily GM-CSF for patients with very high-risk resected melanoma: a pilot trial. Proc Am Soc Clin Oncol. 2002;21:abstr 2784. [Google Scholar]
- Elias EG, Zapas JL, McCarron EC, Beam SL, Hasskamp JH, Culpepper WJ. Sequential administration of GM-CSF (Sargramostim) and IL-2 +/−autologous vaccine as adjuvant therapy in cutaneous melanoma: an interim report of a phase II clinical trial. Cancer Biother Radiopharm. 2008;23:285–291. doi: 10.1089/cbr.2007.0438. [DOI] [PubMed] [Google Scholar]
- Si Z, Hersey P, Coates AS. Clinical responses and lymphoid infiltrates in metastatic melanoma following treatment with intralesional GM-CSF. Melanoma Res. 1996;6:247–255. doi: 10.1097/00008390-199606000-00008. [DOI] [PubMed] [Google Scholar]
- Nasi ML, Lieberman P, Busam KJ, Prieto V, Panageas KS, Lewis JJ, Houghton AN, Chapman PB. Intradermal injection of granulocyte-macrophage colony-stimulating factor (GM-CSF) in patients with metastatic melanoma recruits dendritic cells. Cytokines Cell Mol Ther. 1999;5:139–144. [PubMed] [Google Scholar]
- Hoeller C, Jansen B, Heere-Ress E, Pustelnik T, Mossbacher U, Schlagbauer-Wadl H, Wolff K, Pehamberger H. Perilesional injection of r-GM-CSF in patients with cutaneous melanoma metastases. J Invest Dermatol. 2001;117:371–374. doi: 10.1046/j.0022-202x.2001.01427.x. [DOI] [PubMed] [Google Scholar]
- Rao RD, Anderson PM, Arndt CA, Wettstein PJ, Markovic SN. Aerosolized granulocyte macrophage colony-stimulating factor (GM-CSF) therapy in metastatic cancer. Am J Clin Oncol. 2003;26:493–498. doi: 10.1097/01.coc.0000037664.04141.D0. [DOI] [PubMed] [Google Scholar]
- Markovic SN, Suman VJ, Nevala WK, Geeraerts L, Creagan ET, Erickson LA, Rowland KM Jr, Morton RF, Horvath WL, Pittelkow MR. A dose-escalation study of aerosolized sargramostim in the treatment of metastatic melanoma: an NCCTG Study. Am J Clin Oncol. 2008;31:573–579. doi: 10.1097/COC.0b013e318173a536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato T, Eschelman DJ, Gonsalves CF, Terai M, Chervoneva I, McCue PA, Shields JA, Shields CL, Yamamoto A, Berd D, Mastrangelo MJ, Sullivan KL. Immunoembolization of malignant liver tumors, including uveal melanoma, using granulocyte-macrophage colony-stimulating factor. J Clin Oncol. 2008;26:5436–5442. doi: 10.1200/JCO.2008.16.0705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eschelman DJ, Gonsalves CF, Terai M, Laudadio M, Sullivan KL, Mastrangelo MJ, Sato T. The results of a randomized phase II study using embolization with or without granulocyte-macrophage colony-stimulating factor (GM-CSF) in uveal melanoma patients with hepatic metastasis. J Clin Oncol. 2011;29:abstr 8577. [Google Scholar]
- Vaquerano JE, Cadbury P, Treseler P, Sagebiel R, Leong SP. Regression of in-transit melanoma of the scalp with intralesional recombinant human granulocyte-macrophage colony-stimulating factor. Arch Dermatol. 1999;135:1276–1277. doi: 10.1001/archderm.135.10.1276. [DOI] [PubMed] [Google Scholar]
- Ridolfi L, Ridolfi R. Preliminary experiences of intralesional immunotherapy in cutaneous metastatic melanoma. Hepatogastroenterology. 2002;49:335–339. [PubMed] [Google Scholar]
- Schachter J, Rakowsky E, Sulkes A, Adler A. A sequential four-drug chemotherapy and biotherapy with interferon alpha and GM-CSF–an innovative protocol for the treatment of metastatic melanoma. Cancer Biother Radiopharm. 1998;13:155–164. doi: 10.1089/cbr.1998.13.155. [DOI] [PubMed] [Google Scholar]
- Fruehauf JP, Kong KM, Jakowatz JG. Docetaxel and vinorelbine plus GM-CSF in malignant melanoma. Oncology (Williston Park) 2005;19:19–22. [PubMed] [Google Scholar]
- Jin S, Zhang Q, Kang X, Wang J, Sun W. Malignant melanoma therapy by chemotherapy and autoimmunity induced by cytokine. Cancer Biother Radiopharm. 2009;24:237–241. doi: 10.1089/cbr.2008.0552. [DOI] [PubMed] [Google Scholar]
- O’Day SJ, Atkins MB, Boasberg P, Wang HJ, Thompson JA, Anderson CM, Gonzalez R, Lutzky J, Amatruda T, Hersh EM, Weber JS. Phase II multicenter trial of maintenance biotherapy after induction concurrent Biochemotherapy for patients with metastatic melanoma. J Clin Oncol. 2009;27:6207–6212. doi: 10.1200/JCO.2008.20.3075. [DOI] [PubMed] [Google Scholar]
- Locke F, Clark JI, Gajewski TF. A phase II study of oxaliplatin, docetaxel, and GM-CSF in patients with previously treated advanced melanoma. Cancer Chemother Pharmacol. 2010;65:509–514. doi: 10.1007/s00280-009-1057-y. [DOI] [PubMed] [Google Scholar]
- Lutzky J, Weber R, Nunez Y, Gillett M, Spitler L. A phase 1 study of granulocyte macrophage colony-stimulating factor (sargramostim) and escalating doses of thalidomide in patients with high-risk malignant melanoma. J Immunother. 2009;32:79–85. doi: 10.1097/CJI.0b013e31818c8aaf. [DOI] [PubMed] [Google Scholar]
- Vaughan MM, Moore J, Riches PG, Johnston SR, A’Hern RP, Hill ME, Eisen T, Ayliffe MJ, Thomas JM, Gore ME. GM-CSF with biochemotherapy (cisplatin, DTIC, tamoxifen, IL-2 and interferon-alpha): a phase I trial in melanoma. Ann Oncol. 2000;11:1183–1189. doi: 10.1023/A:1008348005349. [DOI] [PubMed] [Google Scholar]
- Gajewski T, Flickinger S. A phase II study of outpatient chemoimmunotherapy using cisplatin and DTIC followed by GM-CSF, IL-2, and IFN-2b in patients (pts) with metastatic melanoma. Proc Am Soc Clin Oncol. 2000;19:abstr 2271. [Google Scholar]
- Gibbs P, O’Day S, Richards J, Weber J, Anderson C, Gonzalez R. Biochemotherapy (BCT) for stage IV melanoma incorporating temozolomide, decrescendo interleukin-2 (IL-2) and GM-CSF. Proc Am Soc Clin Oncol. 2000;19:2255. doi: 10.1081/cnv-58832. [DOI] [PubMed] [Google Scholar]
- Gong I-Y, Swiger S, Gajewski T. Integration of GM-CSF into outpatient chemoimmunotherapy for metastatic melanoma. Proc Am Soc Clin Oncol. 2002;21:2790. [Google Scholar]
- Groenewegen G, Bloem A, De Gast GC. Phase I/II study of sequential chemoimmunotherapy (SCIT) for metastatic melanoma: outpatient treatment with dacarbazine, granulocyte-macrophage colony-stimulating factor, low-dose interleukin-2, and interferon-alpha. Cancer Immunol Immunother. 2002;51:630–636. doi: 10.1007/s00262-002-0323-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Gast GC, Batchelor D, Kersten MJ, Vyth-Dreese FA, Sein J, van de Kasteele WF, Nooijen WJ, Nieweg OE, de Waal MA, Boogerd W. Temozolomide followed by combined immunotherapy with GM-CSF, low-dose IL2 and IFN alpha in patients with metastatic melanoma. Br J Cancer. 2003;88:175–180. doi: 10.1038/sj.bjc.6600717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith IJ, Kurt RA, Baher AG, Denman S, Justice L, Doran T, Gilbert M, Alvord WG, Urba WJ. Immune effects of escalating doses of granulocyte-macrophage colony-stimulating factor added to a fixed, low-dose, inpatient interleukin-2 regimen: a randomized phase I trial in patients with metastatic melanoma and renal cell carcinoma. J Immunother. 2003;26:130–138. doi: 10.1097/00002371-200303000-00005. [DOI] [PubMed] [Google Scholar]
- Lewis KD, Gibbs P, O’Day S, Richards J, Weber J, Anderson C, Zeng C, Baron A, Russ P, Gonzalez R. A phase II study of biochemotherapy for advanced melanoma incorporating temozolomide, decrescendo interleukin-2 and GM-CSF. Cancer Invest. 2005;23:303–308. doi: 10.1081/CNV-58832. [DOI] [PubMed] [Google Scholar]
- Weber RW, O’Day S, Rose M, Deck R, Ames P, Good J, Meyer J, Allen R, Trautvetter S, Timmerman M, Cruickshank S, Cook M, Gonzalez R, Spitler LE. Low-dose outpatient chemobiotherapy with temozolomide, granulocyte-macrophage colony stimulating factor, interferon-alpha2b, and recombinant interleukin-2 for the treatment of metastatic melanoma. J Clin Oncol. 2005;23:8992–9000. doi: 10.1200/JCO.2005.02.5791. [DOI] [PubMed] [Google Scholar]
- Gunturu KS, Meehan KR, Mackenzie TA, Crocenzi TS, McDermott D, Usherwood EJ, Margolin KA, Crosby NA, Atkins MB, Turk MJ, Ahonen C, Fuse S, Clark JI, Fisher JL, Noelle RJ, Ernstoff MS. Cytokine working group study of lymphodepleting chemotherapy, interleukin-2, and granulocyte-macrophage colony-stimulating factor in patients with metastatic melanoma: clinical outcomes and peripheral-blood cell recovery. J Clin Oncol. 2010;28:1196–1202. doi: 10.1200/JCO.2009.24.8153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutzky J, Lawson DH, Enriquez-Nunez Y, Gabrilovich D. Phase II trial of high-dose interleukin-2 (IL-2) with priming and concomitant sargramostim (GM-CSF) in patients with advanced melanoma. J Clin Oncol. 2010;28:abstr 8560. [Google Scholar]
- Ali OA, Emerich D, Dranoff G, Mooney DJ. In situ regulation of DC subsets and T cells mediates tumor regression in mice. Sci Transl Med. 2009;1:8ra19. doi: 10.1126/scitranslmed.3000359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faries MB, Hsueh EC, Ye X, Hoban M, Morton DL. Effect of granulocyte/macrophage colony-stimulating factor on vaccination with an allogeneic whole-cell melanoma vaccine. Clin Cancer Res. 2009;15:7029–7035. doi: 10.1158/1078-0432.CCR-09-1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slingluff CL Jr, Petroni GR, Yamshchikov GV, Barnd DL, Eastham S, Galavotti H, Patterson JW, Deacon DH, Hibbitts S, Teates D, Neese PY, Grosh WW, Chianese-Bullock KA, Woodson EM, Wiernasz CJ, Merrill P, Gibson J, Ross M, Engelhard VH. Clinical and immunologic results of a randomized phase II trial of vaccination using four melanoma peptides either administered in granulocyte-macrophage colony-stimulating factor in adjuvant or pulsed on dendritic cells. J Clin Oncol. 2003;21:4016–4026. doi: 10.1200/JCO.2003.10.005. [DOI] [PubMed] [Google Scholar]
- Walter S, Weinschenk T, Stenzl A, Zdrojowy R, Pluzanska A, Szczylik C, Staehler M, Brugger W, Dietrich PY, Mendrzyk R, Hilf N, Schoor O, Fritsche J, Mahr A, Maurer D, Vass V, Trautwein C, Lewandrowski P, Flohr C, Pohla H, Stanczak JJ, Bronte V, Mandruzzato S, Biedermann T, Pawelec G, Derhovanessian E, Yamagishi H, Miki T, Hongo F, Takaha N. et al. Multipeptide immune response to cancer vaccine IMA901 after single-dose cyclophosphamide associates with longer patient survival. Nat Med. 2012;18:1254–1261. doi: 10.1038/nm.2883. [DOI] [PubMed] [Google Scholar]
- Chianese-Bullock KA, Pressley J, Garbee C, Hibbitts S, Murphy C, Yamshchikov G, Petroni GR, Bissonette EA, Neese PY, Grosh WW, Merrill P, Fink R, Woodson EM, Wiernasz CJ, Patterson JW, Slingluff CL Jr. MAGE-A1-, MAGE-A10-, and gp100-derived peptides are immunogenic when combined with granulocyte-macrophage colony-stimulating factor and montanide ISA-51 adjuvant and administered as part of a multipeptide vaccine for melanoma. J Immunol. 2005;174:3080–3086. doi: 10.4049/jimmunol.174.5.3080. [DOI] [PubMed] [Google Scholar]
- Scheibenbogen C, Schadendorf D, Bechrakis NE, Nagorsen D, Hofmann U, Servetopoulou F, Letsch A, Philipp A, Foerster MH, Schmittel A, Thiel E, Keilholz U. Effects of granulocyte-macrophage colony-stimulating factor and foreign helper protein as immunologic adjuvants on the T-cell response to vaccination with tyrosinase peptides. Int J Cancer. 2003;104:188–194. doi: 10.1002/ijc.10961. [DOI] [PubMed] [Google Scholar]
- Scheibenbogen C, Schmittel A, Keilholz U, Allgauer T, Hofmann U, Max R, Thiel E, Schadendorf D. Phase 2 trial of vaccination with tyrosinase peptides and granulocyte-macrophage colony-stimulating factor in patients with metastatic melanoma. J Immunother. 2000;23:275–281. doi: 10.1097/00002371-200003000-00012. [DOI] [PubMed] [Google Scholar]
- Jager E, Ringhoffer M, Dienes HP, Arand M, Karbach J, Jager D, Ilsemann C, Hagedorn M, Oesch F, Knuth A. Granulocyte-macrophage-colony-stimulating factor enhances immune responses to melanoma-associated peptides in vivo. Int J Cancer. 1996;67:54–62. doi: 10.1002/(SICI)1097-0215(19960703)67:1<54::AID-IJC11>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- Kirkwood JM, Lee S, Moschos SJ, Albertini MR, Michalak JC, Sander C, Whiteside T, Butterfield LH, Weiner L. Immunogenicity and antitumor effects of vaccination with peptide vaccine+/−granulocyte-monocyte colony-stimulating factor and/or IFN-alpha2b in advanced metastatic melanoma: Eastern Cooperative Oncology Group Phase II Trial E1696. Clin Cancer Res. 2009;15:1443–1451. doi: 10.1158/1078-0432.CCR-08-1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soiffer R, Hodi FS, Haluska F, Jung K, Gillessen S, Singer S, Tanabe K, Duda R, Mentzer S, Jaklitsch M, Bueno R, Clift S, Hardy S, Neuberg D, Mulligan R, Webb I, Mihm M, Dranoff G. Vaccination with irradiated, autologous melanoma cells engineered to secrete granulocyte-macrophage colony-stimulating factor by adenoviral-mediated gene transfer augments antitumor immunity in patients with metastatic melanoma. J Clin Oncol. 2003;21:3343–3350. doi: 10.1200/JCO.2003.07.005. [DOI] [PubMed] [Google Scholar]
- Soiffer R, Lynch T, Mihm M, Jung K, Rhuda C, Schmollinger JC, Hodi FS, Liebster L, Lam P, Mentzer S, Singer S, Tanabe KK, Cosimi AB, Duda R, Sober A, Bhan A, Daley J, Neuberg D, Parry G, Rokovich J, Richards L, Drayer J, Berns A, Clift S, Cohen LK, Mulligan RC, Dranoff G. Vaccination with irradiated autologous melanoma cells engineered to secrete human granulocyte-macrophage colony-stimulating factor generates potent antitumor immunity in patients with metastatic melanoma. Proc Natl Acad Sci USA. 1998;95:13141–13146. doi: 10.1073/pnas.95.22.13141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slingluff CL Jr, Petroni GR, Olson WC, Smolkin ME, Ross MI, Haas NB, Grosh WW, Boisvert ME, Kirkwood JM, Chianese-Bullock KA. Effect of granulocyte/macrophage colony-stimulating factor on circulating CD8+ and CD4+ T-cell responses to a multipeptide melanoma vaccine: outcome of a multicenter randomized trial. Clin Cancer Res. 2009;15:7036–7044. doi: 10.1158/1078-0432.CCR-09-1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer C, Butterfield LH, Lee S, Kim GG, Visus C, Albers A, Kirkwood JM, Whiteside TL. Function but not phenotype of melanoma peptide-specific CD8(+) T cells correlate with survival in a multiepitope peptide vaccine trial (ECOG 1696) Int J Cancer. 2012;131:874–884. doi: 10.1002/ijc.26481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filipazzi P, Valenti R, Huber V, Pilla L, Canese P, Iero M, Castelli C, Mariani L, Parmiani G, Rivoltini L. Identification of a new subset of myeloid suppressor cells in peripheral blood of melanoma patients with modulation by a granulocyte-macrophage colony-stimulation factor-based antitumor vaccine. J Clin Oncol. 2007;25:2546–2553. doi: 10.1200/JCO.2006.08.5829. [DOI] [PubMed] [Google Scholar]
- Parmiani G, Castelli C, Pilla L, Santinami M, Colombo MP, Rivoltini L. Opposite immune functions of GM-CSF administered as vaccine adjuvant in cancer patients. Ann Oncol. 2007;18:226–232. doi: 10.1093/annonc/mdl158. [DOI] [PubMed] [Google Scholar]
- Harrington KJ, Hingorani M, Tanay MA, Hickey J, Bhide SA, Clarke PM, Renouf LC, Thway K, Sibtain A, McNeish IA, Newbold KL, Goldsweig H, Coffin R, Nutting CM. Phase I/II study of oncolytic HSV GM-CSF in combination with radiotherapy and cisplatin in untreated stage III/IV squamous cell cancer of the head and neck. Clin Cancer Res. 2010;16:4005–4015. doi: 10.1158/1078-0432.CCR-10-0196. [DOI] [PubMed] [Google Scholar]
- Hu JCC, Coffin RS, Davis CJ. A phase I study of OncoVEXGM-CSF, a second-generation oncolytic herpes simplex virus expressing granulocyte macrophage colony-stimulating factor. Clin Cancer Res. 2006;12:6737–6747. doi: 10.1158/1078-0432.CCR-06-0759. [DOI] [PubMed] [Google Scholar]
- Kaufman HL, Kim DW, DeRaffele G, Mitcham J, Coffin RS, Kim-Schulze S. Local and distant immunity induced by intralesional vaccination with an oncolytic herpes virus encoding GM-CSF in patients with stage IIIc and IV melanoma. Ann Surg Oncol. 2010;17:718–730. doi: 10.1245/s10434-009-0809-6. [DOI] [PubMed] [Google Scholar]
- Senzer NN, Kaufman HL, Amatruda T, Nemunaitis M, Reid T, Daniels G, Gonzalez R, Glaspy J, Whitman E, Harrington K, Goldsweig H, Marshall T, Love C, Coffin R, Nemunaitis JJ. Phase II clinical trial of a granulocyte-macrophage colony-stimulating factor-encoding, second-generation oncolytic herpesvirus in patients with unresectable metastatic melanoma. J Clin Oncol. 2009;27:5763–5771. doi: 10.1200/JCO.2009.24.3675. [DOI] [PubMed] [Google Scholar]
- Andtbacka RHI, Collichio FA, Amatruda T, Senzer NN, Chesney J, Delman KA, Spitler LE, Puzanov I, Doleman S, Ye Y, Vanderwalde AM, Coffin R, Kaufman H. OPTiM: A randomized phase III trial of talimogene laherparepvec (T-VEC) versus subcutaneous (SC) granulocyte-macrophage colony-stimulating factor (GM-CSF) for the treatment (tx) of unresected stage IIIB/C and IV melanoma. J Clin Oncol. 2013;31:abstr LBA9008. [Google Scholar]
- Hodi FS, Lee SJ, McDermott DF, Rao UNM, Butterfield LH, Tarhini AA, Leming PD, Puzanov I, Kirkwood JM. Multicenter, randomized phase II trial of GM-CSF (GM) plus ipilimumab (Ipi) versus Ipi alone in metastatic melanoma: E1608. J Clin Oncol. 2013;31:abstr CRA9007. [Google Scholar]
- Heo J, Breitbach CJ, Moon A, Kim CW, Patt R, Kim MK, Lee YK, Oh SY, Woo HY, Parato K, Rintoul J, Falls T, Hickman T, Rhee BG, Bell JC, Kirn DH, Hwang TH. Sequential therapy with JX-594, a targeted oncolytic poxvirus, followed by sorafenib in hepatocellular carcinoma: preclinical and clinical demonstration of combination efficacy. Mol Ther. 2011;19:1170–1179. doi: 10.1038/mt.2011.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higano CS, Corman JM, Smith DC, Centeno AS, Steidle CP, Gittleman M, Simons JW, Sacks N, Aimi J, Small EJ. Phase 1/2 dose-escalation study of a GM-CSF-secreting, allogeneic, cellular immunotherapy for metastatic hormone-refractory prostate cancer. Cancer. 2008;113:975–984. doi: 10.1002/cncr.23669. [DOI] [PubMed] [Google Scholar]
- Schoenfeld J, Jinushi M, Nakazaki Y, Wiener D, Park J, Soiffer R, Neuberg D, Mihm M, Hodi FS, Dranoff G. Active immunotherapy induces antibody responses that target tumor angiogenesis. Cancer Res. 2010;70:10150–10160. doi: 10.1158/0008-5472.CAN-10-1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senzer N, Barve M, Kuhn J, Melnyk A, Beitsch P, Lazar M, Lifshitz S, Magee M, Oh J, Mill SW, Bedell C, Higgs C, Kumar P, Yu Y, Norvell F, Phalon C, Taquet N, Rao DD, Wang Z, Jay CM, Pappen BO, Wallraven G, Brunicardi FC, Shanahan DM, Maples PB, Nemunaitis J. Phase I trial of “bi-shRNAi(furin)/GMCSF DNA/autologous tumor cell” vaccine (FANG) in advanced cancer. Mol Ther. 2012;20:679–686. doi: 10.1038/mt.2011.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adamina M, Rosenthal R, Weber WP, Frey DM, Viehl CT, Bolli M, Huegli RW, Jacob AL, Heberer M, Oertli D, Marti W, Spagnoli GC, Zajac P. Intranodal immunization with a vaccinia virus encoding multiple antigenic epitopes and costimulatory molecules in metastatic melanoma. Mol Ther. 2010;18:651–659. doi: 10.1038/mt.2009.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weide B, Pascolo S, Scheel B, Derhovanessian E, Pflugfelder A, Eigentler TK, Pawelec G, Hoerr I, Rammensee HG, Garbe C. Direct injection of protamine-protected mRNA: results of a phase 1/2 vaccination trial in metastatic melanoma patients. J Immunother. 2009;32:498–507. doi: 10.1097/CJI.0b013e3181a00068. [DOI] [PubMed] [Google Scholar]
- Dillman RO, Cornforth AN, Depriest C, McClay EF, Amatruda TT, de Leon C, Ellis RE, Mayorga C, Carbonell D, Cubellis JM. Tumor stem cell antigens as consolidative active specific immunotherapy: a randomized phase II trial of dendritic cells versus tumor cells in patients with metastatic melanoma. J Immunother. 2012;35:641–649. doi: 10.1097/CJI.0b013e31826f79c8. [DOI] [PubMed] [Google Scholar]
- Perales MA, Yuan J, Powel S, Gallardo HF, Rasalan TS, Gonzalez C, Manukian G, Wang J, Zhang Y, Chapman PB, Krown SE, Livingston PO, Ejadi S, Panageas KS, Engelhorn ME, Terzulli SL, Houghton AN, Wolchok JD. Phase I/II study of GM-CSF DNA as an adjuvant for a multipeptide cancer vaccine in patients with advanced melanoma. Mol Ther. 2008;16:2022–2029. doi: 10.1038/mt.2008.196. [DOI] [PMC free article] [PubMed] [Google Scholar]


