Abstract
Background
While evidence suggests that depression is associated with medical morbidity and mortality, the potential role of mania has received less attention. This analysis evaluated the association between manic spectrum episodes and risk of all-cause mortality over a 26-year follow-up in a population-based study.
Methods
Participants included 14,870 adults (mean age 48.2 ± 20.3; 58.2% female; 31.1% non-white) from 4 sites of the Epidemiologic Catchment Area Study who completed the Diagnostic Interview Schedule (DIS) mania assessment between 1980 and 1983 and had vital status data available through 2007. Participants were grouped into 4 mutually exclusive categories based on DIS mania assessment: 1) manic episode (n=46); 2) hypomanic episode (n =195); 3) sub-threshold manic symptoms (n =1,041); and 4) no manic spectrum episodes (n =13,588). To determine vital status, participants were matched with the National Death Index. Participants with manic spectrum episodes were compared to those without such episodes with regard to mortality after 26 years.
Results
After adjusting for major depressive symptoms and demographic differences, odds of mortality at follow-up for participants with lifetime manic spectrum episodes in the 30-44 and 45-64 year age cohorts at baseline were higher than those with no lifetime manic spectrum episodes in the same age cohorts (OR=1.39, 95% CI = [1.00, 1.93] and OR=1.41, 95% CI = [1.02, 1.95] respectively).
Conclusions
History of lifetime manic spectrum episodes in early to mid adulthood is associated with increased risk of all-cause mortality in mid to late life.
Limitations
Future studies of mania and mortality should evaluate specific causes of mortality.
Keywords: Mania, Bipolar Disorder, ECA, Manic Spectrum, Mortality, Diagnostic Interview Schedule
1. Introduction
Multiple studies have examined depression as a risk factor for mortality, and several systematic reviews have supported a positive association between depression and mortality (Lawson et al., 1999, Cuijpers and Smit, 2002, Sax and Dewwy, 2001, Cole et al., 1999). Meta-analyses have estimated a mortality rate among psychiatric inpatients and outpatients with depression that is 2.7 times higher as compared to the general population (Lawson et al., 1999) and 1.8 times higher for depressed compared to non-depressed individuals in the community (Cuijpers and Smit, 2002). Studies of depression in the community also support the association between minor and subclinical depression with increased risk of mortality (Cuijpers and Smit, 2002, Anda et al., Zonderman et al., 1989, Thomas et al., 1992, Simonsick et al., 1995, Barefoot and Schroll, 1996, Pennix et al., 1999). These findings suggest that the association between depression and mortality may extend beyond cases of depression that are severe enough to result in hospitalization and includes milder cases identified among individuals in the community.
While many community-based studies have evaluated the association between depression and mortality, most studies examining the relationship between bipolar disorder and mortality are based on data from case-registers of patients diagnosed with bipolar disorder at a psychiatric or other health facility. Most of these studies have concluded that bipolar disorder is associated with an increased risk of all-cause and cause-specific mortality (Osby et al., 2001, Hoyer et al., 2000, Sharma and Markar, 1994, Black et al., 1987a, Laursen et al., 2007, Hoang et al., 2011, Chang et al., 2011, Angst et al., 2002, Tsai et al., 2005, Laursen, 2011). However, findings from previous case-register studies supporting an association between bipolar disorder and mortality can only be generalized to cases severe enough to warrant inpatient or outpatient treatment and not to the many individuals with bipolar disorder in the community who do not seek treatment or only rarely seek treatment. Past research indicates that many individuals with bipolar disorder are not diagnosed properly and do not receive proper psychiatric care (McAlpine and Mechanic, 2000, Hirschfelt, et al., 2003, Kupfer et al., 2002). The average delay between onset of bipolar disorder symptoms and proper diagnosis and treatment has been estimated to be as long as six to eight years, suggesting that there are many symptomatic but undiagnosed individuals in the community (Wang et al., 2005). Additionally, it has been estimated that only 32% of those meeting diagnostic criteria for bipolar I or bipolar II disorders had sought treatment in the past 12 months (Regier et al., 1993). Therefore, studies that extend beyond clinical populations are needed to fully understand the association between bipolar disorder and mortality in the general population. Furthermore, although the community prevalence of bipolar disorder type I and II account for an estimated 1-2% of the general population (Regier et al., 1993, Kessler, 1994), the latest evidence suggests that the prevalence of bipolar spectrum disorders may be as high as 6.4% (Judd and Akiskal, 1998). This higher prevalence takes into account subtler or milder presentations of manic symptoms that are common but often do not receive medical attention. However, the risk of increased mortality related to bipolar spectrum episodes in the community has not yet been investigated.
While research supports the association between unipolar depression and mortality as discussed above, the role of mania has received less attention. Individuals with bipolar disorder spend a substantial amount of their lifetime in both depressed (up to 31%) and manic (up to 9%) mood states (Judd et al., 2002), and it is possible that both depressed and manic mood states are independently responsible for the association between bipolar disorder and physical morbidities and mortality. To our knowledge, no study to date has examined risk of mortality in the community across the full spectrum of manic episodes either in the context of bipolar disorder or independent of a major depressive episode. Here we determined the association between manic spectrum symptoms and 26-year all-cause mortality in a large population-based study.
2. Methods
2.1 Study Sample
The Epidemiologic Catchment Area (ECA) Program of research was initiated in response to the 1978 report of the President’s Commission on Mental Health (President’s Commission on Mental Health, 1978). The purpose was to collect data on the prevalence and incidence of mental disorders and on the use of and need for services by the mentally ill in a nationally representative sample. Initial data collection for the ECA Program took place across five sites (Baltimore, MD, Durham, NC, Los Angeles, CA, New Haven, CT, and St. Louis, MO) between 1980 and 1983. The study was comprised of a household survey and an institutional survey at each site and included a structured psychiatric diagnostic interview. Further details about the methods (Eaton and Kessler, 1985) and results (Robins and Regier, 1991) of the ECA study can be found elsewhere.
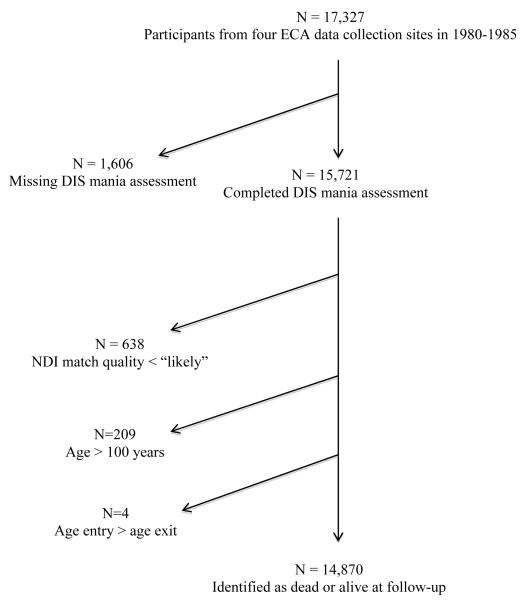
Of the five original sites, four (all except Los Angeles, CA) contributed data from which we could ascertain vital status. Our research team used this information to collect data on mortality of respondents through 2007 for these four sites. Participants were excluded if they: 1) had missing or incomplete data on the mania assessment section of the structured psychiatric interview (N=1,606) (see section 2.2); 2) had a less than “likely” quality of match with the National Death Index (N=638) (see section 2.3); or 3) were projected to be over 100 years old at follow-up (N=209) (these participants were more likely to be deceased but not located). An additional four participants were excluded for apparent data entry errors where age of entry into the study was greater than the recorded age of death. Therefore, the sample for this analysis consisted of 14, 870 of the original 17,327 participants from the four study sites (Figure 1).
Figure 1.
Flow chart for study sample inclusion/exclusion
2.2 Psychiatric assessment: Diagnostic Interview Schedule (DIS) (Robins et al., 1982)
The DIS is a structured interview designed to be administered by a trained lay interviewer and consists mostly of questions with yes/no response options designed to diagnose mental disorders based on the DSM-III criteria. Although the DIS has demonstrated high specificity in validation studies comparing DIS diagnosis of bipolar disorder to that of a psychiatrist, specificity varied a great deal across studies (15%-60%) (Eaton and Kessler, 1985, Robins and Regier, 1991, Robins et al., 1982, Greist et al., 1987). Because our goal was to assess the risk of mortality across the full manic spectrum, we chose to include all DIS mania symptoms in our analysis, not just the full criteria for a DMS-III manic episode or bipolar disorder. For this analysis, participants were grouped into four mutually exclusive categories based on their responses to eight questions on the DIS designed to capture the DSM-III diagnostic criteria for a manic episode, as done previously by Judd and Akiskal (1998). These four groups are described below.
Participants with a history of one or more manic episodes (ManEp; N=46)
Participants in this group met DSM-III criteria for one or more lifetime manic episodes at the time of the ECA study assessment. Specifically, these participants reported having an elevated, expansive or euphoric mood for a week or more (DIS question 100) in addition to at least three other co-occurring manic symptoms, or at least four other manic symptoms if they reported irritable mood (DIS question 110A). These participants also were required to meet the severity criterion of help-seeking behavior or impairment in functioning (DIS questions 113-113C). Additionally, to meet DSM-III criteria for a manic episode, the symptoms could not be attributable to an organic brain disorder, or to drug or alcohol use.
Participants with a history of one or more hypomanic episodes (HypoEp; N=195)
Participants in this group were required to report an elevated, expansive or euphoric mood for a week or more during their lifetime in addition to at least three other cooccurring manic symptoms, or at least four other manic symptoms if they reported irritable mood. Unlike the participants in the “manic episode” group, however, they did not meet the severity criterion for a manic episode (i.e., did not report seeking professional help, taking medication or experiencing significant impairment in life or activities due to symptoms, DIS questions 113-113C).
Participants with a history of sub-threshold manic symptoms (SubManEp; N=1,041)
Participants in this group reported experiencing two or more manic symptoms during their lifetime but did not meet the criteria for a manic or a hypomanic episode as described above.
Participants with no history of manic spectrum episodes (NoManEp; N=13,588)
Participants in this group reported only one or no lifetime manic symptoms.
2.3 Vital Status Assessment
Vital status from the date of interview in 1980-83 through 2007 was ascertained by matching participants with the National Death Index (NDI) (Fillenbaum et al., 2009). Fields for matching included first and last name, sex, race, date of birth, social security number, and father’s surname. Vital status of 97.8% of deceased participants was determined using this method. An additional 82 participants were identified as deceased by matching to the Social Security Death Index (Hill and Rosenwaike, 2001). Within the Baltimore site, records of 53 additional deaths were obtained through fieldwork during the 1993-96 and 2003-04 follow-up interviews that took place only at this study site. The quality of the match between the ECA study participant and the NDI or other search methods was coded on a scale from “definite” to “unconfirmed” (Fillenbaum et al., 2009). Participants were only included in this analysis if their match quality was deemed to be “likely” or better. Age of death for deceased participants was calculated from the date of birth and the recorded date of death. In cases where date of birth was not available, age of death was determined based on age at interview in 1980-83 and date of death. Participants were classified as alive if they were not matched through NDI or other methods and were under 100 years of age.
2.4 Other variables
Other demographic variables collected included participants’ age at first interview (1980-1983 depending on study site), sex, race, marital status, and years of education. History of mental disorders over the lifetime was ascertained from participants’ responses to items in the DIS relevant to the DSM-III depressive symptoms, alcohol abuse/dependence and non-alcohol drug abuse/dependence.
2.5 Statistical Analyses
We compared demographic characteristics of the four groups using Fisher’s exact test for categorical variables and Analysis of Variance (ANOVA) for continuous variables. When significant differences (p<0.05) between groups were identified, we determined pairwise differences with a Tukey-HSD test for continuous variables and a linear combination estimator for categorical variables. After observing significant pairwise differences for each of the manic spectrum episode groups when compared to the NoManEp group, we combined the three manic spectrum groups to form a “lifetime manic spectrum episodes” group (AnyManEp) to evaluate odds of mortality compared with the NoManEp group. To examine the association between lifetime manic spectrum episodes and mortality after adjusting for other risk factors we performed a series of logistic regression analyses. Demographic characteristics, lifetime depressive symptoms, history of alcohol and non-alcohol abuse/dependence that were significant predictors of mortality in univariate analyses were entered as covariates in the multivariate models with lifetime manic spectrum episodes as the primary predictor.
To assess risk of mortality in the AnyManEp group compared to the NoManEp group, we had initially planned to conduct a survival analysis using a Cox proportional hazards model, but had to abandon this strategy when Schoenfeld’s global test revealed that the assumption of proportional hazards was not met. Instead, we stratified the sample into four age categories based on participants’ age at enrollment (<30, 30-44, 45-64, ≥65 years), as has been done in previous studies of bipolar disorder and mortality (Pennix et al., 1999, Laursen et al., 2007, Hoang et al., 2011, Chang et al., 2011). Stratifying by age allowed us to control for heterogeneity in age of entry into the study, which ranged from 18-98 years, and to account for survival bias, especially in the oldest cohort (≥65 years). We conducted age-stratified logistic regression analyses to compare the AnyManEp group to the NoManEp group in different age cohorts with respect to odds of mortality over the 26-year follow up. To control for potential confounders within the age-stratified regression models, we adjusted for demographic characteristics (Model 1), then added depressive symptoms (Model 2), and alcohol and non-alcohol abuse/dependence (Model 3). All statistical analyses were performed using Stata software, version11 (StataCorp, College Station, TX).
3. Results
The NoManEp group differed from all three manic spectrum episode groups on all demographic and health behavior variables except education (Table 1). Specifically, the NoManEp group was older at entry into the study, more likely to be Caucasian, female and married, and less likely to have a lifetime history of depressive symptoms, alcohol abuse/dependence, and non-alcohol drug abuse/dependence. At follow up, the proportion of deaths was higher within the NoManEp group (42.9%) compared to each of the manic spectrum episode groups (13.0-29.7%) (p<0.05 for all). Although the mean age at death was younger for each lifetime manic spectrum episode groups (ManEp: 69.8 years, HypoEp: 64.5 years, SubManEp: 68.8 years) compared to NoManEp group (78.2 years), the difference was only significant in the HypoEp group (p<0.05).
Table 1.
Demographic and health characteristics by lifetime manic episode.
| AnyManEpa | ManEp | HypoEp | SubManEp | NoManEp | Comparis on among the 3 manic spectrum and no mania groups |
|
|---|---|---|---|---|---|---|
| Mean (SD) or N (%) |
Mean (SD) or N (%) |
Mean (SD) or N (%) |
Mean (SD) or N (%) |
Mean (SD) or N (%) |
||
| (N=1,237) | (N=46) | (N=195) | (N=1,041) | (N=13,588) | p-value | |
| Age at entry, years |
37.5 (17.1) | 33.8 (13.7)1 | 34.4(14.5)1 | 38.8 (17.8)1 | 49.6 (20.3) | <0.001 |
| Age of death, years |
67.8 (16.8) | 69.8 (19.0) | 64.5 (16.6)1 | 68.8(16.8) | 78.2 (13.0) | <0.001 |
| Caucasian | 688 (55.6) | 27 (58.7) | 123 (62.1)1,2 | 567 (54.6)1 | 9,608 (70.8) | <0.001 |
| Female | 611 (49.4) | 23 (50.0)1 | 110 (56.4)1,2 | 507 (48.7)1 | 8,014 (59.0) | <0.001 |
| Married | 405 (32.8) | 16 (34.8) | 51 (26.3)1,2 | 354 (34.0)1 | 6,509 (47.9) | <0.001 |
| Education, years |
11.4 (3.2) | 11.3 (3.1) | 11.7 (2.9) | 11.3 (3.2) | 11.2 (3.4) | 0.162 |
| Depressive symptoms |
5.3 (2.6) | 5.3 (2.6)1,2,3 | 6.0 (2.3)12 | 3.9 (2.4)1 | 1.4 (1.8) | <0.001 |
| Hx Alcohol Abuse/Depen dence |
386 (31.4) | 17 (37.8)1 | 74 (38.1)1,2 | 307 (29.7)1 | 1,415 (10.5) | <0.001 |
| Hx Non- Alcohol DrugaAbuse/Depen dence |
247 (20.1) | 13 (28.3)1 | 59 (30.6)1,2 | 179 (17.3)1 | 604 (4.5) | <0.001 |
| Deceased during follow- up |
330 (27.1) | 6 (13.0)1,2 | 40 (20.5)1,2 | 307 (29.7)1 | 5,826 (42.9) | <0.001 |
significant (p<0.05) pairwise difference with the no lifetime manic spectrum episode (NoManEp) group
significant (p<0.05) pairwise difference with lifetime sub-threshold manic episode (SubManEp) group
significant (p<0.05) pairwise difference with lifetime hypomanic episode (HypoEp) group
Differences in baseline characteristics between the three manic spectrum episode groups were also observed (Table 1). Compared to the SubManEp group, participants in the HypoEp group were more likely to be Caucasian (62.1% vs. 54.6%) and female (56.4% vs. 48.7%), were less likely to be married (26.3% vs. 34.0%), had more alcohol abuse/dependence (38.1% vs. 29.7%) and non-alcohol drug abuse/dependence (30.6% vs. 17.3%) (p<0.05 for all). Differences between ManEp and SubManEp groups on these demographic and behavioral characteristics were not significant. All groups differed on mean number of lifetime depressive symptoms, with the HypoEp group reporting the most depressive symptoms (6.0), followed by the ManEp group (5.3) and SubManEp group (3.9) (p<0.05 for all). The proportion of participants who died during the follow up was higher in the SubManEp group (29.7%) compared to the HypoEp (20.5%) and ManEp (13.0%) groups (p<0.05 for both). Differences in mean age of death between ManEp, HypoEp, and SubManEp groups were not significant.
Table 2 shows the odds of mortality for manic spectrum episodes, demographic characteristics, behavioral risk factors and depressive symptoms. As expected, having more education and being married were protective against mortality in all models, whereas being older was associated with greater odds of mortality (p <0.001 for all). Female sex was not associated with mortality in the unadjusted model but demonstrated a protective effect when other demographic characteristics were added to the model. In the unadjusted models, having a lifetime history of alcohol abuse/dependence, non-alcohol drug abuse/dependence or manic spectrum episodes appeared to be protective; however, once age was adjusted for, all three of these factors were associated with a greater odds of mortality (p <0.01 for all). Depressive symptoms were not significantly associated with mortality in the unadjusted model or when the model only adjusted for demographic characteristics. When lifetime alcohol and non-alcohol drug abuse/dependence were adjusted for, depression symptoms demonstrated a protective effect (p <0.01).
Table 2.
Odds ratios for mortality for baseline demographic and health characteristics of four ECA sites with 14,870 respondents followed from 1980-83 through 2007.
| Unadjusted | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Age at entry, years | 1.11a | 1.11, 1.12 |
1.11 a | 1.11, 1.12 |
1.11 a | 1.11, 1.12 |
1.12 a | 1.11, 1.12 |
| Caucasian | 1.99 a | 1.85, 2.14 |
ns | ns | ns | ns | ns | ns |
| Female | ns | ns | 0.55 a | 0.50, 0.61 |
0.59 a | 0.50, 0.61 |
0.59 a | 0.54, 0.66 |
| Married | 0.85 a | 0.80, 0.91 |
0.69 a | 0.63, 0.77 |
0.69 a | 0.63, 0.76 |
0.72 a | 0.65, 0.79 |
| Education, years | 0.81 a | 0.81, 0.82 |
0.96 a | 0.95, 0.98 |
0.96 a | 0.95, 0.98 |
0.97 a | 0.95, 0.98 |
| Hx Alcohol Abuse/Dependence |
0.75 a | 0.68, 0.83 |
1.41 a | 1.22, 1.65 |
1.43 a | 1.23, 1.66 |
1.34b | 1.14, 1.56 |
| Hx Non-Alcohol Drug Abuse/Dependence |
0.15 a | 0.13, 0.20 |
1.56 a | 1.22, 2.00 |
1.59 a | 1.23, 2.04 |
1.42 a | 1.10, 1.83 |
| Depressive symptoms |
0.85 a | 0.83, 0.87 |
ns | ns | ns | ns | 0.95 b | 0.91, 0.99 |
| AnyManEp | 0.5 a | 0.45, 0.57 |
1.42 a | 1.18, 1.70 |
1.49 a | 1.23, 1.25 |
1.39 a | 1.15, 1.68 |
adjusted for age, gender, education, marital status, and race
adjusted for age, gender, education, marital status, race, and history of depressive symptoms
adjusted for age, gender, education, marital status, race, history of depressive symptoms, history of alcohol abuse/dependence, and history of non-alcohol drug abuse/dependence
p≤0.001
p<0.01
ns- p>0.05
Table 3 compares the odds of mortality between the AnyManEp group and the NoManEp group for the entire sample and within each of the four age strata. After adjusting for age and other demographic characteristics, being in the AnyManEp group was associated with 1.42 greater odds of mortality compared to those in the NoManEp group (p<0.001) in the overall sample. This association remained significant after adding lifetime depressive symptoms, alcohol and non-alcohol drug abuse /dependence to the model (1.33, p<0.001). In the age-stratified models adjusting only for demographic characteristics, the odds ratio for mortality among participants in the AnyManEp group aged 45-64 was 1.39 (p<0.042). The higher odds ratio for mortality in this age stratum remained significant after adjusting for history of depressive symptoms (1.41, p=0.04). When history of alcohol and non-alcohol drug abuse/dependence were added to the model, this association was attenuated (1.34, p=0.082). In the AnyManEp group aged 30-44, the odds ratio for mortality was significantly higher than the NoManEp group after adjusting for demographic characteristics and history of depressive symptoms (1.39, p=0.05). After adjusting for history of alcohol and non-alcohol drug abuse/dependence, this association was no longer significant (1.30, p=0.12). Groups did not differ in odds of mortality among participants in the youngest (<30 years) or oldest (≥65 years) age strata in any of the models (p>0.05 for all).
Table 3.
Age-stratified prevalence and odds ratios for mortality comparing participants with any lifetime manic spectrum episodes to those with no lifetime history of manic spectrum episodes.
| Any lifetime manic spectrum episodes |
No lifetime manic spectrum episodes |
Logistic regression analyses | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Alive | Deceased | Total | Alive | Deceased | Model 1 | Model 2 | Model 3 | ||||||||
| N | N | Row % |
N | Row % |
N | N | Ro w % |
N | Row % |
OR | 95% CI p-value |
OR | 95% CI p- value |
OR | 95% CI p-value |
|
| Age, years |
||||||||||||||||
| <30 | 563 | 497 | 92.7 | 39 | 7.3 | 3,112 | 2,93 6 |
95.3 | 176 | 5.7 | 1.14 | 0.79, 1.65 p=0.471 |
1.29 | 0.868, 1.90 p=0.2 09 |
1.20 | 0.81, 1.78 p=0.368 |
| 30-44 | 386 | 325 | 84.2 | 61 | 16.8 | 3,012 | 2,66 9 |
88.6 | 343 | 11.2 | 1.35 | 0.99, 1.84 p=0.058 |
1.39 | 1.00, 1.93 p=0.0 5 |
1.30 | 0.93, 1.82 p =0.122 |
| 45-64 | 193 | 102 | 52.9 | 91 | 47.2 | 3,090 | 1,62 5 |
52.6 | 1,46 5 |
47.4 | 1.39 | 1.01, 1.91 p=0.042 |
1.41 | 1.02, 1.95 p=0.0 4 |
1.34 | 0.96, 1.86 p =0.082 |
| ≥ 65 | 167 | 16 | 9.6 | 151 | 90.4 | 4,374 | 532 | 12.2 | 3,84 2 |
87.8 | 1.63 | 0.94, 2.82 p=0.084 |
1.63 | 0.93, 2.86 p=0.0 87 |
1.56 | 0.89, 2.74 p=0.121 |
| Total sampl e |
1,282 | 929 | 72.5 | 353 | 27.5 | 13,58 8 |
7,76 2 |
57.1 | 5,82 6 |
42.9 | 1.42 | 1.18, 1.70 p<0.001 |
1.41 | 1.16, 1.71 p=0.0 01 |
1.33 | 1.10, 1.62 p=0.004 |
adjusted for age, gender, education, marital status, and race
adjusted for age, gender, education, marital status, race, and history of depressive symptoms
adjusted for age, gender, education, marital status, race, history of depressive symptoms, history of alcohol abuse/dependence, and history of non-alcohol drug abuse/dependence
OR – odds ratio
CI- confidence interval
4. Discussion
These findings from a large population-based study suggest that a lifetime history of manic spectrum episodes is associated with an increased risk of all-cause mortality over a 26-year follow up in middle-aged cohorts (those aged 30-64 years at enrollment), and that this increased risk persists even after adjusting for lifetime depressive symptoms. These findings are consistent with previous findings from a record linkage study of mortality among bipolar patients discharged from hospitals in England between 1999-2006 (Hoang et al., 2011). After adjusting for age and sex, standardized all-cause mortality ratios in that study ranged from 3.4-8.0 within one year after discharge in those aged <45 years (Hoang et al., 2011). The reported risk of mortality in that study was substantially higher than the age and sex adjusted 1.39 increased odds among those aged 30-44 in our study, perhaps due to that study’s clinical sample. Taken together, these findings may suggest that while patients with bipolar disorder severe enough to require inpatient treatment are at greatest risk, individuals with the more common manic spectrum episodes in the community are also at increased risk of mortality.
Also consistent with previous studies of bipolar disorder, AnyManEp participants in this study had more alcohol and non-alcohol drug abuse/dependence than the general population (Laursen, 2011, McAlpine and Mechanic, 2000). This higher prevalence was most pronounced in those participants with a lifetime history of manic or hypomanic episodes (i.e., those with greater illness severity). In the 30-44 and 45-64 age groups, the odds of mortality associated with manic episodes decreased by 9% and 7% respectively, and was no longer statistically significant after adjusting for these behavioral risk factors for mortality. The same trend was observed in the <30 age cohort, although the outcome was not statistically significant in either model. These findings may suggest that premature mortality in individuals with a history of manic symptoms may be at least partially attributed to modifiable behavioral risk factors such as substance abuse/dependence. Studies of bipolar disorder have reported similar findings with unnatural causes of death in younger age groups and mortality related to medical comorbidity in middle age and older adult cohorts (Tsai et al., 2005, Carney and Jones, 2006, Ostacher et al., 2006, Laursen, 2011).
Findings from this study did not suggest increased odds of mortality among the oldest cohort (≥65 years). This could be because the majority of participants who were ≥65 years of age in 1980-83 were deceased by the 26 year follow-up. Alternatively, this could be an artifact of survival bias, with older individuals with lifetime history of mania not surviving to participate in the study in 1980-83, or a recall bias, with older adults not remembering symptoms occurring earlier in life, or a cohort effect, with older adults being less inclined to report affective symptoms. This could explain why, in our models, prior to adjusting for age, lifetime history of manic symptoms (as well as history of alcohol and non-alcohol abuse/dependence) appears to be protective. A strong cohort effect with older individuals (i.e. those more likely to be deceased at follow-up) not recognizing, not remembering or not wanting to report substance abuse, manic and depressive symptoms presents a weakness of the DIS method of assessment of these disorders in older adults sampled for this study.
5. Limitations
This study had several additional limitations that should be taken into consideration when interpreting the findings. First, this study lacked data on baseline health characteristics such as medical comorbidity and smoking habits in three of the for study sites, which may explain the increased risk of mortality, especially in middle-aged cohorts. A previous study reported increased incidence of cardiovascular disease and higher smoking prevalence among participants with lifetime manic spectrum episodes in the Baltimore ECA study site (Ramsey et al., 2010).39 Other studies have reported similar results for bipolar disorder (Laursen, 2011, Black, et al., 1987b, Weinger et al., 2011, Fiedorowicz et al., 2009). Second, the specific causes of death were not included in these analyses. Understanding risk factors and related causes of mortality could be informative in developing cohort-specific interventions to reduce risk of mortality in this population. Third, data on age of onset and number of manic spectrum episodes were not available for analysis in this study. Future studies with data on causes of mortality and age of onset are needed. Despite these limitations, this study benefitted from a large, diverse sample of respondents from urban areas throughout the US, and a structured diagnostic interview. Furthermore, it is the first study to assess symptoms across the full manic spectrum as they relate to mortality. This study takes into account the potential confounding effect of depression, an established risk factor for mortality, across the full spectrum of depressive symptoms, demonstrating the independent effect of mania on mortality.
Acknowledgments
This study was supported by NIDA grant number DA026652.
Footnotes
The authors have no acknowledgements. Dr. Mojtabai has received consulting fees from Lundbeck pharmaceutical company and research funding and consulting fees from Bristol Myers Squibb pharmaceutical company. No other authors have conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anda R, Williamson D, Jones D, Macera C, Eaker E, Glassman A, Marks J. Depressed affect, hopelessness, and the risk of ischemic heart disease in a cohort of US adults. Epidemiology. 1993;4:285–94. doi: 10.1097/00001648-199307000-00003. [DOI] [PubMed] [Google Scholar]
- Angst F, Stassen H, Clayton P, et al. Mortality of patients with mood disorders: Follow-up over 34-38 years. J. Affect. Disord. 2002;68:167–181. doi: 10.1016/s0165-0327(01)00377-9. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Schroll M. Symptoms of depression, acute myocardial infarction, and total mortality in a community sample. Circulation. 1996;93:1976–1980. doi: 10.1161/01.cir.93.11.1976. [DOI] [PubMed] [Google Scholar]
- Black D, Winokur G, Nasrallah A. Mortality in patients with primary unipolar depression, secondary unipolar depression, and bipolar affective disorder: A comparison with general population mortality. Int. J. Psychiatry Med. 1987a;17:351–360. doi: 10.2190/vl1b-7yee-91j5-mwra. [DOI] [PubMed] [Google Scholar]
- Black D, Winokur G, Nasrallah A. Is death from natural causes still excessive in psychiatric patients? A follow-up of 1593 patients with major affective disorder. J. Nerv. Ment. Dis. 1987b;175:674–680. doi: 10.1097/00005053-198711000-00005. [DOI] [PubMed] [Google Scholar]
- Carney C, Jones E. Medical comorbidity in women and men with bipolar disorders: A population-based controlled study. Psychosom. Med. 2006;21:1133–1137. doi: 10.1097/01.psy.0000237316.09601.88. [DOI] [PubMed] [Google Scholar]
- Chang C, Hayes R, Perera G, Broadbent M, Fernandes A, Lee W, Hotopf M, Steward R. Life expectancy an birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLos ONE. 2011;6:e19590. doi: 10.1371/journal.pone.0019590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole M, Bellavance F, Mansour A. Prognosis of depression in elderly community and primary care populations: A systematic review and meta-analysis. Am. J. Psychiatry. 1999;156:1182–1189. doi: 10.1176/ajp.156.8.1182. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J. Affect. Disord. 2002;72:227–236. doi: 10.1016/s0165-0327(01)00413-x. [DOI] [PubMed] [Google Scholar]
- Eaton WW, Kessler LG, editors. Epidemiologic Field Methods in Psychiatry: the NIMH Epidemiologic Catchment Area Program. Academic Press; New York: 1985. [Google Scholar]
- Fiedorowicz J, Solomon D, Endicott J, Leon A, Li C, Rice J, Coryell W. Manic/hypomanic symptom burden predicts cardiovascular mortality with bipolar disorder in the Collaborative Depression Study. Psychosom. Med. 2009;71:598–606. doi: 10.1097/PSY.0b013e3181acee26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fillenbaum G, Burchett B, Blazer D. Identifying a national death index match. Am J. Epidemiology. 2009;170:515–518. doi: 10.1093/aje/kwp155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greist J, Klein M, Erdman H, Bires J, Bass S, Macntinger P, Kresge D. Comparison of computer-and interviewer-administered versions of the Diagnostic Interview Schedule. Hosp Community Psychiatry. 1987;38:1304–1311. doi: 10.1176/ps.38.12.1304. [DOI] [PubMed] [Google Scholar]
- Hill M, Rosenwaike I. The Social Security Administration’s Death Master File: The Completeness of Death Reporting at Older Ages. Soc. Secur. Bull. 2001;64:45. [PubMed] [Google Scholar]
- Hirschfeld RM, Calabrese JR, Weissman MM, Reed M, Davies MA, Frye MA, Keck PE, Jr, Lewis L, McElroy SL, McNulty JP, Wagner KD. Screening for bipolar disorder in the community. J. Clin. Psychiatry. 2003;64:53–59. doi: 10.4088/jcp.v64n0111. [DOI] [PubMed] [Google Scholar]
- Hoang U, Stewart R, Goldacre M. Mortality after hospital discharge for people with schizophrenia or bipolar disorder: Retrospective study of linked English hospital episode statistics, 1999-2006. BMJ. 2011;343:360. doi: 10.1136/bmj.d5422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyer E, Mortensen P, Olesen A. Mortality and causes of death in a total national sample of patients with affective disorders admitted for the first time between 1973 and 1993. Br. J.Psychiatry. 2000;176:76–82. doi: 10.1192/bjp.176.1.76. [DOI] [PubMed] [Google Scholar]
- Judd L, Akiskal H. The prevalence and disability of bipolar spectrum disorders in the US population: re-analysis of the ECA database taking into account subthreshold cases. J. Affect. Disord. 1998;73:123–131. doi: 10.1016/s0165-0327(02)00332-4. [DOI] [PubMed] [Google Scholar]
- Judd L, Akiskal H, Schettler P, Endicott J, Maser J, Solomon D, Leon A, Rice J, Keller M. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch. Gen. Psychiatry. 2002;59:530–537. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- Kessler R. The National Comorbidity Survey of the United States. Int. Rev. Psychiatry. 1994;6:365–376. [Google Scholar]
- Kupfer DJ, Frank E, Grochocinski VJ, Cluss PA, Houck PR, Stapf DA. Demographic and clinical characteristics of individuals in a bipolar disorder case registry. J. Clin. Psychiatry. 2002;63:120–125. doi: 10.4088/jcp.v63n0206. [DOI] [PubMed] [Google Scholar]
- Laursen T. Life expectancy among persons with schizophrenia or bipolar affective disorder. Schizophr. Res. 2011;131:101–104. doi: 10.1016/j.schres.2011.06.008. [DOI] [PubMed] [Google Scholar]
- Laursen T, Munk-Olsen T, Gasse C. Chronic somatic comorbidity and excess mortality due to natural causes in persons with schizophrenia or bipolar affective disorder. PLos ONE. 2011;6:e24597. doi: 10.1371/journal.pone.0024597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laursen T, Munk-Olsen T, Nordentoft M, Mortensen P. Increased mortality among patients admitted with major psychiatric disorders: a register-based study comparing mortality in unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia. J. Clin. Psychiatry. 2007;68:899–907. doi: 10.4088/jcp.v68n0612. [DOI] [PubMed] [Google Scholar]
- Lawson R, Wulsin L, Waillant G, Wells V. A systematic review of the mortality of depression. Psychosom. Med. 1999;61:6–17. doi: 10.1097/00006842-199901000-00003. [DOI] [PubMed] [Google Scholar]
- McAlpine D, Mechanic D. Utilization of specialty mental health care among persons with severe mental illness: The role of demographics, need, insurance, and risk. Health Serv. Res. 2000;35:277–293. [PMC free article] [PubMed] [Google Scholar]
- Osby U, Brandt L, Correia N, Ehbom A, Sparen P. Excess mortality in bipolar and unipolar disorder in Sweden. Arch. Gen. Psychiatry. 2001;58:844–850. doi: 10.1001/archpsyc.58.9.844. [DOI] [PubMed] [Google Scholar]
- Ostacher M, Nierenberg A, Perlis R, Eidelman P, Borrelli D, Tran T, Marzilli-Ericson G, Weiss R, Sachs G. The relationship between smoking and suicidal behavior, comorbidity, and course of illness in bipolar disorder. J. Clin. Psychiatry. 2006;67:1907–1911. doi: 10.4088/jcp.v67n1210. [DOI] [PubMed] [Google Scholar]
- Pennix B, Geerlings S, Deeg D, van Eijk J, van Tilburg W, Beekman A. Minor and major depression and the risk of death in older persons. Arch. Gen. Psychiatry. 1999;56:889–895. doi: 10.1001/archpsyc.56.10.889. [DOI] [PubMed] [Google Scholar]
- President’s Commission on Mental Health . Report to the president from the President’s Commission on Mental Health (4 vols) Superintendent of Documents, U.S. Government Printing Office; Washington, DC: 1978. [Google Scholar]
- Ramsey C, Leoutsakos J, Mayer L, Eaton W, Lee HB. History of manic and hypomanic episodes and risk of incident cardiovascular disease: 11.5 year follow-up from the Baltimore Epidemiologic Catchment Area Study. J. Affect. Disord. 2010;125:35–41. doi: 10.1016/j.jad.2009.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regier D, Farmer M, Rae D, Myers J, Kramer M, Robins L, George L, Karno M, Locke B. One-month prevalence of mental disorders in the United States and sociodemographic characteristics: the Epidemiologic Catchment Area study. Acta Psychiatr. Scand. 1993;88:35–47. doi: 10.1111/j.1600-0447.1993.tb03411.x. [DOI] [PubMed] [Google Scholar]
- Robins LN, Regier D, editors. Psychiatric Disorders in America: the Epidemiologic Catchment Area Study. Free Press; New York: 1991. [Google Scholar]
- Robins L, Helzer J, Ratcliff K, Seyfried W. Validity of the diagnostic interview schedule, version II: DSM-III diagnosis. Psychol. Med. 1982;12:855–870. doi: 10.1017/s0033291700049151. [DOI] [PubMed] [Google Scholar]
- Sax P, Dewwy M. Depression, depressive symptoms and mortality in persons aged 60 and older living in the community: A systematic review of the literature. Int. J. Geriatr. Psychiatry. 2001;16:622–630. doi: 10.1002/gps.396. [DOI] [PubMed] [Google Scholar]
- Sharma R, Markar H. Mortality in affective disorder. J. Affect. Disord. 1994;31:91–96. doi: 10.1016/0165-0327(94)90112-0. [DOI] [PubMed] [Google Scholar]
- Simonsick EM, Wallace RB, Blazer DG, Berkman LF. Depressive symptomatology and hypertension-associated morbidity and mortality in older adults. Psychosom. Med. 1995;57:427–435. doi: 10.1097/00006842-199509000-00003. [DOI] [PubMed] [Google Scholar]
- Thomas C, Kelman HR, Kennedy GJ, Ahn C, Yang C. Depressive symptoms and mortality in elderly persons. Journal of Gerontology. 1992;47:580–587. doi: 10.1093/geronj/47.2.s80. [DOI] [PubMed] [Google Scholar]
- Tsai S, Lee C, Kuo C, Chen C. A retrospective analysis of risk and protective factors for natural death in bipolar disorder. J. Clin. Psychiatry. 2005;66:1586–1591. doi: 10.4088/jcp.v66n1215. [DOI] [PubMed] [Google Scholar]
- Wang S, Berglund P, Olfson M, Pincus H, Wells K,MD, Kessler R. Failure and Delay in Initial Treatment Contact After First Onset of Mental Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- Weiner M, Warren W, Fiedorowicz J. Cardiovascular morbidity and mortality in bipolar disorder. Am. J. Clin. Psychiatry. 2011;23:40–47. [PMC free article] [PubMed] [Google Scholar]
- Zonderman AB, Costa PT, McCrae RR. Depression as a risk for cancer morbidity and mortality in a nationally representative sample. JAMA. 1989;262:1191–1195. [PubMed] [Google Scholar]