Abstract
We report the case of a 37-year-old man with isolated unilateral absence of the pulmonary artery (UAPA), which was diagnosed upon the occurrence of hemoptysis. Plain chest radiography demonstrated decreased left pulmonary volume. Computed tomography of the chest revealed the complete absence of the left pulmonary artery. Angiography revealed marked dilation of the left bronchial artery, inferior phrenic artery, internal thoracic artery, and the arterial branches of the thyrocervical trunk. These arteries were considered as collateral circulation to the left lung. In cases with UAPA, collateral circulation should be evaluated by angiography to obtain useful information for treatment.
Keywords: pulmonary artery, hemoptysis, angiography
Introduction
Unilateral absence of the pulmonary artery (UAPA) is a rare congenital malformation,1) which is often associated with cardiac malformation.2) In the absence of associated cardiac malformation, the condition may be asymptomatic until adult age.3,4) We encountered a case with isolated UAPA, which was diagnosed upon the occurrence of hemoptysis, and angiography was subsequently performed.
Case Report
A 37-year-old man with no previous medical history presented with hemoptysis and pressure discomfort in the left chest. Upon admission, his temperature was 36.8°C, respiratory rate was 18/min, pulse rate was 62 beats/min, blood pressure was 126/68 mmHg, and oxygen saturation level was 99% (room air). No clinical signs of cyanosis, edema or clubbing of the fingers were found. Rhonchi were noted all over the left chest. Cardiac examination revealed normal heart sounds without murmurs.
Laboratory tests showed the following results: leukocytes 7660/µL, hemoglobin 14.5 g/dL, platelets 41.8 × 104/µL, albumin 4.2 g/dL, creatinine 0.88 mg/dL, C-reactive protein 0.20 mg/dL, brain natriuretic peptide 24 pg/mL, activated partial thromboplastin time 24.6 sec, prothrombin time 95%, fibrinogen 378 mg/dL, and D-dimer 1.2 µg/mL.
The chest X-ray demonstrated decreased left pulmonary volume and leftward deviation of the mediastinum (Fig. 1A). The contrast-enhanced computed tomography (CT) scan in the mediastinal window revealed the absence of a left pulmonary artery and the presence of a right aortic arch (Fig. 1B and 1C). No cardiac malformation was detected by ultrasound. Bronchoscopy revealed dilated mucosal capillary vessels in all the observable bronchi in the left lung (Fig. 2A and 2B). There were no abnormal findings within the bronchial lumen. Spirometry showed a predicted vital capacity (VC) of 82.2%, and a ratio of forced expiratory volume in 1 second to the forced vital capacity (FEV1/FVC) of 83.5%.
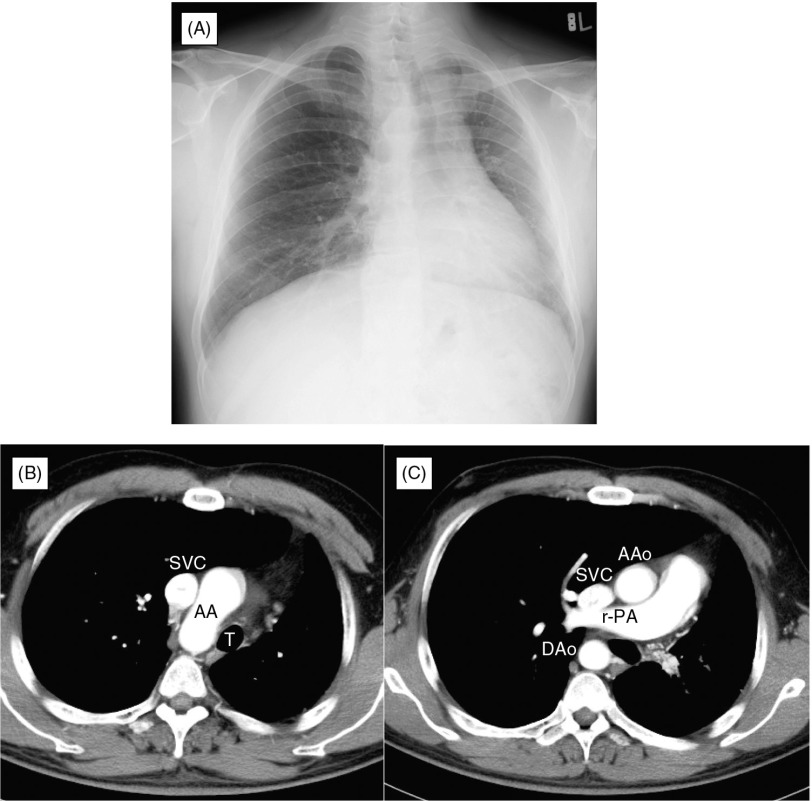
Fig. 1.
(A) Plain chest radiograph: Decreased left pulmonary volume and leftward deviation of the mediastinum are present. (B, C) Contrast-enhanced chest computed tomography scan in the mediastinal window: The left pulmonary artery is absent and the right aortic arch is present. AA: aortic arch; T: trachea; SVC: inferior vena cava; r-PA: right pulmonary artery; AAo: ascending aorta; DAo: descending aorta.
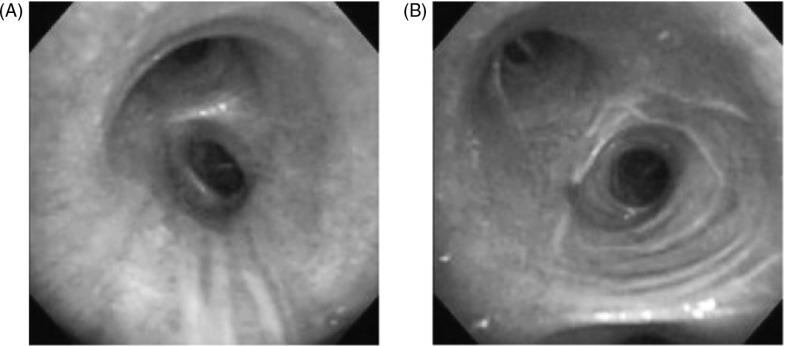
Fig. 2.
Bronchoscopy revealed dilated mucosal capillary vessels surrounding all the observable bronchi in the left lung. (A) The second carina. (B) The orifice of the left upper lobe bronchus.
Based on the above findings, a diagnosis of isolated UAPA was made. Therefore, we performed angiography to evaluate vascular lesions that could produce the hemoptysis and also to examine collateral circulation.
Angiography: In angiography of the pulmonary artery, while the right pulmonary artery could be depicted, the left pulmonary artery was completely absent from the point of origin (Fig. 3A). Pressure in the pulmonary trunk was 43/19 (average 27) mmHg. A markedly dilated left bronchial artery originated from the thoracic descending aorta at the level of the tracheal bifurcation (Fig. 3B). Particularly, blood vessels to the left superior lobe were dilated and tortuous. The left inferior phrenic artery was also highly dilated and collateral vessels ascending along the left pulmonary basilar region and left cardiac margin were depicted (Fig. 3C). Angiography of the left subclavian artery demonstrated a highly dilated and tortuous left internal thoracic artery (Fig. 3D). The vessels that originated from the thyrocervical trunk and were distributed to the left aspect of the trachea were also dilated.
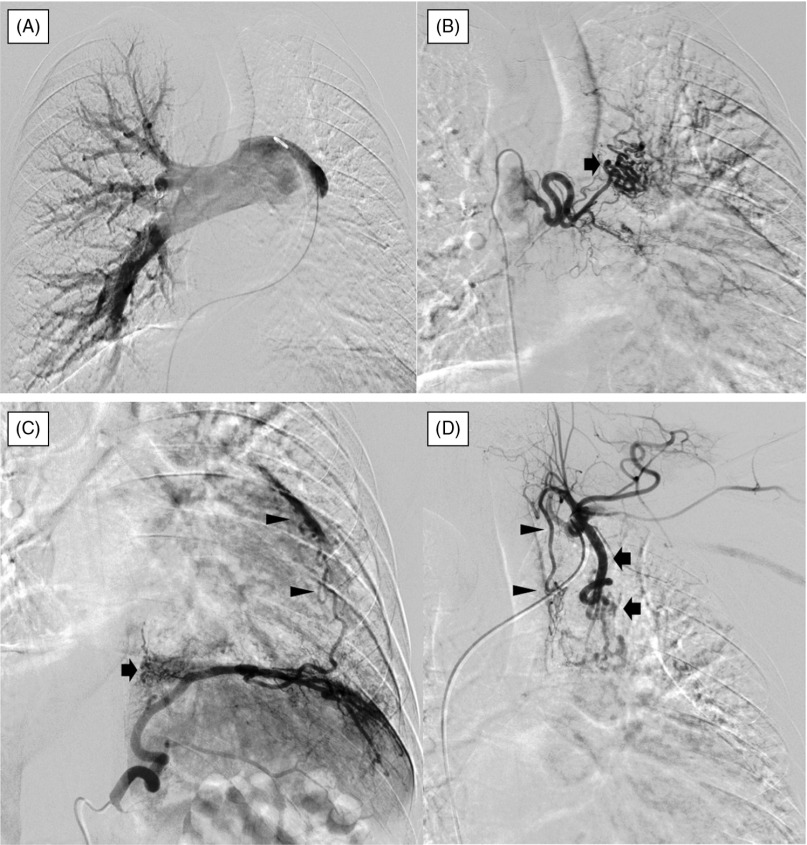
Fig. 3.
Angiography. (A) Angiography of the pulmonary artery: Although the right pulmonary artery is depicted, the left pulmonary artery is completely absent from its origin. (B) Angiography of the left bronchial artery: The artery originates from the descending thoracic aorta at the level of the tracheal bifurcation and is highly dilated. Blood vessels to the left superior lobe were dilated and tortuous (arrow). (C) Angiography of the left inferior phrenic artery: The inferior phrenic artery is highly dilated and collateral vessels ascending along the left pulmonary basilar region (arrow) and left cardiac margin (arrowheads) are depicted. (D) Angiography of the left subclavian artery: The left internal thoracic artery is highly dilated and tortuous (arrows). The vessels that originate from the thyrocervical trunk and are distributed to the left aspect of the trachea are dilated (arrowheads).
On digital subtraction angiography of the left bronchial artery, left inferior phrenic artery, and left subclavian artery, the pulmonary vein was depicted on the venous phase. Hence, these arteries were considered as collateral circulation.
This was the first episode of hemoptysis in this case, and as the amount was small, oral nifedipine was administered as a vasodilator for conservative treatment of pulmonary hypertension.
Discussion
UAPA represents a congenital malformation first reported by Fraentzel in 1868.5) This condition is likely to be associated with cardiac malformation, such as the tetralogy of Fallot, ventricular septal defect, transposition of great vessels, and aortic arch anomalies,2,4) but may also occur in isolation.4) Bouros, et al.1) investigated chest radiographs collected from 600000 subjects to determine the incidence and reported that UAPA was found in 6 cases, of which 3 had no cardiac malformation (0.0005%).
The embryological basis of UAPA is as follows.6) The pulmonary artery branches are formed from the 6th aortic arches in embryos at approximately the 4th week of gestation. During normal development, the proximal portions of the 6th arches persist, forming the right and left main branches of the pulmonary trunk. On the right side, the distal portion of the 6th arch disappears, while on the left side, the distal portion persists as the ductus arteriosus. The pulmonary vascular bed is established separately and is not dependent on the 6th arch for its development. This pulmonary plexus of vessels is connected in its early stages to the ventral branches of the dorsal aorta. These systemic connections normally disappear at a later stage of development, and the pulmonary vascular bed is then supplied by the developing branches of the right and left pulmonary arteries. Disappearance of the proximal portion of either the right or left 6th arch results in the absence of a main branch of the pulmonary artery. The peripheral pulmonary vessels, including the pulmonary veins, may form normally even when a main branch of the pulmonary artery is absent, because they develop independently. In such a case, the above-mentioned systemic connections become dilated, and the bronchial artery, intercostal artery, subclavian artery, and inferior phrenic artery function as the collateral circulation of the pulmonary arteries on the affected side.7) Ten, et al.4) reported that the deficiency was more common on the right (67%) than on the left (37%). Furthermore, 3 of the 108 patients with UAPA had an absent pulmonary artery on the same side as that of the aortic arch, suggesting that in most cases of UAPA, the pulmonary artery is absent on the side opposite to that of the aortic arch.
With regard to symptoms, Ten, et al.4) reported dyspnea or exercise limitation in 40% of cases, frequent respiratory infections in 37%, and hemoptysis in 20%. In addition, 15%4) to 24%3) of cases were reported to be asymptomatic. Hemoptysis, which was also seen in our case, is presumed to be caused by excessive collateral circulation and fragility of the vessels including the capillary bed.8)
Angiography is suitable for evaluation of the collateral circulation, and also contributes greatly to treatment. Although hemoptysis is likely to resolve naturally,7) in cases where repeated hemoptysis is observed, angiography is used to evaluate the collateral circulation, and the blood vessels responsible for the hemoptysis are embolized.9) If hemoptysis recurs after the embolization, pneumonectomy may be performed.4) Evaluation of the collateral circulation using angiography will also provide useful information for handling blood vessels during surgery.10)
Ten, et al.4) reported that pulmonary hypertension was found in 44% of isolated UAPA cases. Inability of the decreased pulmonary vascular bed to cope with increased blood flow leads to pulmonary hypertension.3) Many patients with UAPA can remain asymptomatic for a long time, but the development of pulmonary hypertension may preclude long-term survival, and the overall mortality rate of UAPA was reported to be 7%.4) Our case was isolated UAPA without cardiac malformation, which was detected when hemoptysis occurred. The patient presented with pulmonary hypertension when he visited our hospital. Isolated UAPA may have an asymptomatic course until adulthood, so by the time symptoms appear, the disease may have progressed to include pulmonary hypertension. Such cases require clinical caution.
Conclusions
On imaging of the chest for hemoptysis, if an abnormal shadow is not observed in the lung field and lung volume reduction is observed on one side, the possibility of UAPA should be taken into account. In such cases, collateral circulation should be evaluated by angiography to obtain useful information for treatment.
Acknowledgements
The authors are indebted to Dr. Helena Popiel (MS, PhD, Lecturer) and Dr. Edward F. Barroga (DVM, PhD, Associate Professor) of the Department of International Medical Communications of Tokyo Medical University for their editorial review of the English manuscript.
Disclosure Statement
The authors declare that they have no conflict of interest associated with this study.
References
- Bouros D, Pare P, Panagou P, et al. The varied manifestation of pulmonary artery agenesis in adulthood. Chest 1995; 108: 670-6 [DOI] [PubMed] [Google Scholar]
- Komatsu Y, Hanaoka M, Ito M, et al. Unilateral absence of the pulmonary artery incidentally found after an episode of hemoptysis. Intern Med 2007; 46: 1805-8 [DOI] [PubMed] [Google Scholar]
- Koga H, Hidaka T, Miyako K, et al. Age-related clinical characteristics of isolated congenital unilateral absence of a pulmonary artery. Pediatr Cardiol 2010; 31: 1186-90 [DOI] [PubMed] [Google Scholar]
- Ten Harkel AD, Blom NA, Ottenkamp J. Isolated unilateral absence of a pulmonary artery: a case report and review of the literature. Chest 2002; 122: 1471-7 [DOI] [PubMed] [Google Scholar]
- Fraentzel O. Ein Fall von abnormer Communication der Aorta mit der Arteria pulmonalis. Virchows Arch 1868; 43: 420-6 [Google Scholar]
- Sherrick DW, Kincaid OW, Dushane JW. Agenesis of a main branch of the pulmonary artery. Am J Roentgenol Radium Ther Nucl Med 1962; 87: 917-28 [PubMed] [Google Scholar]
- Lin YM, Liang KW, Ting CT. Unilateral pulmonary artery agenesis with presentation of hemoptysis: a case report. Zhonghua Yi Xue Za Zhi (Taipei) 1999; 62: 644-7 [PubMed] [Google Scholar]
- de Mello Junior WT, Coutinho Nogueira JR, Santos M, et al. Isolated absence of the right pulmonary artery as a cause of massive hemoptysis. Interact Cardiovasc Thorac Surg 2008; 7: 1183-5 [DOI] [PubMed] [Google Scholar]
- Reñé M, Sans J, Dominguez J, et al. Unilateral pulmonary artery agenesis presenting with hemoptysis: treatment by embolization of systemic collaterals. Cardiovasc Intervent Radiol 1995; 18: 251-4 [DOI] [PubMed] [Google Scholar]
- Ohtsuka T, Nomori H, Watanabe K, et al. Isolated unilateral absence of a pulmonary artery treated by pneumonectomy in an adult: report of a case. Surg Today 2006; 36: 525-7 [DOI] [PubMed] [Google Scholar]