Abstract
Background:
Although the periorbital region forms less than 1% of the total body surface, it has a very complex anatomy; therefore, it requires a detailed approach. In this work, we aim to present the clinical applications and related literature for the algorithm of the technique which will be applied, according to the location of the defect, in choosing the surgery treatment method. Factors affecting the results and different treatment methods of the anatomical region, including its difficult reconstruction, will also be included.
Materials and Methods:
A review of 177 periorbital region defect reconstructions was performed.
Results:
As a treatment method, in 76 (43%) patients primary closure was chosen, 39 (22%) patients had grafts and in 62 (35%) patients a flap was chosen as a treatment alternative. With respect to postoperative complications, there were a total of 6 (3.38%) patients observed with venous congestion. In 11 (6.21%) patients ectropion developed, in 1 (0.56%) patient minimal space between the eyelids while monitoring recovery was observed and in 1 (0.56%) patient, flap loss was observed due to a circulatory disorder.
Conclusions:
The aim of reconstruction is to repair the defect suitable to normal physiological and anatomical values. As a result, before the surgical treatments in this difficult anatomical region, the defect width and anatomical localization must be evaluated. The most suitable reconstruction method must be identified, using an evaluation of the algorithm and the required functional and esthetical results can be obtained with intraoperative flexible behavior and a change of method, when necessary.
Keywords: Algorithm, periorbital defects, reconstruction
INTRODUCTION
The periorbital region forms less than 1% of the total body surface and due to its complex anatomy, it requires a detailed approach.[1] The soft-tissue defects of this region occur in trauma, tumors, burns, radiation, infection and congenital anomalies.[2,3] The aims of the ideal reconstruction of the periorbital region are: (1) To provide ocular surface lubricity and form an internal layer in the smooth mucus membrane structure, protecting against corneal irritation. (2) To form tars that imitates the shape and hardness of the lid. (3) To form fixed lid edges with the lashes out of corneal contact. (4) To obtain medial and lateral ligaments for stability and movement of the lid. (5) To provide enough muscles for the necessary tonus for the movement of the lid. (6) To form a thin skin, allowing for lid movement. (7) To provide enough levator movement to lift the upper lid and (8) To obtain an esthetical image.[4] Due to these reasons, the construction of this region still includes some difficulties for reconstructive surgeons.
The surgical techniques that are used in the reconstruction of the periorbital region change, according to the periorbital region zone of defect, how the eyelid is affected as a percentage, or the full or partial layer thickness of the defect. The surgical techniques applied in this region include: Split thickness skin grafting, Tenzel rotational flap, lid switch flap, Cutler-Beard flap, forehead flap, glabellar flap, tarsoconjunctival advancement (Hughes), Tripier, Mustarde's lid switch flap, nasolabial flap and local flaps.[1,5]
In this work, we aim to present the clinical applications and related literature for the algorithm of the technique, which will be applied according to the location of the defect, in choosing the surgery treatment method, factors affecting the results and different treatment methods of this anatomical region with difficult reconstruction.
MATERIALS AND METHODS
In this study, the patients were studied retrospectively, those who reported during a 4-year period to the Ministry of Health, Dışkapı Yıldırım Beyazıt Training Research Hospital at the plastic, reconstructive and esthetic surgery clinic for treatment of a periorbital region defect. In this way, 177 patients were obtained and evaluated in terms of age; gender; cause, location and size of defect; surgery treatment methods applied; form of anesthesia; and the different flap alternatives applied.
RESULTS
The age distribution ranged between 8 and 77 years, with 80 (45.2%) of the patients being women and 97 (54.8%) of the patients being men. The overall average patient age was 58.50 years, with the average age of the men being 56.78 and of women being 60.22 years. Of these patients, 132 were operated on with local anesthesia, while 45 of them were operated on under general anesthesia.
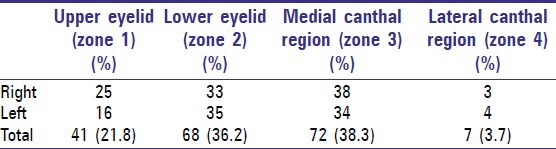
The defect cause in 170 (96.05%) of the patients were tumoral lesions, in 6 (3.39%) patients there was trauma and in 1 (0.56%) patient there was a congenital eyelid defect. The tumoral lesions were observed in 148 (87.1%) patients as basal cell carcinoma, in 8 (4.8%) patients as squamous cell carcinoma, in 3 (1.8%) patients as hemangioma, in 7 (4.1%) patients as nevi, in 2 (1.1%) patients as pyogenic granuloma and in 2 (1.1%) patients as papilloma. The localizations of the defects are summarized in Table 1.
Table 1.
Localization of defects
As a treatment method, 76 (43%) patients were treated with direct (primary) closure (10 were full section defects depending on wedge excision, the other 66 were partial section defects). Grafts were given to 39 (22%) patients and in 62 (35%) patients a flap was chosen as the treatment alternative.
The flap treatments included forehead flaps in eight patients (12.9%), glabellar flaps in eight patients (12.9%), Mustarde flaps in nine patients (14.5%), V-Y flaps from the cheek in five patients (8%), V-Y flaps from the upper eyelid in five patients (8%), lid switch flaps (for upper eyelid defects) in two patients (3.3%), Tripier flaps (for lower eyelid defects) in five patients (8%), Fricke flaps in three patients (4.9%) (two patients for upper, one patient for lower eyelid defects), medially based orbicularis oculi myocutaneous flap for a medial canthal region defect in one patient (1.6%), superficial temporal artery frontal branch based island flaps in four patients (6.5%) (2 for lower, 2 for upper eyelid defects), temporoparietal fascia flap in one patient (1.6%) for an upper eyelid defect and a nasolabial flap was used in two patients (3.3%) for lower eyelid defects. In nine patients (14.5%) reconstruction using local flaps (Limberg, rotation and transposition) was used.
With respect to postoperative complications, a total of 6 (3.38%) patients were observed with venous congestion, including two patients having upper eyelid V-Y flaps, two patients having superficial temporal artery frontal branch based island flaps, one patient having a Tripier flap and one patient having a medially based orbicularis oculi myocutaneous flap. With medical dressing, recovery was obtained and a second intervention was not needed. In 10 patients having skin grafts and one patient having a Mustarde cheek flap (total of 11 [6.21%] patients) ectropion developed. These complications were corrected in the skin graft cases by redoing the graft and by applying temporary tarsorrhaphy. In the cheek flap case the complication was corrected by excision and lateral suspension. In 1 (0.56%) patient having an upper V-Y flap, there was minimal space between the eyelids, which was closely monitored during recovery. In 1 (0.56%) patient having a superficial temporal artery frontal branch based island flap, the loss was observed according to a circulatory disorder. The defect that formed after debridement was closed using local flaps.
DISCUSSION
The periorbital region requires different and special care in terms of reconstruction, because of its complex anatomy and important structures. This area was divided into five anatomical regions by Spinelli in order to promote the localization of defects and reconstruction. These regions include: Zone 1, upper eyelid; Zone 2, lower eyelid; Zone 3, medial canthal region; Zone 4, lateral canthal region; Zone 5, other facial regions related to these regions.[2] In Table 2, our clinical applications of the surgery technique algorithms, which can be used in defects of each region, were summarized with the related literature.
Table 2.
Periorbital reconstructive algorithm, based on the zones
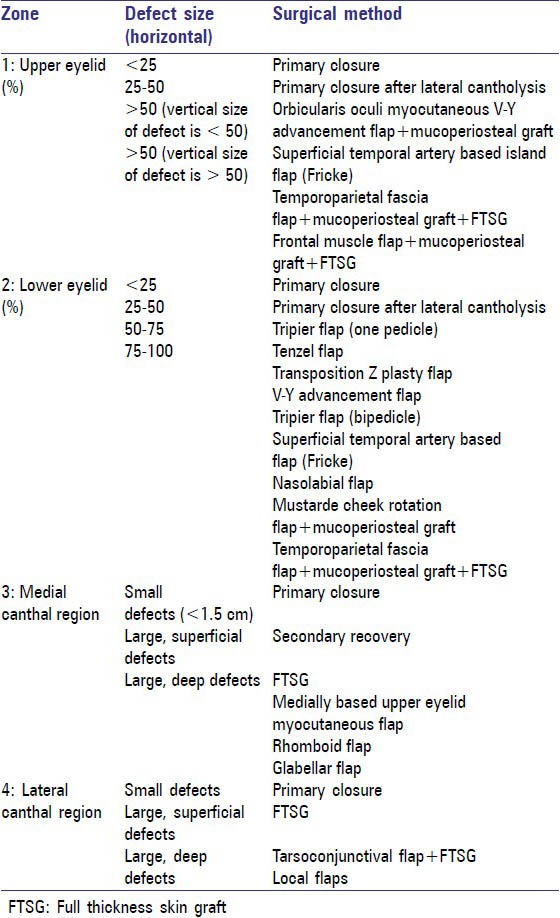
Zone 1-upper eyelid
There are many different methods defined in the upper eyelid reconstruction. A retroangular flap can be an excellent option in properly selected cases for both upper and lower eyelid reconstruction. Tan et al. believe that the thickness of the flap can safely be modified according to the site, size and depth of the defect, because the retroangular flap is an arterial flap with a reliable vascular supply. It may be thinned to accommodate more superficial defects, such as those on the eyelid.[6] The Tessier flap has been defined for the reconstruction of total or subtotal defects of the lower eyelid.[7] When there was tissue lateral of the eyelid, the Tessier flap modification was used for total or subtotal defects of the upper eyelid. The flap angular artery base was planned vertically to the orbitonasal angle and 90° could be transposed. The posterior lamella is repaired with a buccal mucosa graft and the flap donor field was covered directly or with a full skin graft. The modified Tessier flap, which Avram et al. defined, can be used as a single-row method in 60% or more upper eyelid defects.[8]
The nasal chondromucosal flap is another method that is generally used in repairing total or subtotal upper eyelid defects. This method was first defined by Micali et al. as a nasal lateral full thickness mucosal-chondrocutaneous flap. However, the most important disadvantage of this flap is its thickness, providing full layer tissue reconstruction. Scuderi et al. used this method in the repair of an ipsilateral axial chondromucosal flap (posterior lamella) and they also modified the anterior lamella by repairing it with a graft or local flaps. They reported that with thickness in a flap like this, there was no thinning process needed later.[9] However, in this situation, the process was more complicated.
In the upper eyelid edge full layer defects, the repair of the posterior lamella using a mucosal graft and anterior lamella using a bipediculated myocutaneous flap, was also described. From the upper part of the defect, a bipediculated flap is taken forward to the defect and the flap donor region is covered with a Fricke (temporofrontal) flap.[10] In some studies, as in this method, a Tripier flap was used as bipediculated for upper eyelid edge partial defects.[11] However, this flap should not be used for wide upper eyelid defects. Additionally, in this method, there are more than one donor region scars.
Another method used in limited defects is the myotarsocutaneous V-Y flap. It is a procedure in which there is a lateral canthal region for enough support and for repairing 25-50% of the defects of the upper eyelid. It involves the flap tars and conjunctiva, it is elevated with the orbicular muscle flap and the flap is taken forward horizontally.[12]
Among two new methods are those of Jean and Brusati. Raymond et al. (in more than 50% of upper eyelid defects) reported repairing posterior lamella defects by using palatal mucoperiosteal grafts and repairing anterior lamella defects by lifting the frontal muscle flaps and using full layer skin grafts, going in from the maximum limit of the upper eyelid defect.[13] The frontal muscle, which is used in this method, is only lifted to a vascular bed which feeds the skin graft of the upper lamella and for the mucoperiosteal graft which forms the lower lamella. In this situation, there is a morbidity of the muscle, irrelevant to the defect. Brusati et al. used forehead galeal flaps to fix wide defects of the upper eyelid. The repair of the posterior lamella was done using a buccal mucosal graft and the anterior part of the galeal flap was closed with a retroauricular skin graft.[14] However, in this method the morbidity of the donor region is greater.
In partial or total full layer defects of the upper eyelid, two step reconstruction methods were also described. In the first step, the posterior lamella was repaired by lifting the tarsoconjunctival flap from the donor lower eyelid, whereas the anterior lamella was closed by a full thickness skin graft. In the second step, after 5-8 weeks, the flap is separated. Mauriello et al. used a modified Hughes method analogue in the full layer defect reconstruction of the tarsoconjunctival flap of the lower eyelid. Due to this, it was named the “reverse” modified Hughes method.[15]
In this article, the orbicularis oculi V-Y flap has an important place in the reconstruction of upper eyelid defects. The orbicularis oculi myocutaneous V-Y advancement flap was first defined by Demir et al. in 2008.[5] This method can be used horizontally in 100% defects, although the defect cannot involve more than 50% of the upper eyelid vertical length. In partial or full thickness defects, it can be a repair option, while in full layer defects (for repair of the posterior lamella) a mucoperiosteal graft is taken from the palatine. The flap is planned as a reverse V, with a similar width to the upper part of the defect and is elevated to involving the orbicularis oculi muscle and taken forward to adapt onto the defect. This method is a reconstruction option which is one step, easy to apply, available for use in all defects, suitable for the anatomy, has a minimum donor region scar and is not a prohibitor for sight [Figure 1].[5]
Figure 1.

(a) Preoperative appearance of the tumoral lesion in the left upper eyelid, (b) Appearance of the planning after excision, (c) Appearance of the split thickness upper eyelid defect after excision and harvested orbicularis oculi myocutaneous V-Y advancement flap, (d) Postoperative appearance of the normal closure of the eyelid
Zone 2-lower eyelid
When we searched the literature, we found that the lateral nasal artery based island mucochondrocutaneous flap is another flap alternative for total eyelid loss. With this method, a single repair is done with a flap involving all elements (skin, muscle and conjunctiva) of the eyelid. There is only one donor region and it is covered primarily without causing functional or esthetical deformation. The disadvantages are the difficulty of the dissection and the formation of bulk tissue that has the potential of forming an unacceptable size and esthetic problems in most cases.[16]
In total layer defects of the lower eyelid, between 30% and 60% (defects of 60% of the anterior lamella with less posterior lamella loss) include the defined orbicularis oculi muscle skin flap, involving a tarsoconjunctival island from the upper eyelid. Its advantages include: Suitable tissue, involving all elements of the eyelid, not necessary to cover the eye after operation, single step and can be done under local anesthesia. Its disadvantages are: Care must be taken when separating the levator muscle on the tars from the insertion, causing trauma and dysfunction of a muscle, possibility of opening between eyelids and being technically difficult.[17] Atik et al. presented a new technique using a combination of the cross-upper eyelid and conchal cartilage for the reconstruction of the lower eyelid.[18]
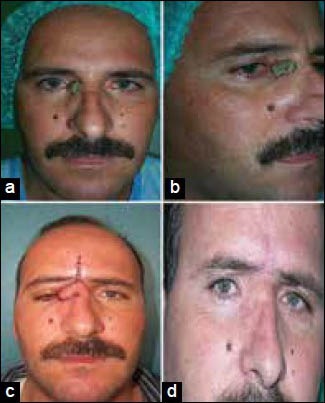
The cheek rotation flap (Mustarde cheek flap) is the best known method for the reconstruction of wide defects in lower eyelids. This method was applied to nine patients [Figure 2]. In this technique for a total thickness repair, there is a need for lining tissue to support the cheek flap. Chondromucosal, mucoperiosteal and conchal cartilage grafts are preferred. Today, instead of cartilage, homologs or otologs of fascia latae are used for support. The fascia latae on the medial canthal tendon and lateral orbital rim is fixed. Then the fascia latae and the inner part of flap are covered by a buccal mucosa graft. In this case, the irritation of the cornea and conjunctiva is lessened. With this method for total and subtotal defects, an efficient horizontal tensile power can be maintained with one step.[19] The possible complication of this method is an ectropion risk, which we observed in one patient.
Figure 2.

(a) Preoperative appearance of the tumoral lesion in the right lower eyelid, (b) Appearance of the split thickness lower eyelid defect, after excision, and harvested Mustarde cheek rotation flap, (c) Postoperative appearance of the early result, (d) Postoperative appearance of the late result
Hocaoğlu et al. used a temporoparietal fascia flap in a pediatric case having a full layer defect. In repairing the posterior lamella, a nasal septal chondromucosal graft was used, whereas the anterior part was covered with a retroauricular graft. As a result, it is possible to provide an aesthetic result that causes no donor scar in an observable region.[20]
The flap surgery techniques that we use frequently are: Mustarde cheek flap, Tripier, V-Y, superficial temporal artery frontal branch based island flap and nasolabial flap [Figure 3]. In partial thickness defects, the Tripier or V-Y flap were preferred, whereas in wide and full layer defects, the Mustarde cheek flap was used, with regard to the tissue laxity of the patient. We do not prefer these methods in the reconstruction of Zone 2 defects which prevent temporary vision, as they are two step methods of upper eyelid repair and do not to cause any morbidity in the upper eyelid or discomfort for the patient.
Figure 3.

(a) Preoperative appearance of the tumoral lesion in the right lower eyelid, (b) Appearance of the preoperative two-different planing, (c) Appearance of the full thickness lower eyelid defect, after excision, and harvested superficial temporal artery frontal branch based island flap, (d) Postoperative appearance of the early result
Zone 3-medial canthal region
The V-Y flap from the medial eyelid skin, lower eyelid flaps, superior based bilobe flap, forehead and glabellar flaps are the methods that can be used in this region.[1,21,22] The glabellar flap is a thick flap that has the disadvantage of forming bulk tissue. It requires a secondary thinning operation and the flap pediculate must be departed, causing an obvious donor region scar. Apart from these, the Hughes and Cutler-Beard flaps can be used, which are two-step methods and sight is prohibited. However, these must be kept for the defects on the edge of the eyelid.[1,21]
The important point in the reconstruction of Zone 3 is scaffolding of the tarsoligament on the bone. If there are any canthal tendons, these can be used for scaffolding. If there are no canthal tendons, nasal periosteal flaps are prepared and used for support. This provides the fixation of the upper and lower eyelids. The other important structure in that region is the lacrimal drainage system, which can be protected by intubation with a silicone tube during reconstruction. In malignant lesions, especially, wide excisions involving the lacrimal system can be done as a necessity of tumor surgery, if necessary. The reconstruction of the lacrimal system can be left for afterwards and the covering of the defect can be planed as a first step.
For the reconstruction of this region, Goldstein defined the medially based myocutaneous flap from the upper eyelid in 1983. The anatomical base of the flap was shown by Corso in 1961. The major perforators that feed this flap originate from the supratrochlear and infratrochlear vessels. In the literature, this flap has been reported as thin, secure, having good accordance with skin color, having less donor region morbidity, single step and can be used in multiple ways.[23]
We use direct covering in small defects clinically; however, in repairing superficial wide defects, total thickness skin grafts are used. In deep and wide defects, the repair was done with flaps and the glabellar and forehead flaps were frequently used. We sometimes prefer lower lid and cheek V-Y flaps, V-Y-S-plasty, rhomboid and rotation flaps [Figure 4]. Although the glabellar flap and forehead flaps are thick and the color accordance is less, in this study, they are preferred in the patients that have deep and wide Zone 3 defects and in some patients with a shortage of tissue, including the lateral nose.
Figure 4.
(a) Preoperative anterior appearance of the tumoral lesion in the right medial canthal region, (b) Preoperative oblique appearance of the tumoral lesion in the right medial canthal region, (c) Postoperative appearance of the early result of the glabellar flap, (d) Postoperative appearance of the late result of the glabellar flap
Zone 4-lateral canthal region
In the reconstruction of this region, as well as in lateral canthal tendon defects, tendons must be scaffolded to the lateral orbital wall by permanent stitching. Laxity, which can be observed in elderly patients, can be fixed by plication.[24] If the defect also involves the eyelids, repairs can be done by using methods such as the tarsoconjunctival flap, Cutler-Beard flap and Hughes flap, which are used in Zone 1 and 2 defects. Local flaps, such as the rotation and rhomboid flaps, are other alternatives that can be used in reconstruction.[1]
In general, defects in this region are rarely seen, compared with other regions and we prefer to cover small defects directly and use random patterned local flaps for wide defects. Lateral canthal tendon reconstruction was done for stability of the eyelid in necessary cases.
In periorbital regional defects, the option for the reconstruction method relates to the wideness of the defect. In addition, the location and depth of the defect, its relationship to the anatomical structures and the age of the patient are the important factors in choosing the method. The aim of reconstruction is to repair the defect suitable to normal physiologic and anatomic values. The tissues used for periorbital region reconstruction must involve good vascularized thin, flexible skin, muscle, tarsoligamentous and mucosal membranes. The tissues that have these characteristics are usually neighboring structures.[2,3] Eyelids are formed of the anterior lamella, which involves skin and muscle with posterior lamella, involving conjunctiva, tarsal plaques and eyelid retractors. In eyelid reconstructions, at least one of these lamellas must be reconstructed with vascularized tissues.[24]
As a result, before surgical treatment in this difficult anatomical region, the defect width and anatomical localization must be evaluated. According to this, the most suitable reconstruction method must be identified with the evaluation of the algorithm and the required functional and esthetic results can be obtained with intraoperative flexible behavior, as well as changing the method when necessary.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Codner MA. Reconstruction of the eyelids and orbit. In: Coleman JJ 3rd, editor. Plastic Surgery Indications, Operations and Outcomes. Ch. 87. Vol. 3. St. Louis: Mosby; 2000. pp. 1425–64. Sayfa. [Google Scholar]
- 2.Spinelli HM, Jelks GW. Periocular reconstruction: A systematic approach. Plast Reconstr Surg. 1993;91:1017–24. [PubMed] [Google Scholar]
- 3.Köse R. Periorbital yumuşak dokuların onarımı. Fırat Tıp Derg. 2005;10:12–7. [Google Scholar]
- 4.Patel BC, Flaharty PM, Anderson RL. Reconstruction of the eyelids. In: Baker SR, Swanson NA, editors. Local Flaps in Facial Reconstruction. Ch. 16. St. Louis: Mosby; 1995. [Google Scholar]
- 5.Demir Z, Yüce S, Karamürsel S, Celebioglu S. Orbicularis oculi myocutaneous advancement flap for upper eyelid reconstruction. Plast Reconstr Surg. 2008;121:443–50. doi: 10.1097/01.prs.0000297649.71049.ae. [DOI] [PubMed] [Google Scholar]
- 6.Tan O, Atik B, Ergen D. The retroangular flap revisited. Dermatol Surg. 2007;33:1343–9. doi: 10.1111/j.1524-4725.2007.33287.x. [DOI] [PubMed] [Google Scholar]
- 7.Tessier P. New York, NY: Masson Publishing USA, Inc; 1981. Eyelid reconstruction or blepharopoesis in plastic surgery of the orbit and eyelids. [Google Scholar]
- 8.Avram DR, Hurwitz JJ, Kratky V. Modified Tessier flap for reconstruction of the upper eyelid. Ophthalmic Surg. 1991;22:467–9. [PubMed] [Google Scholar]
- 9.Scuderi N, Ribuffo D, Chiummariello S. Total and subtotal upper eyelid reconstruction with the nasal chondromucosal flap: A 10-year experience. Plast Reconstr Surg. 2005;115:1259–65. doi: 10.1097/01.prs.0000156774.66841.0f. [DOI] [PubMed] [Google Scholar]
- 10.Moschella F, Cordova A. Upper eyelid reconstruction with mucosa-lined bipedicled myocutaneous flaps. Br J Plast Surg. 1995;48:294–9. doi: 10.1016/0007-1226(95)90067-5. [DOI] [PubMed] [Google Scholar]
- 11.Elliot D, Britto JA. Tripier's innervated myocutaneous flap 1889. Br J Plast Surg. 2004;57:543–9. doi: 10.1016/j.bjps.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 12.Okada E, Iwahira Y, Maruyama Y. The V-Y advancement myotarsocutaneous flap for upper eyelid reconstruction. Plast Reconstr Surg. 1997;100:996–8. doi: 10.1097/00006534-199709001-00025. [DOI] [PubMed] [Google Scholar]
- 13.Jean RD, Wong WW, Martin MC. Single-stage frontalis muscle flap for full-thickness reconstruction of the upper eyelid. J Craniofac Surg. 2011;22:1762–4. doi: 10.1097/SCS.0b013e31822e6321. [DOI] [PubMed] [Google Scholar]
- 14.Brusati R, Colletti G, Redaelli V. Upper eyelid reconstruction with forehead galeal flap. J Plast Reconstr Aesthet Surg. 2009;62:901–5. doi: 10.1016/j.bjps.2007.11.055. [DOI] [PubMed] [Google Scholar]
- 15.Mauriello JA, Jr, Antonacci R. Single tarsoconjunctival flap (lower eyelid) for upper eyelid reconstruction (“reverse” modified Hughes procedure) Ophthalmic Surg. 1994;25:374–8. [PubMed] [Google Scholar]
- 16.Porfiris E, Georgiou P, Harkiolakis G, Popa CV, Sandris P, Sgouras N. Island mucochrondrocutaneous flap for reconstruction of total loss of the lower eyelid. Plast Reconstr Surg. 1997;100:104–7. doi: 10.1097/00006534-199707000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Porfiris E, Christopoulos A, Sandris P, Georgiou P, Ioannidis A, Popa CV, et al. Upper eyelid orbicularis oculi flap with tarsoconjunctival island for reconstruction of full-thickness lower lid defects. Plast Reconstr Surg. 1999;103:186–91. doi: 10.1097/00006534-199901000-00030. [DOI] [PubMed] [Google Scholar]
- 18.Atik B, Tan O, Bekerecioglu M, Cinal A, Tekes L. Reconstruction of lower eyelid defects using a cross upper eyelid flap composited with ear cartilage. Dermatol Surg. 2007;33:709–12. doi: 10.1111/j.1524-4725.2007.33147.x. [DOI] [PubMed] [Google Scholar]
- 19.Matsumoto K, Nakanishi H, Urano Y, Kubo Y, Nagae H. Lower eyelid reconstruction with a cheek flap supported by fascia lata. Plast Reconstr Surg. 1999;103:1650–4. doi: 10.1097/00006534-199905060-00011. [DOI] [PubMed] [Google Scholar]
- 20.Hocaoğlu E, Özden BÇ, Aydın H. Lower eyelid reconstruction in a paediatric face: A one-stage aesthetic approach using the versatile temporoparietal fascia flap. J Plast Reconstr Aesthet Surg. 2012;65:e246–9. doi: 10.1016/j.bjps.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 21.Perry JD, Taban M. Superiorly based bilobed flap for inferior medial canthal and nasojugal fold defect reconstruction. Ophthal Plast Reconstr Surg. 2009;25:276–9. doi: 10.1097/IOP.0b013e3181ac76dd. [DOI] [PubMed] [Google Scholar]
- 22.Tan O. An algorythmic approach to restoration of the fronto-naso-periorbital skin defects using the forehead flaps. J Craniomaxillofac Surg. 2010;38:11–8. doi: 10.1016/j.jcms.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 23.Jelks GW, Glat PM, Jelks EB, Longaker MT. Medial canthal reconstruction using a medially based upper eyelid myocutaneous flap. Plast Reconstr Surg. 2002;110:1636–43. doi: 10.1097/01.PRS.0000033020.40691.B2. [DOI] [PubMed] [Google Scholar]
- 24.Jewett BS, Shockley WW. Reconstructive options for periocular defects. Otolaryngol Clin North Am. 2001;34:601–25. doi: 10.1016/s0030-6665(05)70008-6. [DOI] [PubMed] [Google Scholar]


