Abstract
Background and Objectives
With increasing numbers of people with limited English proficiency in the United States, there is growing concern about the potential adverse effect of language barriers on patient care. We sought to compare the non-English language fluency of practicing physicians by physician race/ethnicity and location of medical school education.
Methods
We used cross-sectional analyses of California Medical Board Survey (2007) data of 61,138 practicing physicians. Measures examined were self-reported physician language fluency in 34 languages, race/ethnicity, and medical school of graduation.
Results
Forty-two percent of physicians reported having fluency in at least one language other than English. Fifty-six percent of international medical graduates (IMGs) reported fluency in a language other than English, compared to 37% of US medical graduates (USMG). Although the majority of physicians with fluency in Spanish are not Latino, fluency in Asian languages is primarily restricted to physicians who are of Asian race/ethnicity. Eighty-seven percent of physicians with fluency in Mandarin, Cantonese, or other Chinese languages are of Chinese ethnicity. A similar association between ethnicity and fluency was found for Southeast Asian languages, Pacific Island languages, and South Asian languages. IMGs constituted more than 80% of the physicians with fluency in Arabic, South Asian, and Pacific Islander languages.
Conclusions
IMGs contribute to the diversity of languages spoken by California physicians.
A growing body of literature documents the adverse influence of language barriers on quality of medical care. An estimated 24 million people in the United States speak English “less than very well” and, therefore, are considered to have limited English proficiency (LEP); these individuals are at risk of facing language barriers or experiencing suboptimal doctor-patient communication.1 Patients with LEP are often cared for by physicians who do not speak their primary language and thus receive less patient-centered care—even after accounting for the use of interpreters.2,3 They are also more likely to report adverse medication reactions,4 treatment non-adherence,5-7 longer emergency care visits,8 decreased satisfaction with care,9-11 and receiving fewer recommended health care services.12-14 Physicians who speak the same language as their patients provide an opportunity for improvements in these outcomes.
Little information is known about what types of physicians speak the non-English languages commonly spoken among the US population. A study by Yoon et al found that physicians of many racial-ethnic backgrounds spoke Spanish and that physicians fluent in Spanish were more likely than their counterparts to practice in areas with more LEP Spanish-speaking residents.15 However, this study was limited to Spanish language and did not address physician fluency in other non-English languages. Learning about physician fluency in Asian languages is of particular importance as there are now more than 8 million Asian and Pacific Island language speakers in the United States, of whom half have LEP.1 Other than English and Spanish, Chinese is the most commonly spoken language, with an estimated 2 million speakers.16
In particular, there is limited published research on the relative linguistic contributions of US and international medical graduate (IMG) physicians in the United States and their potential roles in enhancing communications with patients who have LEP.15 US medical graduates (USMGs) and IMGS both contribute to the cultural and ethnic diversity of the physician workforce, but IMGs may be more likely than USMGs to be fluent in the language of their culture of origin. As such, they may play an important role in improving language access, particularly in underserved areas where many people have LEP. In fact, IMGs represent about one quarter of practicing physicians in the United States and are more likely than USMGs to practice in underserved17-19 and rural20 areas. In 2007, IMGs accounted for 41% and 45% of residents in family medicine and internal medicine, respectively.21
The purpose of this study was to examine fluency in non-English languages among practicing physicians in California. This issue is particularly important for California because it is one of the more linguistically diverse states in the United States and is home to an estimated 6.7 million people with LEP.1 We hypothesized that (1) few physicians have fluency in non-English languages other than Spanish and (2) physicians who are IMGs contribute disproportionately to the linguistic diversity among California physicians.
Methods
Sample
The California Medical Board licenses physicians with doctor of medicine (MD) degrees. All physicians must apply to be relicensed every 2 years and are instructed to complete a survey questionnaire with each biennial application for relicensure. As of July 2007, the Medical Board listed 109,763 physicians with an active California license who had completed one or more cycles of relicensure since 2001 and were therefore eligible for the Medical Board survey. Of these physicians, 83% had completed at least one survey. Physicians completed mandatory questionnaire items on weekly hours in patient care, research, teaching and administration; training status; self-designated specialties; and board certification. Detailed survey methods have been published elsewhere.18,22,23 For this study, we restricted our analysis to physicians with a practice address in California and no longer in training (n=61,138).
Measures
Physicians were asked to complete two voluntary items on ethnicity and language that were present on all surveys from 2001 onward: (1) to select their self-identified race/ethnicity from among a detailed list of 28 ethnicities and (2) to indicate if they were fluent in any of 34 languages listed on the survey. The specific question about fluency was: “In addition to English, indicate any additional languages in which you are fluent.” Physicians were allowed to check more than one response to the race-ethnicity and language items.
We created language categories by collapsing languages corresponding to a geographic region. A Chinese language category consisted of physicians who reported fluency in Cantonese, Mandarin, and other Chinese dialects. Respondents who were fluent in Hmong, Cambodian, Vietnamese, Thai, Lao, and Mien were collapsed into a Southeast Asian language category. Finally, we composed a Pacific Islander language category by combining those who spoke Samoan, Tagalog, and Ilocano.
We used a similar approach to physician race/ethnicity categories. Physicians who selected their race/ethnicity as Cambodian, Indonesian, Laotian/Hmong, Thai, or Vietnamese were categorized as Southeast Asian. Those who selected their ethnicity as Fijian, Filipino, Guamanian, Hawaiian, Samoan, Tongan, or other Pacific Islander were categorized as Pacific Islander.
Physician responses about specialty were categorized as either primary care (family medicine, general internal medicine, and general pediatrics) or non-primary care specialties. We also examined administrative data on physician age (categorized as < 35, 35–44, 55–64, and > 65 years), gender, and medical school of graduation categorized as USMG versus IMG. Physicians who attended medical school in Canada were included in the USMG category.
Analysis
Stata 10.1 statistical software (Stata Corporation LP 2008, College Station, TX) was used for all analyses. We first computed frequencies to compare physician characteristics between IMG and USMG physicians. We computed the percentage of physicians who reported fluency of selected languages within defined racial/ethnic groups, and performed a similar analysis of language fluency comparing IMGs and USMGs. To investigate interactions between these two key predictor variables, we stratified physicians by race/ethnicity and compared language fluency among IMGs and USMGs in the same racial-ethnic categories for selected languages. We used χ2 tests to test for statistically significant differences between categorical variables within groups. We considered a P value of <.05 to indicate a significant difference between groups.
Results
Response Rates
Ten percent of the sample responded “declined to state” to the language fluency question. In addition, 6.2% of respondents did not respond to the question on race/ethnicity, and 7.8% responded “decline to state.” Also, 0.1% of physicians had missing data on medical school of graduation. Nonrespondents were more likely than respondents to be USMGs (15% versus 10% IMGs, P<.001), older age (P<0.001), males (15% versus 12% females, P<.001), non-primary care physicians (13% versus 10% primacy care, P<.001), and self-report fluency in < two non-English languages (P<.001).
Respondents
The mean age of the respondents was 52 (SD=11) years, and 72% were male. Seventy-six percent of physicians were USMGs, and 24% were IMGs. Forty-two percent of California physicians reported having fluency in at least one language other than English. Table 1 compares the characteristics of IMG and USMG physicians. IMG physicians were slightly older (P<.001) and more likely to report fluency in a language other than English (P<.001). Fifty-six percent of IMG physicians reported fluency in one language other than English, compared with 37% of USMGs.
Table 1.
Characteristics of International Medical Graduate (IMG) and US Medical Graduate (USMG) Patient Care Physicians in California
| Physician Characteristic |
IMG
(n=14,637) |
USMG
(n=46,458) |
P Value* |
|---|---|---|---|
| Study sample (%) | 24 | 76 | |
| Age (%) | |||
| <46 years | 23 | 33 | <.001 |
| 46–55 years | 30 | 29 | |
| 56–65 years | 33 | 25 | |
| >65 years | 14 | 13 | |
| Gender (%) | |||
| Female | 31 | 26 | <.001 |
| Race/Ethnicity (%) | |||
| Non-Latino white | 36 | 70 | <.001 |
| Latino | 6 | 5 | |
| Black | 1 | 4 | |
| Asian | 31 | 16 | |
| South Asian | 19 | 2 | |
| Other | 7 | 3 | |
| Self-reported language fluency (%) | |||
| Speak English only | 16 | 55 | <.001 |
| Speak one other language | 56 | 37 | |
| Speak two or more other languages | 28 | 8 | |
| Medical specialty (%) | |||
| Primary care† | 58 | 69 | <.001 |
| Non-primary care | 42 | 31 |
Calculated with χ2 tests for group comparison
Family medicine, general internal medicine, and general pediatrics
Race/Ethnicity and Languages
Table 2 shows the distribution of race/ethnicity among physicians speaking selected languages. Fifty-two percent of all Spanish-speaking physicians were non-Latino white, and 23% were Latinos. Seventeen percent of non-Latino white physicians reported fluency in Spanish compared to 92% of Latino physicians. In contrast to Spanish, 87% of physicians who reported fluency in Chinese languages were of Chinese ethnicity. A similar pattern was seen for Southeast Asian and Pacific Island languages.
Table 2.
Distribution of Physician Self-reported Fluency in Selected Languages According to Physician Race/Ethnicity
| Race-Ethnicity | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Language(s) | Non- Latino White |
Black | Latino | Chinese | Southeast Asian* |
Pacific Islander † |
Indian/ Pakistani |
Other Asian |
Native American/ Other |
Decline/ Missing |
| Spanish (%) (n=11,001) |
52 | 3 | 23 | 4 | 1 | 5 | 3 | 4 | 4 | 9 |
| Chinese (%) ‡ (n=3,511) % |
2 | 0 | 0 | 87 | 2 | 2 | 0 | 7 | 6 | 4 |
| Southeast Asian (%) § (n=1,420) % |
4 | 0 | 1 | 5 | 88 | 1 | 1 | 1 | 5 | 3 |
| Pacific Islander (%) ¶ (n=1,742) % |
5 | 0 | 1 | 8 | 0 | 82 | 1 | 12 | 7 | 3 |
| Hindi/ Punjabi (%) (n=2,652) |
3 | 0 | 0 | 0 | 0 | 0 | 91 | 2 | 9 | 5 |
Ethnic background: = Cambodian, Indonesian, Laotian/Hmong, Thai, and Vietnamese;
= Fijian, Filipino, Guamanian, Hawaiian, Samoan, Tongan, and other Pacific Islander
Foreign language: = Mandarin, Cantonese, and other Chinese languages;
= Hmong, Lao, Mien, Thai, Vietnamese, and Cambodian;
= Samoan, Tagalog, and Ilocano.
Percentages in each row do not add up to 100% due to some physicians selecting more than one ethnic background.
Table 3 shows the distribution of USMG and IMG status among physicians fluent in selected languages. The majority of physicians who speak Samoan, Tagalog, or Ilocano are IMGs (82%). A similar pattern was observed for physicians fluent in Arabic, Farsi, Russian, and Hindi/Punjabi. In contrast, the majority of physicians who speak a Chinese or Southeast Asian language are USMGs.
Table 3.
Distribution of Medical School of Graduation (USMG Versus IMG) Among Physicians With Self-reported Fluency in Selected Languages
| Language(s) | US Medical Graduate |
International Medical Graduate |
|---|---|---|
| Spanish (%) (n=11,001) |
73 | 27 |
| Cantonese/Mandarin/Other Chinese (%) (n=3,511) |
60 | 40 |
| Hmong/Lao/Mien/Thai/Vietnamese/Cambodian (%) (n=1,420) |
60 | 40 |
| Korean (%) (n=1,043) |
51 | 49 |
| Farsi (%) (n=1,569) |
40 | 60 |
| Russian (%) (n=730) |
32 | 68 |
| Arabic (%) (n=954) |
19 | 81 |
| Samoan/Tagalog/Ilocano (%) (n=1,742) |
18 | 82 |
| Hindi/Punjabi (%) (n=2,652) |
16 | 84 |
For all language categories the difference between USMGs and IMGs is statistically significant, P value < .001, calculated with χ2 tests.
USMG—US medical graduate
IMG—international medical graduate
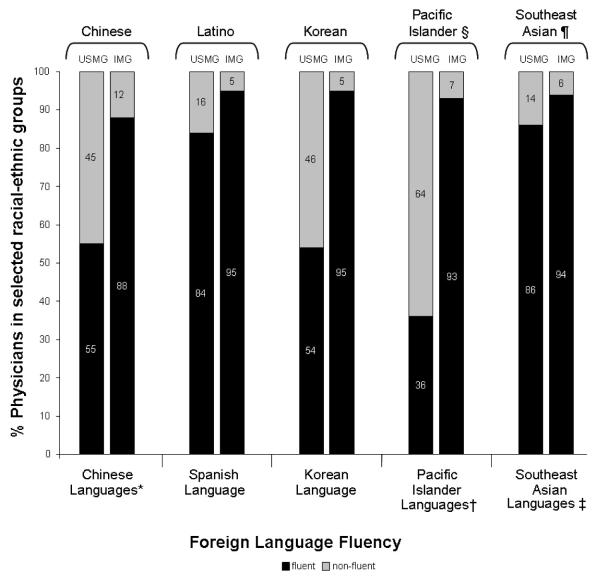
Figure 1 illustrates the distribution of physician language fluency by IMG or USMG status within selected race/ethnicities. Among physicians of Pacific Islander, Chinese, and Korean ethnicities, IMGs were significantly more likely than USMGs to speak the concordant non-English language. The largest discrepancy was observed for physicians of Korean ethnicity, in that 93% of Korean IMGs reported language fluency in Korean compared to only 35% of Korean USMGs. In contrast, Latino USMGs had rates of Spanish language fluency similar to those of Latino IMG physicians. Southeast Asian physicians also showed only small differences in physician non-English language fluency between IMGs and USMGs. Spanish language fluency also varied for non-Latino white physicians depending on whether they graduated from domestic or international medical schools. Only 16% of non-Latino white USMGs reported Spanish fluency, compared to 24% of non-Latino white IMGs (P<.001) (data not shown).
Figure 1.
Self-reported Language Fluency Among California Physicians According to Race/Ethnicity and Medical School of Graduation (USMG Versus IMG)
When stratified by physician specialty, primary care physicians were more likely (P<.05) than physicians in non-primary care specialties to self-report speaking a foreign language, with the difference most pronounced for Spanish (Table 4). Among primary care physicians, the difference in rates of Spanish language fluency by USMG and IMG status was not statistically significant (23% for USMGs versus 24% for IMGs, P=.48). In contrast, non-primary care IMG physicians were significantly more likely to speak Spanish compared to non-primary care USMGs (18% versus 15%, P<.001). We did not find significant differences in selected non-English language fluency based on physician gender or age.
Table 4.
Percent of California Physicians That Self-reported Fluency in Selected Languages by Specialty (Primary Care Versus Non-primary Care) and Medical School of Graduation (USMG Versus IMG)
| Physician Specialty | Fluency in Language | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Spanish (%) |
Chinese Language† (%) |
Southeast Asian Language‡ (%) |
Pacific Islander Language§ (%) |
Korean Language (%) |
||||||
| Non-Primary Care (n=36,591) |
15.5 | 5.3 | 1.8 | 2.0 | 1.7 | |||||
| USMG | 14.9 | P<.001 | 4.1 | P<.001 | 1.5 | P<.001 | 0.5 | P<.001 | 1.1 | P<.001 |
| IMG | 17.8 | 10.1 | 2.8 | 7.6 | 4.1 | |||||
| Primary Care (n=18,483) |
23.5 | 7.2 | 3.6 | 4.7 | 1.8 | |||||
| USMG | 23.4 | P=.48 | 6.0 | P<.001 | 2.6 | P<.001 | 1.0 | P<.001 | 1.3 | P<.001 |
| IMG | 23.9 | 10.1 | 5.7 | 13.2 | 2.9 | |||||
Foreign Language: =Mandarin, Cantonese, and other Chinese languages;
=Hmong, Lao, Mien, Thai, Vietnamese, and Cambodian;
=Samoan, Tagalog, and Ilocano. Primary Care Specialties = family medicine, general internal medicine, and general pediatrics.
Note: All P values calculated using χ2 tests. For all language categories, primary care physicians were more likely (P<.05) than physicians in non-primary care specialties to self-report fluency in the corresponding language.
USMG—US medical graduate
IMG—international medical graduate.
Medical school graduated was used to classify physicians as USMG or IMG.
Discussion
We found substantial variation in fluency in non-English languages among physicians in California according to physicians’ race/ethnicity and whether they graduated from a US or international medical school. Our results add to the scant literature that has examined self-reported language fluency among practicing physicians.
One key finding of our study is that physician fluency in Asian languages is primarily restricted to physicians in specific race/ethnicities. The majority of physicians who speak Cantonese, Mandarin, or other Chinese dialects are of Chinese ethnicity. A similar pattern was found for physicians who speak a Pacific Island language and Southeast Asian language.
In contrast, for Spanish language, we found that fluency is not restricted to Latinos, a finding similar to that of a previous study of California physicians.15 The majority of California physicians who report Spanish language fluency are non-Latino white. This finding reflects the large proportion of non-Latino white physicians (45%) in California relative to the small proportion of Latino physicians (4%).22 Many non-Latino US students learn Spanish during their K–12 years of education as part of their obligatory second language in school. Traditionally, few schools at this level have offered language courses in non-romance languages.24
Our study extends the work of Yoon et al15 in several important ways. First, our study included a much larger sample of physicians than that in any prior study of physician language fluency. Moreover, this study is one of the first to examine fluency in non-English languages other than Spanish and is also one of the first to distinguish between the fluency of IMGs and USMGs in these languages.
Our results also show that IMGs make different contributions to language fluency within an ethnic group, depending on the specific ethnic group. For example, Latino USMGs reported Spanish language fluency at comparable rates to Latino IMGs. However, for Asian and Pacific Island languages, IMGs are much more likely to report fluency compared to their US-trained peers.
Finally, we found variation in fluency among physicians depending on whether they were in primary care or non-primary care specialties. Effective communication is especially important in primary care because these physicians develop long-term relationships with patients and families, care for patients with multiple medical conditions, and regularly delve into psychosocial medical issues. As a result, language fluency may be especially critical for these physicians. Good doctor-patient communication, however, is fundamental to the practice of medicine and is therefore important for all physicians regardless of specialty.
Limitations
Our study has several limitations. First, using survey data from California may limit generalizability of the results to physicians in other states. Second, physician race/ethnicity and language fluency are based on self-report and may be subject to reporting bias. Self-report, however, is the standard for collecting information on race-ethnicity. Third, the California Medical Board Survey does not formally test for language fluency using standardized assessments and, therefore, we have no objective measure of physician language fluency. However, other research indicates that physicians and medical students are cognizant of the degree to which they are fluent.25,26 Nonetheless, in this study, physician fluency may range from medical terminology commonly taught during medical school or graduate medical education programs to proficient native speakers. We also do not have data on nonverbal communication, regional dialects, and other aspects of doctor-patient communication.
Policy Implications
Our findings have several policy implications. First, in California, there are an estimated 4.6 million people who speak Spanish at home and speak English with LEP. This coupled with an additional 1.5 million Californians who speak an Asian/Pacific Islander language at home and are LEP underscores the continued need for physicians who speak languages other than English.1
Second, if the nation moves toward a policy of self sufficiency in the physician workforce during the next several decades with fewer IMGs entering the US workforce, it will be important to understand the implications of such a policy on language access. Because IMGs currently make a significant contribution to language access, shifts in workforce policy may inadvertently exacerbate language barriers for patients with LEP.
Finally, although our study focuses on California physicians, other states in the United States are now experiencing increases in their population’s linguistic diversity, which is creating a new demand for bilingual or multilingual health care providers.27,28 The California Medical Board Survey demonstrates the value of systematically collecting data on physician language fluency. This type of data collection of physician language fluency should be incorporated into other physician workforce databases, particularly in states with changing linguistic diversity.
Conclusions
While the finding that physicians of different ethnicities self-report Spanish fluency is positive, having Latino physicians is important for patient care because Latino physicians are more likely than non-Latino whites to practice in underserved communities and care for uninsured patients.29-31 Similarly significant, Latino physicians are in a unique position to provide culturally appropriate health care to Spanish-speaking patients. Future research should address how physician language fluency is related to practice location.
In conclusion, our study of California physicians found that physician fluency in non-English languages other than Spanish is limited to physicians in specific racial/ethnic groups and that IMGs contribute significantly to the overall linguistic diversity among physicians. Because physician language fluency is associated with improved patient-centered outcomes and patients may prefer to receive care in their primary language, physician workforce and medical education policies should ensure that there is linguistic diversity among practicing physicians and physician trainees.
Acknowledgments
The authors thank Robert E. Bjork, PhD, for editorial comments on an early draft of this manuscript.
Drs Moreno and Walker were funded by the Robert Wood Johnson Clinical Scholars Program at the University of California, Los Angeles. Dr Walker also received partial support from the University of California, Los Angeles Resource Center for Minority Aging Research/Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under NIH/NIA Grant P30AG021684.
Footnotes
Preliminary results of this study were presented as a works in progress abstract at the 2008 North American Primary Care Research Group Annual Meeting in Puerto Rico.
References
- 1.US Census Bureau [Accessed November 30, 2009];American Community Survey. 2006–2008 Available at www.census.gov.
- 2.Rivadeneyra R, Elderkin-Thompson V, Silver RC, Waitzkin H. Patient centeredness in medical encounters requiring an interpreter. Am J Med. 2000;108:470–4. doi: 10.1016/s0002-9343(99)00445-3. [DOI] [PubMed] [Google Scholar]
- 3.Ngo-Metzger Q, Sorkin DH, Phillips RS, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007;22(2 suppl):324–30. doi: 10.1007/s11606-007-0340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilson E, Chen AH, Grumbach K, Wang F, Fernandez A. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20:800–6. doi: 10.1111/j.1525-1497.2005.0174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karter AJ, Ferrara A, Darbinian JA, Ackerson LM, Selby JV. Self-monitoring of blood glucose: language and financial barriers in a managed care population with diabetes. Diabetes Care. 2000;23:477–83. doi: 10.2337/diacare.23.4.477. [DOI] [PubMed] [Google Scholar]
- 6.Kravitz RL, Helms LJ, Azari R, Antonius D, Melnikow J. Comparing the use of physician time and health care resources among patients speaking English, Spanish, and Russian. Med Care. 2000;38:728–38. doi: 10.1097/00005650-200007000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Manson A. Language concordance as a determinant of patient compliance and emergency room use in patients with asthma. Med Care. 1988;26:1119–28. doi: 10.1097/00005650-198812000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Hampers LC, Cha S, Gutglass DJ, Binns HJ, Krug SE. Language barriers and resource utilization in a pediatric emergency department. Pediatrics. 1999;103:1253–6. doi: 10.1542/peds.103.6.1253. [DOI] [PubMed] [Google Scholar]
- 9.Baker DW, Hayes R, Fortier JP. Interpreter use and satisfaction with interpersonal aspects of care for Spanish-speaking patients. Med Care. 1998;36:1461–70. doi: 10.1097/00005650-199810000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Carrasquillo O, Orav EJ, Brennan TA, Burstin HR. Impact of language barriers on patient satisfaction in an emergency department. J Gen Intern Med. 1999;14:82–7. doi: 10.1046/j.1525-1497.1999.00293.x. [DOI] [PubMed] [Google Scholar]
- 11.Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD. Are Latinos less satisfied with communication by health care providers? J Gen Intern Med. 1999;14:409–17. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng EM, Chen A, Cunningham W. Primary language and receipt of recommended health care among Hispanics in the United States. J Gen Intern Med. 2007;22(2 suppl):283–8. doi: 10.1007/s11606-007-0346-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacobs EA, Karavolos K, Rathouz PJ, Ferris TG, Powell LH. Limited English proficiency and breast and cervical cancer screening in a multi-ethnic population. Am J Public Health. 2005;95:1410–6. doi: 10.2105/AJPH.2004.041418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harlan LC, Bernstein AB, Kessler LG. Cervical cancer screening: who is not screened and why? Am J Public Health. 1991;81:885–90. doi: 10.2105/ajph.81.7.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoon J, Grumbach K, Bindman AB. Access to Spanish-speaking physicians in California: supply, insurance, or both. J Am Board Fam Pract. 2004;17:165–72. doi: 10.3122/jabfm.17.3.165. [DOI] [PubMed] [Google Scholar]
- 16.Shin B, Bruno R. Language use and English-speaking ability: 2000. US Census Bureau; Washington, DC: 2003. [Google Scholar]
- 17.Polsky D, Kletke PR, Wozniak GD, Escarce JJ. Initial practice locations of international medical graduates. Health Serv Res. 2002;37:907–28. doi: 10.1034/j.1600-0560.2002.58.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mertz E, Jain R, Breckler J, Chen E, Grumbach K. Foreign versus domestic education of physicians for the United States: a case study of physicians of South Asian ethnicity in California. J Health Care Poor Underserved. 2007;18:984–93. doi: 10.1353/hpu.2007.0100. [DOI] [PubMed] [Google Scholar]
- 19.Mick SS, Lee SY, Wodchis WP. Variations in geographical distribution of foreign and domestically trained physicians in the United States: “safety nets” or “surplus exacerbation”? Soc Sci Med. 2000;50:185–202. doi: 10.1016/s0277-9536(99)00183-5. [DOI] [PubMed] [Google Scholar]
- 20.Baer L, Konrad T, Slifkin R. If fewer international medical graduates are allowed in the US, who might replace them in rural, underserved areas? University of North Carolina at Chapel Hill; Chapel Hill, NC: May, 2001. [Google Scholar]
- 21.Brotherton SE, Etzel SI. Graduate medical education, 2007–2008. JAMA. 2008;300:1228–43. doi: 10.1001/jama.300.10.1228. [DOI] [PubMed] [Google Scholar]
- 22.Grumbach K, Odom K, Moreno G, Chen E, Vercammen-Grandjean C, Mertz E. California physician diversity: new findings from the California Medical Board Survey. UCSF Center for California Health Workforce Studies; San Francisco: Apr, 2003. [Google Scholar]
- 23.Grumbach K, Chattopadhyay A, Bindman AB. Fewer and more specialized: a new assessment of physician supply in California. California HealthCare Foundation; Oakland, Calif: Jun, 2009. [Google Scholar]
- 24.High school coursetaking: findings from The Condition of Education . Institute of Education Sciences. National Center for Education Statistics; Jun, 2007. 2007. [Google Scholar]
- 25.Fernandez A, Schillinger D, Grumbach K, et al. Physician language ability and cultural competence. An exploratory study of communication with Spanish-speaking patients. J Gen Intern Med. 2004;19:167–74. doi: 10.1111/j.1525-1497.2004.30266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reuland DS, Frasier PY, Olson MD, Slatt LM, Aleman MA, Fernandez A. Accuracy of self-assessed Spanish fluency in medical students. Teach Learn Med. 2009;21:305–9. doi: 10.1080/10401330903228489. [DOI] [PubMed] [Google Scholar]
- 27.Cunningham P, Banker M, Artiga S, Tolbert J. “New Growth Communities” and “Major Hispanic Centers.”. Kaiser Commission on Medicaid and the Uninsured; Sep, 2006. Health coverage and access to care for Hispanics. [Google Scholar]
- 28.Guzman B. The Hispanic population: Census Brief 2000 US. Bureau of the Census; Washington, DC: 2001. [Google Scholar]
- 29.Komaromy M, Grumbach K, Drake M, et al. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996;334:1305–10. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- 30.Moy E, Bartman BA. Physician race and care of minority and medically indigent patients. JAMA. 1995;273:1515–20. [PubMed] [Google Scholar]
- 31.Xu G, Fields SK, Laine C, Veloski JJ, Barzansky B, Martini CJ. The relationship between the race/ethnicity of generalist physicians and their care for underserved populations. Am J Public Health. 1997;87:817–22. doi: 10.2105/ajph.87.5.817. [DOI] [PMC free article] [PubMed] [Google Scholar]