Abstract
Background
Inhibition of the activated epidermal growth factor receptor (EGFR) with either enzymatic kinase inhibitors or anti-EGFR antibodies such as cetuximab, is an effective modality of treatment for multiple human cancers. Enzymatic EGFR inhibitors are effective for lung adenocarcinomas with somatic kinase domain EGFR mutations while, paradoxically, anti-EGFR antibodies are more effective in colon and head and neck cancers where EGFR mutations occur less frequently. In colorectal cancer, anti-EGFR antibodies are routinely used as second-line therapy of KRAS wild-type tumors. However, detailed mechanisms and genomic predictors for pharmacological response to these antibodies in colon cancer remain unclear.
Findings
We describe a case of colorectal adenocarcinoma, which was found to harbor a kinase domain mutation, G724S, in EGFR through whole genome sequencing. We show that G724S mutant EGFR is oncogenic and that it differs from classic lung cancer derived EGFR mutants in that it is cetuximab responsive in vitro, yet relatively insensitive to small molecule kinase inhibitors. Through biochemical and cellular pharmacologic studies, we have determined that cells harboring the colon cancer-derived G719S and G724S mutants are responsive to cetuximab therapy in vitro and found that the requirement for asymmetric dimerization of these mutant EGFR to promote cellular transformation may explain their greater inhibition by cetuximab than small-molecule kinase inhibitors.
Conclusion
The colon-cancer derived G719S and G724S mutants are oncogenic and sensitive in vitro to cetuximab. These data suggest that patients with these mutations may benefit from the use of anti-EGFR antibodies as part of the first-line therapy.
Findings
Activation of the epidermal growth factor receptor (EGFR) oncoprotein, a member of the ErbB family of receptor tyrosine kinases, is among the most common oncogenic driving events in human cancer [1]. Genomic mechanisms for activating the EGFR gene include nucleotide substitutions and in-frame insertions/deletions of the kinase domain in lung adenocarcinoma and papillary thyroid carcinomas, and multi-exonic deletions (exons 2 through 7: EGFR variant III or vIII), nucleotide substitutions of the extracellular domain and carboxyl terminal deletions in glioblastoma [2-6]. EGFR is also activated by high-copy amplifications in many epithelial cancer types, prominently in lung and upper gastrointestinal carcinomas as well as glioblastoma and head and neck cancer [7-10]. Furthermore, EGFR protein is over-expressed in many cancers even without evidence of focused genomic alteration, as observed in many cases of colorectal carcinoma where EGFR kinase domain mutations were found in only 3 out of 224 cases, 1.3% subjected to whole exome sequencing [11,12]. Given the elevated expression and genomic alterations present in EGFR, multiple cancer therapies have targeted EGFR, as both its kinase activity and its dependence on extracellular ligand signaling have rendered EGFR vulnerable to therapeutic intervention. FDA-approved EGFR targeted inhibitors include the low-molecular-weight ATP-competitive kinase inhibitors, such as gefitinib and erlotinib, and humanized monoclonal antibodies directed against the extracellular domain, notably cetuximab and panitumumab [13]. Although high-level expression of EGFR ligands and/or increased EGFR gene copy numbers may be predictive markers for antitumor response by cetuximab in colon cancer [14-16], and patients with RAS driven cancers are known not to benefit from cetuximab treatment, a clear molecular explanation of cancer response to cetuximab has remained elusive.
Genomic studies identify G724S mutant in colorectal carcinomas
Colorectal adenocarcinoma has been a classic model to study the progressive accumulation of genomic lesions leading to cellular transformation. Key genomic features of these tumors involve inactivation of tumor suppressors such as APC, TP53 and SMAD4 and mutational activation of oncogenes including KRAS, NRAS, BRAF and PIK3CA[17]. Given the role of cetuximab in therapy of these cancers, initial efforts to identify activating EGFR mutations identified few such events, though potentially activating events such as G719S were seen [18]. More recent reports have also identified potentially mutations of ERBB3[19] and amplifications and mutations of ERBB2 in CRC [12,20]. We have previously reported whole genome sequence analysis of nine colorectal carcinoma/normal pairs,leading to the identification of activating translocations of TCF7L2 and of the association of Fusobacterium nucleatum with colorectal carcinomas [21,22]. Here, we report genomic analysis of a tenth anonymized case of colorectal carcinoma. Whole genome sequencing was performed on the genomic DNA from colorectal carcinoma tissue and adjacent non-neoplastic colonic tissue to a median coverage of 32.5x and 34.2x coverage, respectively, with 86.8% of the genome sequenced to adequate depth for mutation calling.
An analysis of somatic genome structural alterations by comparison of tumor-derived and non-neoplastic derived sequences identified 63 somatic structural rearrangements, including a deletion of the APC tumor suppressor gene (Figure 1A, Additional file 1: Figure S1A, and Additional file 2: Table S1). Comparison of nucleotide sequences between the colorectal tumor and normal colon identified an overall mutation rate of 6.7 mutations/Mb including 18,401 somatic nucleotide substitutions, and 983 somatic insertions and deletions of < 37 bases (Figure 1B and Additional file 3: Table S2). As observed in other colorectal cancers [21,23,24], mutation analysis identified a marked elevation in the rate of C to T transitions at CpG dinucleotides (82/Mb). Analysis of non-synonymous coding mutations revealed a total of 119 alterations in 116 genes (Additional file 4: Table S3). Prominent mutations included a somatic R175H substitution in the TP53 tumor suppressor gene and a somatic G724S substitution in the EGFR oncogene (Figure 1B and Additional file 1: Figure S1B). Somatic mutations of common colorectal adenocarcinoma oncogenes KRAS, BRAF, NRAS and PIK3CA[23] were not detected.
Figure 1.
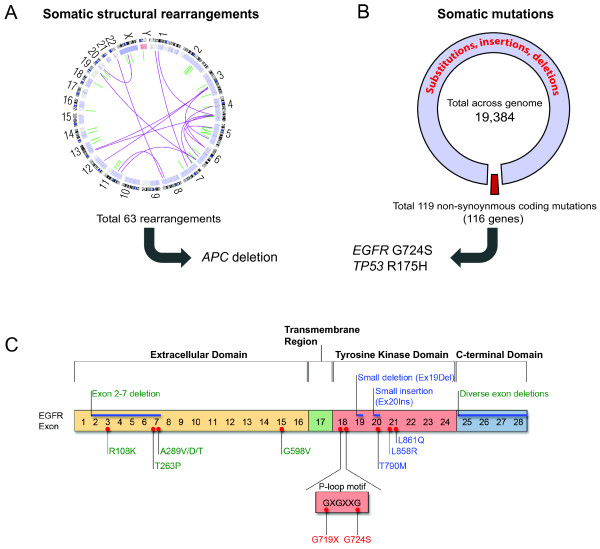
Identification of a somatic EGFR mutation in colorectal adenocarcinoma via whole genome sequencing. (A) Depiction of the somatic structural rearrangements in this colorectal cancer genome by a Circos plot. The chromosomes are depicted along the circle with somatic rearrangements depicted in purple (interchromosomal) and green (intrachromosomal), including a deletion at the APC tumor suppressor locus. (B) Depiction of numbers of candidate mutations and non-synonymous alterations in coding genes, and mutations in known cancer genes, TP53 and EGFR. (C) Schematic of somatic EGFR mutations found in glioblastoma (green lettering), lung adenocarcinoma (blue lettering) and colorectal adenocarcinoma (red lettering), with insertions and deletions above the domain structure, and substitution mutations below the domain structure indicated by red dots.
The absence of both KRAS and BRAF mutations are common features seen in colorectal cancers that are responsive to cetuximab [25,26], thus making the EGFR mutation in this case of particular interest. The somatic G724S mutation in EGFR occurs at the final glycine of the GxGxxG nucleotide-binding motif that is essential for ATP binding and is conserved among all protein kinases (Figure 1C) [27,28]. Substitution of EGFR G719, the first residue of this motif, to serine, cysteine, or alanine, has been observed in lung adenocarcinomas (~1%), and one G719S mutant and four G724S mutants have been reported in colorectal carcinomas that were sequenced for EGFR (Figure 1C) [18,29] (COSMIC database). In addition, these EGFR mutations were found to be mutually exclusive with well known KRAS, BRAF and PIK3CA oncogenic driver mutations, demonstrating their potential role in tumorigenesis (COSMIC database).
Colon-cancer derived G719S and G724S mutants are oncogenic and sensitive to cetuximab
To determine whether the G724S mutant is oncogenic and to evaluate its pharmacologic sensitivity, we generated this mutant in vitro and retrovirally transduced it into NIH-3T3 cells. While wild-type EGFR expressing NIH-3T3 cells form colonies in soft agar only in the presence of ligand, NIH-3T3 cells that express EGFR G724S form colonies in the absence of exogenous ligand, as do the lung and colon cancer-derived G719S mutants (Additional file 1: Figure S2A) [30]. Furthermore, both G719S and G724S mutants undergo constitutive tyrosine-phosphorylation, which is further increased by EGF treatment, whereas phosphorylation of wild-type EGFR requires induction by EGF (Additional file 1: Figure S2B). These data demonstrate that colon-cancer derived G719S and G724S mutants are oncogenically active in the absence of ligand stimulation.
To test whether G719S and G724S EGFR mutants are cetuximab-sensitive in vitro, we ectopically expressed these mutants in Ba/F3 cells, rendering these cells IL-3 independent but dependent on exogenous oncogenic EGFR signaling [31]. Ba/F3 cells expressing the colon-cancer derived G724S mutant and the lung/colon cancer-derived G719S mutant showed sensitivity to cetuximab with an IC50 value of ~ 0.3 μg/ml (Figure 2A). In contrast to their high cetuximab sensitivity, Ba/F3 cells dependent on EGFR G719S and G724S mutants were only moderately sensitive to erlotinib with an IC50 value of ~ 0.3 μM (Additional file 1: Figure S3A), consistent with previous reports on G719X mutants in vitro and in lung cancer clinical trials [30-33] and with the failure of a previously identified patient with EGFR G724S mutant colorectal cancer to respond to gefitinib [29].
Figure 2.
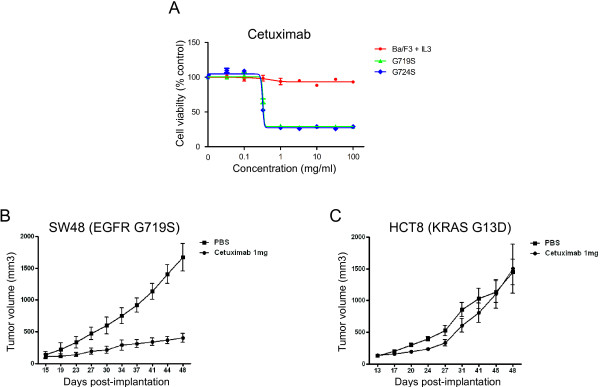
Pharmacological effects of cetuximab against oncogenic G719S and G724S mutants in vitro and in vivo. (A) Cetuximab suppresses the growth of Ba/F3 cells dependent upon the G719S and G724S mutants, but not control cells. Ba/F3 cells transformed with the indicated EGFR mutants were treated with cetuximab at the concentrations indicated and assayed for viability after 72 hours of drug treatment. The results are indicated as mean +/- SD of sextuplicate wells and are representative of three independent experiments (B and C) Cetuximab is effective against SW48 (EGFR G719S mutant)-induced tumors but not HCT8 (KRAS G13D mutant) induced-tumors in xenografted mice. BALB/c-nu/nu mice (6–8 weeks of age) were injected subcutaneously to the flank with 0.5 ~ 1x107 SW48 or HCT8 cells in 150 ~ 200 μl of PBS. Tumor sizes were measured two times a week using a Vernier caliper and tumor volumes were calculated according to the formula of (short diameter)2 x (long diameter)/2. When tumor volume reached around 100 ~ 150 mm3, mice were randomized into each group. After confirming that mean tumor volumes were not statistically different between two groups, mice were administered either with PBS or cetuximab (1 mg/mouse) intra-peritoneally twice a week.
In order to further examine the efficacy of cetuximab, we expanded our studies by generating xenograft mouse models with either SW48 or HCT8 colon cancer cells, which harbor either EGFR G719S or KRAS G13D mutation, respectively. Here, we found that consistent with in vitro response (Additional file 1: Figure S3B), cetuximab treatment dramatically suppressed tumor formation driven by SW48 cells (Figure 2B), suggesting the anti-tumor effect of cetuximab against tumors harboring EGFR G719S mutant. In contrast, cetuximab treatment was ineffective for the tumors driven by HCT8, which is consistent with the previous findings that KRAS-mutant tumors are insensitive to cetuximab (Figure 2C). Taken together, we found that G719S and G724S mutants are oncogenic in the absence of ligand stimulation and effectively respond to cetuximab in vivo and in vitro.
Asymmetric dimerization is required for oncogenic activity of G719S and G724S mutant
Recently, we reported that a subset of lung cancer-derived oncogenic EGFR mutants such as L858R require asymmetric dimerization for biochemical activation and oncogenic transforming activity, meaning that their oncogenic ability depend on formation of an EGFR homodimer in which two distinct regions of the two molecule dimerize [34]. By contrast, we showed that other EGFR mutants are oncogenic without the requirement for dimerization, including the gefitinib-resistant exon 20 insertion mutant and the T790M mutant [34]. Furthermore, we found that dimerization-dependent L858R mutant shows a dramatic response to cetuximab, whereas tumors driven by dimerization-independent mutants such as T790M are resistant to the antibody, suggesting that there is a close correlation between dimerization dependency of lung cancer-derived oncogenic mutant EGFR and pharmacological effects of cetuximab [34]. Given that colon cancer-derived G719S and G724S mutants are sensitive to cetuximab, we sought to examine whether oncogenic potential of these mutants are dependent on the asymmetric dimerization like lung cancer-derived L858R mutant.
To test the hypothesis that cetuximab sensitivity of G719S and G724S mutants is a function of their dimerization dependence, we generated G719S and G724S mutants with compound substitution mutations at the dimerization interface in the N-lobe or C-lobe that disrupt the asymmetric dimerization of EGFR [35]. Specifically, we generated epitope-tagged EGFR expression constructs that combined a receiver-impairing mutation (L704N) and/or an activator-impairing mutation (I941R) with oncogenic G719S and G724S mutants. The single or compound EGFR mutants were expressed in NIH-3T3 cells by retroviral transduction, and the EGFR mutant-expressing cells were assayed for their ability to grow in soft agar. In this system, the transforming ability of dimerization-dependent mutants is predicted to be abolished by cis mutation of the L704 or I941 mutations. Furthermore, co-expression of the L704N and I941R mutant forms, in contrast, is predicted to restore transforming ability that is dimerization-dependent, because the two mutant forms can heterodimerize. Therefore, this experiment allows us to test whether specific EGFR kinase domain mutants can induce cellular transformation in a dimerization dependent or independent fashion.
Dimerization-impairing cis mutations in EGFR, L704N and I941R, significantly reduced the ability of the cetuximab-sensitive G719S and G724S mutants to promote colony formation upon retroviral transduction (Figure 3A and B, L704N or I941R); colony-forming activity was partially or completely restored by co-expression of the L704N and I941R mutants in trans (Figure 3A and B, L704N&I941R). Consistent with these results, we found that constitutive and EGF-inducible autophosphorylation of the G719S and G724S mutants (Figures 3C and D, lanes 1 and 2), is attenuated by the introduction of L704N and I941R dimerization-impairing mutations (Figures 3C and D, lanes 3, 4, 5, and 6). Furthermore, receptor phosphorylation is partially rescued by co-expression of either G719S/L704N or G719S/I941R mutants or the cognate combination in a G724S mutant background (Figure 3C and D, lanes 7 and 8). Taken together, these data suggest that colon cancer-derived cetuximab-sensitive G719S and G724S mutants acquire their oncogenic potentials following asymmetric dimerization, respectively, which are similar to lung-cancer derived L858R mutant [35]. Furthermore, these results are consistent with our model that EGFR variants that are dependent on dimerization can be inhibited by cetuximab.
Figure 3.
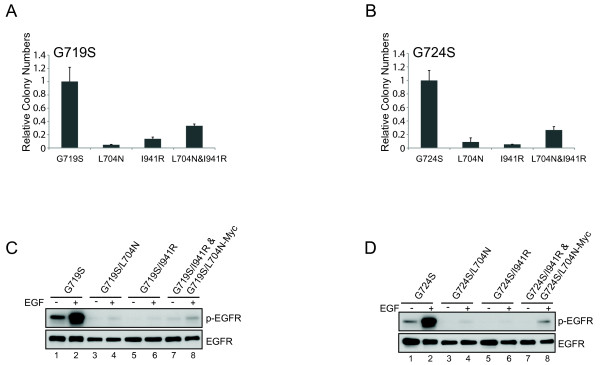
Dimerization disruption has effects on the transforming activity of G719S and G724S EGFR proteins. (A and B) G719S and G724S mutants are dependent on asymmetric dimerization for their transforming potential. NIH-3T3 cells expressing the indicated EGFR mutants with or without receiver-impairing (L704N) or/and activator-impairing (I941R) mutations were assayed for anchorage-independent growth in soft agar. The bar graph depicts the relative number of colonies in the dimerization-defective mutants normalized to the number of colonies formed by cells expressing the respective parental mutants (n = 3, mean + SD). (C and D) Ligand-induced and constitutive tyrosine-phosphorylation is abrogated on dimerization-impaired compound mutants of cetuximab-sensitive EGFR mutants. Whole cell lysates from the same cells analyzed in Figure 3A and B expressing G719S (C), and G724S (D) mutants with or/and without dimerization-impairing mutations (L704N or I941R) in the absence or presence of EGF treatment for 15 minutes (25 ng/ml) were subjected to immunoblotting with antibodies against phospho-tyrosine (4G10) and EGFR.
In summary, our findings suggest that EGFR mutation may underlie at least some cases of cetuximab responsiveness in colorectal carcinoma. While EGFR mutation has historically been believed to be rare in colorectal carcinomas, whole exome sequencing published through The Cancer Genome Atlas identified somatic non-synonymous coding EGFR mutations in 10 of 224 colorectal carcinoma cases (or 4.5%) [12]. While many such mutations may be passenger alterations that do not activate EGFR signaling, these results do speak to the potential for mutational activation of EGFR to result in susceptibility to anti-EGFR antibodies in a small fraction of CRC cases. Indeed, the recent demonstration of secondary somatic mutation in the EGFR extracellular domain conferring acquired resistance to cetuximab [36] is consistent with attribution of responses to cetuximab to EGFR blockade. Anti-EGFR therapy in metastatic colorectal cancer has been reserved for second-line therapy after failure of initial empiric chemotherapy but is now increasingly also used as part of first-line therapy for RAS wild-type patients. As genomic diagnostics enter into routine clinical practice, patients whose CRCs harbor potentially oncogenic EGFR mutations will be identified, including those at codons 719 and 724. These results suggest that in such patients, therapeutic approaches utilizing EGFR-directed antibody as part of their initial therapy should be evaluated given the greater potential dependence on EGFR signaling in these patients.
Competing interests
Relating to the content of this work, a patent titled “Methods of predicting response to EGFR antibody therapy” (WO2012065071 A2) was filed by the authors of this manuscript (JB, AB, JC, ML, MM, JT). MM: Inventor on a patent for EGFR mutation analysis in lung cancer, and a consultant to and equity holder in Foundation Medicine. The other authors declare that they have no competing interests.
Authors’ contributions
JC and AB conceived and designed study; performed experiments; analyzed and interpreted data; wrote the manuscript. ML, KC, NW, CS, DV and GG performed genomic analysis. MY, SO, JT, JJ, JB provided samples and coordinated sample preparation. AC, NK, AP, SL, JW and HH conducted in vivo and in vitro experiments. SG and ESL supervised the genomic analysis process. HG, ME and WP analyzed and interpreted data. MM conceived and designed study; analyzed and interpreted data; wrote the manuscript. All authors read and approved the final manuscript.
Supplementary Material
Supplemental Figures.
Somatic structural rearrangements identified in a colorectal adenocarcinoma whole genome sequence using the dRanger tool.
Somatic mutations and small insertions/deletions identified across the genome of a colorectal adenocarcinoma tumor using whole genome sequencing.
Somatic mutations predicted to cause non-synonymous changes in protein coding genes as identified from whole genome sequencing of a colorectal adenocarcinoma.
Contributor Information
Jeonghee Cho, Email: jeong.cho@skku.edu.
Adam J Bass, Email: Adam_Bass@dfci.harvard.edu.
Michael S Lawrence, Email: lawrence@broadinstitute.org.
Kristian Cibulskis, Email: kcibul@broadinstitute.org.
Ahye Cho, Email: ahye0619@gmail.com.
Shi-Nai Lee, Email: 33fantasy@greencross.com.
Mai Yamauchi, Email: Mai_Yamauchi@dfci.harvard.edu.
Nikhil Wagle, Email: NWAGLE@partners.org.
Panisa Pochanard, Email: panisa.pochanard@gmail.com.
Nayoung Kim, Email: nayoung718@skku.edu.
Angela KJ Park, Email: angela008@skku.edu.
Jonghwa Won, Email: agnes@greencross.com.
Hyung-Suk Hur, Email: hurhs@greencross.com.
Heidi Greulich, Email: Heidig@broadinstitute.org.
Shuji Ogino, Email: Shuji_Ogino@dfci.harvard.edu.
Carrie Sougnez, Email: carrie@broadinstitute.org.
Douglas Voet, Email: dvoet@broadinstitute.org.
Josep Tabernero, Email: jtabernero@vhio.net.
Jose Jimenez, Email: jjimenez@vhio.net.
Jose Baselga, Email: baselgaj@mskcc.org.
Stacey B Gabriel, Email: stacey@broadinstitute.org.
Eric S Lander, Email: eric@broadinstitute.org.
Gad Getz, Email: gadgetz@broadinstitute.org.
Michael J Eck, Email: eck@red.dfci.harvard.edu.
Woong-Yang Park, Email: woongyang@skku.edu.
Matthew Meyerson, Email: matthew_meyerson@dfci.harvard.edu.
Acknowledgements
We would like to thank all Meyerson lab members for thoughtful discussion. These works were in part supported by NCI R01 CA116020 (MM and MJE) and Samsung Medical Center intramural grant SGI-13-15 (JC).
References
- Hynes NE, Lane HA. ERBB receptors and cancer: the complexity of targeted inhibitors. Nat Rev Cancer. 2005;5:341–354. doi: 10.1038/nrc1609. [DOI] [PubMed] [Google Scholar]
- Chan SK, Gullick WJ, Hill ME. Mutations of the epidermal growth factor receptor in non-small cell lung cancer – search and destroy. Eur J Cancer. 2006;42:17–23. doi: 10.1016/j.ejca.2005.07.031. [DOI] [PubMed] [Google Scholar]
- Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, Harris PL, Haserlat SM, Supko JG, Haluska FG, Louis DN, Christiani DC, Settleman J, Haber DA. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–2139. doi: 10.1056/NEJMoa040938. [DOI] [PubMed] [Google Scholar]
- Pao W, Miller V, Zakowski M, Doherty J, Politi K, Sarkaria I, Singh B, Heelan R, Rusch V, Fulton L, Mardis E, Kupfer D, Wilson R, Kris M, Varmus H. EGF receptor gene mutations are common in lung cancers from "never smokers" and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci U S A. 2004;101:13306–13311. doi: 10.1073/pnas.0405220101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paez JG, Janne PA, Lee JC, Tracy S, Greulich H, Gabriel S, Herman P, Kaye FJ, Lindeman N, Boggon TJ, Naoki K, Sasaki H, Fujii Y, Eck MJ, Sellers WR, Johnson BE, Meyerson M. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–1500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- Cho J, Pastorino S, Zeng Q, Xu X, Johnson W, Vandenberg S, Verhaak R, Cherniack AD, Watanabe H, Dutt A, Kwon J, Chao YS, Onofrio RC, Chiang D, Yuza Y, Kesari S, Meyerson M. Glioblastoma-derived epidermal growth factor receptor carboxyl-terminal deletion mutants are transforming and are sensitive to EGFR-directed therapies. Cancer Res. 2011;71:7587–7596. doi: 10.1158/0008-5472.CAN-11-0821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirono Y, Tsugawa K, Fushida S, Ninomiya I, Yonemura Y, Miyazaki I, Endou Y, Tanaka M, Sasaki T. Amplification of epidermal growth factor receptor gene and its relationship to survival in human gastric cancer. Oncology. 1995;52:182–188. doi: 10.1159/000227455. [DOI] [PubMed] [Google Scholar]
- al-Kasspooles M, Moore JH, Orringer MB, Beer DG. Amplification and over-expression of the EGFR and erbB-2 genes in human esophageal adenocarcinomas. Int J Cancer. 1993;54:213–219. doi: 10.1002/ijc.2910540209. [DOI] [PubMed] [Google Scholar]
- Leonard JH, Kearsley JH, Chenevix-Trench G, Hayward NK. Analysis of gene amplification in head-and-neck squamous-cell carcinoma. Int J Cancer. 1991;48:511–515. doi: 10.1002/ijc.2910480406. [DOI] [PubMed] [Google Scholar]
- Cancer Genome Atlas Research N. Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature. 2008;455:1061–1068. doi: 10.1038/nature07385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spano JP, Lagorce C, Atlan D, Milano G, Domont J, Benamouzig R, Attar A, Benichou J, Martin A, Morere JF, Raphael M, Penault-Llorca F, Breau JL, Fagard R, Khayat D, Wind P. Impact of EGFR expression on colorectal cancer patient prognosis and survival. Ann Oncol. 2005;16:102–108. doi: 10.1093/annonc/mdi006. [DOI] [PubMed] [Google Scholar]
- Cancer Genome Atlas N. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–337. doi: 10.1038/nature11252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson KW, Sandler AB. EGFR tyrosine kinase inhibitors: difference in efficacy and resistance. Curr Oncol Rep. 2013;15:396–404. doi: 10.1007/s11912-013-0323-7. [DOI] [PubMed] [Google Scholar]
- Khambata-Ford S, Garrett CR, Meropol NJ, Basik M, Harbison CT, Wu S, Wong TW, Huang X, Takimoto CH, Godwin AK, Tan BR, Krishnamurthi SS, Burris HA 3rd, Poplin EA, Hidalgo M, Baselga J, Clark EA, Mauro DJ. Expression of epiregulin and amphiregulin and K-ras mutation status predict disease control in metastatic colorectal cancer patients treated with cetuximab. J Clin Oncol. 2007;25:3230–3237. doi: 10.1200/JCO.2006.10.5437. [DOI] [PubMed] [Google Scholar]
- Yonesaka K, Zejnullahu K, Lindeman N, Homes AJ, Jackman DM, Zhao F, Rogers AM, Johnson BE, Janne PA. Autocrine production of amphiregulin predicts sensitivity to both gefitinib and cetuximab in EGFR wild-type cancers. Clin Cancer Res. 2008;14:6963–6973. doi: 10.1158/1078-0432.CCR-08-0957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch FR, Herbst RS, Olsen C, Chansky K, Crowley J, Kelly K, Franklin WA, Bunn PA Jr, Varella-Garcia M, Gandara DR. Increased EGFR gene copy number detected by fluorescent in situ hybridization predicts outcome in non-small-cell lung cancer patients treated with cetuximab and chemotherapy. J Clin Oncol. 2008;26:3351–3357. doi: 10.1200/JCO.2007.14.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fearon ER. Molecular genetics of colorectal cancer. Annu Rev Pathol. 2011;6:479–507. doi: 10.1146/annurev-pathol-011110-130235. [DOI] [PubMed] [Google Scholar]
- Barber TD, Vogelstein B, Kinzler KW, Velculescu VE. Somatic mutations of EGFR in colorectal cancers and glioblastomas. N Engl J Med. 2004;351:2883. doi: 10.1056/NEJM200412303512724. [DOI] [PubMed] [Google Scholar]
- Jaiswal BS, Kljavin NM, Stawiski EW, Chan E, Parikh C, Durinck S, Chaudhuri S, Pujara K, Guillory J, Edgar KA, Janakiraman V, Scholz RP, Bowman KK, Lorenzo M, Li H, Wu J, Yuan W, Peters BA, Kan Z, Stinson J, Mak M, Modrusan Z, Eigenbrot C, Firestein R, Stern HM, Rajalingam K, Schaefer G, Merchant MA, Sliwkowski MX, de Sauvage FJ. et al. Oncogenic ERBB3 mutations in human cancers. Cancer Cell. 2013;23:603–617. doi: 10.1016/j.ccr.2013.04.012. [DOI] [PubMed] [Google Scholar]
- Dulak AM, Schumacher SE, van Lieshout J, Imamura Y, Fox C, Shim B, Ramos AH, Saksena G, Baca SC, Baselga J, Tabernero J, Barretina J, Enzinger PC, Corso G, Roviello F, Lin L, Bandla S, Luketich JD, Pennathur A, Meyerson M, Ogino S, Shivdasani RA, Beer DG, Godfrey TE, Beroukhim R, Bass AJ. Gastrointestinal adenocarcinomas of the esophagus, stomach, and colon exhibit distinct patterns of genome instability and oncogenesis. Cancer Res. 2012;72:4383–4393. doi: 10.1158/0008-5472.CAN-11-3893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass AJ, Lawrence MS, Brace LE, Ramos AH, Drier Y, Cibulskis K, Sougnez C, Voet D, Saksena G, Sivachenko A, Jing R, Parkin M, Pugh T, Verhaak RG, Stransky N, Boutin AT, Barretina J, Solit DB, Vakiani E, Shao W, Mishina Y, Warmuth M, Jimenez J, Chiang DY, Signoretti S, Kaelin WG, Spardy N, Hahn WC, Hoshida Y, Ogino S. et al. Genomic sequencing of colorectal adenocarcinomas identifies a recurrent VTI1A-TCF7L2 fusion. Nat Genet. 2011;43:964–968. doi: 10.1038/ng.936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostic AD, Gevers D, Pedamallu CS, Michaud M, Duke F, Earl AM, Ojesina AI, Jung J, Bass AJ, Tabernero J, Baselga J, Liu C, Shivdasani RA, Ogino S, Birren BW, Huttenhower C, Garrett WS, Meyerson M. Genomic analysis identifies association of Fusobacterium with colorectal carcinoma. Genome Res. 2012;22:292–298. doi: 10.1101/gr.126573.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjoblom T, Jones S, Wood LD, Parsons DW, Lin J, Barber TD, Mandelker D, Leary RJ, Ptak J, Silliman N, Szabo S, Buckhaults P, Farrell C, Meeh P, Markowitz SD, Willis J, Dawson D, Willson JK, Gazdar AF, Hartigan J, Wu L, Liu C, Parmigiani G, Park BH, Bachman KE, Papadopoulos N, Vogelstein B, Kinzler KW, Velculescu VE. The consensus coding sequences of human breast and colorectal cancers. Science. 2006;314:268–274. doi: 10.1126/science.1133427. [DOI] [PubMed] [Google Scholar]
- Wood LD, Parsons DW, Jones S, Lin J, Sjoblom T, Leary RJ, Shen D, Boca SM, Barber T, Ptak J, Silliman N, Szabo S, Dezso Z, Ustyanksky V, Nikolskaya T, Nikolsky Y, Karchin R, Wilson PA, Kaminker JS, Zhang Z, Croshaw R, Willis J, Dawson D, Shipitsin M, Willson JK, Sukumar S, Polyak K, Park BH, Pethiyagoda CL, Pant PV. et al. The genomic landscapes of human breast and colorectal cancers. Science. 2007;318:1108–1113. doi: 10.1126/science.1145720. [DOI] [PubMed] [Google Scholar]
- Karapetis CS, Khambata-Ford S, Jonker DJ, O'Callaghan CJ, Tu D, Tebbutt NC, Simes RJ, Chalchal H, Shapiro JD, Robitaille S, Price TJ, Shepherd L, Au HJ, Langer C, Moore MJ, Zalcberg JR. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008;359:1757–1765. doi: 10.1056/NEJMoa0804385. [DOI] [PubMed] [Google Scholar]
- De Roock W, Claes B, Bernasconi D, De Schutter J, Biesmans B, Fountzilas G, Kalogeras KT, Kotoula V, Papamichael D, Laurent-Puig P, Penault-Llorca F, Rougier P, Vincenzi B, Santini D, Tonini G, Cappuzzo F, Frattini M, Molinari F, Saletti P, De Dosso S, Martini M, Bardelli A, Siena S, Sartore-Bianchi A, Tabernero J, Macarulla T, Di Fiore F, Gangloff AO, Ciardiello F, Pfeiffer P. et al. Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol. 2010;11:753–762. doi: 10.1016/S1470-2045(10)70130-3. [DOI] [PubMed] [Google Scholar]
- Hanks SK, Hunter T. Protein kinases 6. The eukaryotic protein kinase superfamily: kinase (catalytic) domain structure and classification. FASEB J. 1995;9:576–596. [PubMed] [Google Scholar]
- Hemmer W, McGlone M, Tsigelny I, Taylor SS. Role of the glycine triad in the ATP-binding site of cAMP-dependent protein kinase. J Biol Chem. 1997;272:16946–16954. doi: 10.1074/jbc.272.27.16946. [DOI] [PubMed] [Google Scholar]
- Ogino S, Meyerhardt JA, Cantor M, Brahmandam M, Clark JW, Namgyal C, Kawasaki T, Kinsella K, Michelini AL, Enzinger PC, Kulke MH, Ryan DP, Loda M, Fuchs CS. Molecular alterations in tumors and response to combination chemotherapy with gefitinib for advanced colorectal cancer. Clin Cancer Res. 2005;11:6650–6656. doi: 10.1158/1078-0432.CCR-05-0738. [DOI] [PubMed] [Google Scholar]
- Greulich H, Chen TH, Feng W, Janne PA, Alvarez JV, Zappaterra M, Bulmer SE, Frank DA, Hahn WC, Sellers WR, Meyerson M. Oncogenic transformation by inhibitor-sensitive and -resistant EGFR mutants. PLoS Med. 2005;2:e313. doi: 10.1371/journal.pmed.0020313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang J, Greulich H, Janne PA, Sellers WR, Meyerson M, Griffin JD. Epidermal growth factor-independent transformation of Ba/F3 cells with cancer-derived epidermal growth factor receptor mutants induces gefitinib-sensitive cell cycle progression. Cancer Res. 2005;65:8968–8974. doi: 10.1158/0008-5472.CAN-05-1829. [DOI] [PubMed] [Google Scholar]
- Han SW, Kim TY, Hwang PG, Jeong S, Kim J, Choi IS, Oh DY, Kim JH, Kim DW, Chung DH, Im SA, Kim YT, Lee JS, Heo DS, Bang YJ, Kim NK. Predictive and prognostic impact of epidermal growth factor receptor mutation in non-small-cell lung cancer patients treated with gefitinib. J Clin Oncol. 2005;23:2493–2501. doi: 10.1200/JCO.2005.01.388. [DOI] [PubMed] [Google Scholar]
- Sequist LV, Besse B, Lynch TJ, Miller VA, Wong KK, Gitlitz B, Eaton K, Zacharchuk C, Freyman A, Powell C, Ananthakrishnan R, Quinn S, Soria JC. Neratinib, an irreversible pan-ErbB receptor tyrosine kinase inhibitor: results of a phase II trial in patients with advanced non-small-cell lung cancer. J Clin Oncol. 2010;28:3076–3083. doi: 10.1200/JCO.2009.27.9414. [DOI] [PubMed] [Google Scholar]
- Cho J, Chen L, Sangji N, Okabe T, Yonesaka K, Francis JM, Flavin RJ, Johnson W, Kwon J, Yu S, Greulich H, Johnson BE, Eck MJ, Janne PA, Wong KK, Meyerson M. Cetuximab response of lung cancer-derived EGF receptor mutants is associated with asymmetric dimerization. Cancer Res. 2013;73:6770–6779. doi: 10.1158/0008-5472.CAN-13-1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Gureasko J, Shen K, Cole PA, Kuriyan J. An allosteric mechanism for activation of the kinase domain of epidermal growth factor receptor. Cell. 2006;125:1137–1149. doi: 10.1016/j.cell.2006.05.013. [DOI] [PubMed] [Google Scholar]
- Montagut C, Dalmases A, Bellosillo B, Crespo M, Pairet S, Iglesias M, Salido M, Gallen M, Marsters S, Tsai SP, Minoche A, Seshagiri S, Serrano S, Himmelbauer H, Bellmunt J, Rovira A, Settleman J, Bosch F, Albanell J. Identification of a mutation in the extracellular domain of the Epidermal Growth Factor Receptor conferring cetuximab resistance in colorectal cancer. Nat Med. 2012;18:221–223. doi: 10.1038/nm.2609. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figures.
Somatic structural rearrangements identified in a colorectal adenocarcinoma whole genome sequence using the dRanger tool.
Somatic mutations and small insertions/deletions identified across the genome of a colorectal adenocarcinoma tumor using whole genome sequencing.
Somatic mutations predicted to cause non-synonymous changes in protein coding genes as identified from whole genome sequencing of a colorectal adenocarcinoma.


