G&H How do the tissue adhesives currently being used for therapeutic endoscopy work?
YB Currently, there are 2 categories of tissue adhesives: fibrin glue and cyanoacrylates. Fibrin glue is a combination of thrombin and fibrinogen that, when injected together, forms a tissue plug that can be used in the gastrointestinal (GI) tract. The chemical cyanoacrylate was originally developed by Kodak and is now available in various formulations. Cyanoacrylates are injected as liquids and solidify into “superglue” on contact with water or blood. Both fibrin glue and cyanoacrylates are commercially available in the United States for medical use; however, they are not approved by the US Food and Drug Administration for injection into blood vessels or the GI tract. Although there is a fair amount of experience with these tissue adhesives in GI endoscopy, both in the United States and internationally, this use is technically off-label. Therefore, an institutional investigational device exemption might be required prior to such use, particularly in the case of cyanoacrylates.
G&H What are the specific indications for the use of these agents?
YB Cyanoacrylates have primarily been used in the treatment of bleeding from gastric varices with excellent results. They also have been used to treat bleeding esophageal varices that are refractory to standard endo-scopic treatment (such as banding and sclerosants). Cya-noacrylates have been used in a few cases of nonvariceal bleeding (eg, following endoscopic mucosal resection) with variable success. Finally, they can be used as rescue therapy for leaks from the bile or pancreatic duct when standard endoscopic therapy, such as stenting, has failed.
G&H How do these tissue adhesives compare with more traditional treatments, such as banding, clipping, thermal ablation, and epinephrine injection?
YB It depends on the specific indication. For treatment of gastric varices, banding and epinephrine or sclerosant injection are not effective. In this setting, cyanoacrylate injection is very effective and is definitely better than the other available endoscopic options.
G&H Are there any safety concerns associated with the use of cyanoacrylates and fibrin glue?
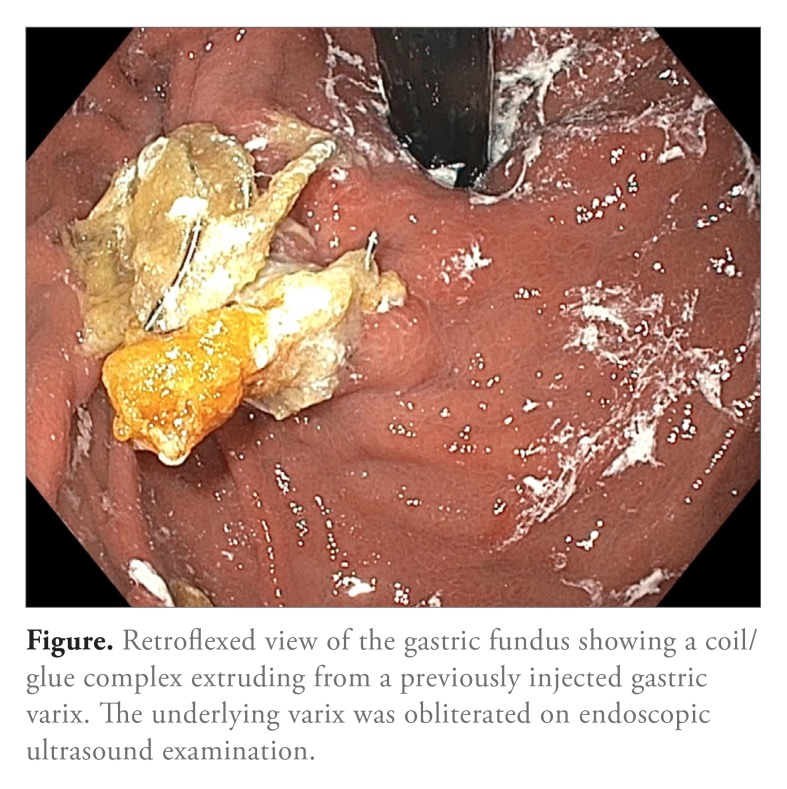
YB For cyanoacrylates, the most significant concern is the risk of embolization with intervascular injection. The injected liquid solidifies in approximately 30 seconds to 2 minutes, depending on the type of cyanoacrylate used. If injected too rapidly, the glue might embolize from the intended site of treatment into the pulmonary or systemic circulation, possibly resulting in portal or splenic vein thrombosis, pulmonary embolism, or stroke. To minimize this risk, a coil can be inserted into the gastric varix under endoscopic ultrasound guidance prior to injecting the cyanoacrylate. The coil acts as a scaffold to hold the cyanoacrylate plug in place and prevent migration. There are some preliminary data that suggest that this might be a good strategy (Figure); however, more studies are needed to make a definitive conclusion. Transient fever or mild pain is common after injection, and patients receive antibiotics pre- and posttreatment (3 days) in our practice.
G&H Do cyanoacrylates and fibrin glue have the potential to clog up the instrument channels of endoscopes, resulting in the need for repair or replacement?
YB Because cyanoacrylates solidify rapidly, the injecting catheter or device should be outside of the endoscope during delivery. Inadvertent injection within the working channel of the endoscope will result in high-grade blockage and require the endoscope to be sent out for repair. It is usually not possible to flush or push the plug out with a cleaning brush. This is a very important consideration. Some physicians pretreat the working channel of their endoscope with silicon to decrease this risk.
G&H How difficult are the tissue adhesives to administer?
YB There are 2 components to answering this question. The first involves the technical difficulty of what and where to inject. For example, gastric varices might be more challenging to inject than esophageal varices and are better treated under endoscopic ultrasound guidance in my opinion. Also, the physician needs some experience with the injection technique, the best endoscope position, and so on. The second component is the preparation that goes into injecting either of the tissue adhesives. For example, cyanoacrylates are available in 0.5-mL ampoules and require aspiration of multiple ampoules into a syringe prior to injection—this can take time and requires training the assisting nurse. It is also important to be careful about the injection itself, which has to be done slowly, in a drop-by-drop or drip-it-in manner, rather than a rapid flush into the blood vessel.
G&H How much does it cost to use these tissue adhesives, particularly compared with more traditional treatments?
YB Fortunately, tissue adhesives are fairly cost-effective. An ampoule containing 0.5 mL of cyanoacrylate usually costs anywhere between $25 and $30. Accounting for multiple ampoules and the cost of the injecting needle, the total cost is very comparable to that of banding or thermal ablation.
G&H Are there any new tissue adhesives on the horizon?
YB There is a new product, HemoSpray (Cook Medical), which was developed by the military for use in the battlefield. This compound can be sprayed onto a bleeding vessel, creating immediate closure. HemoSpray has been used in a few places overseas, but it has not yet been validated in the United States. (Only a few cases have been published.) At this point, there is not enough information available to recommend it or not.
On the other hand, fibrin glue is usually utilized for closure of GI fistulae, as the fibrin plug can be injected endo-scopically into the fistula tract. This is performed in conjunction with other endoscopic therapy (fistula ablation, stent placement, or endoscopic suturing) as multimodality therapy for the best results. There have also been attempts to use fibrin glue in certain cases of GI bleeding, particularly ulcer bleeding, although this has been done more often in Europe than the United States. However, results have been mixed.
However, for other types of GI bleeding, including esophageal varices and nonvariceal bleeding, traditional therapies, such as banding, clipping, ablation, and epinephrine, would be the first line of treatment, as they are usually effective. Cyanoacrylate and fibrin glue injections would be used only as rescue therapy or last-line therapy in these settings.
For treating fistulae, certain leaks in the bile or pancreatic duct that do not respond to standard treatment could be treated with cyanoacrylates. Fibrin glue is used in combination with clips, thermal ablation, suturing, and so on in this setting. There are no good comparative studies looking at the efficacy of individual treatment modalities, but my experience has been that, if used alone, fibrin glue is inadequate for sealing fistulae.
If a cyanoacrylate is injected for a leak in the bile or pancreatic duct, the physician should be very careful not to overinject and block off” the duct itself; only the fistula/leak site should be injected, and a prophylactic stent should be placed after injection.
Fibrin glue is used mainly in fistulae and is generally well tolerated. There are small risks of anaphylaxis and allergic reactions or coagulopathy due to antibody formation to the fibrinogen or thrombin components. However, these risks were more significant in the past when bovine thrombin was used; conversion to human-derived components has mitigated these issues.
Another precaution that can be taken to protect the instrument is to avoid pulling the needle back out immediately through the endoscope after injecting the blood vessel. Instead, the entire endoscope should be completely removed, and the tip of the needle should be cleaned with alcohol before removing it from the endoscope.
Fibrin glue can also cause blockage of the working channel of the endoscope that might require repair. A fibrin plug can form within the working channel if the 2 components are not delivered properly (through a double-lumen catheter) and end up aggregating before they exit the endoscope (ie, the fibrinogen and thrombin meet in the channel of the endoscope). This risk is not as large as with cyanoacrylates, but it certainly should be taken into consideration.
As for the fibrin glue, the fibrinogen and thrombin components must first be thawed and then warmed up, usually with a small heating device, which can take up to 10 minutes. A double-lumen catheter is usually used so that the 2 components are separate but delivered concurrently; this way, they aggregate only at the distal end of the catheter.
Figure.
Retroflexed view of the gastric fundus showing a coil/glue complex extruding from a previously injected gastric varix. The underlying varix was obliterated on endoscopic ultrasound examination.
Footnotes
Dr Bhat has no relevant conflicts of interest to disclose.
Suggested Reading
- ASGE Technology Committee; Bhat YM, Banerjee S, Barth BA, et al. Tissue adhesives: cyanoacrylate glue and fibrin sealant. Gastrointest Endosc. 2013;78(2):209–215. doi: 10.1016/j.gie.2013.04.166. [DOI] [PubMed] [Google Scholar]
- Binmoeller KF, Weilert F, Shah JN, Kim J. EUS-guided transesophageal treatment of gastric fundal varices with combined coiling and cyanoacrylate glue injection (with videos) Gastrointest Endosc. 2011;74(5):1019–1025. doi: 10.1016/j.gie.2011.06.030. [DOI] [PubMed] [Google Scholar]
- Park W, Yeh R, Triadafilopoulous G. Injection therapies for variceal bleeding disorders of the GI tract. Gastrointest Endosc. 2008;67(2):313–323. doi: 10.1016/j.gie.2007.09.052. [DOI] [PubMed] [Google Scholar]
- Procaccini N, Al-Osaimi A, Northup P, et al. Endoscopic cyanoacrylate versus transjugular intrahepatic portosystemic shunt for gastric variceal bleeding: a single- center US. analysis. Gastrointest Endosc. 2009;70(5):881–887. doi: 10.1016/j.gie.2009.03.1169. [DOI] [PubMed] [Google Scholar]
- Sarin SK, Jain AK, Jain M, Gupta R. A randomized controlled trial of cyanoacry-late versus alcohol injection in patients with isolated fundic varices. Am J Gastro-enterol. 2002;97(4):1010–1015. doi: 10.1111/j.1572-0241.2002.05622.x. [DOI] [PubMed] [Google Scholar]
- Seewald S, Sriram PV, Nagra M, et al. The expert approach: cyanoacrylate glue in gastric variceal bleeding. Endoscopy. 2002;34(11):926–932. doi: 10.1055/s-2002-35312. [DOI] [PubMed] [Google Scholar]