Abstract
Ameloblastic carcinoma (AC) is a rare primary odontogenic tumor that has histological features of both ameloblastoma and carcinoma. A total number of 92 case reports speak about its rare incidence, affecting mostly the mandible as a locally destructive lesion. The maxilla is affected even more rarely as only 35 cases have been reported until 2012 in scientific literature. The clinical course of AC is generally aggressive, with extensive local bone destruction. The most common clinical features include swelling, pain, trismus, significant bone resorption with tooth mobility, dysphonia and intraoral fistula. We report two cases of AC with aggressive behavior.
Keywords: Ameloblastoma, ameloblastic carcinoma, odontogenic carcinoma
INTRODUCTION
Ameloblastic carcinoma (AC) is characterized by malignant cytological features in combination with the overall histological pattern of ameloblastoma. The term malignant ameloblastoma is confined to those ameloblastomas that metastasize despite an apparently typical benign histology in both the primary and the metastatic lesions.[1] The incidence ratio of AC to malignant ameloblastoma is 2:1.[2]
In this article, we report two cases of AC, one involving left maxilla (primary type), which would be an addition to existing 35 cases previously reported and the other one affecting the left side of mandible arising ex ameloblastoma.
CASE REPORTS
Case 1
This paper reports a case of a 21-year-old male patient who reported to our department with the complaint of a painless, rapidly growing swelling, over the left side of mid-face since 4 months [Figure 1]. He had difficulty in chewing on the left side and three episodes of epistaxis for the last 1 month. On extraoral examination, a firm diffuse, non-tender swelling with normal overlying skin over a left side of mid face measuring 5 cm × 6 cm × 4 cm was observed. The swelling was seen extending superiorly from left infraorbital region inferiorly up to 1 cm below the commissure, medially from the philtrum region obliterating the nasolabial fold and extending laterally up to 3 cm anterior to the left ear lobule. Intraorally, a firm swelling involving left maxilla extending from distal aspect left maxillary central incisor up to the second molar region with more buccal cortical expansion, obliterating left buccal vestibule and displacing lateral incisor, canine, premolars and maxillary first molar palatally, but without any mobility was observed. All associated teeth were vital. Swelling was negative on aspiration. On neck examination, no cervical lymphadenopathy was found. Orthopantomograph showed a unilocular radiolucent lesion affecting the left maxilla displacing lateral incisor, canine, both premolars and molars [Figure 2]. The patient's vital signs were as Followes: Heart rate – 76/min, blood pressure – 126/78 mm Hg and respiratory rate – 14/min. His medical condition was not suggestive of any systemic diseases and the biochemical and hematological investigations were all within the normal limits.
Figure 1.

Preoperative photograph of case 1 showing expansile swelling over the left anterior maxilla
Figure 2.

Orthopantomograph showing a well-defined unilocular radiolucent lesion affecting left maxilla with multiple displaced teeth
On performing incisional biopsy, it was found that the outer cortical plate was lost, the growth being attached to the mucoperiosteum. The gross appearance of the specimen was slimy in character. The initial histopathology report was that of follicular variant of ameloblastoma with a, suspicion of AC.
The patient was planned for wide resection of tumor with normal margins through the modified Weber Ferguson approach under general anesthesia [Figure 3]. Resection was done with adequate margins, orbital floor was spared and proper hemostasis achieved. The surgical procedure was uneventful. The defect was closed with a surgical obturator. The resected specimen was sent for histopathologic examination [Figure 4]. The histopathological study revealed that the tumor was composed of follicles of odontogenic epithelial islands in a dense, mature connective stroma. Islands resembled dental organs with peripheral layer of ameloblast- like cells and centrally stellate reticulum-like cells. Furthermore seen was acanthomatous change (squamous metaplasia with keratin pearl formation) within the follicle, which also showed comedo necrosis [Figure 5]. These cells showed nuclear hyperchromatism, nuclear pleomorphism, increased nuclear-cytoplasmic ratio and mitotic figures or abnormal mitosis [Figure 6]. The histopathological examination also showed clear cells and fascicles of plump spindle cells merging with other cells of the follicular ameloblastomatous epithelium. This confirmed the diagnosis as AC (spindle cell variant). The patient was then referred to radiotherapy department, where he received 25 fractions of 1.8 Gy each for a period of 5 weeks (45 Gy). Post-radiation mucositis was reported.
Figure 3.

Intraoperative photograph showing the tumor involving the left maxilla exposed via modified Weber-Ferguson incision
Figure 4.

Resected tumor after sub-total maxillectomy
Figure 5.
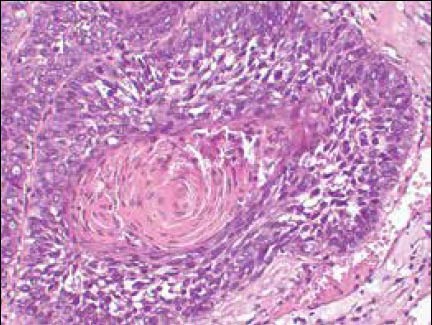
Photomicrograph showing odontogenic epithelial island with peripheral ameloblast-like cells (pre-ameloblasts) and centrally stellatereticulum like cells. Also seen is acanthomatous change (squamous metaplasia with keratin pearl formation) within the follicle, which also shows comedo necrosis (H and E, ×40 objective)
Figure 6.
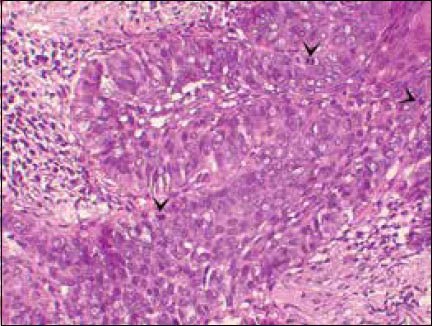
Photomicrograph showing nuclear yperchromatism and pleomorphism. Arrowheads point out mitotic figures (H and E, ×40 objective)
The patient was regularly followed-up for 1 month interval for a period of 6 months. To rule out distant metastasis, he was sent to the Department of Pulmonary Medicine and Gastroenterology of this institution, but they have cleared for any distant metastasis. Presently, after the 15 month postoperative period, there has been no recurrence at the primary site and no distant metastasis or regional lymphadenopathy has been observed. Patient is regular to his follow-up and maintaining his oral hygiene [Figure 7].
Figure 7.

Postoperative photograph after 6 months
Case 2
This was a case of a 70-year-old male patient who reported to our department with the complaint of rapidly growing painless swelling of the left side of lower jaw with difficulty in chewing, multiple mobile teeth over left side of both jaws and progressive loss of teeth for last 6 months [Figure 8]. He had the past history of a similar lesion over the left lower jaw, which was treated by en-bloc resection 20 years back. The histopathology then was suggestive of ameloblastoma.
Figure 8.

Preoperative photograph of Case 2 showing swelling over left mid and lower face
On extraoral examination, a firm diffuse non-tender swelling over left side of face extended superiorly from the left infraorbital region to the lower border of mandible inferiorly. Medially, it extended up to one-third of both upper and lower lips with an elevated angle of mouth and laterally 1 inch anterior to the angle of mandible with more medio-lateral expansion measuring about 10 cm × 8 cm × 6 cm. Neither paresthesia was associated with the swelling nor was any regional lymph node palpable. Intraoral examination revealed a painless firm proliferative growth from midline up to the left anterior border of ramus with an obliterated left side buccal sulcus and extended lingually with expansion of the lingual cortex and a medially displaced tongue [Figure 9]. The swelling was negative on aspiration. No cervical lymphadenopathy was found. Orthopantomogram showed a multilocular radiolucent lesion involving left angle and ramus of mandible with multiple areas of resorption over anterior border of ramus and maxillary alveolus distal to premolar region [Figure 10].
Figure 9.

Case 2: Intraoral view showing the swelling involving left mandibular alveolus, obliterating the vestibule with buccal cortical expansion
Figure 10.

Orthopantomograph showing multiple ill-defined radiolucencies over the angle and ramus region of left side of mandible with displaced adjacent teeth
His medical history was suggestive of Type 2 diabetes mellitus, under irregular medication. His vitals were as followes: Blood pressure – 148/96 mm Hg, heart rate – 76/min, respiratory rate – 14/min and afebrile. Fasting blood glucose (FBG) came out with 202 mg/dl. Endocrinology consultation was done and he was advised injection Human insulin 28 U in three divided doses 6/8/14 U subcutaneously. After 3 days, the FBG level reported to be 92 mg/dl. The patient was then planned for an incisional biopsy under the local anesthesia. It was suggestive of follicular variant of ameloblastoma. He was then taken up for surgical resection of the lesion with 2 cm of bony margins on the symphysis region. After hemi-mandibulectomy, the defect was reconstructed with the placement of 2.4 mm titanium reconstruction plate with condyle and surgical wound was closed primarily in layers [Figure 11]. Postoperative recovery was uneventful and the surgical wound healed well. The resected specimen was sent for histopathologic examination [Figure 12]. To our surprise, the histopathology report came out with diagnosis of AC. He was sent to radiotherapy department for further intervention, but he refused to undergo it.
Figure 11.

Operated site after the resection of tumour (hemimandibulectomy) done followed by placement of 2.4 mm titanium reconstruction plate
Figure 12.

Resected hemi-mandible with 2 cm margin
After about 8 months, the patient again turned up with a firm, tender swelling over the left side mid and lower face extending to the neck [Figure 13]. The computed tomography (CT) scan showed a hypodense image of approximately 12 cm × 16 cm size present over left side mandibular and submandibular region. He was planned for resection of tumor under general anesthesia. The submandibular incision was given and the tumor appeared firm in consistency, surrounding the reconstruction plate, it was in close approximation to the great vessels and while removing it, the left internal carotid artery got injured; the vessel was clamped and repaired with 6-0 prolene suture. The tumor was removed with normal margins along with the reconstruction plate. Hemostasis achieved and closure done in layers. The postoperative recovery was delayed, with unstable blood pressure. Patient was shifted to intensive care unit and placed on ventilator support. The next day right side hemiparesis of whole body was detected and the CT scan showed left parietal infarct. Serum urea and creatinine were also marked elevated. After 3 days, the patient died due to multiorgan failure followed by cardiorespiratory arrest.
Figure 13.

Case 2: Recurrence with marked swelling over left side lower face extending to the neck after 8 months of surgery
DISCUSSION
Odontogenic tumors are rare tumors of tooth forming apparatus involving jaw bones. In North America, between 11% and 24% of odontogenic tumors are ameloblastomas,[2] while among sub-Saharan Africans it accounts for 66-99%.[3] The tumor is frequently quoted as comprising 1% of all oral tumors among Caucasians,[4] approximately 80% are found in the mandible and 20% in the maxilla. Mostly it is asymptomatic and the symptoms appear with the expansion of the jaw. In 1955, Small and Waldron showed that 47% of maxillary ameloblastomas occur in the molar region, 33% occur in the antrum and floor of the nose, 9% occur in both the premolar and the canine regions and 2% occur in the palate.[5] There are three variants of this tumor, including the solid or multicystic variant, the unicystic variant and the peripheral variant. A review of the international literature by Reichart et al. in 1995 found the solid or multicystic variant to be the most common, comprising 92% of the 3677 cases of ameloblastoma, while the unicystic and peripheral variants accounted for 6% and 2% of the cases, respectively.[6]
AC is an extremely rare malignant odontogenic epithelial neoplasm that may arise de novo or from a pre-existing odontogenic lesion.[1,7] There are about 92 cases reported from 1984 to 2012 in scientific literature. The age of presentation ranges from 7 to 91 years. Males are more frequently affected with M:F ratio of 2.3:1. The most common site is mandible with about 56 reported cases, 35 cases in maxilla and in only one case arising from anterior skull base.[8] Posterior portion of jaw is more commonly involved. Clinically, AC causes expansion of the jaw, grows rapidly, frequently causes pain and often results in perforation of the cortex. Involvement of the nasal cavity is usually related to local invasion of the maxillary ACs. Although regional and distant metastasis is the feature of malignant ameloblastoma, but in few cases of AC, these lesions have been known to metastasize mostly to the lung or regional lymph nodes.[9] Few cases reported with metastasis to the brain, bone marrow and liver.[10,11,12,13,14] MacIntosh pointed out that the first site of reported ameloblastic metastasis was the lung and originally believed to be due to aspiration from the oral lesion rather than a true hematogenous or lymphatic spread. Indeed, enucleation and curettage surgeries might liberate neoplastic cells into the upper airway that could find their way into the lower airway.[15] Zwahlen et al. reported a case with histologically proven myocardial metastasis of a maxillary malignant ameloblastoma.[16]
The pathogenesis for malignant transformation of ameloblastoma may occur either spontaneously or because of induction following chemotherapy or post-surgical radiation.[6,17] Aggressive behavior and metastatic potential associated with ameloblastoma has been noted in two of its variants – one is the granular cell type and the other clear cell type.[18,19] Pulmonary metastasis was reported in two of the 20 granular cell ameloblastomas reviewed by Hartman.[20] Furthermore, the cases of malignant ameloblastoma reported by Tsukada et al.,[21] Hoke and Harrelson[22] were of granular cell type.
Histologically it shows features of ameloblastoma with cytologic atypia, high mitotic index, reverse polarization, peripheral palisading and necrosis, neural and vascular invasion. There are various tumors which may mimic AC histologically or clinically which includes primary intra-alveolar epidermoid carcinoma,[23] squamous cell carcinoma arising in the lining of an odontogenic cyst,[24] acanthomatous ameloblastoma and kerato-ameloblastoma,[25] squamous odontogenic tumor,[26] calcifying epithelial odontogenic tumor, salivary gland neoplasms such as pseudoadamantine adenocarcinoma, ductal carcinoma, high-grade mucoepidermiod carcinoma and metastatic carcinoma to the jaws from lung, breast and gastrointestinal tract. Yoon et al. compared the immunohistochemical markers and found that the significant expression of cytokeratin 18, parenchymal matrix metalloproteinases-2 (MMP-2), stromal MMP-9 and Ki-67 differentiated AC from ameloblastoma.[27]
The management of the AC is similar to that for ameloblastoma along with radiotherapy as reported by various authors. Literature also suggests only few case reports in which neck was addressed. The neck dissection was not performed in both the cases because no neck nodes were detected on clinical examination. Addressing no neck dissection in cases of squamous cell carcinoma is still in controversy. As our diagnosis was AC with no palpable neck nodes, we have not addressed the neck. Prior to the mid-1980s, the literature was lacking with well-documented evidence regarding the relative radioresponsiveness of the ameloblastoma. Until this point, it was believed that ameloblastoma was radioresistant. In 1984, Atkinson et al. published their review of 10 patients undergoing the delivery of megavoltage irradiation. Nine of the patients responded, three of whom underwent surgical salvage. Of the 10 patients, seven showed no evidence of disease after surgery and/or radiation therapy, with follow-up ranging from 1 to 10 years.[28] Additional evidence suggesting the value of radiation therapy in treating the ameloblastoma has been reported by Gardner.[29]
Radiotherapy and chemotherapy seem to have limited value in AC and although primary radiotherapy was expected to be useful in the cases with perineural or massive soft-tissue invasion and in positive surgical margins.[13,30] Dhir et al. reviewed 18 patients with maxillary AC. In 11 of 18, radiotherapy was used either as primary or secondary treatment in the case of metastasis and/or recurrence.[30] Jensen et al. in 2011 introduced carbon ion therapy for multiple recurring AC.[31] Horváth et al. reported a case of mandibular AC with pleura-pulmonary and bone marrow metastasis in a 8-year-old girl. They prescribed five cycles of chemotherapy with vincristine, endoxane, adriamycin, carboplatin and etoposide. It resulted in tumor shrinkage but no significant effect upon pulmonary site and the patient died after 8 months.[32] Hence, the role of chemotherapy is still unpredictable. 77
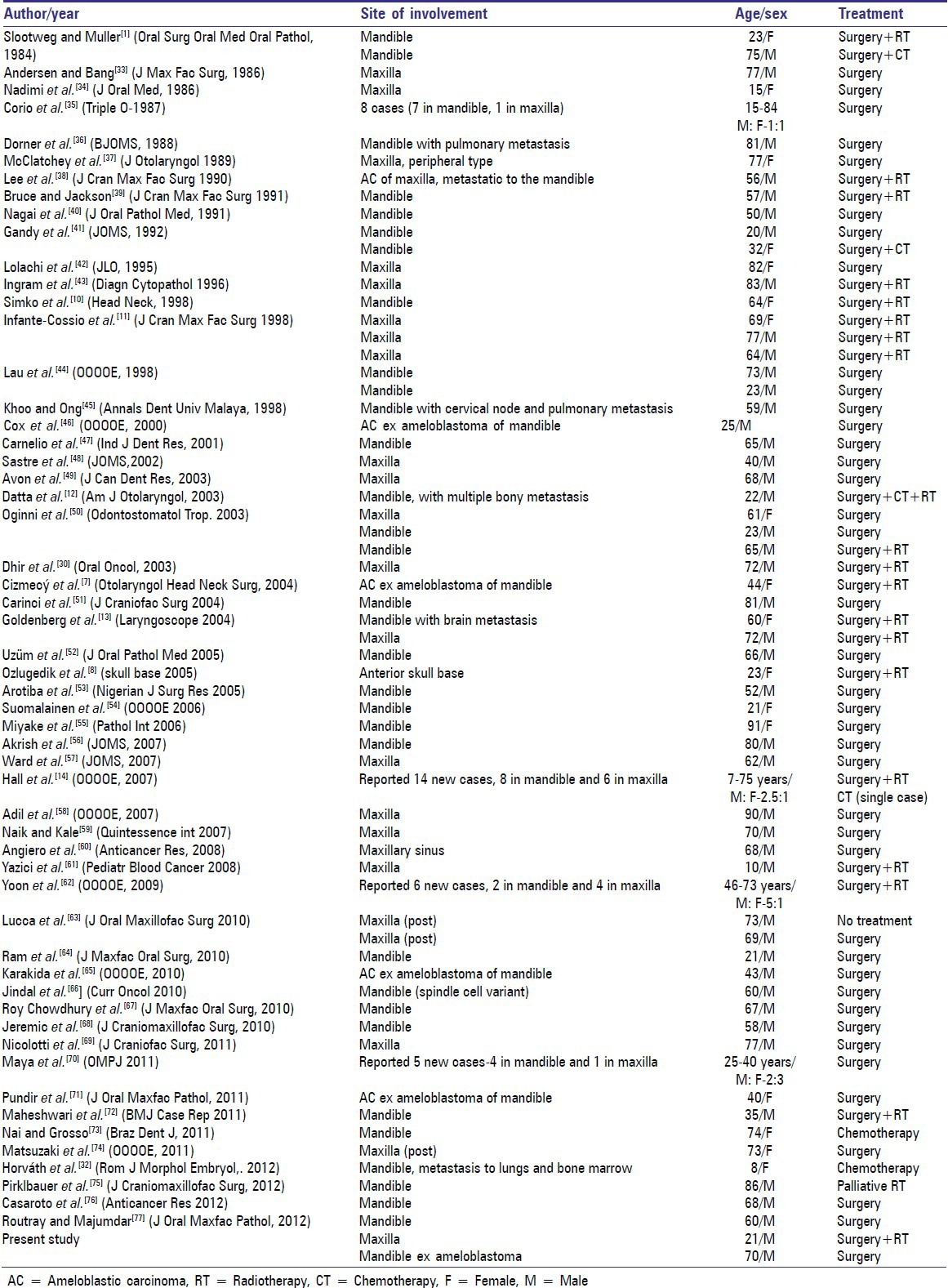
Survival rate depends upon local recurrence, regional or distant metastasis. Infante-Cossio et al. reported a maximum 5 years of follow-up in two patients with no evidence of local recurrence, regional or distant metastasis. Third patient showed local recurrence and he died after few months of it. Hence, after surgery and radiotherapy, 5 years of survival rate can be accepted as a standard if no recurrence or metastasis occurs.[11] Case reports of AC affecting both the jaws, which have been published at the time of writing this article, have been listed in Table 1.
Table 1.
Total review of literature of AC from 1984 to 2012
CONCLUSION
Based on the above study although, ameloblastoma is a slowly growing, locally aggressive tumor. Any change in its growth pattern should cause suspicion of malignancy. AC is likely to metastasize. Therefore, complete history and general systemic examination are required to rule out any distant metastasis. Radiotherapy has definite role in cure of AC as in our cases; recurrence was seen in the patient who refused to undergo it.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Slootweg PJ, Müller H. Malignant ameloblastoma or ameloblastic carcinoma. Oral Surg Oral Med Oral Pathol. 1984;57:168–76. doi: 10.1016/0030-4220(84)90207-x. [DOI] [PubMed] [Google Scholar]
- 2.Regezi JA, Kerr DA, Courtney RM. Odontogenic tumors: Analysis of 706 cases. J Oral Surg. 1978;36:771–8. [PubMed] [Google Scholar]
- 3.Mosadomi A. Odontogenic tumors in an African population. Analysis of twenty-nine cases seen over a 5-year period. Oral Surg Oral Med Oral Pathol. 1975;40:502–21. doi: 10.1016/0030-4220(75)90248-0. [DOI] [PubMed] [Google Scholar]
- 4.Arotiba JT, Ogunbiyi JO, Obiechina AE. Odontogenic tumours: A 15-year review from Ibadan, Nigeria. Br J Oral Maxillofac Surg. 1997;35:363–7. doi: 10.1016/s0266-4356(97)90411-3. [DOI] [PubMed] [Google Scholar]
- 5.Small IA, Waldron CA. Ameloblastomas of the jaws. Oral Surg Oral Med Oral Pathol. 1955;8:281–97. doi: 10.1016/0030-4220(55)90350-9. [DOI] [PubMed] [Google Scholar]
- 6.Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: Biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995;31B:86–99. doi: 10.1016/0964-1955(94)00037-5. [DOI] [PubMed] [Google Scholar]
- 7.Cizmecý O, Aslan A, Onel D, Demiryont M. Ameloblastic carcinoma ex ameloblastoma of the mandible: Case report. Otolaryngol Head Neck Surg. 2004;130:633–4. doi: 10.1016/j.otohns.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 8.Ozlugedik S, Ozcan M, Basturk O, Deren O, Kaptanoglu E, Adanali G, et al. Ameloblastic carcinoma arising from anterior skull base. Skull Base. 2005;15:269–72. doi: 10.1055/s-2005-918621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eversole LR. Malignant epithelial odontogenic tumors. Semin Diagn Pathol. 1999;16:317–24. [PubMed] [Google Scholar]
- 10.Simko EJ, Brannon RB, Eibling DE. Ameloblastic carcinoma of the mandible. Head Neck. 1998;20:654–9. doi: 10.1002/(sici)1097-0347(199810)20:7<654::aid-hed14>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 11.Infante-Cossio P, Hernandez-Guisado JM, Fernandez-Machin P, Garcia-Perla A, Rollon-Mayordomo A, Gutierrez-Perez JL. Ameloblastic carcinoma of the maxilla: A report of 3 cases. J Craniomaxillofac Surg. 1998;26:159–62. doi: 10.1016/s1010-5182(98)80006-1. [DOI] [PubMed] [Google Scholar]
- 12.Datta R, Winston JS, Diaz-Reyes G, Loree TR, Myers L, Kuriakose MA, et al. Ameloblastic carcinoma: Report of an aggressive case with multiple bony metastases. Am J Otolaryngol. 2003;24:64–9. doi: 10.1053/ajot.2003.15. [DOI] [PubMed] [Google Scholar]
- 13.Goldenberg D, Sciubba J, Koch W, Tufano RP. Malignant odontogenic tumors: A 22-year experience. Laryngoscope. 2004;114:1770–4. doi: 10.1097/00005537-200410000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Hall JM, Weathers DR, Unni KK. Ameloblastic carcinoma: An analysis of 14 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:799–807. doi: 10.1016/j.tripleo.2006.11.048. [DOI] [PubMed] [Google Scholar]
- 15.MacIntosh RB. Aggressive management of ameloblastoma. Oral Maxillofac Surg Clin North Am. 1991;3:73. [Google Scholar]
- 16.Zwahlen RA, Vogt P, Fischer FS, Grätz KW. Case report: Myocardial metastasis of a maxillary malignant ameloblastoma. J Oral Maxillofac Surg. 2003;61:731–4. doi: 10.1053/joms.2003.50146. [DOI] [PubMed] [Google Scholar]
- 17.Gardner DG. Some current concepts on the pathology of ameloblastomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:660–9. doi: 10.1016/s1079-2104(96)80441-0. [DOI] [PubMed] [Google Scholar]
- 18.Hansen LS, Eversole LR, Green TL, Powell NB. Clear cell odontogenic tumor – A new histologic variant with aggressive potential. Head Neck Surg. 1985;8:115–23. doi: 10.1002/hed.2890080208. [DOI] [PubMed] [Google Scholar]
- 19.Waldron CA, Small IA, Silverman H. Clear cell ameloblastoma - An odontogenic carcinoma. J Oral Maxillofac Surg. 1985;43:707–17. doi: 10.1016/0278-2391(85)90198-3. [DOI] [PubMed] [Google Scholar]
- 20.Hartman KS. Granular-cell ameloblastoma. Oral Surg Oral Med Oral Pathol. 1974;38:241–53. doi: 10.1016/0030-4220(74)90063-2. [DOI] [PubMed] [Google Scholar]
- 21.Tsukada Y, Delapava S, Pickren JW. Granular-cell ameloblastoma with metastasis to the lungs: Report of a case and review of the literature. Cancer. 1965;18:916–25. doi: 10.1002/1097-0142(196507)18:7<916::aid-cncr2820180722>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 22.Hoke HF, Jr, Harrelson AB. Granular cell ameloblastoma with metastasis to the cervical vertebrae. Observations on the origin of the granular cells. Cancer. 1967;20:991–9. doi: 10.1002/1097-0142(196706)20:6<991::aid-cncr2820200609>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 23.Shear M. Primary intra-alveolar epidermoid carcinoma of the jaw. J Pathol. 1969;97:645–51. doi: 10.1002/path.1710970409. [DOI] [PubMed] [Google Scholar]
- 24.Gardner AF. The odontogenic cyst as a potential carcinoma: A clinicopathologic appraisal. J Am Dent Assoc. 1969;78:746–55. doi: 10.14219/jada.archive.1969.0290. [DOI] [PubMed] [Google Scholar]
- 25.Pindborg JJ. Copenhagen: Munksgaard; 1970. Pathology of the Dental Hard Tissues; pp. 371–7. [Google Scholar]
- 26.Pullon PA, Shafer WG, Elzay RP, Kerr DA, Corio RL. Squamous odontogenic tumor. Report of six cases of a previously undescribed lesion. Oral Surg Oral Med Oral Pathol. 1975;40:616–30. doi: 10.1016/0030-4220(75)90372-2. [DOI] [PubMed] [Google Scholar]
- 27.Yoon HJ, Jo BC, Shin WJ, Cho YA, Lee JI, Hong SP, et al. Comparative immunohistochemical study of ameloblastoma and ameloblastic carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:767–76. doi: 10.1016/j.tripleo.2011.06.036. [DOI] [PubMed] [Google Scholar]
- 28.Atkinson CH, Harwood AR, Cummings BJ. Ameloblastoma of the jaw. A reappraisal of the role of megavoltage irradiation. Cancer. 1984;53:869–73. doi: 10.1002/1097-0142(19840215)53:4<869::aid-cncr2820530409>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 29.Gardner DG. Radiotherapy in the treatment of ameloblastoma. Int J Oral Maxillofac Surg. 1988;17:201–5. doi: 10.1016/s0901-5027(88)80033-x. [DOI] [PubMed] [Google Scholar]
- 30.Dhir K, Sciubba J, Tufano RP. Ameloblastic carcinoma of the maxilla. Oral Oncol. 2003;39:736–41. doi: 10.1016/s1368-8375(03)00036-8. [DOI] [PubMed] [Google Scholar]
- 31.Jensen AD, Ecker S, Ellerbrock M, Nikoghosyan A, Debus J, Münter MW. Carbon ion therapy for ameloblastic carcinoma. Radiat Oncol. 2011;6:13. doi: 10.1186/1748-717X-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Horváth A, Horváth E, Popşor S. Mandibular ameloblastic carcinoma in a young patient. Rom J Morphol Embryol. 2012;53:179–83. [PubMed] [Google Scholar]
- 33.Andersen E, Bang G. Ameloblastic carcinoma of the maxilla. A case report. J Maxillofac Surg. 1986;14:338–40. doi: 10.1016/s0301-0503(86)80320-4. [DOI] [PubMed] [Google Scholar]
- 34.Nadimi H, Toto PD, Jaffe E, McReynolds HD. Basement membrane defect in ameloblastic carcinoma: A case study. J Oral Med. 1986;41:79–81. [PubMed] [Google Scholar]
- 35.Corio RL, Goldblatt LI, Edwards PA, Hartman KS. Ameloblastic carcinoma: A clinicopathologic study and assessment of eight cases. Oral Surg Oral Med Oral Pathol. 1987;64:570–6. doi: 10.1016/0030-4220(87)90063-6. [DOI] [PubMed] [Google Scholar]
- 36.Dorner L, Sear AJ, Smith GT. A case of ameloblastic carcinoma with pulmonary metastases. Br J Oral Maxillofac Surg. 1988;26:503–10. doi: 10.1016/0266-4356(88)90073-3. [DOI] [PubMed] [Google Scholar]
- 37.McClatchey KD, Sullivan MJ, Paugh DR. Peripheral ameloblastic carcinoma: A case report of a rare neoplasm. J Otolaryngol. 1989;18:109–11. [PubMed] [Google Scholar]
- 38.Lee L, Maxymiw WG, Wood RE. Ameloblastic carcinoma of the maxilla metastatic to the mandible. Case report. J Craniomaxillofac Surg. 1990;18:247–50. doi: 10.1016/s1010-5182(05)80424-x. [DOI] [PubMed] [Google Scholar]
- 39.Bruce RA, Jackson IT. Ameloblastic carcinoma. Report of an aggressive case and review of the literature. J Craniomaxillofac Surg. 1991;19:267–71. doi: 10.1016/s1010-5182(05)80068-x. [DOI] [PubMed] [Google Scholar]
- 40.Nagai N, Takeshita N, Nagatsuka H, Inoue M, Nishijima K, Nojima T, et al. Ameloblastic carcinoma: Case report and review. J Oral Pathol Med. 1991;20:460–3. doi: 10.1111/j.1600-0714.1991.tb00439.x. [DOI] [PubMed] [Google Scholar]
- 41.Gandy SR, Keller EE, Unni KK. Ameloblastic carcinoma: Report of two cases. J Oral Maxillofac Surg. 1992;50:1097–102. doi: 10.1016/0278-2391(92)90499-p. [DOI] [PubMed] [Google Scholar]
- 42.Lolachi CM, Madan SK, Jacobs JR. Ameloblastic carcinoma of the maxilla. J Laryngol Otol. 1995;109:1019–22. doi: 10.1017/s0022215100131925. [DOI] [PubMed] [Google Scholar]
- 43.Ingram EA, Evans ML, Zitsch RP., 3rd Fine-needle aspiration cytology of ameloblastic carcinoma of the maxilla: A rare tumor. Diagn Cytopathol. 1996;14:249–52. doi: 10.1002/(SICI)1097-0339(199604)14:3<249::AID-DC10>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 44.Lau SK, Tideman H, Wu PC. Ameloblastic carcinoma of the jaws. A report of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:78–81. doi: 10.1016/s1079-2104(98)90402-4. [DOI] [PubMed] [Google Scholar]
- 45.Khoo SP, Ong ST. Ameloblastic carcinoma: A case with cervical node and pulmonary metastases. Ann Dent Univ Malaya. 1998;5:49–52. [Google Scholar]
- 46.Cox DP, Muller S, Carlson GW, Murray D. Ameloblastic carcinoma ex ameloblastoma of the mandible with malignancy-associated hypercalcemia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:716–22. doi: 10.1067/moe.2000.109076. [DOI] [PubMed] [Google Scholar]
- 47.Carnelio S, Solomon M, Manohar V. Ameloblastic carcinoma. A case report with review of literature. Indian J Dent Res. 2001;12:238–41. [PubMed] [Google Scholar]
- 48.Sastre J, Muñoz M, Naval L, Adrados M. Ameloblastic carcinoma of the maxilla: Report of a case. J Oral Maxillofac Surg. 2002;60:102–4. doi: 10.1053/joms.2002.29086. [DOI] [PubMed] [Google Scholar]
- 49.Avon SL, McComb J, Clokie C. Ameloblastic carcinoma: Case report and literature review. J Can Dent Assoc. 2003;69:573–6. [PubMed] [Google Scholar]
- 50.Oginni FO, Ugboko VI, Owotade JF, Adebiyi KE. Ameloblastic carcinoma of the jaws. A report of three Nigerian cases. Odontostomatol Trop. 2003;26:19–22. [PubMed] [Google Scholar]
- 51.Carinci F, Palmieri A, Delaiti G, Rubini C, Fioroni M, Martinelli M, et al. Expression profiling of ameloblastic carcinoma. J Craniofac Surg. 2004;15:264–9. doi: 10.1097/00001665-200403000-00022. [DOI] [PubMed] [Google Scholar]
- 52.Uzüm N, Akyol G, Asal K, Köybaşioğlu A. Ameloblastic carcinoma containing melanocyte and melanin pigment in the mandible: A case report and review of the literature. J Oral Pathol Med. 2005;34:618–20. doi: 10.1111/j.1600-0714.2005.00306.x. [DOI] [PubMed] [Google Scholar]
- 53.Arotiba JT, Mohammed AZ, Adebola RA, Adeola DS, Ajike SO, Rafindadi AH. Ameloblastic carcinoma: report of a case. Niger J Surg Res. 2005;7:222–5. [Google Scholar]
- 54.Suomalainen A, Hietanen J, Robinson S, Peltola JS. Ameloblastic carcinoma of the mandible resembling odontogenic cyst in a panoramic radiograph. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:638–42. doi: 10.1016/j.tripleo.2005.07.033. [DOI] [PubMed] [Google Scholar]
- 55.Miyake T, Tanaka Y, Kato K, Tanaka M, Sato Y, Ijiri R, et al. Gene mutation analysis and immunohistochemical study of beta-catenin in odontogenic tumors. Pathol Int. 2006;56:732–7. doi: 10.1111/j.1440-1827.2006.02039.x. [DOI] [PubMed] [Google Scholar]
- 56.Akrish S, Buchner A, Shoshani Y, Vered M, Dayan D. Ameloblastic carcinoma: Report of a new case, literature review, and comparison to ameloblastoma. J Oral Maxillofac Surg. 2007;65:777–83. doi: 10.1016/j.joms.2005.11.116. [DOI] [PubMed] [Google Scholar]
- 57.Ward BB, Edlund S, Sciubba J, Helman JI. Ameloblastic carcinoma (primary type) isolated to the anterior maxilla: Case report with review of the literature. J Oral Maxillofac Surg. 2007;65:1800–3. doi: 10.1016/j.joms.2006.06.265. [DOI] [PubMed] [Google Scholar]
- 58.Benlyazid A, Lacroix-Triki M, Aziza R, Gomez-Brouchet A, Guichard M, Sarini J. Ameloblastic carcinoma of the maxilla: Case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e17–24. doi: 10.1016/j.tripleo.2007.05.026. [DOI] [PubMed] [Google Scholar]
- 59.Naik V, Kale AD. Ameloblastic carcinoma: A case report. Quintessence Int. 2007;38:873–9. [PubMed] [Google Scholar]
- 60.Angiero F, Borloni R, Macchi M, Stefani M. Ameloblastic carcinoma of the maxillary sinus. Anticancer Res. 2008;28:3847–54. [PubMed] [Google Scholar]
- 61.Yazici N, Karagöz B, Varan A, Yilmaz T, Oztürk A, Usubütün A, et al. Maxillary ameloblastic carcinoma in a child. Pediatr Blood Cancer. 2008;50:175–6. doi: 10.1002/pbc.20889. [DOI] [PubMed] [Google Scholar]
- 62.Yoon HJ, Hong SP, Lee JI, Lee SS, Hong SD. Ameloblastic carcinoma: An analysis of 6 cases with review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:904–13. doi: 10.1016/j.tripleo.2009.06.045. [DOI] [PubMed] [Google Scholar]
- 63.Lucca M, D’Innocenzo R, Kraus JA, Gagari E, Hall J, Shastri K. Ameloblastic carcinoma of the maxilla: A report of 2 cases. J Oral Maxillofac Surg. 2010;68:2564–9. doi: 10.1016/j.joms.2009.09.088. [DOI] [PubMed] [Google Scholar]
- 64.Ram H, Mohammad S, Husain N, Gupta PN. Ameloblastic carcinoma. J Maxillofac Oral Surg. 2010;9:415–9. doi: 10.1007/s12663-010-0169-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Karakida K, Aoki T, Sakamoto H, Takahashi M, Akamatsu T, Ogura G, et al. Ameloblastic carcinoma, secondary type: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e33–7. doi: 10.1016/j.tripleo.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 66.Jindal C, Palaskar S, Kaur H, Shankari M. Low-grade spindle-cell ameloblastic carcinoma: Report of an unusual case with immunohistochemical findings and review of the literature. Curr Oncol. 2010;17:52–7. doi: 10.3747/co.v17i5.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roy Chowdhury SK, Ramen S, Chattopadhyay PK, Moorchung N, Rajkumar K. Ameloblastic Carcinoma of the mandible. J Maxillofac Oral Surg. 2010;9:198–201. doi: 10.1007/s12663-010-0051-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jeremic JV, Nikolic ZS, Boricic IV, Tacevic ZD, Tomanovic NR, Drcic LJ, et al. Total mandibular reconstruction after resection of rare “honeycomb-like” ameloblastic carcinoma – A case report. J Craniomaxillofac Surg. 2010;38:465–8. doi: 10.1016/j.jcms.2009.10.020. [DOI] [PubMed] [Google Scholar]
- 69.Nicolotti M, Brucoli M, Arcuri F, Benech A. Ameloblastic carcinoma: Rare localization of a rare neoplasm. J Craniofac Surg. 2011;22:2353–5. doi: 10.1097/SCS.0b013e318231e49b. [DOI] [PubMed] [Google Scholar]
- 70.Maya R, Sekar B, Murali S, Mathew S, Chacko J, Paul G. Ameloblastic carcinoma-Review and histopathology of 5 cases. Oral Maxillofac Pathol J. 2011;2:154–60. [Google Scholar]
- 71.Pundir S, Saxena S, Rathod V, Aggrawal P. Ameloblastic carcinoma: Secondary dedifferentiated carcinoma of the mandible: Report of a rare entity with a brief review. J Oral Maxillofac Pathol. 2011;15:201–4. doi: 10.4103/0973-029X.84501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Maheshwari V, Varshney M, Alam K, Jain A, Siddiqui MA, Gaur K, et al. Ameloblastic carcinoma: a rare entity. BMJ Case Reports. 2011:1–5. doi: 10.1136/bcr.01.2011.3678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nai GA, Grosso RN. Fine-needle aspiration biopsy of ameloblastic carcinoma of the mandible: A case report. Braz Dent J. 2011;22:254–7. doi: 10.1590/s0103-64402011000300013. [DOI] [PubMed] [Google Scholar]
- 74.Matsuzaki H, Katase N, Hara M, Asaumi J, Yanagi Y, Unetsubo T, et al. Ameloblastic carcinoma: A case report with radiological features of computed tomography and magnetic resonance imaging and positron emission tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:e40–7. doi: 10.1016/j.tripleo.2011.01.023. [DOI] [PubMed] [Google Scholar]
- 75.Pirklbauer K, Kozakowski N, Russmueller G, Ewers R, Klug C. Manifestation of an ameloblastic carcinoma ten years after follicular cyst enucleation in the mandibular ramus. J Craniomaxillofac Surg. 2012;40:362–5. doi: 10.1016/j.jcms.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 76.Casaroto AR, Toledo GL, Filho JL, Soares CT, Capelari MM, Lara VS. Ameloblastic carcinoma, primary type: Case report, immunohistochemical analysis and literature review. Anticancer Res. 2012;32:1515–25. [PubMed] [Google Scholar]
- 77.Routray S, Majumdar S. Ameloblastic carcinoma: Sometimes a challenge. J Oral Maxillofac Pathol. 2012;16:156–8. doi: 10.4103/0973-029X.92998. [DOI] [PMC free article] [PubMed] [Google Scholar]


