Abstract
Lung cancer requiring double bronchial and vascular reconstruction of the pulmonary artery is a challenging procedure usually performed by thoracotomy. However, recent development of video-assisted thoracoscopic techniques allows experienced and skilled surgeons to perform these cases through a minimally invasive approach. Most of these complex thoracoscopic resections are performed by using 3 to 4 incisions. We present the first report of a right side combined vascular reconstruction and bronchoplasty performed through a single-incision video-assisted thoracoscopic surgery (VATS) technique.
Keywords: Thoracoscopy/video-assisted thoracoscopic surgery (VATS), minimally invasive surgery, pulmonary artery reconstruction, vasculoplasty, vascular reconstruction, bronchoplasty, surgery/incisions/technique
Introduction
In the past two decades with increasing frequency video-assisted thoracoscopic surgery (VATS) has been performed for lung cancer treatment. However, complex cases are only performed in a few centers. Most surgeons use a 3-4 port VATS approach for difficult resections such as bronchial or vascular sleeves. This report describes the technique for a right upper lobectomy with bronchoplasty and vascular reconstruction by using a uniportal VATS technique.
Clinical summary
A 73-year-old male, smoker, with severe comorbidities (COPD, obesity, hypertension and cardiomiopathy) was diagnosed with a right upper lobe (RUL) tumor. The CT scan showed the tumor located on the posterior segment of the RUL with bronchial and vascular invasion by lymph nodes (Figure 1). The pulmonary function test was normal (FEV1 70%). The patient was proposed for single incision VATS approach.
Figure 1.
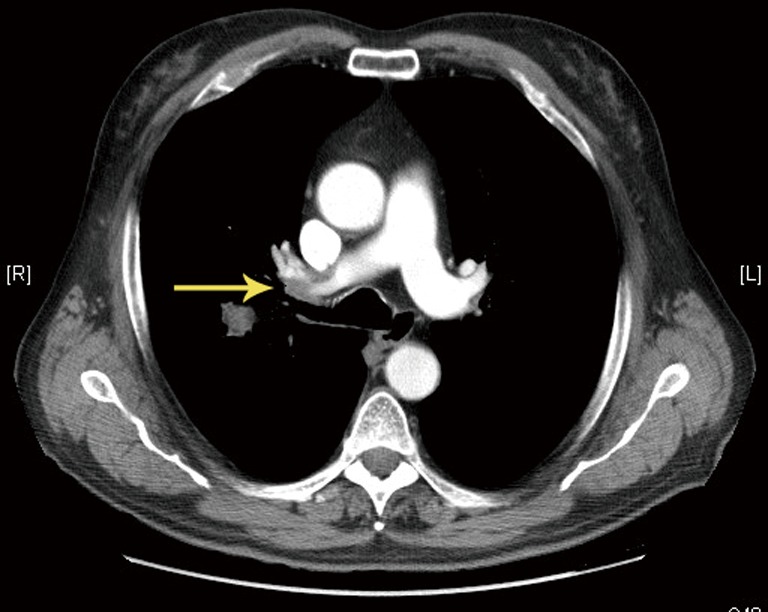
Computed tomography scan showing right upper lobe (RUL) bronchial and vascular lymph node invasion.
Surgical technique
Under general anesthesia, a VATS approach using a 4 cm single-incision was made in the 5th intercostal space with no rib spreading (no soft tissue retractor and no direct vision).
A tumor was detected in the RUL and lymph nodes were involving the bronchus and apical-anterior branch of the pulmonary artery (PA) and interlobar artery. The incomplete fissure was divided from anterior to posterior from the hilum to expose and control the artery. The RUL bronchus was not possible to be dissected so it was transected by using a long knife. The main pulmonary artery and the basal trunk were dissected to have adequate proximal and distal vascular control. Before clamping the PA, 5,000 units of heparin were injected intravenously to prevent clotting. The interlobar artery was occluded by using a double vascular sling vessel loop and the main PA was closed using a thoracoscopic clamp (Scanlan International, Inc, Saint Paul, MN, USA). The clamp was placed towards the anterior portion of the incision and the vessel loop was placed in the posterior part. The camera was located in the posterior part of the incision, and the instrumentation was placed and used below the camera.
The PA was transected laterally and the specimen was temporarily placed in the costo-diaphragmatic space. The defects in the interlobar artery and base of apico-anterior branch were repaired by using interrupted double lateral 4-0 monofilament non-absorbable sutures. The sutures were tied and the air was released through one of the posterior branches which was cut and then closed by using a vascular clip (Click aV, GrenaR) (Figure 2). The specimen was then removed in a protective bag (1).
Figure 2.
Bronchovascular resection and reconstruction.
The bronchus was reconstructed and closed by using interrupted double sutures of 3-0 PDS (Figure 3). The lung was inflated and no air leak was observed. Systematic lymph node dissection was then performed to complete the procedure and a single chest tube was placed (Figure 4). Total surgery time was 310 min and estimated blood loss was 180 cc. The chest tube was removed on the sixth postoperative day and the patient was discharged on the same day with no complications and excellent recovery.
Figure 3.

Surgical image of instrumentation during bronchoplasty.
Figure 4.

Postoperative result with chest tube placed in the posterior part of the incision.
Discussion
Bronchovascular reconstructive surgery is a technically feasible alternative to pneumonectomy and has the advantage of sparing the functioning of the lung parenchyma. These procedures are very complex and usually performed by open surgery (2). However, with the recent developments in VATS technology and acquired experience, this surgery can be performed thoracoscopically by experienced and skilled VATS surgeons. There are very few articles published in the literature describing a combined bronchial and vascular reconstruction by VATS, and these resections are reported on the left side by using conventional multiport thoracoscopic technique (3,4). We have recently published the first case of double sleeve VATS resection by a single incision approach (5).
As our experience has grown with the single-port VATS approach (6) we have increased the rate of thoracoscopic sleeve procedures and decreased the incidence of pneumonectomy and today our list of contraindications is very limited (7). Advanced uniportal thoracoscopic procedures as bronchial sleeve lobectomy (8), lobectomy with chest wall resection, vascular reconstruction (9) and double sleeve (5) have already been performed with good postoperative outcomes. To April 2014 we have performed 11 uniportal VATS lobectomies with reconstruction: wedge bronchoplasty (3 cases), bronchial sleeve (5 cases), pulmonary arterioplasty 3 (1 vascular reconstruction, 1 vascular reconstruction combined with bronchoplasty and one double bronchovascular sleeve). The postoperative course of these patients was uneventful. Mean operative time was 215±54 minutes (range, 120-310 minutes) and median hospital stay was 6 days (range, 2-21 days).
The success in performing complex lobectomies by uniportal approach is a result of skills and experience accumulated over time by performing many uniportal VATS surgeries (6). The advantage of uniportal VATS surgery is the vision is direct to the target tissue providing a similar angle of view as for open surgery. Conventional multi-port VATS triangulation creates a new optical plane with genesis of torsional angle that is not favorable with standard two-dimension monitors. Another advantage of the uniportal VATS technique is that instruments inserted parallel to the camera mimic inside the chest maneuvers performed during open surgery. This geometric uniportal VATS concept facilitates the bronchovascular reconstruction in complex resections such as the one described in this article (10).
Most of the published cases requiring sleeve or vascular reconstruction are located on the left side. Infiltration of the PA on the right side requiring arterial reconstruction is less frequent. Reconstruction of the PA enables complete cancer resection while preserving functioning pulmonary tissue, and has a definitive role in the surgical management of lung cancer. In this particular case there was a partial infiltration of the surface of the artery (base of apical-anterior and posterior branch) by lymph nodes needing tangential resection with direct repair, and a total sleeve was not necessary. In this case partial resection of the PA was performed in conjunction with bronchoplasty of the RUL. The use of thoracoscopic instruments with proximal and distal articulation (Scanlan International, Inc, Saint Paul, MN, USA) facilitate the instrumentation through a single-incision, especially for clamping the main pulmonary artery with no interference to the broncho-vascular reconstruction. For clamping the basal trunk we usually prefer to use a double vessel loop or a bulldog-clamp (placed inside the cavity) to facilitate the instrumentation.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Gonzalez-Rivas Diego, Fieira Eva, de la Torre Mercedes, Delgado Maria. Bronchovascular right upper lobe reconstruction by uniportal video-assisted thoracoscopic surgery. Asvide 2014;1:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rendina EA, De Giacomo T, Venuta F, et al. Lung conservation techniques: bronchial sleeve resection and reconstruction of the pulmonary artery. Semin Surg Oncol 2000;18:165-72 [DOI] [PubMed] [Google Scholar]
- 3.Han Y, Zhou S, Yu D, et al. Video-assisted thoracic surgery (VATS) left upper sleeve lobectomy with partial pulmonary artery resection. J Thorac Dis 2013;5:S301-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu L, Mei J, Pu Q, et al. Thoracoscopic bronchovascular double sleeve lobectomy for non-small-cell lung cancer. Eur J Cardiothorac Surg. 2014 doi: 10.1093/ejcts/ezu103. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gonzalez-Rivas D, Paradela M, Fernandez R, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32 [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5:S234-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7 [DOI] [PubMed] [Google Scholar]
- 9.Gonzalez-Rivas D, Delgado M, Fieira E, et al. Single-port video-assisted thoracoscopic lobectomy with pulmonary artery reconstruction. Interact Cardiovasc Thorac Surg 2013;17:889-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5:S214-6 [DOI] [PMC free article] [PubMed] [Google Scholar]


