Abstract
Background:
Ultrasound examination is very frequently used for the evaluation of abnormalities in various organs of the body. Our aim was to determine whether the requests by family physicians (FPs) for ultrasound examinations were appropriate. Our secondary objective was to enumerate positive and negative ultrasound reports for various diagnostic indications.
Materials and Methods:
This cross-sectional study was conducted during the period of month between June and August 2010, at the Family Medicine Department of North West Armed Forces Prince Salman Hospital, Tabuk. We reviewed the ultrasound requests of all patients included in this study and the findings of the procedure. Data were analyzed using the Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL), version 16.0.
Results:
The requests and reports of 815 patients for ultrasound were reviewed. Females comprised 58.7% of the referred cases. The mean age of the sample at referral was 30 ± 18.5 for females and 34 ± 20.7 for males. Only 46% of the request forms contained conclusive information and instructions. Abdominal/pelvic ultrasounds were the most frequently requested; Nearly 71.2% of the ultrasound scans were normal. Abdominal/pelvis ultrasound was more likely to be reported as normal than ultrasound scans of other regions (P = 0.007). Patients aged 41-60 years were more likely to have an abnormal ultrasound (P = 0.02).
Conclusion:
Our findings suggest that FPs have to be educated about imaging referral protocols in order to achieve better outcomes.
Keywords: Diagnosis, family practice, indications, requests, ultrasound
INTRODUCTION
Ultrasound examinations are used for the screening and diagnosis of occult diseases or in cases where physicians need to confirm a diagnosis. Ultrasound examinations are also frequently used in physical therapy where they can be of prognostic value. They are also often used to reassure or alleviate patient anxiety.
Ultrasound has broad applications in family medicine, including its use for the evaluation of abnormalities in various superficial and deep organs of the body. Common indications for ultrasound use include chronic abdominal pain, palpable masses, flank pain, hematuria, scrotal swelling, and irregular menstrual cycles. It is a relatively inexpensive, safe noninvasive diagnostic tool.
At present, many radiology departments do not only perform ultrasound examinations after physician request, they also provide direct access to ultrasound services. Some studies show that over 40% of diagnostic radiology examinations may be unnecessary,[1,2] including the “questionable” use of ultrasound.[2] The factors that contribute to the rise in the volume of imaging services include more availability and accessibility, increased demand by patients and physicians, favorable reimbursement, and improvement in the quality of imaging techniques.[3] Besides the cost, excessive imaging may lead to additional diagnostic tests and over-treatment of benign incidental findings.[4]
In 1990, the Royal College of Radiologists released guidelines for radiologic referral, and several studies showed that the application of these guidelines can lead to a considerable decrease in the frequency of inappropriate ultrasound requests.[5,6,7] Unfortunately, in a survey that investigated the use of the American College of Radiology (ACR) appropriateness criteria, it was found that only 2% of the specialist physicians and residents reported following the ACR's appropriateness criteria when ordering imaging scans.[8] Furthermore, retrospective studies[9,10,11] showed that among other imaging modalities, the proportion of inappropriate requests was higher for ultrasound scans. In one study,[11] it was reported that approximately 55% of ultrasound requests did not conform to the guidelines as compared to 40% of requests for computed tomography scans and 11% of magnetic resonance imaging scans. In another study,[12] it was demonstrated that 76% of ultrasound requests were unjustified; a high proportion of the requests also lacked information or a clear clinical query.
We conducted this study to determine whether family physicians (FPs) at North West Armed Force Prince Salman Hospital, Tabuk, made requests for ultrasound examinations appropriately. Our secondary objective was to enumerate positive and negative ultrasound reports for various diagnostic indications.
MATERIALS AND METHODS
This was a cross-sectional study conducted from June to August, 2010, on all FPs at the Family Medicine Department of North West Armed Forces Prince Salman Hospital (NWAFPSH), Tabuk, and its three peripheral family medicine clinics. The Family Medicine Department of NWAFPSH is one of the largest departments of the hospital. It has >80 physicians working at different competency levels, namely, general physicians (GP), registrars, senior registrars, and consultants. The department supervises nine peripheral clinics, which are attached to military units.
During the study period, 68,738 patients were examined at the family medicine clinics of the hospital, with an average daily turnover of 881 patients. A total of 815 patients were referred to radiology for an initial ultrasound examination. Pregnant women and patients who were referred for a follow-up ultrasound examination were excluded from the study.
All FPs were routinely required to fill a standardized request form for an ultrasound referral. A predesigned referral request was used for all varieties of radiological procedures. The form included the patient's identification, clinical history, examination findings, provisional diagnosis, requested procedure, and special instructions for carrying out the examination. When patients presented at the reception counter of the Radiology Department to register for the procedure, a referral request form was scanned and saved in the computer, and an appointment date and time given to the patient. During the procedure, the radiologist could review the scanned copy of the referral request, which had the clinical information written by the requesting FP.
The investigator had access to the scanned referral request and report after obtaining written permission from the administration of the Radiology Department. Referral request forms for ultrasound examination and procedure reports were examined on a daily basis, and the required information was transferred to a predesigned questionnaire. The patient's history, name of the requesting FP and reporting radiologist were kept confidential and were not considered necessary to any aspect of this study.
Data were analyzed using the Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL), version 16.0. Means and standard deviations were computed for quantitative variables, while frequencies and percentages were calculated for categorical variables. Univariate logistic regression was used to determine the association between the referring physician's qualification and the age of the patient. P < 0.05 was considered to be significant.
RESULTS
Of the 815 patients who were referred for an initial ultrasound, 478 (58.7%) were females. The mean age at referral was 30 ± 18.5 years for females and 34 ± 20.7 years for males. The mean age of patients who were referred for a breast ultrasound was 29 years. The age and sex of the patient were not mentioned in two request forms.
Most ultrasound examinations were requested by GPs (n = 399; 49.0%), followed by consultants (n = 158; 19.4%), registrars (n = 151; 18.5%), and senior registrars (n = 107; 13.1%). 93% of the ultrasound examinations were ordered as routine investigations, while the rest were marked “urgent”. 98% of the ultrasound scans were performed and reported by radiology registrars. The requested procedure was illegible in 76 (9.3%) of the request forms and the radiologist had to confirm the clinical query by calling the requesting physician. Instructions for the procedure were not mentioned in 187 (23%) of the requests; the clinical history of the patient and the provisional diagnosis were not mentioned in 50% and 56% of the requests, respectively. In those cases, the radiologist contacted the referring physician by phone for clarification of the instructions before proceeding with the procedure. Only 46% of the request forms contained conclusive information and instructions.
The clinical indications for the requested ultrasound examinations are listed in Table 1. The most frequently requested radiology investigations were abdominal and pelvic ultrasound [Figure 1]. Ultrasound results were normal in 581 (71.2%) of the cases [Table 2]. The highest proportion of abnormal ultrasound reports were observed in scans of the scrotum/testis, followed by neck/thyroid and the breast [Table 3].
Table 1.
Distribution of clinical indications for ultrasound requests by gender
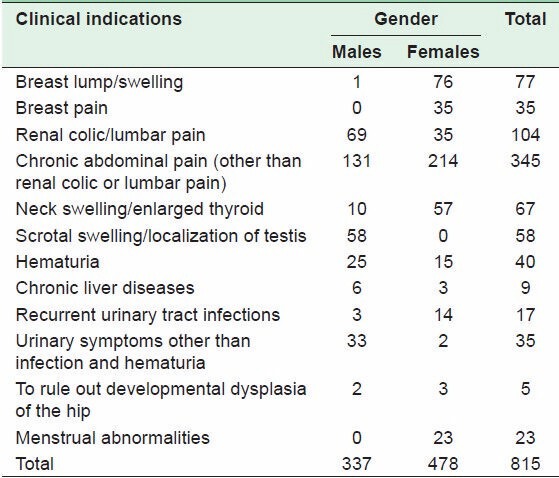
Figure 1.
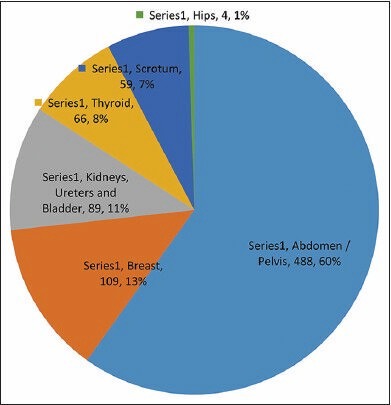
Proportion of ultrasound scans by type
Table 2.
Frequency of ultrasound findings
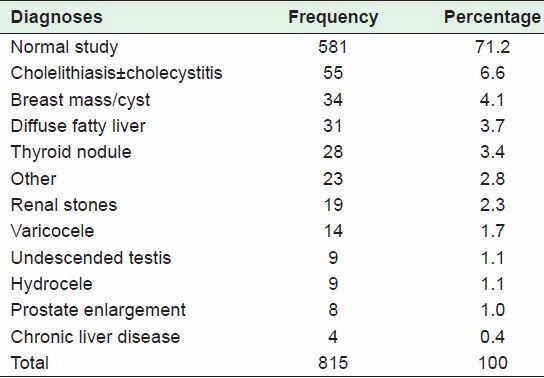
Table 3.
Frequency of abnormal reports for different ultrasound procedures*
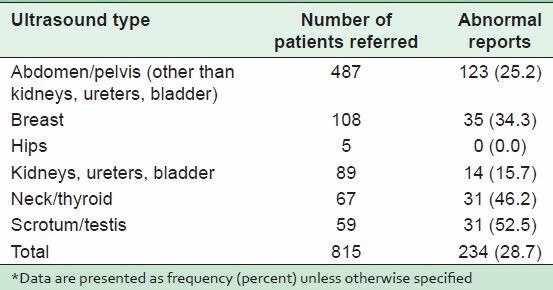
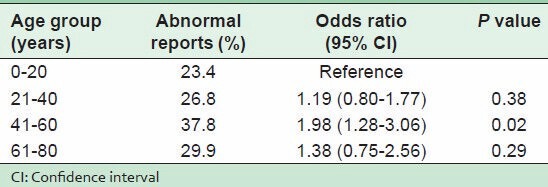
Abdominal/pelvic ultrasound was more likely to be reported as normal compared to ultrasound of any other region (P = 0.007). There was no difference in the likelihood of an abnormal report based on the qualification of the physician. However, patients aged 41-60 years were more likely to have an abnormal ultrasound finding [P = 0.02; Table 4].
Table 4.
Univariate logistic regression showing association between age and the probability of an abnormal ultrasound report
DISCUSSION
Family physicians provide comprehensive primary health care in the outpatient setting, where primary investigations like blood, urine, stool and radio-diagnostic imaging are the first step in managing patients with acute and chronic complaints. Ultrasound is relatively noninvasive, safe, and well-tolerated by the patients; hence, it is very frequently used in family practice. The Royal College of General Practitioners and Radiographers also allow trained GPs to perform ultrasound examinations in primary care.[13]
For any diagnostic procedure, physicians of any specialty should provide detailed clinical information on the request form in order to orient the radiologist to the particular pathology for which the procedure was requested. The patient's identification, age, sex, provisional diagnosis, and instructions for the procedure should be mentioned clearly and in legible writing. In our study, we found that only 46% of the referrals provided the required information, implying that it is necessary to educate FPs about radiology referral protocols so that results obtained from the referral would be beneficial.
Upper abdominal pain was the most frequent complaint for which an abdominal/pelvic ultrasound was requested. This is consistent with a previous study[14] in which pain was the most common indication for an abdominal ultrasound. Yet, pain was shown to have a low yield for abnormal ultrasound findings, but the scanning of abdominal swellings/masses gave the highest proportion of abnormal findings.[14] Some authors[15] have reported that a normal ultrasound scan may help to alleviate patient anxiety. Furthermore, there are reports that abdominal ultrasound examinations can reduce the number of patients referred to a medical specialist, and that prereferral investigations may speed up patients' care at specialty clinics.[4,16,17] On the other hand, it could be argued that the inappropriate use of imaging studies is usually the result of patient requests, high public expectations for imaging tests, and physicians' fear of liability for a missed diagnosis.[18,19] This, consequently, increases the cost of primary health care, may also provoke anxiety and lead to over-treatment as a result of incidental positive findings.[4,20]
Among the patients referred for ultrasound, only 28.8% had an abnormal report, which is consistent with the findings of a previous study.[4] About 60% of all the requests were for abdominal and pelvic ultrasounds, 25% of which showed abnormal findings. Similar results were observed in other studies conducted abroad in which 25-30% of the results of abdominal examinations were abnormal.[21,22]
The most frequent finding on ultrasound imaging in patients with lower urinary tract symptoms was prostate hypertrophy, which is in line with results reported by other authors.[23] In their study, the authors found that in patients presenting with symptoms of abdominal/lumbar pain or hematuria, ultrasound was positive for urolithiasis in 13% of the cases, whereas an abnormal report was documented in only 16% of the ultrasound scans requested for suspected cholecystitis. Conversely, another study showed that ultrasound findings were positive in 28% of the cases of suspected cholelithiasis.[16] It is plausible that because our study was conducted in a military hospital, where all kinds of diagnostic modalities are provided free of charge, physicians request investigations without a clinical indication, primarily to satisfy patients.
Among female patients who presented with a breast lump or pain, there was an abnormal ultrasound finding in approximately 34.3%; the mean age of patients referred for a breast ultrasound was 29 years. This was in accordance with the guideline that an ultrasound should be the first modality for the evaluation of a breast mass in women younger than 30 years.[24]
During the study period, about 46.2% of the patients who presented with a neck swelling or an enlarged thyroid had abnormal ultrasound findings. Because of the increase in the use of ultrasound in the management of clinically abnormal thyroid glands, it is now recommended in the initial evaluation of thyroid nodules,[25] which are reportedly palpable in 7% of adults; 5% of these nodules are malignant.[26] Ultrasound also detects smaller nodules that are not clinically palpable.[27] Hence, requests for ultrasound scans of the thyroid were appropriate at the Family Medicine Department of NWAFPSH.
CONCLUSION
Our study indicates that there is a need to educate FPs about imaging referral protocols in order to achieve better outcomes. Although ultrasound is relatively safe and inexpensive, physicians should be aware of the marginal gain from each subsequent imaging request. Requests for ultrasound scans should have a clinical indication, and the decision to request for imaging should not be based on such factors as patient request or physician satisfaction.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hofmann B. Too much of a good thing is wonderful. A conceptual analysis of excessive examinations and diagnostic futility in diagnostic radiology? Med Health Care Philos. 2010;13:139–48. doi: 10.1007/s11019-010-9233-8. [DOI] [PubMed] [Google Scholar]
- 2.Mariani PJ. Ultrasound use and “overuse”. West J Emerg Med. 2010;11:319–21. [PMC free article] [PubMed] [Google Scholar]
- 3.Smith-Bindman R, Miglioretti DL, Larson EB. Rising use of diagnostic medical imaging in a large integrated health system. Health Aff (Millwood) 2008;27:1491–502. doi: 10.1377/hlthaff.27.6.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Speets AM, Hoes AW, van der Graaf Y, Kalmijn S, de Wit NJ, van Swijndregt AD, et al. Upper abdominal ultrasound in general practice: Indications, diagnostic yield and consequences for patient management. Fam Pract. 2006;23:507–11. doi: 10.1093/fampra/cml027. [DOI] [PubMed] [Google Scholar]
- 5.Carton M, Auvert B, Guerini H, Boulard JC, Heautot JF, Landre MF, et al. Assessment of radiological referral practice and effect of computer-based guidelines on radiological requests in two emergency departments. Clin Radiol. 2002;57:123–8. doi: 10.1053/crad.2001.0827. [DOI] [PubMed] [Google Scholar]
- 6.Kerry S, Oakeshott P, Dundas D, Williams J. Influence of postal distribution of the Royal College of Radiologists' guidelines, together with feedback on radiological referral rates, on X-ray referrals from general practice: A randomized controlled trial. Fam Pract. 2000;17:46–52. doi: 10.1093/fampra/17.1.46. [DOI] [PubMed] [Google Scholar]
- 7.Glaves J. The use of radiological guidelines to achieve a sustained reduction in the number of radiographic examinations of the cervical spine, lumbar spine and knees performed for GPs. Clin Radiol. 2005;60:914–20. doi: 10.1016/j.crad.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 8.Bautista AB, Burgos A, Nickel BJ, Yoon JJ, Tilara AA, Amorosa JK, et al. Do clinicians use the American College of Radiology Appropriateness criteria in the management of their patients? AJR Am J Roentgenol. 2009;192:1581–5. doi: 10.2214/AJR.08.1622. [DOI] [PubMed] [Google Scholar]
- 9.Liel Y, Fraenkel N. Brief report: Use and misuse of thyroid ultrasound in the initial workup of patients with suspected thyroid problems referred by primary care physicians to an endocrine clinic. J Gen Intern Med. 2005;20:766–8. doi: 10.1111/j.1525-1497.2005.0124.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lackner K, Krug B, Stützer H, Sechtem U, Heindel W. A prospective study to assess the need for requested radiological studies. Rofo. 1996;165:4–9. doi: 10.1055/s-2007-1015706. [DOI] [PubMed] [Google Scholar]
- 11.Van Breuseghem I, Geusens E. Assessment of the appropriateness of requested radiological examinations for outpatients and the potential financial consequences of guideline application. JBR-BTR. 2006;89:8–11. [PubMed] [Google Scholar]
- 12.Sardanelli F, Quarenghi M, Fausto A, Aliprandi A, Cuppone MT. How many medical requests for US, body CT, and musculoskeletal MR exams in outpatients are inadequate? Radiol Med. 2005;109:229–33. [PubMed] [Google Scholar]
- 13.Robinson L, Potterton J, Owen P. Diagnostic ultrasound: A primary care-led service? Br J Gen Pract. 1997;47:293–6. [PMC free article] [PubMed] [Google Scholar]
- 14.Aboud M, Mkony C, Wustner M. Elective abdominal ultrasonography by surgeons at MNH, Dar-Es-Salaam, Tanzania. East Cent Afr J Surg. 2006;11:52–56. [Google Scholar]
- 15.O'Mahony N, McCarthy E, McDermott R, O'Keeffe S. Who's the doctor. Patients' perceptions of the role of the breast radiologist: A lesson for all radiologists? Br J Radiol. 2012;85:e1184–9. doi: 10.1259/bjr/74006772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cherryman G. Imaging in primary care. Br J Gen Pract. 2006;56:563–4. [PMC free article] [PubMed] [Google Scholar]
- 17.Connor SE, Banerjee AK. General practitioner requests for upper abdominal ultrasound: Their effect on clinical outcome. Br J Radiol. 1998;71:1021–5. doi: 10.1259/bjr.71.850.10211061. [DOI] [PubMed] [Google Scholar]
- 18.Dunnick NR, Applegate KE, Arenson RL. The inappropriate use of imaging studies: A report of the 2004 Intersociety Conference. J Am Coll Radiol. 2005;2:401–6. doi: 10.1016/j.jacr.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 19.Cohen O, Kahan E, Zalewski S, Kitai E. Medical investigations requested by patients: How do primary care physicians react? Fam Med. 1999;31:426–31. [PubMed] [Google Scholar]
- 20.Severens JL, Sonke G, Laheij RJ, Verbeek AL, De Vries Robbé PF. Efficient diagnostic test sequence: Applications of the probability-modifying plot. J Clin Epidemiol. 2001;54:1228–37. doi: 10.1016/s0895-4356(01)00391-2. [DOI] [PubMed] [Google Scholar]
- 21.Charlesworth CH, Sampson MA. How do general practitioners compare with the outpatient department when requesting upper abdominal ultrasound examinations? Clin Radiol. 1994;49:343–5. doi: 10.1016/s0009-9260(05)81803-3. [DOI] [PubMed] [Google Scholar]
- 22.Colquhoun IR, Saywell WR, Dewbury KC. An analysis of referrals for primary diagnostic abdominal ultrasound to a general X-ray department. Br J Radiol. 1988;61:297–300. doi: 10.1259/0007-1285-61-724-297. [DOI] [PubMed] [Google Scholar]
- 23.Patel NS, Blick C, Kumar PV, Malone PR. The diagnostic value of abdominal ultrasound, urine cytology and prostate-specific antigen testing in the lower urinary tract symptoms clinic. Int J Clin Pract. 2009;63:1734–8. doi: 10.1111/j.1742-1241.2009.02138.x. [DOI] [PubMed] [Google Scholar]
- 24.Houssami N, Brennan M, French J, Fitzgerald P. Breast imaging in general practice. Aust Fam Physician. 2005;34:467–73. [PubMed] [Google Scholar]
- 25.Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214. doi: 10.1089/thy.2009.0110. [DOI] [PubMed] [Google Scholar]
- 26.Brennan M, French J. Thyroid lumps and bumps. Aust Fam Physician. 2007;36:531–6. [PubMed] [Google Scholar]
- 27.Marqusee E, Benson CB, Frates MC, Doubilet PM, Larsen PR, Cibas ES, et al. Usefulness of ultrasonography in the management of nodular thyroid disease. Ann Intern Med. 2000;133:696–700. doi: 10.7326/0003-4819-133-9-200011070-00011. [DOI] [PubMed] [Google Scholar]


