Abstract
Objective: The purpose of this study was to evaluate the managemant results of patients with penetrating abdominal injuries. Material and Methods: One hundred twenty (120) patients who were admitted to the Emergency Department of Haydarpasa Numune Training and Research Hospital between December 2003 and December 2010 with abdominal stab wounds were included to retrospective study. The data of all patients regarding age, gender, FAST and CT results, injured organs, surgical procedures, length of hospital stay, follow-up were examined. USG findings were classified as follows: true positive (TP), in cases of positive USG findings, and positive laparotomy; true negative (TN), in cases of negative USG findings, and negative physical examination and follow-up findings; false negative (FN), in cases of negative USG findings, and positive laparotomy; and false positive (FP), in cases of positive USG findings, and negative physical examination and follow-up findings. Abdominopelvic CT extended from the lower chest to the symphysis pubis. CT was performed by administering radiopaque agents via intravenous (i.v.) rectal or oral route. Results: One hundred twenty (120) patients who were admitted to the Emergency Department of Haydarpasa Numune Training and Research Hospital between December 2003 and December 2010 with stab abdominal injuries were hospitalized. According to USG findings, 45.7% were TP, 82.4% were TN, 10.6% were FN, and 34.3% were FP. Thirty-five patients with hemodynamic stability and positive FAST findings and 15 patients with positive hemodynamic stability but negative FAST findings underwent computed tomography. Conclusion: Serial FAST and CT help guide treatment for stable patients with penetrating sharp injuries to the abdomen.
Keywords: Stab wound, FAST, computed tomography
Introduction
Penetrating abdominal injuries may cause considerable troubles at emergency service. The rate of non-therapeutic or negative laparotomy has been reported to be approximately 30% if routine laparotomy is performed in all penetrating injuries [1,2]. Morbidity rates range from 3%-16% in negative laparotomy cases. Therefore, the selective approach has been used in most centers instead of emergency laparotomy [3,4]. Focused Assessment with Sonography in Trauma (FAST) patient has been introduced for this purpose. FAST is widely used as it is inexpensive, portable, non-invasive, highly sensitive, frequently repeatable due to not involving x-rays, easily applied by surgeons and enables a rapid response in about 4-5 minutes [5-8]. Computed tomography (CT) has an important place in detection of the injuries in solid organs such as liver, kidney and spleen as well as in monitoring of hemodynamically stable patients [9,10]. CT remains the radiologic standart for investigating the injured abdomen but requires patient transfer and inevitable delay (bowel preparation) and is unsuitable for patients who are clinically unstable [11].
The aim of this study was to investigate the use of computed tomography (CT) and focused assessment with sonography for trauma (FAST) for the initial assessment of penetrating abdominal injuries.
Materials and methods
One hundred twenty patients who were admitted to the Emergency Department of Haydarpasa Numune Training and Research Hospital between December 2003 and December 2010 with abdominal stab wounds were included to retrospective study. The data of all patients regarding age, gender, FAST and CT results, surgical procedures, injured organs, length of hospital stay, follow-up were examined. Initial resuscitation measures were applied to all patients including tetanus and antibiotic prophylaxis. All wounds were explorated under local anaesthesia for penetration into the intraabdominal cavity. Hemodinamic instability and overt peritoneal irritation signs were accepted as definite indications for laparotomy.
FAST was performed by a General Electric Logic 200 device using a 3.5 Megahertz abdominal probe. The presence of free fluid in the perihepatic area (which includes the Morrison pouch), perisplenic region (which includes the splenorenal recess), paracolic gutters and cul-de-sac space were considered as positive FAST. The contrast enhanced spiral CT of the abdomen and pelvis was performed to further evaluate the extent of solid organ and/or bowel injury in FAST + patients. CT was performed by administering radiopaque agents via intravenous (i.v.) rectal or oral route. Patients with normal CT results were followed-up and the patients with surgical pathology in CT underwent laparotomy. Hemodynamically stable FAST (-) patients without peritoneal irritation signs were followed-up. Whereas patients with suspicious peritoneal irritation signs were evaluated with abdominopelvic CT. Negative laparotomy was defined as any surgical exploration without intraabdominal organ injury. On the other hand, non-therapeutic laparotomy was considered in injuries and bleeding lesions of the rectus muscle, omentum, or solid and hollow viscus organs which did not cause any hemodynamic instability or peritonitis.
Statistical analyses were performed using Number Cruncher Statistical System (NCSS) 2007 & PASS 2008 statistical software (Keysville, UT, USA. Qualitative data were compared by a Chi-square test and Fisher’s Exact test. A statistical significance level was accepted as a p<0.05.
Results
Of 120 patients, 109 (90.8%) were men and 11 (9.2%) were women. The mean age was 29.75 ± 10.89 years. Eighty-two patients (68.3%) were followed-up without surgery. The reasons for surgery were acute abdomen in 29 patients (24.1%), and hemorrhage in 9 patients (7.6%). The mean time until surgery was 37 ± 10.30 hours.
The small intestines were the most commonly injured hollow organs (35.7%), while the liver was the most commonly injured solid organ (28.5%) in the gastrointestinal system. The injured organs according to surgical findings are presented in Figure 1. According to USG findings, 45.7% were TP, 82.4% were TN, 10.6% were FN, and 34.3% were FP.
Figure 1.
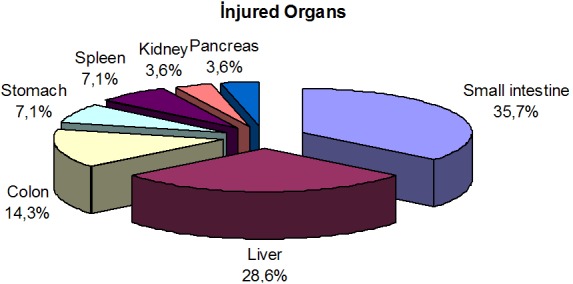
Distribution of organ injuries according to surgical findings.
The median length of hospital stay was found 5 (Range: 0-13) days in surgical treatment group. It was 3 (Range: 1-10) days in follow-up without surgery group. It was stastically high in surgically treated group (p=0.001).
A comparison of the length of hospital stay according to surgical treatment and follow-up without surgery is presented in Table 1. Conservative follow-up without surgery rates in patients with no pathologic findings on USG were significantly higher with pathologic findings on USG (p=0.001). In other words, it is more likely that the patients are follow-up without undergoing an operation if USG findings are normal. There was no statistically significant difference between negative (n=7, 13.3%) and non-therapeutic laparotomy (n=6, 13.6%) rates in the two groups based on USG findings (p=0.059). It was not possible to lower negative laparotomy or non-therapeutic laparotomy rates through the use of USG. There was a statistically significant difference between pathology requiring surgery rates according to USG findings (p=0.001). The rate of detecting pathology requiring surgery in patients with no pathologic findings on USG was significantly lower compared to other group Table 2.
Table 1.
Comparison of length of hospital stays
| Surgical treatment | Length of hospital stay (day) | p | |
|---|---|---|---|
|
| |||
| Median | Min-Mak | ||
| Follow-up without surgery (n=82) | 3 | 1-10 | 0.001* |
| Surgical treatment (n=38) | 5 | 0-13 | |
Mann Whitney U test p<0.01.
Table 2.
Comparison of treatment alternatives in patients evaluated by USG
| No pathologic findings on USG (n=85) | Pathologic findings on USG (n=35) | P | |
|---|---|---|---|
|
| |||
| n (%) | n (%) | ||
| Follow-up | 70 (82.4) | 12 (34.3) | 0.001* |
| Negative laparotomy | 4 (4.7) | 3 (8.6) | +0.415 |
| Non-therapeutic laparotomy | 2 (2.4) | 4 (11.4) | +0.059 |
| Negative + non-therapeutic laparotomy | 6 (7.1) | 7 (20.0) | +0.053 |
| Pathology requiring surgery | 9 (10.6) | 16 (45.7) | 0.001* |
Chi-square test.
Fisher’s Exact test.
p<0.01.
Emergency CT was performed in 50 patients. Hemodynamically stable FAST (+) 35 patients (29.1%) underwent CT. CT result returned normal in 12 patients (34.2%) who were put on follow-up programme. 23 patients (65.6%) with positive CT findings and whose peritoneal irritation findings were suspicious, underwent surgery and 16 patients (45.7%) required surgery. Hemodynamically stable FAST (-) patients were put on follow-up and 15 of the patients underwent CT. They underwent an operation upon obtaining positive results on CT. 9 of these patients (10.6%) required surgery.
Discussion
Approximately 10% of all trauma-related deaths occur as a result of blunt or penetrating abdominal injuries [12]. The fact that these deaths can be prevented by early diagnosis and appropriate and rapid treatment increases the significance of this subject. Because the likelihood of visceral injuries is over 90% in abdominal gunshot injuries, laparotomy is inevitable. There is no doubt about the necessity of emergency laparotomy in patients with signs of hemodynamic instability or peritoneal irritation following penetrating injuries [13-15]. Surgeons find it challenging to define the indications for laparotomy in individuals who are asymptomatic or who present minimal symptoms following suspicious penetrating abdominal injuries. Several methods can be used to aid in diagnosis. FAST is a helpful diagnostic tool which is frequently used in the selective approach to prevent negative and non-therapeutic surgical procedures [16]. FAST was initially started in Europe and Japan in the eighties to be adopted by North America in the early nineties. From there it has spread worldwide.
FAST is a goal directed study answering a simple question as to whether there is intraperitoneal fluid or not [17]. A rapid, portable and reliable method of screening these patients is desired. Results of the current study demonstrate that focused abdominal US is sensitive (94%), specific (98%), and accurate (95%) for detecting hemiperitoneum [11]. FAST has had a significant effect in the management of abdominal trauma, with its ease of rapid performance, portability, and noninvasive nature, resulting in a significant increase in its use over the past 2 decades [18].
The likelihood of follow-up without surgery was high (89.5%) when there were no pathologic findings on USG. The specificity of USG was reported to be 94% in the study conducted by Udobi et al [1]. and 98% in the study by Boulanger et al. However, it should be noted that high specificities may be associated with the fact that gunshot injuries and penetrating injuries have been classified within the same category in these studies. The FP rate of the present study (34.3%; absence of surgical pathology in the presence of pathologic findings on USG) was lower than the previous studies. This rate was reported to be 46% in the series of Udobi et al. 67% in the series of Boulanger et al [19] and 48% in the series of Soffer et al [2]. Theoretically, FP rate would be expected to increase the non-therapeutic surgery rate. In the present study, the decision of surgery was based on physical examination, laboratory findings, and other imaging methods together with USG.
In patients with free fluid or with solid organ injury, CT is used to perform further investigation and to evaluate the injuries if the patients are hemodynamically stable. Although it provides more accurate and clear results, it has the disadvantages of patients transfer, lack of active resuscitation and irradiation. Hemodynamically stable trauma patients with negative results on ultrasonography should undergo control CT scanning that involves more detailed examination along with clinical follow-up in order to confirm the absence of any injury [20,21]. It must be kept in mind that solid organ injuries may not manifest with free fluid within the abdominal cavity [22].
CT is preferred over USG by some of the centers due to the fact that it provides more accurate results about the degree and margins of the injuries. It has an important place in detection of the injuries in solid organs such as liver, kidney and spleen as well as in follow-up of hemodynamically stable patients. Besides, arterial-venous phase images of the solid organs can be obtained and hollow organ perforations can be detected by searching for extravasation of the opaque substance from the organ lumen after administering radiopaque agent from either oral or intravenous (and even rectal) route [23]. Hemodynamically stable or stabilized patients by fluid resuscitation with positive findings on USG should undergo control CT scans. USG should be preferred if an emergency surgical intervention is required, in other words, if there is penetrating injury accompanied by hypotension and if there is no sufficient time to perform CT.
Complications can be serious in negative laparotomy. While mortality rates range from 0%-6%, complication rates have been reported as 5%-22% [24]. The negative laparotomy rate has been reported as 12% and the non-therapeutic laparotomy rate as 23% in studies in which exploration has been performed on a routine basis, whereas these rates have been reduced to 7% for negative laparotomy and to 4% for non-therapeutic laparotomy after the implementation of selective approaches in routine practice. In a penetrating thoracoabdominal stabbing injury series involving 117 patients, Taviloglu et al [23] reported non-therapeutic laparotomy rate as 12%, and negative laparotomy rate as 0%. In the present study, these rates were 5.8% and 5%, respectively.
It was noted in the present study that pathology requiring surgery was present in 9 (10.6%) patients without any pathologic findings on USG. If these patients had only been evaluated by USG, pathologies requiring surgery would not have been diagnosed in a timely manner.
In general, the results of FAST will depend on three factors: the ultrasound machine, the patient and the operator. USG, a subjective diagnostic method, depends on the experience of the medical staff and undoubtedly changes the results. Failure of USG to detect clinically significant pathologies, particularly in intestinal injuries in the early period, is well-known [24,25]. FAST, a procees intended for the liquid material, may not be able to define the injures (diaphragmatic or hollow viscus injury) whether hemiperitoneum not going to develop or not yet developed. In penetrating injuries, the small intestine and colon, which are hollow organs, and the liver, which is a solid organ with the widest anterior part are the most susceptible organs to injury. In the present study, the small intestine and colon were the most frequently injured hollow organs (10 patients [35.7%] and 4 patients [14.2%], respectively), and the liver was the most frequently injured solid organ (8 patients [28.4%]). In the present study, significantly shorter length of hospital stay in patients who were conservatively followed-up without surgical intervention compared to those who underwent surgery (p<0.01) supports the selective approach.
In conclusion, we suggest that USG is a useful diagnostic tool for the surgeon to determine the appropriate treatment alternative in penetrating abdominal injury. The likelihood of conservative follow-up without surgery is high in the case of normal USG findings. FAST can be a useful initial diagnostic study after penetrating abdominal trauma. A positive FAST is a strong predictor of injury, and patients should proceed directly to laparotomy. If FAST is negative, additional diagnostic studies like CT should be performed to rule out occult injury. In the emergency room setting, although FAST examination might be the first choice in patients with penetrating abdominal trauma, CT may be the second choice for further investigation in the case of clinical suspicion.
Disclosure of conflict of interest
None.
References
- 1.Udobi KF, Rodriguez A, Chiu WC, Scalea TM. Role of ultrasonography in penetrating abdominal trauma: A prospective clinical study. J Trauma. 2001;50:475–479. doi: 10.1097/00005373-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Soffer D, McKenney MG, Cohn S, Garcia-Roca R, Namias N, Schulman C, Lynn M, Lopez P. A prospective evaluation of ultrasonography for the diagnosis of penetrating torso injury. J Trauma. 2004;56:953–959. doi: 10.1097/01.ta.0000127806.39852.4e. [DOI] [PubMed] [Google Scholar]
- 3.Sirinek KR, Page CP, Root HD. Is exploratory celiotomy necessary for all patients with truncal stab wounds? Arch Surg. 1990;125:844–848. doi: 10.1001/archsurg.1990.01410190036006. [DOI] [PubMed] [Google Scholar]
- 4.Demetriades D, Vandenbassche P, Ritz M. Non-therapeutic operations for penetrating trauma: early morbidity and mortality. Br J Surg. 1993;80:860–861. doi: 10.1002/bjs.1800800716. [DOI] [PubMed] [Google Scholar]
- 5.Bokhari F, Nagy K, Roberts R, Brakenridge S, Smith R, Joseph K, An G, Barrett J. The ultrasound screen for penetrating truncal trauma. Am Surg. 2004;70:316–320. [PubMed] [Google Scholar]
- 6.Buzio M, Bertello A, Bau G, Mao P. Ultrasound in trauma (FAST) Minerva Chir. 2000;55:89–95. [PubMed] [Google Scholar]
- 7.Tsui CL, Fung HT, Chung KL, Kam CW. Focused abdominal sonography for trauma in the emergency department for blunt abdominal trauma. Int J Emerg Med. 2008;1:183–187. doi: 10.1007/s12245-008-0050-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bodge PJ, Edwards MJR, Kruit MC, van Vugt AB. Sonography in a clinical algorithm for early evaluation of 1671 patients with blunt abdominal trauma. AJR. 1999;172:905–910. doi: 10.2214/ajr.172.4.10587119. [DOI] [PubMed] [Google Scholar]
- 9.Mircelal K, Özer M, Özgür F, Barış G, Taylan S, Gökhan İ. Diagnostic peritoneal lavage; is it really an obituary. Ege Tip Dergisi. 2007;46:33–36. [Google Scholar]
- 10.Oguz B. Abdomimal Traumas. Turkiye Klinikleri J Radiol-Special Topics. 2011;4:151–62. [Google Scholar]
- 11.Lingawi SS, Buckley AR. Focused Abdominal US in Patients with Trauma. Radiology. 2000;217:426–429. doi: 10.1148/radiology.217.2.r00nv23426. [DOI] [PubMed] [Google Scholar]
- 12.Ertekin C, Taviloglu K, Guloglu R, Kurtoglu M. Travma 1. Baski: Istanbul Medikal Yayincilik Ltd Sti.; 1995. Abdominal injury; pp. 875–885. Bolum 16. [Google Scholar]
- 13.Topaloglu U. Approach to patients with multiple trauma. The Medical Journal of Haydarpasa Numune Training and Research Hospital. 2005;45:100–106. [Google Scholar]
- 14.Como JJ, Bokhari F, Chiu WC, Duane TM, Holevar MR, Tandoh MA, Ivatury RR, Scalea TM. Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma. 2010;68:721–33. doi: 10.1097/TA.0b013e3181cf7d07. [DOI] [PubMed] [Google Scholar]
- 15.Biffl WL, Moore EE. Management guidelines for penetrating abdominal trauma. Curr Opin Crit Care. 2010;16:609–617. doi: 10.1097/MCC.0b013e32833f52d2. [DOI] [PubMed] [Google Scholar]
- 16.Dittrich K, Abu-Zidan FM. Role of Ultrasound in Mass-Caualty Situations. Int J Disaster Med. 2004;2:18–23. [Google Scholar]
- 17.Radwan MM, Abu-Zidan FM. Focused Assessment Sonograph Trauma (FAST) and CT scan in blunt abdominal trauma: surgeon’s perspective. Afr Health Sci. 2006;6:187–190. doi: 10.5555/afhs.2006.6.3.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel NY, Riherd JM. Focused Assessment with Sonography for Trauma: Methods, Accuracy, and Indications. Surg Clin N Am. 2011;91:195–207. doi: 10.1016/j.suc.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 19.Boulanger BR, Kearnery PA, Tsuei B, Ochoa JB. The routine use of sonography in penetrating torso injury is beneficial. J Trauma. 2001;51:320–325. doi: 10.1097/00005373-200108000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Aydin U, Yazici P, Uguz A, Tamsel S, Solak İ, Kaplan H. Comprasion the results of ultrasonography with computed tomography of traumatized patients. Yeni Tip Dergisi. 2008;25:36–39. [Google Scholar]
- 21.Rhea JT, Gardza DH, Novelline RA. Controversies in emergency radiology; CT versus ultrasound in the evaluation of blunt abdominal trauma. Emerg Radiol. 2004;10:289–295. doi: 10.1007/s10140-004-0337-4. [DOI] [PubMed] [Google Scholar]
- 22.Leppaniemi A, Salo J, Haapiainen R. Complications of negative laparotomy for truncal stab wounds. J Trauma. 1995;38:54–58. doi: 10.1097/00005373-199501000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Taviloglu K, Gunay K, Ertekin C. Abdominal stab wounds: the role of selective management. Eur J Surgery. 1998;164:17–21. doi: 10.1080/110241598750004904. [DOI] [PubMed] [Google Scholar]
- 24.Freeman P. The role of ultrasound in the assessment of the trauma patient. Aust J Rural Health. 1999;7:85–89. doi: 10.1046/j.1440-1584.1999.00233.x. [DOI] [PubMed] [Google Scholar]
- 25.Smith J. Focused assessment with sonography in trauma (FAST): should its role be reconsidered? Postgrad Med J. 2010;86:285–291. doi: 10.1136/pgmj.2008.076711. [DOI] [PubMed] [Google Scholar]


