Abstract
Background
There is much interest in ultra-short alcohol screening in primary care that may support brief alcohol interventions. Brief screening consisting of one or two questions might be used alone or in combination with longer tests as recommended by the Primary Care Service Framework.
Aim
To investigate whether a simple one and two question screening might prove an accurate and acceptable screening method in primary care.
Design and setting
A systematic literature search, critical appraisal and meta-analysis were conducted.
Method
A comprehensive search identified 61 analyses of single questions to detect alcohol problems including 17 that took place in primary care, using a robust interview standard. Despite focusing alcohol-use disorder in primary care settings, heterogeneity remained high, therefore random effects and bivariate meta-analyses were used.
Results
After adjustments, diagnostic accuracy of a single-question approach was given by a sensitivity of 54.5% (95% CI = 43.0% to 65.5%) and a specificity of 87.3% (95% CI = 81.5% to 91.5%) using meta-analytic weighting. Two questions had a sensitivity of 87.2% (95% CI = 69.9% to 97.7%) and specificity of 79.8% (95% CI = 75.7% to 83.6%). Looking at each question individually, the most successful single question was a modification of the Single Alcohol Screening Question (SASQ) namely, ‘How often do you have six or more drinks on one occasion?’. The optimal approach appears to be two questions followed by the CAGE questionnaire, which achieved an overall accuracy of 90.9% and required only 3.3 questions per attendee.
Conclusion
Two brief questions can be used as an initial screen for alcohol problems but only when combined with a second-step screen. A brief alcohol intervention should be considered in those individuals who answer positively on both steps.
Keywords: alcohol, diagnostic accuracy, diagnostic validity, primary care, sensitivity, specificity
INTRODUCTION
Alcohol problems are common in primary care with between 7% and 30% of attendees having at-risk drinking or an alcohol-use disorder.1–3 In a meta-analysis of five in primary care studies the pooled prevalence of lifetime problem drinking was 19.8%.4 Many authors have therefore suggested that GPs are well positioned to identify and manage alcohol problems.5,6 Several effective treatment packages called ‘brief alcohol interventions’ have been developed and tested.7,8 Clearly these interventions require adequate initial identification of alcohol problems, yet only about one-third of such individuals are detected by their GP.9–12 Studies conducted in the US, UK, Australia, and Finland indicate that clinicians frequently do not screen for problem drinking, and fail to address the problem in at least one-third to one-half of cases even when the diagnosis is known.9,13–18 A recent meta-analysis found that GPs had a clinical detection sensitivity of 42% but alcohol problems were recorded correctly in the notes only 27.3% of the time.19
In response to these concerns The Institute of Medicine, the National Institute on Alcohol Abuse and Alcoholism (NIAAA), the American Medical Association, and the American Society of Addiction Medicine have all recommended that clinicians routinely ask patients about alcohol use.20–23 In order to screen for problem drinking, the US NIAAA and the US Preventive Services Task Force (USPSTF) recommend population screening; that is, physicians should ask all attendees whether they drink, and assess the specific quantity, frequency, and pattern of consumption, but they did not recommend a specific tool.24 In 2004, the USPSTF recommended screening is accompanied by behavioural counselling interventions to reduce alcohol misuse by adults in primary care settings.25 The NIAAA also recommends targeted screening (case-finding) in that all patients who drink alcohol should be screened with the four CAGE questions.21 In the UK, the Primary Care Service Framework prefers the 10 AUDIT questions; in fact, it recommends an algorithm approach whereby either the Single Alcohol Screening Question (SASQ) (1 item), Fast Alcohol Screening Test (FAST) (4 items), Alcohol-use disorders Identification Test (AUDIT)-C (3 items) or AUDIT-PC (5 items) is applied as an initial first step, followed by the remaining AUDIT questions given to those who initially score positive on the screening test.26 Yet choice of the initial steps is not yet clear,27 and no evidence has yet been presented for algorithm approaches.
How this fits in
Screening for alcohol misuse in primary care is important because it is common and because brief interventions can be effective. However, the most useful simple screening questions to ask remain to be defined. In a meta-analysis of their use, it appears that both 1- and 2-item screening questions have value, and that they should be followed by a second, more detailed assessment to determine the need for intervention or referral.
In reality, many GPs have difficulty applying routine alcohol screening, although most state that they often inquire about drinking behaviours.21,28 Indeed observational studies have shown that screening for alcohol problems is far from routine in primary care.18,29–32 In the UK, alcohol screening sometimes occurs at patient registration but is usually opportunistic.33 Investigations into alcohol screening practices have consistently found that most physicians ask patients about consumption, but few go beyond an initial inquiry.31,34 Most alcohol discussions last less than 1 minute.35 D’Amico et al examined primary care physician practices in over 7000 visits; practitioners asked only 29% of all attendees about their drinking over the course of 1 year, although they asked 44% of problem drinkers about their drinking. Of those individuals with problem drinking, 49% received relevant advice.36
Lessons from screening studies for depression suggest that ultra-short methods consisting of one or two questions might be valuable in some circumstances.37 However such methods often have low positive predictive value.38 The aim of this study was to find out whether very simple one and two question screening might prove an accurate and acceptable screening method in primary care using quantitative meta-analysis. It was hypothesised that one question might have good rule-in but poor rule-out performance when used alone.
METHODS
Inclusion/exclusion criteria
The principal inclusion criteria were studies that examined the diagnostic accuracy of simple verbal questions to identify those with defined alcohol problems in primary care. No language restrictions were applied. This study was principally concerned with the accuracy of detecting those individuals with defined alcohol problems, as opposed to an assessment of alcohol intake, therefore to minimise heterogeneity, the criterion standard required (established by interview) was the DSM or ICD ‘alcohol-use disorder’, rather than alcohol dependence. Alcohol-use disorder can be further subdivided into alcohol abuse and alcohol dependence. Studies that did not present sufficient primary data or failed to employ an adequate criterion standard were excluded (such as studies based on self-reported alcohol use).39 The initial citations were screened to exclude studies that did not assess 1- or 2-item questions to identify alcohol problems. After this initial sifting process, papers were independently evaluated for eligibility. Disagreements were resolved by discussion.
Search, sources, and appraisal
A systematic literature search, critical appraisal and meta-analysis were conducted. MEDLINE/PubMed and Embase abstract databases were searched from inception to January 2014 (Appendix 1). In four full text collections (Science Direct, Ingenta Select, Ovid Full text, Blackwell-Wiley Interscience) the same search terms were used (Appendix 1) but as a full text search and citation search. The abstract database, Web of Knowledge (4.0, ISI) was searched, using the same terms as in Appendix 1 as a text word search, and using key papers in a reverse citation search. Appraisal of each article was conducted by all authors independently using QUADAS.40 This is a standardised quality appraisal form and is recommended by a number of organisations such as the Cochrane Collaboration and the National Institute of Health and Clinical Excellence. No abstracts or non-English articles were found.
Data collection process
A standardised data extraction form was used, which was developed and piloted on several previous systematic reviews of diagnostic accuracy conducted by the authors.41 Data extraction was conducted independently, checked, and differences were resolved by discussion. Variables extracted were: country of study, setting, patient characteristics (such as age and sex), reference standard (including cut-off if relevant), question used to identify alcohol problems, sample size, blindness of the interviewers to the index test, and Youden scores (sensitivity + specificity - 1).42 For the purposes of the meta-analyses sensitivity, specificity, and prevalence of alcohol-use disorder (as measured by the reference standard) were extracted. In addition, if not provided in the papers, 2×2 tables (true positives, false positives, true negatives, and false negatives) were calculated from this data for inclusion in the meta-analysis. Secondary outcomes were an area under the curve analysis (see below) for screening and case-finding performance.
Analysis
Meta-analysis
Random effects meta-analysis were used to synthesise and provide pooled estimates of sensitivity and specificity for the use of a single question or two questions to identify people with alcohol problems. In addition, a bivariate meta-analysis was conducted using the metandi commands in Stata (version 10). This method fits a 2-level model, with independent binomial distributions for the true positives and true negatives conditional on the sensitivity and specificity in each study, and a bivariate normal model for the logit transforms of sensitivity and specificity between studies.43 A summary Receiver Operator Characteristic curve (sROC), where each data point represents a separate study, was then constructed using the bivariate model to produce a 95% confidence ellipse within ROC space. Additionally, a Bayesian curve analysis was undertaken, which plots all post-test probabilities from all pre-test probabilities regardless of prevalence. Heterogeneity was assessed using the I2 statistic.44 In addition, publication bias was assessed both visually using funnel plots and formally using the Begg-Mazumdar test.45
Accuracy and clinical utility
Further analyses were conducted to assess the accuracy and clinical utility of one or two questions to identify people with alcohol problems, both generally (using any one-question or two-question approach) and in comparison with one another. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), likelihood ratios and clinical utility index were calculated using the online calculator (www.clinicalutility.co.uk). Clinical utility index allows a qualitative measure of clinical accuracy.46 Positive clinical utility is a proxy for rule-in accuracy or case-finding. Negative clinical utility is a proxy for rule-out accuracy or screening.
RESULTS
Study description and methods
There were 15 tests of individual questions identified in six publications47–52 and two tests of two-question approaches, involving 5646 unique individuals.39,50 All were diagnostic accuracy studies. The sample size of individual studies ranged from 227 to 1333 individuals (33–261 with alcohol-use disorders) (Tables 1 and 2). Most studies used a DSM-based definition of alcohol-use disorder, specifically alcohol abuse and no study examined alcohol dependence. One study defined substance abuse according to DSM-III-R.50 The pooled prevalence of alcohol-use disorder was 21.0% (95% CI = 20.0% to 22.1%).
Table 1.
QUADAS Methodological appraisal of single-question studies
| Study ID | Representative spectrum? | Reference standard acceptable? | Acceptable delay between tests? | Partial verification avoided? | Differential verification avoided? | Incorporation avoided? | Ref standard blinded? | Index test blinded? | Relevant clinical information | Uninterpretable results reported? | Withdrawals explained? |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Single-question studies | |||||||||||
| Bradley et al, 200149 | Unclear | Yes | Yes | Unclear | Yes | No | Yes | Unclear | Yes | No | Yes |
| Brown et al, 200150 | Yes | Yes | Yes | Yes | Yes | No | Unclear | Unclear | Yes | No | No |
| Fleming et al, 199147 | Yes | Yes | Yes | Yes | Yes | No | Unclear | Unclear | Yes | No | No |
| Seale et al, 200651 | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | No | No |
| Smith et al, 200952 | Unclear | Yes | Unclear | Yes | Yes | Yes | No | Unclear | Unclear | No | Yes |
| Volk, et al, 199747 | Yes | Yes | Yes | Yes | Yes | No | Unclear | Unclear | Unclear | No | Unclear |
| Two-question studies | |||||||||||
| Brown et al, 200150 | Yes | Yes | Yes | Yes | Yes | No | Unclear | Unclear | Yes | No | No |
| Vinson et al, 200739 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | No | No |
Table 2.
Statistical appraisal of single- and two-question studies
| Author | Phrase of questions | Criterion standard | Total sample | All cases | Non-cases | Unadjusted sensitivity | Unadjusted specificity | Unadjusted PPV | Unadjusted NPV |
|---|---|---|---|---|---|---|---|---|---|
| Single-question studies | |||||||||
|
| |||||||||
| Seale et al, 200651 | SASQ (When was the last time you had more than X drinks in one day? | Alcohol-use disorder (DSM-IV) | 625 | 127 | 498 | 0.866 | 0.490 | 0.302 | 0.935 |
|
| |||||||||
| Fleming et al, 199147 | Unique — Have you ever had a drinking problem? | Alcohol-use disorder (DSM-III) | 280 | 82 | 198 | 0.573 | 0.879 | 0.662 | 0.833 |
|
| |||||||||
| Unique — Do you have a current drinking problem? | Alcohol-use disorder (DSM-III) | 280 | 82 | 198 | 0.317 | 0.970 | 0.813 | 0.774 | |
|
| |||||||||
| Brown et al, 200150 | Unique — In the last year, how many times have you not remembered things that happened while you were drinking or using drugs? | Substance Use Disorder (CIDI-SAM for DSM-III-R) | 1136 | 261 | 875 | 0.483 | 0.925 | 0.656 | 0.857 |
|
| |||||||||
| Unique — In the last year, have you ever drunk or used drugs more than you meant to? | Substance Use Disorder (CIDI-SAM for DSM-III-R) | 1136 | 261 | 875 | 0.701 | 0.809 | 0.523 | 0.901 | |
|
| |||||||||
| Unique — Have you felt you wanted or needed to cut down on your drinking or drug use in the last year? | Substance Use Disorder (CIDI-SAM for DSM-III-R) | 1136 | 261 | 875 | 0.563 | 0.917 | 0.668 | 0.876 | |
|
| |||||||||
| Unique — In the last year, have you drunk or used non-prescription drugs to deal with your feelings, stress, or frustration? | Substance Use Disorder (CIDI-SAM for DSM-III-R) | 1136 | 261 | 875 | 0.544 | 0.869 | 0.553 | 0.865 | |
|
| |||||||||
| Unique — As a result of your drinking or drug use, did anything happen in the last year that you wish didn’t happen? | Substance Use Disorder (CIDI-SAM for DSM-III-R) | 1136 | 261 | 875 | 0.410 | 0.960 | 0.754 | 0.845 | |
|
| |||||||||
| Bradley et al, 200149 | SASQ-Modified How often do you have six or more drinks on one occasion? | Alcohol-use disorder (DSM-III-R) or hazardous drinking (NAAA) | 227 | 92 | 135 | 0.772 | 0.830 | 0.755 | 0.842 |
|
| |||||||||
| SASQ-Modified Maximum number of drinks per occasion | Alcohol-use disorder (DSM-III-R) or hazardous drinking (NAAA) | 227 | 92 | 135 | 0.587 | 0.770 | 0.635 | 0.732 | |
|
| |||||||||
| Volk et al, 199748 | CAGE: cut down question | Alcohol-use disorder (DSM-IV) | 1333 | 205 | 1128 | 0.629 | 0.840 | 0.417 | 0.926 |
|
| |||||||||
| CAGE: annoyed question | Alcohol-use disorder (DSM-IV) | 1333 | 205 | 1128 | 0.239 | 0.930 | 0.383 | 0.871 | |
|
| |||||||||
| CAGE: guilty question | Alcohol-use disorder (DSM-IV) | 1333 | 205 | 1128 | 0.371 | 0.900 | 0.402 | 0.887 | |
|
| |||||||||
| CAGE: eye-opener question | Alcohol-use disorder (DSM-IV) | 1333 | 205 | 1128 | 0.210 | 0.950 | 0.434 | 0.869 | |
|
| |||||||||
| Smith et al 200952 | SASQ-Modified How many times in the past year have you had X or more drinks in a day? | Alcohol-use disorder (DSM-IV) | 286 | 33 | 253 | 0.879 | 0.672 | 0.259 | 0.977 |
|
| |||||||||
| Two-question studies | |||||||||
|
| |||||||||
| Brown et al 200150 | In the last year, have you ever drunk or used drugs more than you meant to? OR Have you felt you wanted or needed to cut down on your drinking or drug use in the last year? | Substance Use Disorder (CIDI-SAM for DSM-III-R) | 1136 | 261 | 875 | 0.793 | 0.779 | 0.518 | 0.927 |
|
| |||||||||
| Vinson et al 200739 | Q1 Recurrent drinking in situations in which it is physically hazardous, and Q2 drinking in larger amounts or over a longer period than intended | Alcohol-use disorder (DSM-IV) | 623 | 126 | 498 | 0.944 | 0.819 | 0.569 | 0.983 |
NPV = negative predictive value. PPV = positive predictive value.
Diagnostic accuracy of the single-question test
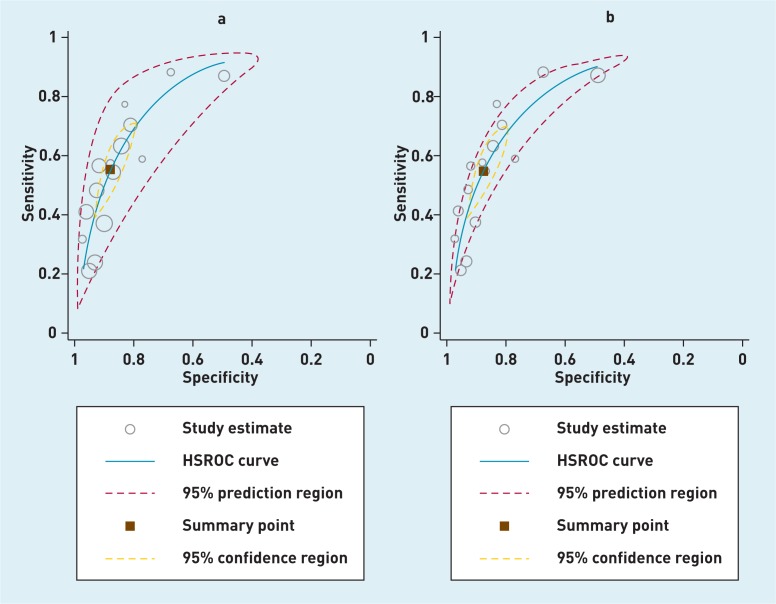
Across 15 analyses a single-question approach facilitated the identification of 453 out of 800 unique individuals with problem drinking (cases), an uncorrected pooled sensitivity of 56.6%. There was no evidence of publication bias (Begg-Mazumdar: Kendall’s Tau-b = 0.21, P = 0.29). A single question allowed identification of 2510 or 3087 unique individuals without problem drinking (non-cases), an uncorrected pooled specificity of 81.3%. There was high heterogeneity present (I2 = 96.3%). On bivariate meta-analysis sensitivity was adjusted to 54.5% (95% CI = 43.0% to 65.5%) and specificity was 87.3% (95% CI = 81.5% to 91.5%) (Figure 1). At the stated prevalence, the PPV was 53.3% (95% CI = 48.0% to 58.5%) and the NPV was 87.8% (95% CI = 85.9% to 89.5%). Positive likelihood ratio was 4.29 (95% CI = 3.84 to 4.80) and negative likelihood ratio 0.52 (95% CI = 0.48 to 0.56). The positive clinical utility index score for the single-question test was 0.287 (95% CI = 0.286 to 0.288) rated as ‘very poor’. The negative clinical utility index score was 0.769 (95% CI = 0.769 to 0.769) rated as ‘good’.
Figure 1.
Bayesian pre-test post-test accuracy of single-question approach to alcohol-use disorder in primary care (a = unadjusted; b adjusted for unique patients).
Based on the Youden scores of each question, the most accurate single questions appeared to be ‘How often do you have six or more drinks on one occasion?’ from the SASQ-modified version. A negative answer to the ‘eye-opener question’ from the CAGE and the question ‘As a result of your drinking or drug use, did anything happen in the last year that you wish didn’t happen?’; both had excellent rule-out performance with low false negatives.
Diagnostic accuracy of two questions
There were only two analyses of a two-question approach that had an adjusted meta-analysis sensitivity of 87.2% (95% CI = 69.9% to 97.7%) and specificity was 79.8% (95% CI = 75.7% to 83.6%). At 21% prevalence, the PPV value was 53.4% (95% CI = 49.4% to 57.6%) and the negative predictive value was 95.9% (95% CI = 94.6% to 97.0%). Positive likelihood ratio was 4.32 (CI = 3.86 to 4.83) and negative likelihood ratio 0.16 (95% CI = 0.12 to 0.21). The positive clinical utility index score for the single-question test was 0.478 (95% CI = 0.477 to 0.479) rated as ‘poor’. The negative clinical utility index score was 0.763 (95% CI = 0.762 to 0.764) rated as ‘good’. In terms of specific questions, based on just two comparisons, the optimal combination of questions was ‘recurrent drinking in situations in which it is physically hazardous combined with drinking in larger amounts or over a longer period than intended’.
Algorithm approach versus routine screening
The merits of an algorithm approach similar to that recommended by the Primary Care Service Framework were examined. An algorithm potentially saves time because only those individuals who screen positive after the first step receive the longer instrument. Using primary care data from two previous meta-analyses a combination of one or two brief questions was compared with either the 4-item CAGE (n = 10, pooled sensitivity = 71% specificity = 91%)53 or the 10-item AUDIT (n = 6, pooled sensitivity = 61.9%, specificity 91.5%).53 Then the accuracy of an algorithm approach was examined, namely a single question or two questions followed by either the CAGE or AUDIT (Table 3).
Table 3.
Algorithm approaches to diagnosis of alcohol problems in primary care in hypothetical 1000 attendees
| Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | Overall accuracy (95% CI) | Positive clinical utility index (95% CI) | Negative clinical utility index (95% CI) | Questions asked per 100 attendees | |
|---|---|---|---|---|---|---|---|---|
| Combined algorithms | ||||||||
| SQ then AUDIT | 0.337 (0.272 to 0.403) | 0.989 (0.981 to 0.996) | 0.886 (0.810 to 0.955) | 0.856 (0.834 to 879) | 0.858 (0.837 to 0.880) | 0.298 (0.292 to 0.303) ‘v poor’ |
0.847 (0.847 to 0.847) ‘excellent’ |
311 |
| 2QQ then AUDIT | 0.540 (0.471to 0.609) | 0.983 (0.973 to 0.992) | 0.885 (0.829 to 0.942) | 0.895 (0.875 to 0.915) | 0.894 (0.875 to 0.913) | 0.478 (0.474 to 0.482) ‘poor’ |
0.880 (0.879 to 0.880) ‘excellent’ |
536 |
| SQ then CAGE | 0.387 (0.319 to 0.455) | 0.988 (0.980 to 0.995) | 0.886 (0.819 to 0.952) | 0.866 (0.844 to 0.888) | 0.867 (0.846 to 0.888) | 0.343 (0.337 to 0.348) ‘v poor’ |
0.855 (0.885 to 0.885) ‘excellent’ |
184 |
| 2QQ then CAGE | 0.620 (0.553 to 0.687) | 0.981 (0.972 to 0.991) | 0.892 (0.841 to 0.944) | 0.912 (0.893 to 0.931) | 0.909 (0.891 to 0.926) | 0.553 (0.549 to 0557) ‘fair’ |
0.895 (0.894 to 0.895) ‘excellent’ |
334 |
| Single applications | ||||||||
| CAGE Single application | 0.615 (0.548 to 0.682) | 0.915 (0.896 to 0.934) | 0.644 (0.576 to 0.712) | 0.905 (0.885 to 0.925) | 0.855 (0.833 to 0.876) | 0.396 (0.392 to 0.400) ‘poor’ |
0.828 (0.828 to 0.828) ‘excellent’ |
400 |
| AUDIT Single application | 0.71 (0.647 to 0.773) | 0.91 (0.890 to 0.930) | 0.664 (0.600 to0.727) | 0.926 (0.908 to 0.944) | 0.870 (to 0.849 to 0.890) | 0.471 (0.468 to 0.475) ‘poor’ |
0.843 (0.842 to 0.843) ‘excellent’ |
1000 |
| SQ Single application | 0.545 (0.476 to 0.614) | 0.873 (0.849 to 0.896) | 0.517 (0.449 to 0.584) | 0.885 (0.862 to 0.907) | 0.807 (0.782 to 0.831) | 0.282 (0.278 to 0.285) ‘v poor’ |
0.772 (0.771 to 0.772) ‘excellent’ |
100 |
| 2QQ Single application | 0.87 (0.823 to 0.917) | 0.798 (0.770 to 0.825) | 0.518 (0.464 to 0.571) | 0.961 (0.946 to 0.976) | 0.812 (0.787 to 0.836) | 0.451 (0.448 to 0.453) ‘poor’ |
0.766 (0.766 to 0.767) ‘excellent’ |
200 |
Table shows hierarchical screening algorithms applied to 1000 hypothetical primary care attendees, of whom 200 have alcohol problems. Calculations from www.clinicalutlity.co.uk. 2QQ = two questions. NPV = negative predictive value. PPV = positive predictive value. SQ = single question.
The most accurate single method was the AUDIT followed by the CAGE, then two-questions and finally a single question. In terms of algorithm approaches the optimal combination was 2QQ then CAGE (0.909, 95% CI = 0.891 to 0.926) although this was almost identically accurate to the 2QQ then the AUDIT (0.894, 95% CI = 0.875 to 0.913). These approaches would be more efficient than CAGE or AUDIT alone. For example for the assessment of 100 hypothetical primary care attendees the AUDIT alone would need 1000 questions to be asked (10 per subject) but the 2QQ and AUDIT algorithm would require 536.
Real-world value
In the same 100 hypothetical attendee scenario as above, at a prevalence of 21%, a GP using only a single question for alcohol-use disorder would correctly identify 11 cases, missing 10. They would correctly identify 69 non-cases and falsely diagnose 10; the overall accuracy would be 80.4%. Using an algorithm approach at the same prevalence, a GP looking for alcohol-use disorder using an algorithm of a single question followed by the CAGE would correctly identify 8 cases, missing 13. They would correctly identify 78 non-cases and falsely diagnose one; the overall accuracy would be 86.1%.
DISCUSSION
Summary
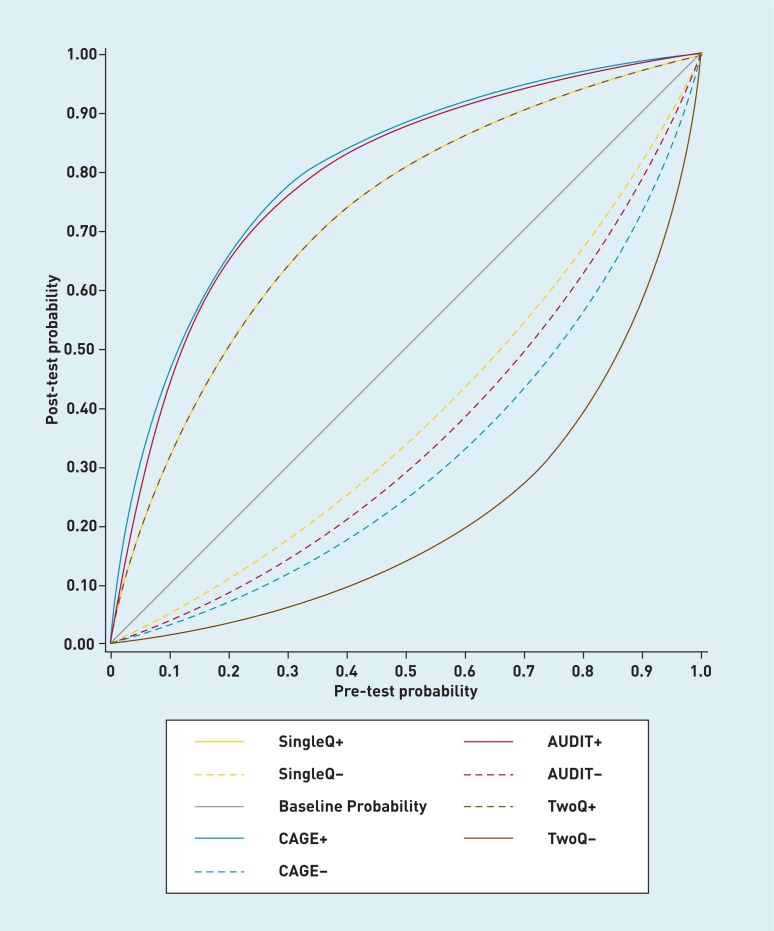
This study is concerned with the methods of detecting those individuals with defined alcohol problems as opposed to an assessment of alcohol intake. In this meta-analysis of 17 tests from seven publications designed to help with the identification of alcohol-use disorder in primary care, a single question had a sensitivity of only 54.5% (95% CI = 43.0% to 65.5%) and specificity of 87.3% (95% CI = 81.5% to 91.5%) but two questions had a sensitivity of 87.2% (95% CI = 69.9% to 97.7%) and a specificity of 79.8% (95% CI = 75.7% to 83.6%). Neither approach is recommended alone because their positive clinical utility was rated as poor for case-finding. For example, PPV was only 50% at a prevalence of 21% (Figure 2). However, when used in algorithmic combination, that is the initial application of one or two questions followed by the longer AUDIT or CAGE only in those who screen positive, then the brief screens are both accurate and efficient.
Figure 2.
Meta-analytic comparison of single question and two question versus CAGE versus AUDIT in primary care (Conditional probability plot using comparison data from CAGE4 and AUDIT .11
Strengths and limitations
This study has several limitations. Despite an extensive search only a small number of studies were found that adhered to a robust interview criterion standard. The study was limited by a lack of data regarding ‘at-risk drinking’ and ‘alcohol dependence’. This could be important as some reports suggest that the CAGE questions perform better in identifying alcohol dependence whereas AUDIT is more sensitive for hazardous and harmful drinkers.54 It was also not possible to separate results by sex, although screening differences may exist in clinical practice for males and females.31 These issues could be addressed in future research. The study also found considerable statistical heterogeneity which could relate to a wide variety of single-question approaches.
Comparison with existing literature
The merits of algorithmic screening have been previously explored.55 The exact approach recommended by the Primary Care Service Framework, namely the SASQ single question ‘How often do you have six or more drinks on one occasion?’ followed by the AUDIT, was reasonably successful. Only two questions followed by the AUDIT and two questions followed by the CAGE were more accurate but at a cost of an additional 2.3 and 0.2 questions per attendee. In clinical practice a GP using only a single question for alcohol-use disorder would be likely to miss 10 cases and falsely diagnose 10 non-cases for every 100 presentations. Using a single question followed by the CAGE the GP would be likely to miss up to 13 cases but with only one false positive. If this rate of missed cases is considered too high, currently the only viable solution is to use a longer questionnaire for all attendees.4,53 However the most common questionnaires for alcohol problems (that is the AUDIT, CAGE, and MAST) are usually considered difficult to use in primary care.56–58 Clinicians prepared to use a few more than two questions have a choice of the three question AUDIT-C59 the 4-item CAGE,4 and the 4-item FAST.60 Of these the FAST and CAGE take only 12–15 seconds in experienced hands but their acceptability in primary care is not yet clear.21,32 The FAST is of particular interest because item 1 on the FAST is in fact the SASQ question (as above) and the authors recommend an algorithmic approach whereby low and high scorers to question 1 receive no further screening but those with intermediate scores receive three follow-up questions extracted from the AUDIT. However the FAST has yet to be evaluated against an interview-based criterion standard in primary care, therefore the authors suggest it requires further testing, particularly alongside other approaches. Further, no single laboratory test has been shown to be a substitute for questionnaire-based screening.61,62
Routine screening
Experts have recommended routine alcohol screening focusing on new patient registrations, general health checks, and special types of consultation.63–65 Mitchell et al previously demonstrated that depression diagnostic accuracy can be improved with multiple assessments.66 The authors expect the authors’ group to occur in relation to alcohol assessment because patients are often seen on multiple occasions. A recent meta-analysis found that GPs had a clinical detection sensitivity for alcohol problems of 42% but a sensitivity of 93.1% when unassisted.19 These figures could be higher in some countries where the recognition of alcohol use is linked to primary care performance incentives. At face value the single-question performance of 54.5% sensitivity and 87.3% specificity is not appreciably different from unassisted ability. However, two questions with a sensitivity of 87.2% and a specificity of 79.8% does seem to be an improvement. This is similar for ultra-short methods of screening for depression where one question is inadequate but two an improvement over clinician judgement.67 Algorithm approaches are better still and can be efficient at the same time. Here the optimal approach appears to be two questions followed by CAGE, which achieved an overall accuracy of 90.9% and requires only 3.3 questions per attendee.
Acceptability
The clinical value of screening tests depends not only on accuracy but also acceptability. The primary purpose of the single item is as a first-step screen to rule-out those unlikely to have an alcohol problem. The authors suggest it is feasible to require one question to be asked routinely, but it is appropriate to examine acceptability even for a single question, as some questions may not be welcome in unselected primary care attendees. Vinson and colleagues rated patients’ comfort with single-item screening. On an ordinal scale in which 1 is ‘very uncomfortable’ and 5 is ‘very comfortable’, patients rated their comfort as 4.2 with a single-question approach.18 Regarding acceptability for staff, clinicians in Missouri were significantly more likely to use the single question than the CAGE questions (81% versus 69%, P = 0.001).18 Assuming a prevalence of 20%, this study found that a GP using a single question as the first step, followed by the AUDIT would achieve the same overall accuracy as the AUDIT or CAGE alone but they would require only 121 questions per 100 attendees rather than 1000 with the AUDIT alone and 400 with the CAGE alone (Table 3). Thus an algorithm approach should retain high acceptability, subject to the choice of the first question. In those that screen positive to both steps, consideration should be given to the brief alcohol interventions where required. An updated Cochrane review identified 24 brief alcohol intervention trials for alcohol problems in general practice.68 After ≥1 year, individuals who received a brief intervention drank less alcohol than individuals in the control group (average difference 38 g per week, range 23g–54 g) although the benefit was not clear for females. A cumulative meta-analysis by date of publication demonstrated that effects have shown significance since 1997.57
That said brief alcohol interventions are performed relatively infrequently in primary care.69 Only 10% of GPs reported doing a brief intervention regularly and 50.0% stated they use this approach occasionally. Furthermore, qualitative work on alcohol screening in the primary care setting in Finland by Aira et al identified that physicians were more comfortable in undertaking a preventive approach for smoking than for alcohol use.70 Factors contributing to this difference were difficulties in recognition and determination of the health risk by physicians, lack of effective tools, and lack of positive feedback after interventions. These must also be considered with any attempts to improve implementation of secondary prevention of alcohol misuse. Even clinicians who participate in successful trials do not necessarily continue with screening and intervention after the study closes.56 It is important to acknowledge that only one study has examined the implementation of single-item screening in primary care. In 126 current drinkers screening rates for alcohol-use disorder increased from 14.6% at baseline to 20.0% after screening implementation and intervention rates rose from 6.3% to 11.8% (P = 0.039).71
Implications for research and practice
From the results of this meta-analysis a cautious recommendation from the authors can be given for one or two verbal question as a screening test for alcohol-use disorder in primary care, but only when paired with a longer screening tool to decide who warrants a brief alcohol intervention. Further research is required to clarify the added value of this approach compared with unaided clinical assessment using a randomised screening implementation study.
Appendix 1. Search results OVID (Embase and Medline)
| # | Searches | Results | Search Type |
|---|---|---|---|
| 1 | alcohol drinking/ or alcoholtoinduced disorders/ or disorders, nervous system/ or alcoholtorelated disorders/ | 90919 | Advanced |
| 2 | exp Alcohol/ | 97021 | Advanced |
| 3 | (drink* or alcohol* or substance abuse or substance misuse).m_titl. | 179279 | Advanced |
| 4 | 1 or 2 | 173857 | Advanced |
| 5 | 3 and 4 | 72133 | Advanced |
| 6 | limit 5 to (‘diagnosis (sensitivity)’ or ‘diagnosis (specificity)’ or ‘diagnosis (optimized)’) | 14267 | Advanced |
| 7 | (sensitivity or specificity or ROC or receivertooperator or accuracy or youden or valid*).mp. [mp=ti, ot, ab, nm, hw, ui, an, sh, tn, dm, mf] | 2249582 | Advanced |
| 8 | 5 and 7 | 5767 | Advanced |
| 9 | 6 or 8 | 16108 | Advanced |
| 10 | (single or question or questions).m_titl. | 198813 | Advanced |
| 11 | 9 and 10 | 96 | Advanced |
| 12 | Primary Health Care/ | 52388 | Advanced |
| 13 | exp Primary Care/ | 92240 | Advanced |
| 14 | (Primary Care or general practit*).mp. [mp=ti, ot, ab, nm, hw, ui, an, sh, tn, dm, mf] | 144598 | Advanced |
| 15 | 12 or 13 or 14 | 198407 | Advanced |
| 16 | 11 and 15 | 14 | Advanced |
| 17 | remove duplicates from 16 | 10 | Advanced |
Funding
None.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: www.bjgp.org/letters
REFERENCES
- 1.Buchsbaum DG, Buchanan RG, Lawton MJ, Schnoll SH. Alcohol consumption patterns in a primary care population. Alcohol Alcohol. 1991;26(2):215–220. doi: 10.1093/oxfordjournals.alcalc.a045103. [DOI] [PubMed] [Google Scholar]
- 2.Fiellin DA, Reid MC, O’Connor PG. Screening for alcohol problems in primary care: a systematic review. Arch Intern Med. 2000;160(13):1977–1989. doi: 10.1001/archinte.160.13.1977. [DOI] [PubMed] [Google Scholar]
- 3.Saitz R. Clinical practice. Unhealthy alcohol use. N Engl J Med. 2005;352:596–607. doi: 10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- 4.Aertgeerts B, Buntinx F, Kester A. The value of the CAGE in screening for alcohol abuse and alcohol dependence in general clinical populations: a diagnostic meta-analysis. J Clin Epidemiol. 2004;57:30–39. doi: 10.1016/S0895-4356(03)00254-3. [DOI] [PubMed] [Google Scholar]
- 5.Fleming MF, Barry KL, Manwell LB, et al. Brief physician advice for problem alcohol drinkers: a randomized controlled trial in community-based primary care practices. JAMA. 1997;277:1039–1045. [PubMed] [Google Scholar]
- 6.Friedmann PD, Saitz R, Samet JH. Management of adults recovering from alcohol or other drug problems: relapse prevention in premature care. JAMA. 1998;279:1227–1231. doi: 10.1001/jama.279.15.1227. [DOI] [PubMed] [Google Scholar]
- 7.Wallace P, Cutler S, Haines A. Randomized controlled trial of general practitioner intervention in patients with excessive alcohol consumption. Br Med J. 1988;297:663–668. doi: 10.1136/bmj.297.6649.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bertholet N, Daeppen JB, Wietlisbach V, et al. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165:986–995. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- 9.Rydon P, Redman S, Sanson-Fisher RW, Reid AL. Detection of alcohol-related problems in general practice. J Stud Alcohol. 1992;53:197–202. doi: 10.15288/jsa.1992.53.197. [DOI] [PubMed] [Google Scholar]
- 10.Cleary PD, Milller M, Bush T, et al. Prevalence and recognition of alcohol abuse in a primary care population. Am J Med. 1988;85:466–471. doi: 10.1016/s0002-9343(88)80079-2. [DOI] [PubMed] [Google Scholar]
- 11.Berner MM, Härter M, Kriston L, et al. Detection and management of alcohol-use disorders in German primary care influenced by non-clinical factors. Alcohol Alcohol. 2007;42(4):308–316. doi: 10.1093/alcalc/agm013. [DOI] [PubMed] [Google Scholar]
- 12.Shore J, Spero MM, Buschbaum D. Screening for alcohol abuse among urban Native Americans in a primary care setting. Psych Serv. 2002;53:757–760. doi: 10.1176/appi.ps.53.6.757. [DOI] [PubMed] [Google Scholar]
- 13.Conigliaro J, Lofgren RP, Hanusa BH. Screening for problem drinking: impact on physician behavior and patient drinking habits. J Gen Intern Med. 1998;13:251–256. doi: 10.1046/j.1525-1497.1998.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaner EF, Heather N, Brodie J, et al. Patient and practitioner characteristics predict brief alcohol intervention in primary care. Br J Gen Pract. 2001;51:822–827. [PMC free article] [PubMed] [Google Scholar]
- 15.Aalto M, Pekuri P, Seppa K. Primary health care professionals’ activity in intervening in patients’ alcohol drinking during a 3-year brief intervention implementation project. Drug Alcohol Depend. 2003;69:9–14. doi: 10.1016/s0376-8716(02)00228-4. [DOI] [PubMed] [Google Scholar]
- 16.Richmond RL, Anderson P. Research in general practice for smokers and excessive drinkers in Australia and the UK. III. Dissemination of interventions. Addiction. 1994;89:49–62. doi: 10.1111/j.1360-0443.1994.tb00849.x. [DOI] [PubMed] [Google Scholar]
- 17.Kaner EF, Lock CA, McAvoy BR, et al. An RCT of three training and support strategies to encourage implementation of screening and brief alcohol intervention by general practitioners. Br J Gen Pract. 1999;49:699–703. [PMC free article] [PubMed] [Google Scholar]
- 18.Vinson DC, Elder NC, Werner JJ, et al. Alcohol-related discussions in primary care: a report from ASPN. J Fam Pract. 2000;49:28–33. [PubMed] [Google Scholar]
- 19.Mitchell AJ, Meader N, Bird V, Rizzo M. Clinical recognition and recording of alcohol disorders by clinicians in primary and secondary care: meta-analysis. Br J Psychiatry. 2012;201:93–100. doi: 10.1192/bjp.bp.110.091199. [DOI] [PubMed] [Google Scholar]
- 20.Institute of Medicine. Broadening the base of treatment for alcohol problems: report of a study by a Committee of the Institute of Medicine, Division of Mental Health and Behavioral Medicine. Washington, DC: National Academy Press; 1990. [Google Scholar]
- 21.National Institute on Alcohol Abuse and Alcoholism. The physician’s guide to helping patients with alcohol problems. Washington, DC: National Institutes of Health; 1995. [Google Scholar]
- 22.Council on Scientific Affairs AMA. AMA guidelines for physician involvement in the care of substance abusing patients. Chicago, IL: American Medical Association; 1979. [Google Scholar]
- 23.American Society of Addiction Medicine Public policy statement on screening for addiction in primary care settings. ASAM News. 1997;17:17–18. [Google Scholar]
- 24.US Preventive Services Task Force. Guide to clinical preventive services. 2nd edn. Alexandria, VA: International Medical Publishing; 1998. [Google Scholar]
- 25.US Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: recommendation statement. Ann Intern Med. 2004;140:554–556. doi: 10.7326/0003-4819-140-7-200404060-00016. [DOI] [PubMed] [Google Scholar]
- 26.NHS Primary Care Contracting. Primary Care Service Framework: alcohol services in primary care. http://cdn.pcc-cic.org.uk/sites/default/files/articles/attachments/primary_care_service_framework_-19may09_clean.doc (accessed 16 Jun 2014)
- 27.Kaner E, Bland M, Cassidy P, et al. Screening and brief interventions for hazardous and harmful alcohol use in primary care: a cluster randomised controlled trial protocol. BMC Public Health. 2009;9:287. doi: 10.1186/1471-2458-9-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Herbert C, Bass F. Early at-risk alcohol intake. Definitions and physicians’ role in modifying behavior. Can Fam Phys. 1997;43:639–644. [PMC free article] [PubMed] [Google Scholar]
- 29.Bradley KA, Curry SJ, Koepsell TD, Larson EB. Primary and secondary prevention of alcohol problems: US internist attitudes and practices. J Gen Intern Med. 1995;10:67–72. doi: 10.1007/BF02600228. [DOI] [PubMed] [Google Scholar]
- 30.Stange KC, Zyzanski SJ, Jaen CR, et al. Illuminating the ‘black box’. A description of 4454 patient visits to 138 family physicians. J Fam Pract. 1998;46:377–389. [PubMed] [Google Scholar]
- 31.Stephan Arndt S, Schultz Sk, Turvey C, Petersen A. Screening for Alcoholism in the Primary Care Setting Are We Talking to the Right People? J Fam Pract. 2002;51:41–46. [PubMed] [Google Scholar]
- 32.Wenrich MD, Paauw DS, Carline JD, et al. Do primary care physicians screen patients about alcohol intake using the CAGE questions? J Gen Intern Med. 1995;10:631–634. doi: 10.1007/BF02602748. [DOI] [PubMed] [Google Scholar]
- 33.Farmer R, Greenwood N. General practitioners’ management of problem drinkers — attitudes, knowledge and practice. Drugs Educ Prev Policy. 2001;8(2):119–129. [Google Scholar]
- 34.Lawner K, Doot M, Gausas J, et al. Implementation of CAGE alcohol screening in a primary care practice. Fam Med. 1997;29:332–335. [PubMed] [Google Scholar]
- 35.Vinson DC, Galliher JM, Reidinger C, et al. Comfortably engaging: which approach to alcohol screening should we use? Ann Fam Med. 2004;2:398–404. doi: 10.1370/afm.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.D’Amico EJ, Paddock SM, Burnam A, et al. Identification of and guidance for problems drinking by general medical providers. Results from a National Survey. Med Care. 2005;43:229–236. doi: 10.1097/00005650-200503000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Mitchell AJ, Coyne JC. Do ultra-short screening instruments accurately detect depression in primary care? A pooled analysis and meta-analysis of 22 studies. Br J Gen Pract. 2007;57(535):144–151. [PMC free article] [PubMed] [Google Scholar]
- 38.Mitchell AJ. Are one or two simple questions sufficient to detect depression in cancer and palliative care? A Bayesian meta-analysis. Br J Cancer. 2008;98:1934–1943. doi: 10.1038/sj.bjc.6604396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vinson DC, Kruse RL, Seale JP. Simplifying alcohol assessment: two questions to identify alcohol-use disorders. Alcohol Clin Exp Res. 2007;31(8):1392–1398. doi: 10.1111/j.1530-0277.2007.00440.x. [DOI] [PubMed] [Google Scholar]
- 40.Whiting P, Rutjes AW, Reitsma JB, et al. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25. doi: 10.1186/1471-2288-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160–174. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- 42.Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–35. doi: 10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 43.Reitsma JB, Glas AS, Rutjes AWS, et al. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58:982–990. doi: 10.1016/j.jclinepi.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 44.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 46.Mitchell AJ. Sensitivity × PPV is a recognized test called the clinical utility index (CUI+) Eur J Epidemiol. 2011;26(3):251–252. doi: 10.1007/s10654-011-9561-x. [DOI] [PubMed] [Google Scholar]
- 47.Fleming MF, Barry KL. The effectiveness of alcoholism screening in an ambulatory care setting. J Stud Alcohol. 1991;52(1):33–36. doi: 10.15288/jsa.1991.52.33. [DOI] [PubMed] [Google Scholar]
- 48.Volk RJ, Cantor SB, Steinbauer JR, Cass AR. Item bias in the CAGE screening test for alcohol-use disorders. J Gen Intern Med. 1997;12:763–769. doi: 10.1046/j.1525-1497.1997.07162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bradley KA, Kivlahan DR, Bush KR, et al. Variations on the CAGE alcohol screening questionnaire: strengths and limitations in VA general medical patients. Alcoholism. 2001;25(10):1472–1478. doi: 10.1097/00000374-200110000-00010. [DOI] [PubMed] [Google Scholar]
- 50.Brown RL, Leonard T, Saunders LA, Papasouliotis O. A two-item conjoint screen for alcohol and other drug problems. J Am Board Fam Pract. 2001;14:95–106. [PubMed] [Google Scholar]
- 51.Seale JP, Boltri JM, Shellenberger S, et al. Primary care validation of a single screening question for drinkers. J Stud Alcohol. 2006;67:778–784. doi: 10.15288/jsa.2006.67.778. [DOI] [PubMed] [Google Scholar]
- 52.Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. Primary Care Validation of a single-question alcohol screening test. J Gen Intern Med. 2009;24(7):783–788. doi: 10.1007/s11606-009-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Berner MM, Kriston L, Bentele M, et al. The alcohol-use disorders identification test for detecting at-risk drinking: a systematic review and meta-analysis. J Stud Alcohol Drugs. 2007;68(3):461–473. doi: 10.15288/jsad.2007.68.461. [DOI] [PubMed] [Google Scholar]
- 54.Fiellin DA, Carrington Reid M, O’Connor PG. Screening for alcohol problems in primary care: a systematic review. Arch Intern Med. 2000;160:1977–1989. doi: 10.1001/archinte.160.13.1977. [DOI] [PubMed] [Google Scholar]
- 55.Canagasaby A, Vinson DC. Screening for hazardous or harmful drinking using one or two quantity to frequency questions. Alcohol Alcohol. 2005;40(3):208–213. doi: 10.1093/alcalc/agh156. [DOI] [PubMed] [Google Scholar]
- 56.Beich A, Gannik D, Malterud K. Screening and brief intervention for excessive alcohol use: qualitative interview study of the experiences of general practitioners. BMJ. 2002;325:870. doi: 10.1136/bmj.325.7369.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Beich A, Thorsen T, Rollnick S. Screening in brief intervention trials targeting excessive drinkers in general practice: systematic review and meta-analysis. BMJ. 2003;327:536–542. doi: 10.1136/bmj.327.7414.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Phelps GL, Johnson NP. Bright light in dark places: physician recognition of alcoholism. JSC Med Assoc. 1990;86:17–18. [PubMed] [Google Scholar]
- 59.Kriston L, Holzel L, Welser A-K, et al. Meta-analysis: are 3 questions enough to detect unhealthy alcohol use? Ann Intern Med. 2008;149:879–888. doi: 10.7326/0003-4819-149-12-200812160-00007. [DOI] [PubMed] [Google Scholar]
- 60.Hodgson R, Alwyn T, John B, et al. The Fast Alcohol Screening Test. Alcohol Alcohol. 2002;37(1):61–66. doi: 10.1093/alcalc/37.1.61. [DOI] [PubMed] [Google Scholar]
- 61.Hoeksema HL, De Bock GH. The value of laboratory tests for the screening and recognition of alcohol abuse in primary care patients. J Fam Pract. 1993;37(3):268–276. [PubMed] [Google Scholar]
- 62.Reynaud M, Schwan R, Loiseaux-Meunier M-N, et al. Patients admitted to emergency services for drunkenness: moderate alcohol users or harmful drinkers? Am J Psychiatry. 2001;158:96–99. doi: 10.1176/appi.ajp.158.1.96. [DOI] [PubMed] [Google Scholar]
- 63.Raistrick D, Heather N, Godfrey C. Review of the effectiveness of treatment for alcohol problems. London: National Treatment Agency for Substance Misuse; 2006. [Google Scholar]
- 64.Parker AJR, Marshall EJ, Ball DM. Diagnosis and management of alcohol-use disorders. BMJ. 2008;336:496–501. doi: 10.1136/bmj.39483.457708.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Coulton S, Drummond C, James D, et al. for the Stepwice Res Team Opportunistic screening for alcohol-use disorders in primary care: comparative study. BMJ. 2006;332(7540):511–514A. doi: 10.1136/bmj.38743.421574.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mitchell AJ, Vaze A, Rao S. Clinical diagnosis of depression in primary care: a meta-analysis. Lancet. 2009;374(9690):609–619. doi: 10.1016/S0140-6736(09)60879-5. [DOI] [PubMed] [Google Scholar]
- 67.Mitchell AJ, Coyne JC. Do ultra-short screening instruments accurately detect depression in primary care? A pooled analysis and meta-analysis of 22 studies. Br J Gen Pract. 2007;57(535):144–151. [PMC free article] [PubMed] [Google Scholar]
- 68.Kaner EF, Dickinson HO, Beyer FR, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007;2:CD004148. doi: 10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- 69.Aalto M, Hyvönen S, Seppä K. Do primary care physicians’ own AUDIT scores predict their use of brief alcohol intervention? A cross-sectional survey. Drug Alcohol Depen. 2006;83(2):169–173. doi: 10.1016/j.drugalcdep.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 70.Aira M, Kauhanen J, Larivaara P, Rautio P. Differences in brief interventions on excessive drinking and smoking by primary care physicians: qualitative study. Prev Med. 2004;38(4):473–478. doi: 10.1016/j.ypmed.2003.11.023. [DOI] [PubMed] [Google Scholar]
- 71.Seale JP, Guyinn MR, Matthews M, et al. Vital signs screening for alcohol misuse in a rural primary care clinic: A feasibility study. Journal of Rural Health. 2008;24(2):133–135. doi: 10.1111/j.1748-0361.2008.00149.x. [DOI] [PubMed] [Google Scholar]