Abstract
Introduction:
Parry-Romberg syndrome (PRS) is a progressive, irreversible disorder characterized by facial lipoatrophy. The patients’ physical and psychological well-being is highly affected. The choice of graft for correction of PRS is dictated by numerous factors. This qualitative study aims to present the patients choice of graft for PRS.
Materials and Methods:
Reports of experience of patients surgically treated for PRS in the period of 2000-2011 are presented.
Result:
A total of 36 patients who had undergone the PRS treatment with fat grafts fulfilled the criteria and were included for the study. Of them 17 (47.2%) were males and 19 (52.8%) were females. For these patients, grafts were obtained from the abdomen in 22 (61.1%) and 14 (38.9%) from the gluteal region. Female PRS patients preferred to have the scar in their gluteal region rather than abdominal region. Similarly, in their immediate postoperative period, most of the patients were apprehensive about the over correction but where satisfied with the long term results of the surgery.
Discussion:
Female PRS patients whose donor site was gluteal region had better perception than those with abdominal grafting. Similarly in immediate postoperative period, they felt that their outcome was not satisfactory. The morphology and metabolic activity of gluteal adipocytes are unique and probably accounts for the better survival rates.
Keywords: Lipoatrophy, Parry-Romberg syndrome, patient preference, scar, subdermal fat grafting
INTRODUCTION
Parry-Romberg syndrome (PRS) is a rare condition where in there is an irreversible, progressive facial hemiatrophy. The disease process begins insidiously that causes a self-limited reduction of the subcutaneous tissue volume along one half of the face. The changes begin by the appearance of scar-like skin changes leading to progressive atrophy of the subcutaneous and adipose tissue, trigeminal neuralgia and changes in the hair and eyes. In severe cases, bone involvement in the form of osteoporosis is observed.[1]
Discoloration and localized loss of hair or alopecia areata, followed by thinning of skin, subcutaneous tissue are usual signs of initiation of the disease. Though may start from any part of the face, it is predominantly seen in areas innervated by the trigeminal nerve and often limiting to one half of the face. With the progression of the disease, depletion of subcutaneous tissue leads to marked craniofacial asymmetry, which leads to esthetic discomfort. This discomfort weakens self-esteem, potentially affecting normal psychological growth and intellectual development of the patient.[1] Several authors have postulated various etiopathogenesis for this uncommon degenerative condition. Some of the theories include cerebral disturbance of fat metabolism, vascular insult to the trigeminal ganglia, trauma, viral infections, endocrine disturbances, autoimmunity and heredity.[2]
Since its description in 1825, many procedures have been described to contain the lost volume due to gradual atrophy of soft-tissues. They include dermis-fat grafts, omental free flaps and musculoskeletal free flaps, cartilage or bone, inclusion of tantalium, acrylic and solid or liquid silicone etc.[2,3] Recently, autologous fat transfer techniques such as liposuction and liposculpture techniques of Illouz, Fournier and Otteni have been employed to increase the soft-tissue mass. A widely employed technique was proposed by Coleman.[4] His works confirmed that the reabsorption of injected fat is a dynamic process and hence would require repeated injection. This led him to describe better methods for the aspiration, processing and application of fat by use of thin cannulas, decantation, centrifugation and filtration of the lipoaspirate. Recently cell-assisted lipotransfer that uses autologous adipose tissue transplant enriched with adipose-derived stem cells has been reported.[3] Irrespective of the treatment modality, the prognosis of the treatment is fair to good. Subdermal fat grafts have been noted to have better and longer stability.[5] The source of subdermal fat is varied. It has been documented that the origin of adipocytes influence the outcome of the graft.[6]
Appearance of face exerts an emotional appeal influencing the human psyche that dictates the social interactions. Diseases such as PRS pose problems for psychosocial difficulties than their normal peers. Studies have identified that people with abnormal facial esthetics experienced adjustment problems often secondary to social difficulties. Very few studies have attempted to understand the patient's perspective with craniofacial abnormalities before and after surgical intervention.[7] In this context, this study was undertaken to estimate the qualitative perception of gluteal and abdominal subdermal fat grafting in PRS using patient interview.
MATERIALS AND METHODS
All adult (≥18 years) cases of PRS treated with subdermal fat graft with at least 1 year follow-up, post-surgically attending a tertiary maxillofacial surgical center in between 2000 and 2011 were included for the study. Besides, gender and type of subdermal grafting, this prospective study collected self-reported details of preoperative, 3 months postoperative and 1 year postoperative self-assessment of their appearance, their own perception and preference of grafts.
Surgery
Preoperative assessment of areas of atrophy was made. A choice of abdominal and gluteal fat graft was based upon the amount of fat to be transposed and the amount of fat available in donor site. The procedure was done in two stages: First to obtain the graft and second to place the graft.
First stage
After adequate preparation of the region, the graft harvesting begins with selecting an inconspicuous donor site, free of infection, scar tissue and adequate immobilizable, the graft is taken from the area near the inguinal crease. For compensating natural contraction, 25% excess in surface area is often taken for harvesting. An ellipse shaped incision is placed to close the wound in the linear fashion. For abdominal graft, the incision is usually placed along the inguinal crease, just above the pubic line while for the gluteal graft, it is around the crease. After obtaining the graft, the donor site was carefully closed in layers.
Second stage
After isolation, the dermis was removed by using Rees dermatome leaving behind the entire fat as the grafting material. Depending on the area of atrophy, incision was placed in the pre-auricular, transparotid or in the submandibular region. The superficial layers were dissected by an artery forceps. The tags of graft were then inserted in to the muscle fascial planes and secured. In the outer aspect they were stabilized using tags placed along the superficial dermis. Over correction was made by up to 30% to compensate for postoperative loss and resorption of the graft. Patients were briefed of this pitfall particularly prior to the surgery and informed consent taken [Figures 1–5].
Figure 1.

Parry Romberg syndrome-facial hemiatrophy with reduction in tissue volume on the left side cheek region
Figure 5.

(a and b) Linear scar in the fat harvested gluteal region (with staples and after removal), (c) Immediate postoperative view, (d) Postoperative view after 6 months follow-up
Figure 2.

(a and b) Harvesting of autologous gluteal region fat graft, (c) Wound closure, (d) Removal of dermis using Rees dermatome and harvested dermis free fat graft, (e and f) Insertion of the fat graft in the defect area after
Figure 3.

(a) Immediate postoperative view showing over correction to compensate for postoperative loss and resorption of graft, (b) Linear scar in graft harvested area, (c and d) Postoperative view after 1 year showing appreciative new facial profile
Figure 4.
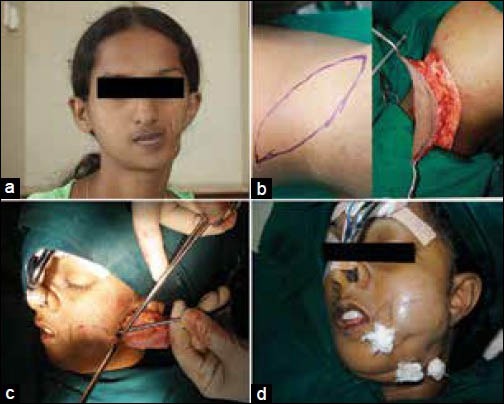
(a) Preoperative view, (b) Harvesting of gluteal region fat graft, (c) Insertion of the harvested graft in the area of defect, (d) Overcorrection of the left side facial defect
RESULT
All 36 cases of PRS were treated and included in this study. In 22 patients (61.6%) graft was obtained from the abdomen while in 14 patients (38.9%) graft was taken from gluteal region. The patients had varying degrees of the disease and atrophy. As the graft is a dynamic substitute, no accurate measurement of the graft or the survival of the graft were calculated for this study.
Of all the 17 male cases, 13 (76.47%) had fat graft isolated from the abdomen and 4 (23.53%) from the gluteal region [Figures 6–8]. In the 19 female cases, 9 (47.37%) had fat graft from the abdomen while 10 cases (52.63%) had the graft from the gluteal region [Figures 9–11]. Young aged and unmarried females and their parents, when offered a choice of the site of fat graft, preferred gluteal region than abdominal region. They were relatively uncomfortable of having a linear scar in their lower abdomen and thought that it could “potentially impede their marriage prospects.” This complaint was observed even in married women too. They related the scar to cesarean section scar and hence the apprehension.
Figure 6.

(a) Preoperative view, (b) Harvesting of the fat graft from the gluteal region, (c and d) Insertion of the fat graft after tissue dissection, (e) Postoperative view after 1 month, (f) Postoperative view after 6 months follow-up
Figure 8.

(a) Insertion of graft in the tissue defect. (b) Harvested wound closure. (c) Immediate postoperative view. (d) Postoperative view after 6 months
Figure 9.

(a) Preoperative view. (b) Harvesting of the abdominal fat graft. (c) Harvested abdominal graft. (d) Dissection through superficial tissue planes
Figure 11.

(a and b) Harvesting of the abdominal fat graft in male patient, (c) Wound closure, (d) Harvested abdominal graft
Figure 7.

(a and b) Preoperative hemiatrophied right side face, (c) Harvesting of the gluteal region fat graft (already operated scar area), (d) Dermis free fat graft
Figure 10.

(a) Insertion of fat graft in the defect area. (b) Stabilization of the graft in the outer aspect. (c) Postoperative view (1 month). (d) Postoperative view after 6 months follow-up
On the other hand, males when offered a choice of gluteal or abdomen as a potential site of graft, they were indifferent. A section of males volunteered to have the graft from the abdominal region as it could, what they perceived as the “Pseudo-tummy tuck.” Hence they had no reservation of the site of the graft.
The inherent nature of graft and surgery demanded over correction of the PRS defect. Though patient and their attendees were informed of this stage repeatedly, they were apprehensive at the immediate postoperative period, especially when the patient was weaned from drugs. The main cause of apprehension is a drastic change in their facial profile and rapidly changing the size of associated edema. Though edema was controlled using medication, repeated assurances were required, until complete dissolution of edema was achieved. Irrespective of gender and age, PRS patients were skeptical of their appearance until 8 weeks postoperatively, when stable results were showed up. A section of female patients were still concerned about a potential “loss of tissue” and “deteriorating size” of the graft. However, by the end of the third postoperative months, more than 90% of patients were comfortable with their new facial profile. Almost all patients were extremely satisfied with their new facial profile since 4 months postoperatively and believed that their facial profile is stable then on.
DISCUSSION
Patients suffering from lipoatrophy of the face have varying level of psychiatric/psychological issues emanating from the disease process.[8] In PRS, though some of the such issues may be directly linked with the disease process, most of them stem from the poor esthetic concern and self-esteem. The perception of one's own image gives the patient the much needed self-confidence and esteem. Better form and increased function after surgical intervention is success in disease such as PRS. Similar studies have been conducted among the lipoatrophied persons living with human immunodeficiency virus.[9]
For PRS, subdermal fat grafting procedure has been documented to provide the lasting result as compared with other methods.[5] Different fat grafting approaches have evolved over time for the effective rehabilitation of PRS[5] The donor site for this procedure is often the gluteal and lower abdominal region. Patients have their own reservation of the site. It is customary to overdo the thickness of the atrophied site, as the fat grafted will disintegrate and absorbed within a very short period of time. Literature sites that resorption may remain active up to a year.[10]
Immediately after surgery, the patient's general perception remained low and they appear not to be satisfied with the surgery. Both gender and site of graft did not influence the trend. In the study population context, males preferred abdominal site as it marginally reduces their girth and probably gives them a pseudosense of a “tummy tuck” effect.[11] Female PRS patients had two concerns: Most of the young, unmarried women preferred to have the gluteal incision. This probably is due to the fear of an unsightly incision in lower abdomen that mimicks a cesarean incision, a cultural taboo in this part of the world among unmarried women. As most female patients seek surgery in anticipation of marriage, these scars retard their choice to the place of incision. The married women too had their reservation for having an unsightly incision in the lower abdominal region. Hence, the acceptance of the lower abdomen as a donor site was very low and this trend is probably reflected in the present study too.
The tunneling and tugging of the fat graft in to the muscle fascia and held by small superficial dermal tag is a procedure that ensures the stay and survival of the facial fat graft. Facial musculatures have very complex movement association and hence the postoperative stability of grafts has always remained a question. Use of the tunneling and tags minimize the movement of graft in the immediate postoperative period ensuring longer dimensional stability.
It is reported that the mean gluteal adipocytes size was largest than any other region.[6] Probably this contributes to longer survival and better adaptation providing increased survival. Increased cell size and mass could help in survival of the graft in the recipient site. The survival of transplanted graft is reported to be dependent on the transferred adipocytes ability to dedifferentiate, lipogenic capacity of donor site, the presence of growth and mitogenic factors. Adipocytes from different anatomical sites are morphologically and metabolically different. The gluteal adipocytes have greater cell size and higher lipogenic activity. Facial recipient sites have shown to have smallest adipocyte size and low Adipose tissue lipoprotein lipase activity, whereas abdominal fat cells have characters in between. In the initial period after transplantation, break down of the fat tissue occur by formation of cyst-like lipid deposits that are devoured by macrophages. Cells survive this period by dedifferentiating to become immature cells. This is followed by a period of revascularization after which the immature cells turn to mature cells. As gluteal adipocytes are larger and metabolically active, they rapidly turn to immature cells and survive the change, as they are more resistant to trauma than others.[11] Hence gluteal subdermal fat graft appears to have better survival indications than other sites.
CONCLUSION
Subdermal fat grafting has been a versatile technique with better outcomes when compared with other techniques. Published evidence indicates that gluteal adipocytes are a distinct, metabolically and morphologically different group of cells that appear to have a longer viability when transferred to face. Use of tags and tunneling ensures postoperative stability of the graft. In initial preoperative period for up to 3 months, the level of acceptance scores dip, later they feel better than their pre-operative condition. This aspect of the surgery has to be forewarned to patients. Surgeons should understand the PRS patient's expectation of the outcome and also should explain the outcomes of surgery before surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Castro-Govea Y, De La Garza-Pineda O, Lara-Arias J, Chacón-Martínez H, Mecott-Rivera G, Salazar-Lozano A, et al. Cell-assisted lipotransfer for the treatment of Parry-Romberg syndrome. Arch Plast Surg. 2012;39:659–62. doi: 10.5999/aps.2012.39.6.659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Onesti MG, Monarca C, Rizzo MI, Mazzocchi M, Scuderi N. Minimally invasive combined treatment for Parry-Romberg syndrome. Aesthetic Plast Surg. 2009;33:452–6. doi: 10.1007/s00266-008-9287-7. [DOI] [PubMed] [Google Scholar]
- 3.Alencar JC, Andrade SH, Pessoa SG, Dias IS. Autologous fat transplantation for the treatment of progressive hemifacial atrophy (Parry-Romberg syndrome: Case report and review of medical literatute) An Bras Dermatol. 2011;86:S85–8. doi: 10.1590/s0365-05962011000700022. [DOI] [PubMed] [Google Scholar]
- 4.Coleman SR. Facial recontouring with lipostructure. Clin Plast Surg. 1997;24:347–67. [PubMed] [Google Scholar]
- 5.Omranifard M, Dahmerdei M, Moghadam NA, Ansari AM, Jazebi N, Otroj Z, et al. Comparison of five methods of fat grafting. J Res Med Sci. 2012;17:S108–12. [Google Scholar]
- 6.Clarkson PM, Katch FI, Kroll W, Lane R, Kamen G. Regional adipose cellularity and reliability of adipose cell size determination. Am J Clin Nutr. 1980;33:2245–52. doi: 10.1093/ajcn/33.11.2245. [DOI] [PubMed] [Google Scholar]
- 7.Marcusson A, Paulin G, Ostrup L. Facial appearance in adults who had cleft lip and palate treated in childhood. Scand J Plast Reconstr Surg Hand Surg. 2002;36:16–23. doi: 10.1080/028443102753478327. [DOI] [PubMed] [Google Scholar]
- 8.Santos CP, Felipe YX, Braga PE, Ramos D, Lima RO, Segurado AC. Self-perception of body changes in persons living with HIV/AIDS: Prevalence and associated factors. AIDS. 2005;19(Suppl 4):S14–21. doi: 10.1097/01.aids.0000191485.92285.c7. [DOI] [PubMed] [Google Scholar]
- 9.Carr A, Hudson J, Chuah J, Mallal S, Law M, Hoy J, et al. HIV protease inhibitor substitution in patients with lipodystrophy: A randomized, controlled, open-label, multicentre study. AIDS. 2001;15:1811–22. doi: 10.1097/00002030-200109280-00010. [DOI] [PubMed] [Google Scholar]
- 10.Baran CN, Celebioğlu S, Sensöz O, Ulusoy G, Civelek B, Ortak T. The behavior of fat grafts in recipient areas with enhanced vascularity. Plast Reconstr Surg. 2002;109:1646–51. doi: 10.1097/00006534-200204150-00023. [DOI] [PubMed] [Google Scholar]
- 11.Hudson DA, Lambert EV, Bloch CE. Site selection for fat autotransplantation: Some observations. Aesthetic Plast Surg. 1990;14:195–7. doi: 10.1007/BF01578349. [DOI] [PubMed] [Google Scholar]


