Abstract
The circadian timing system is critically involved in the maintenance of fluid and electrolyte balance and BP control. However, the role of peripheral circadian clocks in these homeostatic mechanisms remains unknown. We addressed this question in a mouse model carrying a conditional allele of the circadian clock gene Bmal1 and expressing Cre recombinase under the endogenous Renin promoter (Bmal1lox/lox/Ren1dCre mice). Analysis of Bmal1lox/lox/Ren1dCre mice showed that the floxed Bmal1 allele was excised in the kidney. In the kidney, BMAL1 protein expression was absent in the renin-secreting granular cells of the juxtaglomerular apparatus and the collecting duct. A partial reduction of BMAL1 expression was observed in the medullary thick ascending limb. Functional analyses showed that Bmal1lox/lox/Ren1dCre mice exhibited multiple abnormalities, including increased urine volume, changes in the circadian rhythm of urinary sodium excretion, increased GFR, and significantly reduced plasma aldosterone levels. These changes were accompanied by a reduction in BP. These results show that local renal circadian clocks control body fluid and BP homeostasis.
Circadian rhythmicity is a feature of a wide variety of physiologic functions. Many of the functional rhythms are driven by the circadian timing system, a complex mechanism that coordinates all major cellular processes with geophysical time. It is thought that this coordination allows for the anticipatory adaptation of cells and tissues to the circadian changes in functional requirements. The circadian timing system is organized in a hierarchical manner. The master clock of the system is located in the suprachiasmatic nucleus of the hypothalamus and synchronized to the daily light/dark cycle through the retinohypothalamic tract. The peripheral circadian clocks, which are present in virtually all peripheral tissues, are synchronized to geophysical time through a wide range of master clock-dependent stimuli, many of which remain unknown (reviewed in ref.1). It is important to note, however, that, despite the hierarchical structure of the circadian timing system and its continuous resetting by environmental time cues, the intrinsic activity of both central and peripheral circadian clocks is largely self-sustained. On the molecular level, the master clock and peripheral clocks share similar machinery based on transcriptional/translational feedback loops involving transcriptional activators BMAL1, CLOCK, and NPAS2 and their own repressors PER1 and PER2 as well as CRY1 and CRY2 (reviewed in ref.2).
The circadian timing system is critically involved in the maintenance of fluid and electrolyte balance and BP control. In mice, whole-body genetic inactivation of any of the circadian clock transcriptional activators or repressors leads to either increased or decreased BP3–6 (reviewed in ref.7). In clock−/− mice, the decrease in BP is accompanied by deep changes in circadian rhythms of urinary sodium and potassium excretion, loss of the circadian rhythmicity of plasma aldosterone levels, and significant modifications in expression patterns of a great number of renal transcripts involved in different homeostatic functions.8 Doi et al.9 have shown that Cry1/Cry2 double knockout mice exhibit significantly increased plasma aldosterone levels, resulting in salt-sensitive hypertension. In humans, long-term misalignment of intrinsic circadian rhythms with geophysical time (e.g., shift work) is increasingly recognized as a risk factor for the development of hypertension and progression of CKD.10,11 In genetic studies, Woon et al.12 have identified several polymorphisms in the promoter region of the human Bmal1 gene that are associated with hypertension. However, to what extent the pathogenesis of these disorders is caused by a defect in the master clock and/or the local circadian clocks in different peripheral tissues remains unknown.
Here, we studied the role of peripheral circadian clocks in the maintenance of homeostasis of extracellular fluids and BP regulation in a mouse model carrying a conditional allele of the circadian clock gene Bmal1 and expressing Cre recombinase under the endogenous promoter of the Renin gene (Bmal1lox/lox/Renin-1d [Ren1d] Cre mice).13,14 This mouse model was chosen for three reasons. (1) The renin-angiotensin-aldosterone system (RAAS) plays the central role in the regulation of BP. (2) The activity of the RAAS exhibits significant circadian oscillations. (3) The inactivation of Bmal1 results in the complete disruption of the molecular clock. Functional analysis revealed that Bmal1lox/lox/Ren1dCre mice exhibit multiple abnormalities, including defects in renal handling of sodium, water, calcium, magnesium, and pH, significant changes in the circadian pattern of plasma aldosterone levels, an increase in the GFR, and a decrease in BP. These functional changes were accompanied by significant modifications in circadian patterns of mRNA expression of a number of renal transcripts involved in sodium, potassium, and water balance. This study shows, for the first time, that local renal circadian clocks are indispensable for the maintenance of body fluid homeostasis and BP control.
Results
Inactivation Pattern of Bmal1 in Bmal1lox/lox/Ren1dCre Mice
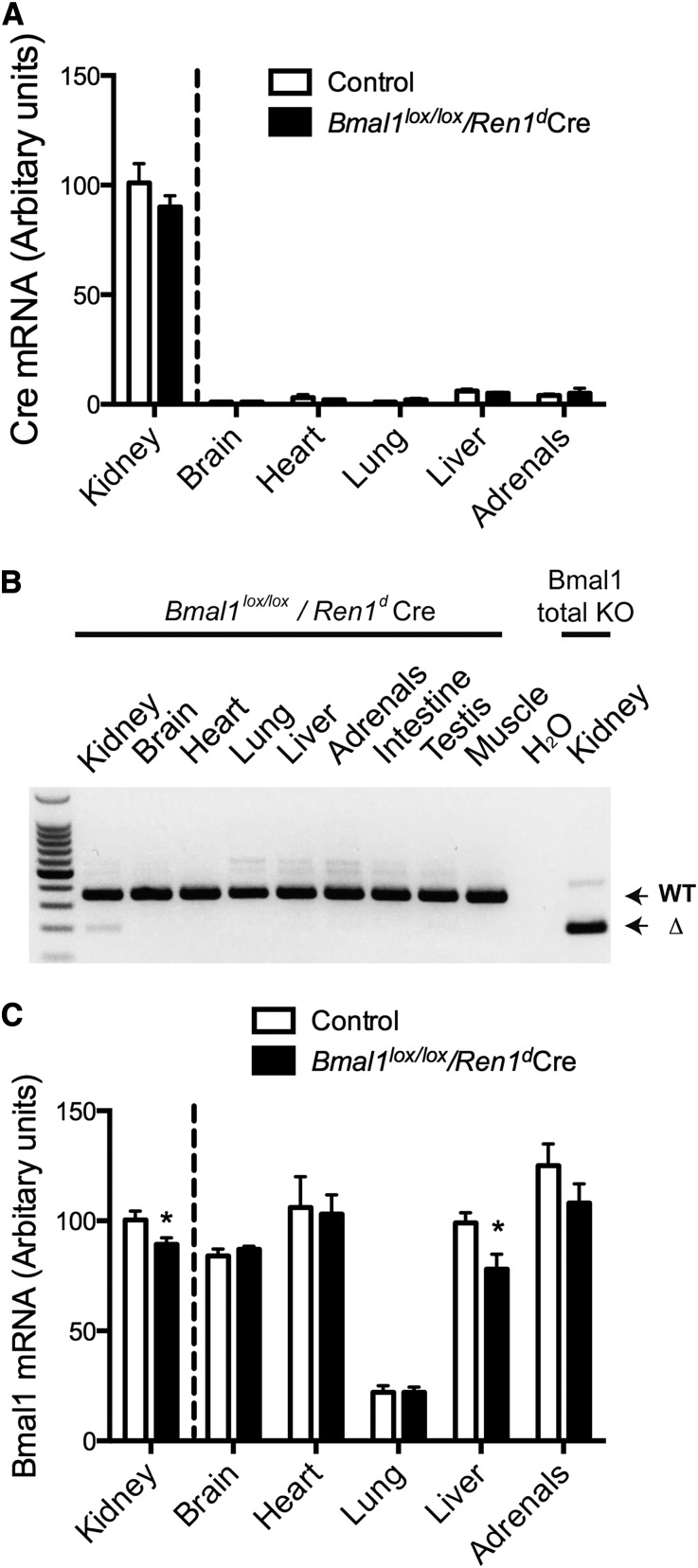
The Bmal1lox/lox/Ren1dCre mice were generated by crossing mice bearing loxP sites flanking the exon 8 of the Bmal1 gene with mice expressing Cre recombinase under the endogenous promoter of the Ren1d gene. The Bmal1lox/lox/Ren1dCre mice were viable and did not show any obvious abnormalities compared with the Ren1dCre mice used as controls (hereafter referred to as control mice). As shown in Supplemental Figure 1, they displayed normal general motion activity and water-drinking behavior. Gene expression analyses were performed at Zeitgeber time 0 (ZT0), the time of maximal expression of Bmal1 mRNA15,16; the protein expression was quantified at ZT4 and/or ZT16, the time of expected maximal and minimal expression of BMAL1 protein, respectively (circadian or ZT, where ZT0 is the time of lights on and ZT12 is the time of lights off).17 The quantitative PCR (qPCR)-based analysis of Cre mRNA levels in different tissues revealed the highest expression in the kidney (Figure 1A). This finding correlated with the observation that the Cre-mediated excision of the floxed Bmal1 allele was detectable only in the kidney, which was, by RT-PCR analysis of total tissue RNA, using primers flanking the floxed region (Figure 1B). Interestingly, the Bmal1 mRNA levels were reduced in not only the kidney but also, the liver, thus suggesting that the circadian clock system in the liver is affected by the disruption of circadian clocks in renal cells (Figure 1C). However, immunohistochemistry showed that the vast majority of liver cells remained positive for Bmal1, and Western blotting did not reveal significant difference in BMAL1 protein expression between control (Supplemental Figure 2A) and Bmal1lox/lox/Ren1dCre mice (Supplemental Figure 2B, ZT4).
Figure 1.
Ren1dCre-mediated Bmal1 inactivation is limited to the kidney. (A) qPCR analysis of Cre mRNA expression (ZT0) in various tissues of control (white bars) and Bmal1lox/lox/Ren1dCre (black bars) mice (primer references are in Supplemental Material); data are mean±SEM (n=5). (B) RT-PCR analysis of Bmal1 mRNA expression (ZT0) in different tissues of Bmal1lox/lox/Ren1dCre mice performed with primers flanking the floxed region. mRNA extracted from kidneys of whole-body (total) knockout (KO) of Bmal1 was used as a control (primer sequences are in Supplemental Material). WT, wild type. (C) qPCR analysis of Bmal1 mRNA expression (ZT0) in various tissues of control (white bars) and Bmal1lox/lox/Ren1dCre (black bars) mice (primer references are in Supplemental Material). Data are mean±SEM (n=5). *P<0.05, t test. Tissues were collected from mice euthanized at ZT0.
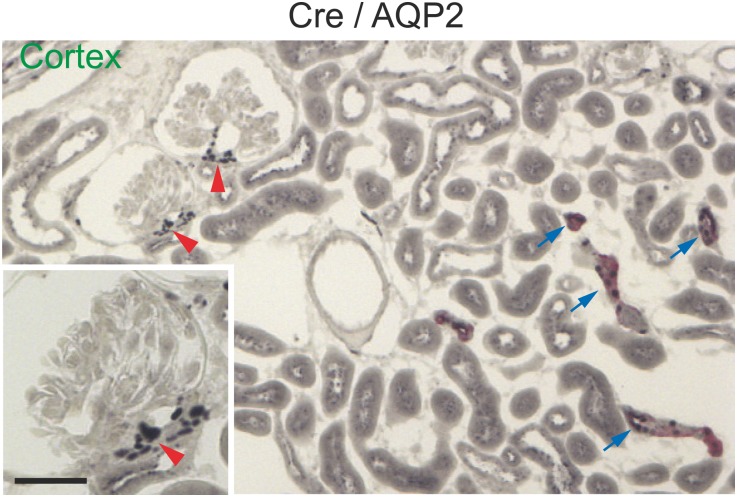
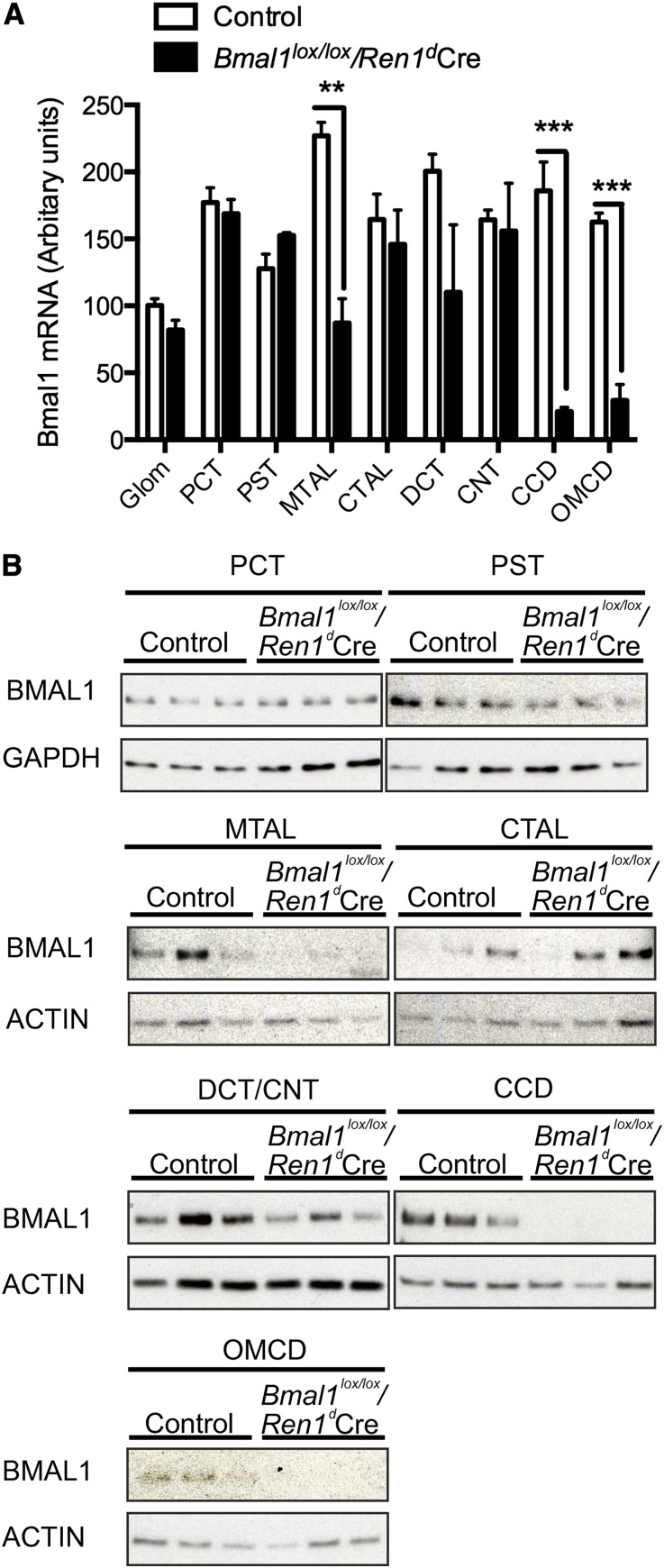
Immunohistochemical analysis of Cre expression in the kidney (ZT4) showed that CRE protein is strongly expressed in the arterioles of the juxtaglomerular apparatus but also present in the cortical collecting duct (CCD) and medullary collecting duct (OMCD); at a weaker level, it is present in the medullary thick ascending limb (MTAL; the Aquaporin-2 water channel was used as a marker of the principal cell of the CCD and OMCD, and Uromodulin was used as a marker of the thick ascending limb) (Figure 2, Supplemental Figure 3). The distribution of Bmal1 mRNA and protein in kidneys of control and Bmal1lox/lox/Ren1dCre mice was examined by qPCR performed on RNAs extracted from microdissected glomeruli or microdissected nephron segments, Western probing of whole-cell lysates prepared from microdissected nephron segments (ZT4), and immunohistochemistry (ZT4 and ZT16). As shown in Figure 3A, the Bmal1 mRNA expression was markedly reduced in the CCD and OMCD. A partial reduction (approximately 60%) in Bmal1 mRNA expression was also observed in the MTAL. Importantly, the decrease in Bmal1 mRNA expression correlated with the deletion of exon 8 of the Bmal1 gene in the same nephron segments (Supplemental Figure 4). Western blot analysis revealed a parallel reduction of BMAL1 protein expression in the CCD, OMCD, and MTAL (Figure 3B). Immunohistochemistry showed that BMAL1 protein is ubiquitously expressed in the kidney of control mice, but it is absent in the juxtaglomerular cells (Supplemental Figure 5, A and E) and the CCD (Supplemental Figure 5, B and F) and OMCD (Supplemental Figure 5, C and G) of Bmal1lox/lox/Ren1dCre mice. The BMAL1 protein expression in the MTAL was significantly reduced; however, a small population of MTAL cells exhibited positive staining for BMAL1 (Supplemental Figure 5, D and H).
Figure 2.
The Ren1dCre mice express the Cre recombinase in the juxtoglomerular apparatus and in the collecting duct. Immunohistochemical localization of Cre recombinase in the renal cortex (ZT4). Strong nuclear Cre staining (black) is present in the arterioles of the juxtaglomerular apparatus (red arrows) and the collecting duct (blue arrows), which is evidenced by costaining with aquaporin-2 (AQP2) water channel (red).
Figure 3.
The Bmal1 is inactivated in multiple tubular segments in kidneys of Ren1dCre mice. (A) mRNA and (B) protein expression of Bmal1 in microdissected glomeruli (glom), proximal convoluted tubule (PCT), proximal straight tubule (PST), MTAL, cortical thick ascending limb (CTAL), distal convoluted tubule (DCT), connecting tubule (CNT), CCD, and OMCD. Microdissection was performed at ZT4. (B) Whole-cell lysates of 20-mm microdissected nephron segments were used for Western blotting (n=3). (A) Data are mean±SEM (n=3). **P<0.01; ***P<0.005, t test. Tissues were collected from mice euthanized at ZT4. GAPDH, glyceraldehyde-3-phosphate dehydrogenase.
Function of the RAAS in Bmal1lox/lox/Ren1dCre Mice
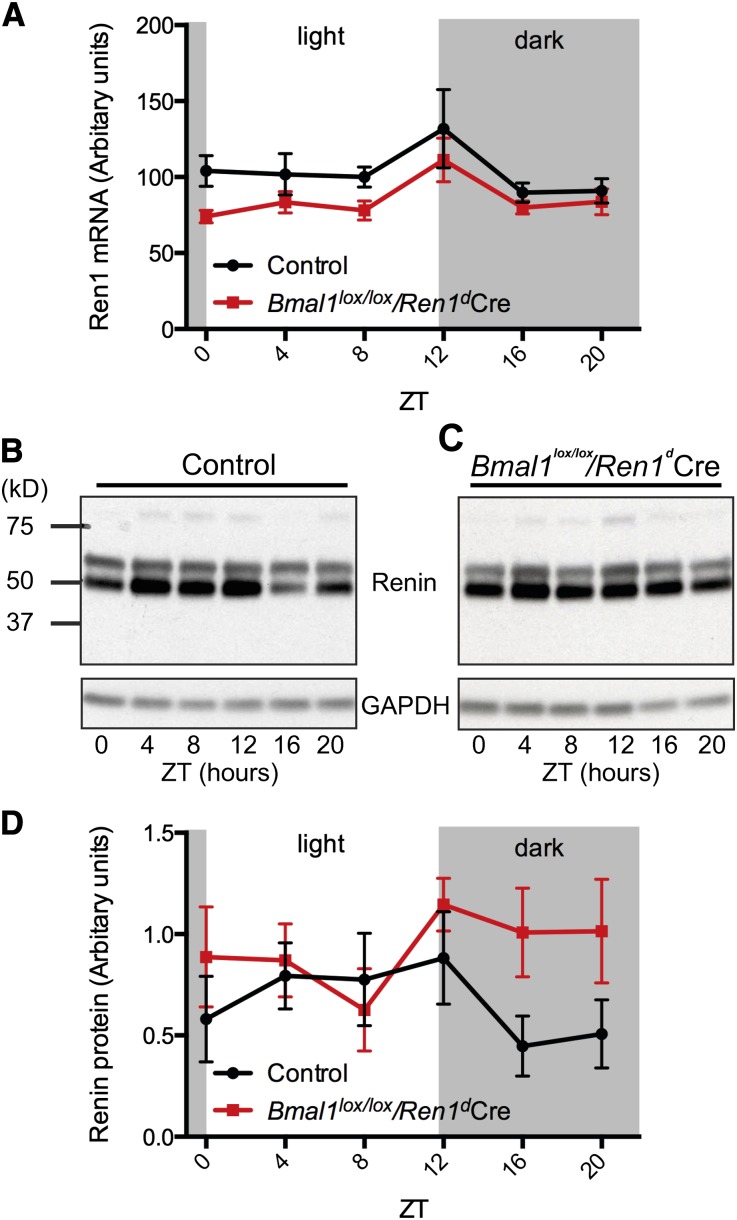
To assess the circadian pattern of the RAAS, mice were adapted to a 12-hour light/12-hour dark cycle for 2 weeks. Tissue and blood samples were collected from mice euthanized every 4 hours over the course of the circadian cycle. As shown in Figure 4A, kidneys from Bmal1lox/lox/Ren1dCre mice exhibited a moderate but significant reduction in Ren1 mRNA expression (P=0.003, ANOVA) (Supplemental Table 1). Western blot analysis revealed that renin protein levels follow a circadian-like pattern in kidneys of control mice, with peak levels during the dark (activity) phase (Figure 4, B and D). This pattern was disrupted in kidneys of Bmal1lox/lox/Ren1dCre mice (P=0.04, ANOVA) (Figure 4, C and D, Supplemental Table 1). We also performed qPCR analysis of cyclooxygenase-2 and peroxisome proliferator-activated receptor-γ, two genes that have been shown to be involved in the regulation of Renin synthesis and/or secretion. As shown in Supplemental Figure 6, the expression patterns of both cyclooxygenase-2 and peroxisome proliferator-activated receptor-γ were significantly changed in kidneys of Bmal1lox/lox/Ren1dCre mice.
Figure 4.
Circadian patterns of renin mRNA and protein expression are significantly modified in kidneys of Ren1dCre mice. Circadian patterns of renin mRNA and protein expression in control and Bmal1lox/lox/Ren1dCre mice. (A) Circadian pattern of renin mRNA expression in kidneys of control (black line) and Bmal1lox/lox/Ren1dCre (red line) mice (n=6/time point). Kidneys were extracted from mice euthanized at indicated circadian time points. Data are mean±SEM (n=6). Significant ANOVA factors: Pgenotype=0.003, Ptime=0.01. (B) Circadian pattern of renin protein expression in kidneys of control mice. This representative Western blot was performed on samples prepared by combining equivalent amounts of protein extracted from kidneys of six independent mice in each time point. (C) Circadian pattern of renin protein expression in kidneys of Bmal1lox/lox/Ren1dCre mice. This representative Western blot was performed on samples prepared by combining equivalent amounts of protein extracted from kidneys of six independent mice in each time point. (D) Densitometry analysis of Western blots performed on the individual samples of kidney protein extracts used in B (control mice; black line) and C (Bmal1lox/lox/Ren1dCre mice; red line; n=6/time point). Data are mean±SEM (n=6). Significant ANOVA factors: Pgenotype=0.04.
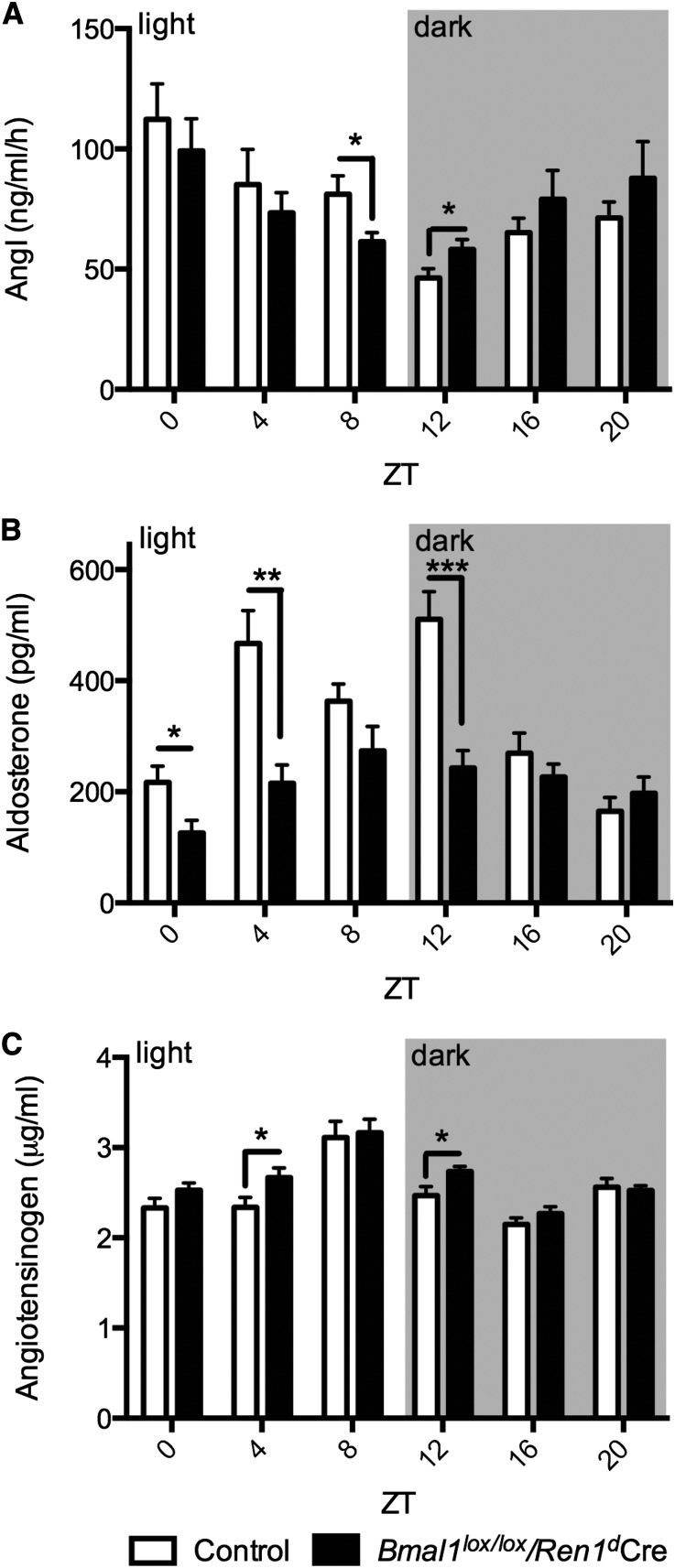
To assess the function of the RAAS, we examined circadian patterns of plasma renin concentrations (PRCs) and plasma aldosterone concentrations in control and Bmal1lox/lox/Ren1dCre mice (Figure 5). As shown in Figure 5, A and B, both the PRCs and plasma aldosterone concentrations exhibited robust circadian rhythms (P<0.001; peak-to-trough amplitude in the circadian rhythm of PRC: 142.0% in control mice, 70.4% in Bmal1lox/lox/Ren1dCre mice; peak-to-trough amplitude in the circadian rhythm of plasma aldosterone concentration: 216.9% in control mice, 117.8% in Bmal1lox/lox/Ren1dCre mice) (Supplemental Table 2). Interestingly, the plasma aldosterone concentration in control (Ren1dCre) mice follows a biphasic pattern, whereas previous studies in mice,8 rats,18 and humans19 have shown that plasma aldosterone concentration follows a bell-shaped circadian curve, with a single peak at the time of transition between the inactive and active periods of the day. A possible explanation for this phenomenon is that the Ren1dCre mice have a specific genetic background with only one copy of the Ren1d gene and one copy of the Ren2 gene.
Figure 5.
Circadian patterns of PRC, plasma aldosterone levels, and plasma angiotensinogen concentration are significantly modified in Ren1dCre mice. Circadian patterns of (A) PRC, (B) plasma aldosterone level, and (C) plasma angiotensinogen concentration in control (white bars) and Bmal1lox/lox/Ren1dCre (black bars) mice (n=10–12/time point). Data are mean±SEM (n=10–12 depending on time point); t test significance: *P<0.05; **P<0.01; ***P<0.005. Significant ANOVA factors: (A) Ptime<0.001; (B) Pgenotype<0.001, Ptime<0.001, Pinteraction<0.001; (C) Pgenotype=0.01, Ptime<0.001.
Importantly, the circadian phases of PRCs and plasma aldosterone concentrations were significantly different in both Bmal1lox/lox/Ren1dCre and control mice (PRC acrophases: ZT1 in control mice and ZT22 in Bmal1lox/lox/Ren1dCre mice; plasma aldosterone concentration acrophases: ZT9 in control mice and ZT10 in Bmal1lox/lox/Ren1dCre mice). ANOVA revealed that the plasma aldosterone concentration was significantly reduced in Bmal1lox/lox/Ren1dCre mice (P<0.001) (Figure 5B, Supplemental Table 1), whereas the PRC was not different from control mice (P=0.79) (Figure 5A, Supplemental Table 1). To address the difference in circadian phases between the PRC and plasma aldosterone concentration, we examined the circadian pattern of plasma angiotensinogen levels. As shown in Figure 5C and Supplemental Table 2, the plasma angiotensin levels exhibited circadian pattern similar to the pattern of plasma aldosterone levels, with the maximal values in the second one half of the light (inactivity) phase (plasma angiotensinogen levels acrophases: ZT8 in control mice and ZT7 in Bmal1lox/lox/Ren1dCre mice; peak-to-trough amplitude in the circadian rhythm of plasma angiotensinogen levels: 44.7% in control mice, 39.6% in Bmal1lox/lox/Ren1dCre mice). ANOVA revealed significant differences in plasma angiotensinogen levels between control and Bmal1lox/lox/Ren1dCre mice (P=0.01) (Supplemental Table 1). This difference, although statistically significant, was slight in absolute terms. Statistical analysis with t test showed moderate differences in plasma aldosterone concentration, PRC, and plasma angiotensinogen levels between control and Bmal1lox/lox/Ren1dCre mice at several time points of the circadian cycle.
Urine and Blood Chemistry, Renal Function, and BP in Bmal1lox/lox/Ren1dCre Mice
Analysis of 24-hour urine samples showed that Bmal1lox/lox/Ren1dCre mice exhibit a mild increase in urinary volume, a decrease in urine osmolality, and a tendency to hypercalciuria, hypermagnesuria, and decreased urinary pH (Table 1). In plasma samples, a significant decrease in plasma osmolality and a tendency to hypochloremia were observed (Table 1). The GFR measured at two circadian time points (ZT6 and ZT18) was significantly increased in Bmal1lox/lox/Ren1dCre mice (Table 1). Of note, in both control and Bmal1lox/lox/Ren1dCre mice, the GFR was significantly higher at ZT18 than ZT6 (control mice: P=0.002; Bmal1lox/lox/Ren1dCre mice: P<0.001; unpaired t test).
Table 1.
Twenty-four–hour urine and plasma chemistry in control and Bmal1lox/lox/Ren1dCre mice
| Control | Bmal1lox/lox/Ren1dCre | P Value | |
|---|---|---|---|
| Body weight (g) | 26.7±3.4 (33) | 26.5±2.4 (33) | NS |
| Urine | |||
| Volume/g body weight (ml/g) | 0.068±0.028 (33) | 0.084±0.029 (33) | 0.03 |
| Osmolality (mosm/kg H2O) | 2937±605 (12) | 2329±341 (12) | 0.01 |
| pH | 6.29±0.17 (12) | 6.11±0.23 (12) | 0.05 |
| UV×Na+/g body weight (μmol/g) | 11.8±3.2 (12) | 10.0±1.3 (12) | NS |
| UV×K+/g body weight (μmol/g) | 32.8±7.3 (12) | 29.6±3.2 (12) | NS |
| UV×Cl−/g body weight (μmol/g) | 20.5±3.9 (12) | 19.6±2.3 (12) | NS |
| UV×Ca2+/g body weight (μmol/g) | 0.13±0.03 (12) | 0.22±0.16 (12) | 0.06 |
| UV×Mg2+/g body weight (μmol/g) | 2.17±0.50 (12) | 2.67±0.70 (12) | 0.06 |
| UV×PO43−/g body weight (μmol/g) | 5.08±1.68 (12) | 5.80±1.96 (12) | NS |
| UV×creatinine/g body weight (μmol/g) | 0.52±0.09 (12) | 0.57±0.14 (12) | NS |
| UV×urea/g body weight (μmol/g) | 146.8±27.4 (12) | 146.9±19.6 (12) | NS |
| UV×urate/g body weight (μmol/g) | 78.3±14.2 (12) | 73.4±16.6 (12) | NS |
| UV×glucose/g body weight (μmol/g) | 0.21±0.03 (12) | 0.29±0.18 (12) | NS |
| UV×total protein/g body weight (mg/g) | 0.65±0.09 (12) | 0.48±0.20 (12) | 0.01 |
| Plasma | |||
| Osmolality (mosm/kg H2O) | 311.1±6.0 (9) | 305.1±3.6 (8) | 0.03 |
| Na+ (mM) | 158.2±0.7 (9) | 157.2±0.9 (9) | NS |
| K+ (mM) | 4.68±0.10 (9) | 4.74±0.16 (9) | NS |
| Cl− (mM) | 122.4±3.0 (9) | 110.0±2.1 (9) | 0.07 |
| Ca2+ (mM) | 2.12±0.10 (9) | 2.07±0.05 (9) | NS |
| Mg2+ (mM) | 1.28±0.09 (9) | 1.27±0.04 (9) | NS |
| Creatinine (μM) | 15.1±2.0 (9) | 15.9±3.0 (9) | NS |
| GFR | |||
| GFR ZT6 (μl/min) | 208.3±18.6 (6) | 263.2±34.5 (5) | 0.01 |
| GFR ZT18 (μl/min) | 322.9±19.1 (5) | 386.9±25.2 (5) | 0.002 |
Values are mean±SD. t test. UV, 24-hour urine volume.
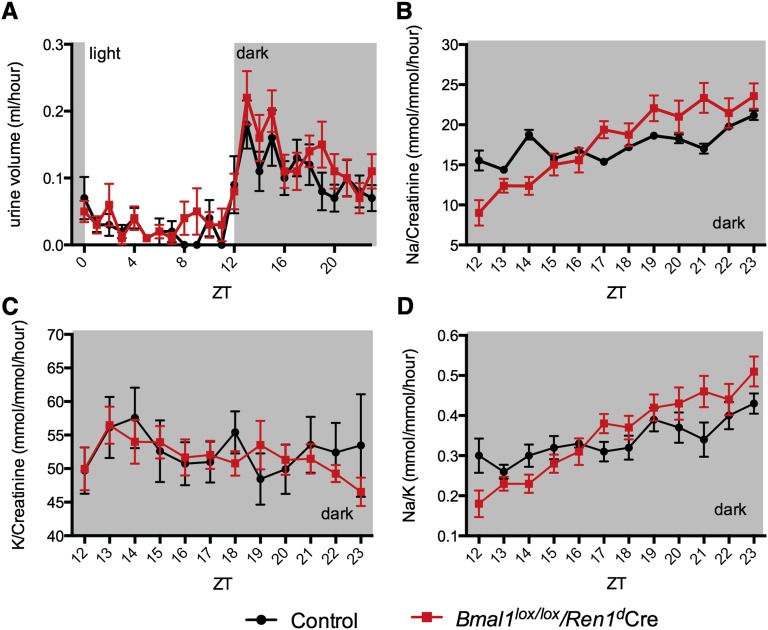
To assess the circadian rhythms of urinary water, sodium, and potassium excretion, urine was collected hourly from freely moving mice housed individually in metabolic cages. As shown in Figure 6A, there was no apparent difference in the circadian rhythms of urinary water excretion. The profiles of urinary sodium and potassium excretion were compared in the dark (activity) phase, where the accuracy of measurement is significantly higher because of higher volumes of collected urines. As shown in Figure 6, B and C, the profile of urinary sodium but not potassium excretion was significantly different between control and Bmal1lox/lox/Ren1dCre mice (P<0.001, interaction) (Supplemental Table 1). This difference was also present when the profiles of the urinary sodium to potassium ratio were compared (Figure 6D, Supplemental Table 1). Circadian expression analysis of several genes involved in renal sodium, potassium, and water handling (αENaC, NCC, Sgk1, ROMK, Aqp2, Aqp3, Aqp4, and Avpr2) revealed that all the selected genes, with the exception of Avpr2, exhibited a moderate but significant reduction in their mRNA expression levels at different time points of the circadian cycle (Supplemental Figure 7). The circadian analysis of plasma samples showed that both sodium and potassium levels exhibit circadian rhythms (Supplemental Table 2); however, there was no difference between control (Supplemental Figure 8A) and Bmal1lox/lox/Ren1dCre mice (Supplemental Figure 8B).
Figure 6.
Local renal circadian clocks control the dynamics of urinary sodium excretion. Circadian patterns of (A) urinary water, (B) sodium, and (C) potassium excretion and (D) urinary sodium-to-potassium ratios in control (black line) and Bmal1lox/lox/Ren1dCre (red line) mice. (A) Circadian pattern of urinary water excretion was determined on the urine collected hourly over the 24-hour circadian cycle. The dynamics of (B) urinary sodium and (C) potassium excretion and (D) the sodium-to-potassium ratio were determined on the urine collected hourly over the 12 hours of the activity phase of the circadian cycle (ZT12–ZT24). Data are mean±SEM (n=21). Significant ANOVA factors: (B) Ptime<0.001, Pinteraction<0.001; (C) Ptime=0.01; (D) Ptime<0.001, Pinteraction<0.001.
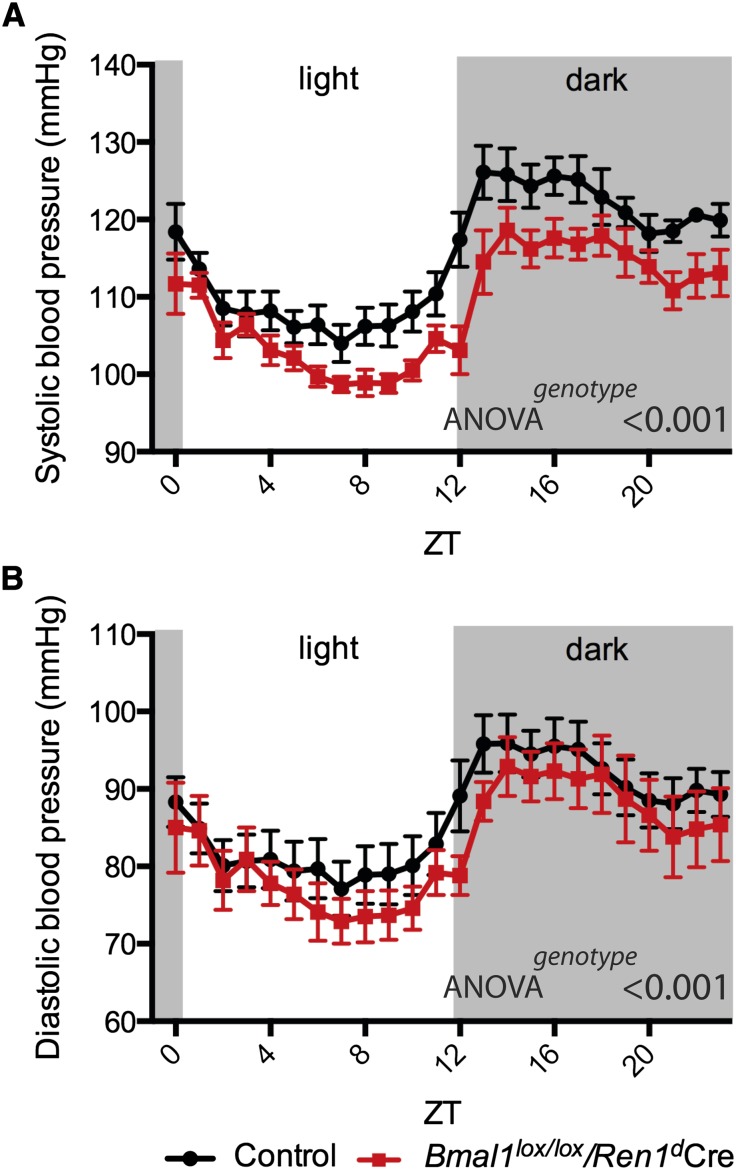
The BP was measured in conscious unrestrained mice using telemetry. As shown in Figure 7, both the systolic and diastolic BPs were significantly decreased in Bmal1lox/lox/Ren1dCre mice (BP recordings over 6 days are shown in Supplemental Figure 9).
Figure 7.
Local renal circadian clocks are required for BP control. (A) Systolic and (B) diastolic BP in control (black line) and Bmal1lox/lox/Ren1dCre (red line) mice. For each mouse, a mean of 6-day recordings was calculated (the 6-day recordings are shown in Supplemental Figure 9); then, the mean of these values was determined for each genotype. Data are mean±SEM (n=7 for both genotypes). Significant ANOVA factors: (B) Ptime<0.001, Pgenotype<0.001.
Discussion
Accumulating evidence suggests that most, if not all, physiologic functions are controlled by the circadian timing system. Although it is generally presumed that peripheral circadian clocks are involved in these regulatory mechanisms, there are only a limited number of studies that have addressed this question experimentally. For instance, Storch et al.14 have shown that the retinal intrinsic circadian clocks have a significant role in visual function. Marcheva et al.20 have shown that the inactivation of the circadian clock in pancreatic islets causes diabetes mellitus because of dysfunction of β cells. In the kidney, the presence of the high-amplitude circadian rhythms in the expression of the circadian clock genes has been evidenced in several studies.8,15,16 However, the functional role of the local renal circadian clocks has not been studied. To address this question, we crossed mice with floxed Bmal1 gene with mice expressing the Cre recombinase under the endogenous promoter of the renin gene. The latter model has been widely used for the conditional inactivation of different genes expressed in the renin-secreting granular cells of the juxtaglomerular apparatus in the kidney.21–29 These studies showed that, at the whole-organ level, the Ren1dCre is strongly expressed in the kidney, whereas in other tested tissues, the Cre expression was at or near background levels.24 Nota bene, clearly, however, these results did not exclude that there might be minor populations of Cre-expressing cells in other tissues as well. These studies also showed that, within the kidney, the Cre expression is not limited to the granular cells but also present in the rest of the afferent arterioles, the interlobular renal arteries, and the tubular segments.13 For instance, Kurt et al.29 have shown the presence of the CRE protein in the collecting duct. Here, we confirmed the tissue expression pattern of Ren1dCre and showed that, in the kidney of Bmal1lox/lox/Ren1dCre mice, the BMAL1 protein is absent in renin-secreting granular cells, the CCD, and the OMCD. Surprisingly, we also found a significant reduction of BMAL1 protein levels in the MTAL. Because to our knowledge, the expression of the renin gene in the thick ascending limb cells has not been reported, additional studies are needed to explain this finding. Collectively, these results suggest that (1) the Bmal1 inactivation in Bmal1lox/lox/Ren1dCre mice is largely kidney-specific and (2) within the kidney, the inactivation of the circadian clock mechanism occurs in subpopulations of both vascular and tubular epithelial cells.
Functional analysis of Bmal1lox/lox/Ren1dCre mice has shown that the local renal circadian clocks are involved in a wide variety of specific homeostatic functions, including the maintenance of sodium, water, calcium, magnesium, chloride, and pH balance. Interestingly, the phenotype of Bmal1lox/lox/Ren1dCre mice is quite similar to the phenotype observed in the total (whole-body) knockout of Clock (clock−/− mice).8,15 The common features include mild polyuria, changes in the circadian pattern of urinary sodium excretion, significant decrease in plasma aldosterone levels, and low BP. Both models also display a circadian time point-dependent reduction in expression levels of several transcripts involved in water and sodium balance (Aqp2, Aqp4, αENaC, and Sgk1). These similarities suggest that, at least in part, the phenotype of clock−/− mice has a renal origin.
Analysis of the renin-angiotensin-aldosterone axis revealed that Bmal1lox/lox/Ren1dCre mice exhibit significant changes in circadian patterns of renin protein and mRNA expression levels in the kidney. However, these changes did not result in the alteration of the PRC. Hence, these results indicate that factors other than renin are responsible for the decreased plasma aldosterone levels and low BP in Bmal1lox/lox/Ren1dCre mice. A surprising finding of our study is that the circadian rhythms of the PRC and plasma aldosterone concentration display nearly opposite circadian phases in both control and Bmal1lox/lox/Ren1dCre mice. The circadian pattern of plasma aldosterone concentration in mice has been examined in several studies, and all of the studies showed the existence of a robust circadian rhythm that reaches its maximum at the time of transition between the light and dark phases.8,9 The circadian variability in plasma aldosterone concentration and/or PRC has been shown in rats,30 humans,31 and dogs.32 To our knowledge, our study is the first to report the circadian pattern of the PRC in mice, which exhibits its maximum at the time of transition between the dark and light phases. These results suggest a provocative hypothesis that circadian rhythmicity in plasma aldosterone concentrations and potentially, BP in mice is determined by the circadian rhythms in plasma angiotensinogen levels and not the rhythmicity in available renin. To some extent, this hypothesis is supported by the study by Kim et al.,33 which showed by using angiotensinogen gene titration in mice that differences in hepatic angiotensinogen mRNA expression were positively correlated with the expression of aldosterone synthase in adrenal glands and negatively correlated with renin expression in the kidney. Alternatively, these findings may suggest that circadian rhythmicity in plasma aldosterone concentrations in mice is mostly determined by the circadian clock-driven mechanisms in adrenal glands.9
An intriguing phenotype of Bmal1lox/lox/Ren1dCre mice is glomerular hyperfiltration, which is not associated with proteinuria or glucosuria. Because the major mechanism of hyperfiltration is the reduction in the vascular resistance of the afferent arteriole, it is tempting to speculate that the circadian clock in the afferent arteriole has a direct effect on the afferent arteriole contractility. An increase in nitric oxide production in tubular cells is an alternative mechanism that could explain this phenomenon.34,35
Collectively, functional analysis of Bmal1lox/lox/Ren1dCre mice has shown that the local renal circadian clocks are involved in a variety of specific renal functions and BP control. The specificity in establishing genotype–phenotype correlations in circadian clock-deficient models consists in the highly pleiotropic role of circadian clocks on both transcriptional/translational and functional levels. Indeed, recent estimates suggest that the circadian clock system controls thousands of genes in a cell type–dependent manner.36 Accordingly, it is not surprising that disruption of circadian clocks in renal cells results in a multitude of functional disturbances. In this study, the circadian clock system was disrupted only in a fraction of renal cell types, whereas the adult kidney is composed of more than 25 terminally differentiated cell types, each of which possesses its own circadian clock. Future studies are needed to fully explore the role of each of these clock systems in renal function.
Concise Methods
Animals
The procedures used to generate and the characterization of Bmal1lox/lox and Ren1dCre mice were described previously.13,14,17,29 The Bmal1lox/lox and Ren1dCre mice were crossed to obtain Bmal1lox/+/Ren1dCre mice. The Bmal1lox/+/Ren1dCre mice were crossed with either Bmal1lox/lox or Bmal1+/+ mice separately to obtain the Bmal1lox/lox/Ren1dCre and Bmal1+/+/Ren1dCre mice; 3- to 5-month-old Bmal1lox/lox/Ren1dCre or Ren1dCre (control) male mice were used in all experiments. The animals were maintained ad libitum on the standard laboratory chow diet (KLIBA NAFAG diet 3800). Before all experiments, mice were adapted to a 12-hour light/ dark cycle. All experiments with animals were performed in accordance with the Swiss guidelines for animal care, which conform to the National Institutes of Health animal care guidelines.
Antibodies
Anti-Cre recombinase antibody was from Novagen. Anti-BMAL1 antibody has been described elsewhere.17 Anti–Aquaporin-2 and antiglyceraldehyde-3-phosphate dehydrogenase antibodies were from Santa Cruz Biotechnology, Antiuromodulin antibody was from LS-Bio. Antiactin antibody was from Sigma-Aldrich. Anti-Renin antibody was from Fitzgerald. Immunohistochemistry and Western blotting protocols are available in Supplemental Material.
Metabolic Cages
Mice were housed in individual metabolic cages (Tecniplast). Urine collection was performed after a 3-day adaptation period. Urine and blood chemistry was analyzed as previously described.8 Hourly urine collection was performed as previously described.8
Blood Levels of RAAS Components
PRC was determined by radioimmunoassay (DPC) according to a previously published protocol.37 Angiotensinogen concentration was determined with mouse total angiotensinogen assay kit from IBL. Plasma aldosterone level was measured by radioimmunoassay (DPC).
GFR
The GFR was determined according to the method described by Qi et al.38
Statistical Analyses
Data are presented as mean±SEM or mean±SD as indicated in the figures. The tests used include the two-tailed unpaired t test and ANOVA. ANOVAs were performed with genotype (control, Bmal1lox/lox/Ren1dCre), time (ZT0, ZT4, ZT8, ZT12, ZT16, and ZT20), and interaction between time and genotype as factors. When possible, the mouse-to-mouse variability was taken into account by adding a factor for individual mice in the ANOVA model. P values are indicated in figures. A P value <0.05 was considered significant. Statistical analysis of circadian oscillations was performed as previously described.15
Disclosures
None.
Supplementary Material
Acknowledgments
This work was supported by Swiss National Science Foundation Research Grant 31003A-132496 (to D.F.) and a grant from the Novartis Foundation (to D.F.).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Tick Tock: Time to Recognize the Kidney Clock,” on pages 1369–1371.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2013060641/-/DCSupplemental.
References
- 1.Saini C, Suter DM, Liani A, Gos P, Schibler U: The mammalian circadian timing system: Synchronization of peripheral clocks. Cold Spring Harb Symp Quant Biol 76: 39–47, 2011 [DOI] [PubMed] [Google Scholar]
- 2.Bass J: Circadian topology of metabolism. Nature 491: 348–356, 2012 [DOI] [PubMed] [Google Scholar]
- 3.Curtis AM, Cheng Y, Kapoor S, Reilly D, Price TS, Fitzgerald GA: Circadian variation of blood pressure and the vascular response to asynchronous stress. Proc Natl Acad Sci USA 104: 3450–3455, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vukolic A, Antic V, Van Vliet BN, Yang Z, Albrecht U, Montani JP: Role of mutation of the circadian clock gene Per2 in cardiovascular circadian rhythms. Am J Physiol Regul Integr Comp Physiol 298: R627–R634, 2010 [DOI] [PubMed] [Google Scholar]
- 5.Wang Q, Maillard M, Schibler U, Burnier M, Gachon F: Cardiac hypertrophy, low blood pressure, and low aldosterone levels in mice devoid of the three circadian PAR bZip transcription factors DBP, HLF, and TEF. Am J Physiol Regul Integr Comp Physiol 299: R1013–R1019, 2010 [DOI] [PubMed] [Google Scholar]
- 6.Stow LR, Richards J, Cheng KY, Lynch IJ, Jeffers LA, Greenlee MM, Cain BD, Wingo CS, Gumz ML: The circadian protein period 1 contributes to blood pressure control and coordinately regulates renal sodium transport genes. Hypertension 59: 1151–1156, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Firsov D, Bonny O: Circadian regulation of renal function. Kidney Int 78: 640–645, 2010 [DOI] [PubMed] [Google Scholar]
- 8.Nikolaeva S, Pradervand S, Centeno G, Zavadova V, Tokonami N, Maillard M, Bonny O, Firsov D: The circadian clock modulates renal sodium handling. J Am Soc Nephrol 23: 1019–1026, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doi M, Takahashi Y, Komatsu R, Yamazaki F, Yamada H, Haraguchi S, Emoto N, Okuno Y, Tsujimoto G, Kanematsu A, Ogawa O, Todo T, Tsutsui K, van der Horst GT, Okamura H: Salt-sensitive hypertension in circadian clock-deficient Cry-null mice involves dysregulated adrenal Hsd3b6. Nat Med 16: 67–74, 2010 [DOI] [PubMed] [Google Scholar]
- 10.Lieu SJ, Curhan GC, Schernhammer ES, Forman JP: Rotating night shift work and disparate hypertension risk in African-Americans. J Hypertens 30: 61–66, 2012 [DOI] [PubMed] [Google Scholar]
- 11.Rubinstein S, Wang C, Qu W: Occupational risk and chronic kidney disease: A population-based study in the United States adult population. Int J Nephrol Renovasc Dis 6: 53–59, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Woon PY, Kaisaki PJ, Bragança J, Bihoreau MT, Levy JC, Farrall M, Gauguier D: Aryl hydrocarbon receptor nuclear translocator-like (BMAL1) is associated with susceptibility to hypertension and type 2 diabetes. Proc Natl Acad Sci U S A 104: 14412–14417, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sequeira López ML, Pentz ES, Nomasa T, Smithies O, Gomez RA: Renin cells are precursors for multiple cell types that switch to the renin phenotype when homeostasis is threatened. Dev Cell 6: 719–728, 2004 [DOI] [PubMed] [Google Scholar]
- 14.Storch KF, Paz C, Signorovitch J, Raviola E, Pawlyk B, Li T, Weitz CJ: Intrinsic circadian clock of the mammalian retina: Importance for retinal processing of visual information. Cell 130: 730–741, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zuber AM, Centeno G, Pradervand S, Nikolaeva S, Maquelin L, Cardinaux L, Bonny O, Firsov D: Molecular clock is involved in predictive circadian adjustment of renal function. Proc Natl Acad Sci USA 106: 16523–16528, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gachon F, Olela FF, Schaad O, Descombes P, Schibler U: The circadian PAR-domain basic leucine zipper transcription factors DBP, TEF, and HLF modulate basal and inducible xenobiotic detoxification. Cell Metab 4: 25–36, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Jouffe C, Cretenet G, Symul L, Martin E, Atger F, Naef F, Gachon F: The circadian clock coordinates ribosome biogenesis. PLoS Biol 11: e1001455, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gomez-Sanchez C, Holland OB, Higgins JR, Kem DC, Kaplan NM: Circadian rhythms of serum renin activity and serum corticosterone, prolactin, and aldosterone concentrations in the male rat on normal and low-sodium diets. Endocrinology 99: 567–572, 1976 [DOI] [PubMed] [Google Scholar]
- 19.Armbruster H, Vetter W, Uhlschmid G, Zaruba K, Beckerhoff B, Nussberger J, Vetter H, Siegenthaler W: Circadian rhythm of plasma renin activity and plasma aldosterone in normal man and in renal allograft recipients. Proc Eur Dial Transplant Assoc 11: 268–276, 1975 [PubMed] [Google Scholar]
- 20.Marcheva B, Ramsey KM, Buhr ED, Kobayashi Y, Su H, Ko CH, Ivanova G, Omura C, Mo S, Vitaterna MH, Lopez JP, Philipson LH, Bradfield CA, Crosby SD, JeBailey L, Wang X, Takahashi JS, Bass J: Disruption of the clock components CLOCK and BMAL1 leads to hypoinsulinaemia and diabetes. Nature 466: 627–631, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gomez RA, Pentz ES, Jin X, Cordaillat M, Sequeira Lopez ML: CBP and p300 are essential for renin cell identity and morphological integrity of the kidney. Am J Physiol Heart Circ Physiol 296: H1255–H1262, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neubauer B, Machura K, Chen M, Weinstein LS, Oppermann M, Sequeira-Lopez ML, Gomez RA, Schnermann J, Castrop H, Kurtz A, Wagner C: Development of vascular renin expression in the kidney critically depends on the cyclic AMP pathway. Am J Physiol Renal Physiol 296: F1006–F1012, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sequeira-Lopez ML, Weatherford ET, Borges GR, Monteagudo MC, Pentz ES, Harfe BD, Carretero O, Sigmund CD, Gomez RA: The microRNA-processing enzyme dicer maintains juxtaglomerular cells. J Am Soc Nephrol 21: 460–467, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Desch M, Schreiber A, Schweda F, Madsen K, Friis UG, Weatherford ET, Sigmund CD, Sequeira Lopez ML, Gomez RA, Todorov VT: Increased renin production in mice with deletion of peroxisome proliferator-activated receptor-gamma in juxtaglomerular cells. Hypertension 55: 660–666, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen L, Faulhaber-Walter R, Wen Y, Huang Y, Mizel D, Chen M, Sequeira Lopez ML, Weinstein LS, Gomez RA, Briggs JP, Schnermann J: Renal failure in mice with Gsalpha deletion in juxtaglomerular cells. Am J Nephrol 32: 83–94, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen L, Kim SM, Eisner C, Oppermann M, Huang Y, Mizel D, Li L, Chen M, Sequeira Lopez ML, Weinstein LS, Gomez RA, Schnermann J, Briggs JP: Stimulation of renin secretion by angiotensin II blockade is Gsalpha-dependent. J Am Soc Nephrol 21: 986–992, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kurt B, Kurtz L, Sequeira-Lopez ML, Gomez RA, Willecke K, Wagner C, Kurtz A: Reciprocal expression of connexin 40 and 45 during phenotypical changes in renin-secreting cells. Am J Physiol Renal Physiol 300: F743–F748, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Castellanos Rivera RM, Monteagudo MC, Pentz ES, Glenn ST, Gross KW, Carretero O, Sequeira-Lopez ML, Gomez RA: Transcriptional regulator RBP-J regulates the number and plasticity of renin cells. Physiol Genomics 43: 1021–1028, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kurt B, Paliege A, Willam C, Schwarzensteiner I, Schucht K, Neymeyer H, Sequeira-Lopez ML, Bachmann S, Gomez RA, Eckardt KU, Kurtz A: Deletion of von Hippel-Lindau protein converts renin-producing cells into erythropoietin-producing cells. J Am Soc Nephrol 24: 433–444, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rodríguez-Sargent C, Cangiano JL, Martínez-Maldonado M: Circadian rhythms of plasma renin levels in the anesthetized rat. Ren Physiol 5: 53–56, 1982 [DOI] [PubMed] [Google Scholar]
- 31.Williams GH, Cain JP, Dluhy RG, Underwood RH: Studies of the control of plasma aldosterone concentration in normal man. I. Response to posture, acute and chronic volume depletion, and sodium loading. J Clin Invest 51: 1731–1742, 1972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mochel JP, Fink M, Peyrou M, Desevaux C, Deurinck M, Giraudel JM, Danhof M: Chronobiology of the renin-angiotensin-aldosterone system in dogs: Relation to blood pressure and renal physiology. Chronobiol Int 30: 1144–1159, 2013 [DOI] [PubMed] [Google Scholar]
- 33.Kim HS, Lee G, John SW, Maeda N, Smithies O: Molecular phenotyping for analyzing subtle genetic effects in mice: Application to an angiotensinogen gene titration. Proc Natl Acad Sci USA 99: 4602–4607, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anea CB, Cheng B, Sharma S, Kumar S, Caldwell RW, Yao L, Ali MI, Merloiu AM, Stepp DW, Black SM, Fulton DJ, Rudic RD: Increased superoxide and endothelial NO synthase uncoupling in blood vessels of Bmal1-knockout mice. Circ Res 111: 1157–1165, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anea CB, Zhang M, Stepp DW, Simkins GB, Reed G, Fulton DJ, Rudic RD: Vascular disease in mice with a dysfunctional circadian clock. Circulation 119: 1510–1517, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koike N, Yoo SH, Huang HC, Kumar V, Lee C, Kim TK, Takahashi JS: Transcriptional architecture and chromatin landscape of the core circadian clock in mammals. Science 338: 349–354, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim SM, Mizel D, Huang YG, Briggs JP, Schnermann J: Adenosine as a mediator of macula densa-dependent inhibition of renin secretion. Am J Physiol Renal Physiol 290: F1016–F1023, 2006 [DOI] [PubMed] [Google Scholar]
- 38.Qi Z, Whitt I, Mehta A, Jin J, Zhao M, Harris RC, Fogo AB, Breyer MD: Serial determination of glomerular filtration rate in conscious mice using FITC-inulin clearance. Am J Physiol Renal Physiol 286: F590–F596, 2004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.