Abstract
Objectives:
The primary aim of this study is to evaluate the success rate of immediately inserted dental implants in sinus lift and the secondary aim is to assess the reliability of performing simultaneous surgery for sinus lift, grafting and implant placement in situations of very low residual bone heights (<4 mm) in the posterior maxillae.
Materials and Methods:
A series of consecutive patients who sought dental implant rehabilitation were included in this study. The sinus lift cases were selected and divided into two groups based on the maxillary alveolar height, ≥4 mm of radiographically measurable bone height (Group 1) and < 4 mm of bone height (Group 2).
Results:
A total of 13 implants were installed in Group 1, whereas 8 implants were installed in Group 2. The success rate for dental implants in the sinus lifts reached 95.2% after a period of 24 months of evaluation, at 100% for Group 1 (bone height ≥ 4 mm) and 87.5% for Group 2 (bone height with < 4 mm). Besides the differences between the percentages of success, statistical differences were not reached when the groups were compared (Fisher's exact test, P = 0.38).
Conclusions:
Despite the limitations of this study, including its low number of participants, the results indicate that simultaneous surgery for sinus lifting, grafting and dental implants in posterior maxillae with very low bone heights (<4 mm) can be performed safely, although with lower success rates than found in patients with higher residual bone heights (>4 mm).
Keywords: Dental implants, immediate dental implants, sinus lift
INTRODUCTION
Dentists are constantly seeking improvements in surgical and prosthetic techniques to reduce treatment time in dental implant therapy.[1] The current implant surfaces have improved bone-implant unions and accelerate bone healing mainly by reducing the osseointegration period and accelerating prosthetic rehabilitation.[1,2,3] Treatments involving reconstructive procedures have still shown no significant improvements in treatment time reductions, despite the development of several bone substitutes. In most cases, it is necessary to wait 4-6 months for bone graft incorporation before installing dental implants, thus greatly increasing the treatment period.[4]
In vertical deficiencies of the posterior region of the maxilla, the main alternative is sinus lift. This technique can be carried out in one or more phases, depending upon the quantity of basal bones (height). The literature suggests that the minimum bone height needed to install the implants in the same surgery is 4-5 mm. In ridges with lower heights, a two-phase procedure is recommended.[3,4,5,6,7,8,9,10,11] In situations where the implants are installed in the same procedure, the total treatment time may be reduced by up to 6 months, while the morbidity, costs and total period of treatment are all lessened considerably.[12] The aim of this study is to evaluate the success rate of immediately inserted dental implants in sinus lift areas and to assess the reliability of performing simultaneous surgery for sinus-lifting, grafting and implant placement in situations of very low residual bone heights (<4 mm) in the posterior maxillae.
MATERIALS AND METHODS
Between March and August 2008, a series of consecutive patients who sought dental implant rehabilitation were included in this study. Exclusion criteria were absolute surgical contraindications or lacerations of the Schneiderian membrane during the surgical procedure [Figure 1]. Smokers and patients with controlled systemic diseases were included.
Figure 1.

Perforation for the maxillary sinus membrane precluding the graft and dental implant procedures
After the determination of implant positioning, the amount of remaining bone in the region where the implants would be installed was measured directly by a panoramic radiograph using a digital micrometer (Western®). Those maxillary sinus cases where the residual bone height was ≥4 mm were included in Group 1 (control), while those maxillary sinus cases where the bone height was <4 mm were included in Group 2 (test) [Figure 2].
Figure 2.

Panoramic radiograph showing the very low residual bone height in the posterior maxillae
The day before the surgery, mouth rinses with chlorhexidine gluconate 0.12% was given. 3 h before the procedure, 8 mg of dexamethasone was given orally and 1 h before the procedure, 1 g of Cephadroxil was given, also orally. After surgery, the patients were kept on Cephadroxil for 7 days, at 1 g in two divided doses. Pain was controlled using acetaminophen 500 mg up to 4 times a day or as necessary.
The incision was made at the alveolar crest and after the subperosteal detachment, an osteotomy was conducted between 10 and 13 mm from the ridge crest in order to gain access to the maxillary sinus with a spherical number 8 diamond drill, taking care not to tear the sinus membrane. Appropriate elevators were used to detach the sinus membrane, creating the area for the bone graft [Figure 3]. The Schneiderian membrane was then protected and the perforations for dental implants were performed. Bovine collagen membrane (Gen-derm®, Mogi Mirim-SP, Brazil) was placed in the region above and distal with the objective of delimiting the cavity to be filled by the biomaterial (Hydroxyapatite; Osteogen®) and obliterating possible unobserved micro-perforations of the membrane. In this simultaneous procedure, the augmentation material was first packed into the medial aspect of the cavity; then, the implants were partially inserted to assess the primary stability. The augmentation material was then packed and condensed into the residual space and the implants were finalized [Figure 4]. The mucoperiostal flap was realigned and sutured. No membrane was used to cover the facial defect in the sinus wall.
Figure 3.
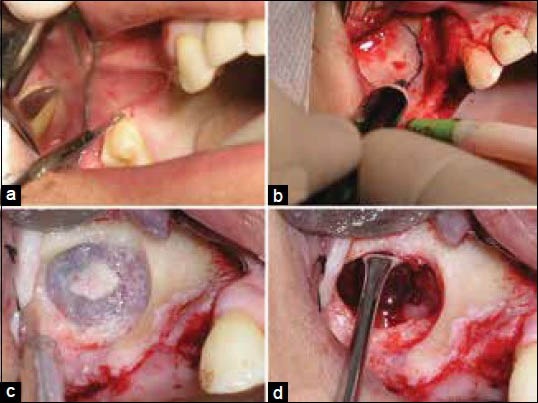
Sinus lift surgical procedure. (a) Incision done, (b) Drawing the surgical ostectomy, (c) Exposure of the maxillary sinus membrane, (d) Elevator used to detach the sinus membrane, creating the region for the bone graft
Figure 4.
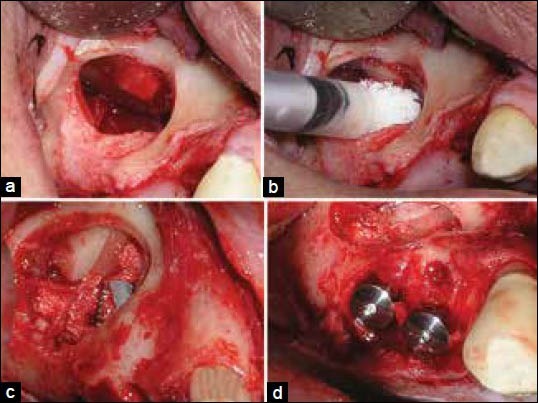
Graft and dental implant procedures. (a) Sinus lift area prepared with Bovine collagen membrane (Gen-derm®, Mogi Mirim-SP, Brazil) placed, (b) Cavity being filled with the biomaterial (Hydroxyapatite; Osteogen®), (c) Dental implant being inserted immediately in the sinus lift area partially filled with augmentation material, (d) Dental implants in place
The areas were opened again 6 months after surgery. During the surgery, the implants underwent a counter-torque of 25 N/cm2 with a manual prosthetic torque wrench corresponding to the installed implant system. If the implant did not present movement, it was considered as osseointegrated and therefore to have secondary stability. After the installation of the prostheses, their rehabilitation was evaluated at 3, 6, 9, 12, 18 and 24 months using the clinical and radiographic examination [Figure 5].
Figure 5.
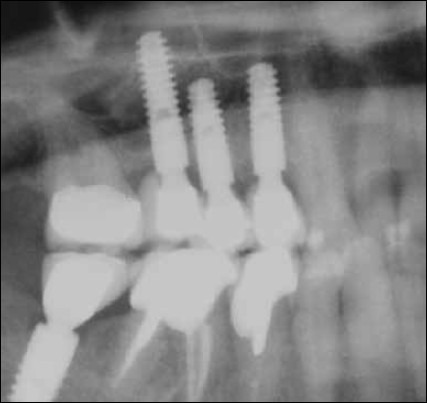
Radiograph showing dental implants and prosthesis in the sinus lift area
Statistical data analysis
The normality test (Kolmogorov-Smirnov test), followed by a non-parametric test (Mann-Whitney U-test) and was used for the statistical analysis of the regions of implant placement (bone height). A Chi-squared test was used to compare differences between the groups according to the distribution of patients and implants, as well as surgical procedures.
RESULTS
From March to August 2008, nine patients underwent 13 maxillary sinus elevation procedures. In those procedures, 21 implants were installed, 13 in Group 1 (controls) and 8 in Group 2 (test). As expected, the amounts of bone height remaining between Groups 1 and 2 were statistically different (Mann-Whitney U-test, P < 0.001). The cases are described in Tables 1 and 2, for the control and test groups, respectively.
Table 1.
Description of the cases of sinus lifting, the remaining bone height, type and brand of inserted implant for the control group (Group 1)
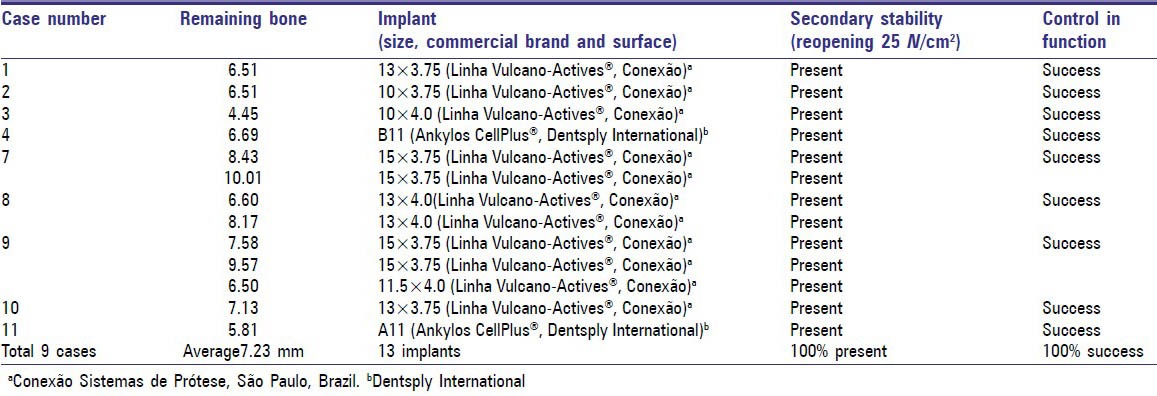
Table 2.
Description of the cases of sinus lifting, the remaining bone height, type and brand of inserted implant for the test group (Group 2)

All implants from the test and control groups presented osseointegration after a counter-torque of 25 N/cm2 at re-opening surgery (6 months after installation). One implant in the test group was lost after 3 months of function [Table 2].
The success rate for dental implants in the sinus lift area reached 95.2% after a period of 24 months of evaluation, at 100% for Group 1 (bone height ≥ 4 mm) and 87.5% for Group 2 (bone height with <4 mm). Besides the differences between the percentages of success, statistical differences were not reached when the groups were compared (Fisher's exact test, P = 0.38).
DISCUSSION
The rehabilitation of partially or totally edentulous patients with implant-supported prostheses has become common practice in dentistry; however, the posterior maxilla frequently represents a challenge because of the lack of bone due to alveolar ridge resorption and maxillary sinus pneumatization.[3] The maxillary sinus elevation technique (sinus-lift) is one of the most commonly used strategies for dental implant rehabilitation in atrophic posterior maxillae; for this protocol, several studies have claimed success rates >90%, with control periods ranging from 1 to 9 years of follow-up.[3,4,5,6,12,13,14,15,16]
Some of the authors consider that, when sinus pneumatization is relevant (residual height of <4 mm), sinus-grafting procedures can be safely and predictably used;[3] however, it is not clear whether both implants and sinus-lift-grafting could be performed within the same surgical procedure. Aiming to reduce the treatment times, the present study observed that it is reliable to install the dental implants during the same surgery during which the reconstructive technique is performed, regardless of the recommended minimum residual bone height of 4 mm.[4,5,6,11] Besides the low number of patients enrolled and the limitations of this research, our results are encouraging, indicating that simultaneous surgery for sinus lifting, grafting and dental implants in the posterior maxilla with very low bone heights can be performed safely, although with lower (but not statistically significant) success rates when compared with procedures on patients with greater amounts of remaining bone height. It was also possible to observe that the employed biomaterial fulfilling the sinus area was previsible, bringing about a low rate of material loss and high rate of osseointegration.
The results of the present study contradict the consensus conference on sinus lifting.[7] According to those authors,[7] when the residual bone height belongs to class C (residual bone height 4-6 mm), a lateral approach involving a grafting material with immediate or delayed implants is advocated; when the residual bone height belongs to class D (residual bone height 1-3 mm), a lateral approach involving a bone grafting material and delayed implant placement is recommended. In this study, we observed a single case of implant loss in the test group that occurred 3 months after the installation of the prosthesis. For this particular case, we believe that the torque and counter-torque procedures needed for UCLA abutments were responsible for the losses associated with systemic conditions, since the patient was a heavy smoker.
This present study also gives support to the current literature showing that performing a single step for the sinus floor elevation, grafting and dental implant placement has a high success rate.[9,10,17,18]
CONCLUSION
Despite the limitations of this study, including its low number of participants, the results indicate that simultaneous surgery for sinus lifting, grafting and dental implants in posterior maxillae with very low bone heights (<4 mm) can be performed safely, although with lower success rates than found in patients with higher residual bone heights (>4 mm).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Albrektsson T, Sennerby L, Wennerberg A. State of the art of oral implants. Periodontol 2000. 2008;47:15–26. doi: 10.1111/j.1600-0757.2007.00247.x. [DOI] [PubMed] [Google Scholar]
- 2.Le Guehennec L, Goyenvalle E, Lopez-Heredia MA, Weiss P, Amouriq Y, Layrolle P. Histomorphometric analysis of the osseointegration of four different implant surfaces in the femoral epiphyses of rabbits. Clin Oral Implants Res. 2008;19:1103–10. doi: 10.1111/j.1600-0501.2008.01547.x. [DOI] [PubMed] [Google Scholar]
- 3.Chiapasco M, Zaniboni M. Methods to treat the edentulous posterior maxilla: Implants with sinus grafting. J Oral Maxillofac Surg. 2009;67:867–71. doi: 10.1016/j.joms.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 4.Kahnberg KE, Vannas-Löfqvist L. Sinus lift procedure using a 2-stage surgical technique: I. Clinical and radiographic report up to 5 years. Int J Oral Maxillofac Implants. 2008;23:876–84. [PubMed] [Google Scholar]
- 5.Raghoebar GM, Vissink A, Reintsema H, Batenburg RH. Bone grafting of the floor of the maxillary sinus for the placement of endosseous implants. Br J Oral Maxillofac Surg. 1997;35:119–25. doi: 10.1016/s0266-4356(97)90687-2. [DOI] [PubMed] [Google Scholar]
- 6.Peleg M, Mazor Z, Chaushu G, Garg AK. Sinus floor augmentation with simultaneous implant placement in the severely atrophic maxilla. J Periodontol. 1998;69:1397–403. doi: 10.1902/jop.1998.69.12.1397. [DOI] [PubMed] [Google Scholar]
- 7.Jensen OT, Shulman LB, Block MS, Iacono VJ. Report of the Sinus Consensus Conference of 1996. Int J Oral Maxillofac Implants. 1998;13(Suppl):11–45. [PubMed] [Google Scholar]
- 8.Tiwana PS, Kushner GM, Haug RH. Maxillary sinus augmentation. Dent Clin North Am. 2006;50:409–24. doi: 10.1016/j.cden.2006.03.004. vii. [DOI] [PubMed] [Google Scholar]
- 9.Chen TW, Chang HS, Leung KW, Lai YL, Kao SY. Implant placement immediately after the lateral approach of the trap door window procedure to create a maxillary sinus lift without bone grafting: A 2-year retrospective evaluation of 47 implants in 33 patients. J Oral Maxillofac Surg. 2007;65:2324–8. doi: 10.1016/j.joms.2007.06.649. [DOI] [PubMed] [Google Scholar]
- 10.Jurisic M, Markovic A, Radulovic M, Brkovic BM, Sándor GK. Maxillary sinus floor augmentation: Comparing osteotome with lateral window immediate and delayed implant placements. An interim report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:820–7. doi: 10.1016/j.tripleo.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 11.de Vicente JC, Hernández-Vallejo G, Braña-Abascal P, Peña I. Maxillary sinus augmentation with autologous bone harvested from the lateral maxillary wall combined with bovine-derived hydroxyapatite: Clinical and histologic observations. Clin Oral Implants Res. 2010;21:430–8. doi: 10.1111/j.1600-0501.2009.01877.x. [DOI] [PubMed] [Google Scholar]
- 12.Lambert F, Lecloux G, Rompen E. One-step approach for implant placement and subantral bone regeneration using bovine hydroxyapatite: A 2- to 6-year follow-up study. Int J Oral Maxillofac Implants. 2010;25:598–606. [PubMed] [Google Scholar]
- 13.Fugazzotto PA, Vlassis J. Long-term success of sinus augmentation using various surgical approaches and grafting materials. Int J Oral Maxillofac Implants. 1998;13:52–8. [PubMed] [Google Scholar]
- 14.Rodriguez A, Anastassov GE, Lee H, Buchbinder D, Wettan H. Maxillary sinus augmentation with deproteinated bovine bone and platelet rich plasma with simultaneous insertion of endosseous implants. J Oral Maxillofac Surg. 2003;61:157–63. doi: 10.1053/joms.2003.50041. [DOI] [PubMed] [Google Scholar]
- 15.Peleg M, Garg AK, Mazor Z. Predictability of simultaneous implant placement in the severely atrophic posterior maxilla: A 9-year longitudinal experience study of 2132 implants placed into 731 human sinus grafts. Int J Oral Maxillofac Implants. 2006;21:94–102. [PubMed] [Google Scholar]
- 16.Manfro R, Nascimento WR, Jr, Loureiro JA, Bortoluzzi MC, Zago CR. Success evaluation of 20 cases of maxillary sinus lifting with filled with 1:1 mixture of particulate, autogenous and Gen-Ox-anorganic bones-A two-year follow-up study. Impl News. 2009;6:39–46. [Google Scholar]
- 17.Aguirre Zorzano LA, Rodríguez Tojo MJ, Aguirre Urizar JM. Maxillary sinus lift with intraoral autologous bone and B - Tricalcium phosphate: Histological and histomorphometric clinical study. Med Oral Patol Oral Cir Bucal. 2007;12:E532–6. [PubMed] [Google Scholar]
- 18.Lee BK. One-stage operation of large oroantral fistula closure, sinus lifting, and autogenous bone grafting for dental implant installation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:707–13. doi: 10.1016/j.tripleo.2007.09.020. [DOI] [PubMed] [Google Scholar]


