Abstract
Chronobiology is the study of biological rhythms. Chronomics investigates interactions with environmental cycles in a genetically coded autoresonance of the biosphere with wrangling space and terrestrial weather. Analytical global and local methods applied to human blood pressure records of around-the-clock measurements covering decades detect physiological-physical interactions, a small yet measurable response to solar and terrestrial magnetism. The chronobiological and chronomic interpretation of ambulatory blood pressure monitoring (C-ABPM) records in the light of time-specified reference values derived from healthy peers matched by sex and age identify vascular variability anomalies (VVAs) for an assessment of cardio-, cerebro-, and renovascular disease risk. Even within the conventionally accepted normal range, VVAs have been associated with a statistically significant increase in risk. Long-term C-ABPM records help to “know ourselves,” serving for relief of psychological and other strain once transient VVAs are linked to the source of a load, prompting adjustment of one's lifestyle for strain reduction. Persistent circadian VVAs can be treated, sometimes by no more than a change in timing of the daily administration of antihypertensive medication. Circadian VVA assessment is an emergency worldwide, prompted in the United States by 1,000 deaths per day every day from problems related to blood pressure. While some heads of state met under United Nation and World Health Organization sponsorship to declare that noncommunicable diseases are a slow-motion disaster, a resolution has been drafted to propose C-ABPM as an added tool complementing purely physical environmental monitoring to contribute also to the understanding of social and natural as well as personal cataclysms.
Keywords: blood pressure, chronomics, coperiodism, combined global and local analyses, space-terrestrial weather, vascular variability anomaly
this article is part of a collection on Pathophysiology of Hypertension. Other articles appearing in this collection, as well as a full archive of all collections, can be found online at http://ajpheart.physiology.org/.
Two meetings in September 2011 assembled heads of state, one in New York, sponsored by the United Nations and World Health Organization; the other in Istanbul, prompted by GEOCHANGE (www.2011.geocataclysm.org). The former in New York assigned highest priority to noncommunicable disease, in the words of Margaret Chan, World Health Organization Director General, a “slow-motion disaster” (58; cf. 4). In opening the other conference in Istanbul (http://www.2011.geocataclysm.org/), one of the undersigned (F. Halberg) advocated an international website with a system for automatic, affordable, unobtrusive, chronobiological, and chronomic interpretation of ambulatory blood pressure monitoring (C-ABPM) for the same purpose of stroke and other severe noncommunicable disease prevention (46; see pp. 23–31). He and a team of the project on the biosphere and the cosmos (BIOCOS) also presented data using C-ABPM to better understand biospheric harbingers of natural disasters and social conflicts, all sharing cycles with the human brain and heart (32). In the United States alone, 1,000 deaths every day are attributed to problems related to undiagnosed/untreated blood pressure abnormalities (26, 66).
Only 100 deaths due to faulty tires (not 1,000 deaths per day) were required to prompt President Clinton to sign the Transportation Recall Enhancement, Accountability, and Documentation (TREAD) Act, so that today we monitor pressure in car tires and put a notice on the dashboard when needed, reminding the driver to check tire pressure. But we do not require similar health monitoring of ourselves, even when it is practical.
The Center for Disease Control (CDC) of the United States estimated blood pressure-related annual cost at $131 billion (26, 66; cf. 57) out of $200 billion for heart disease with an as-yet unaccounted part of the $1.5 trillion annual cost for chronic disease (1). Heads of state could set a high priority on reducing the number of 1,000 deaths/day and the associated cost in the United States alone and mounting worldwide by making C-ABPM widely available. Indeed, not only can C-ABPM guide the timed treatment of vascular variability anomalies (VVAs), harbingers, and possibly reversible causes of stroke (brain attack) and cardiac disease (heart attack), its time structure is intimately related to the human brain for its various behaviors (11, 31), a focus of President Obama's plans.
Status Quo
Whether or not magnetic storms may trigger myocardial infarctions (16, 30) and may shield against sudden cardiac deaths (19), the effects of space weather have long been recognized. Calls for action to control them have been rewarded with the offer of a Nobel Prize (refused under political pressure) to Alexander Leonidovich Chijevskiy (6). Magnetically compensated shielded hospital rooms with local recording were again proposed (unsuccessfully) half a century ago by the undersigned with the late Frederic C. Bartter, then head of the Hypertension-Endocrine Branch at the United States National Institutes of Health, to the clinical center at the National Institutes of Health, which Bartter subsequently directed.
Investigating the heart's dependence on the brain and the cosmos, Abdullah al-Abdulgader and Rollin McCraty have built a geomagnetic monitoring station in the former's estate (Global Coherence Initiative Monitoring Site 2) (43). Their aim is to eventually analyze interactions with the human circulation with magnetic and perhaps other nonphotic cycles, such as gravitational waves. Such an overdue station could be extended by shielded hospital beds (and toilets) (7) to help elucidate the role of the nonphotic environmental cycles in the dynamics of the human heart and brain (43). Looking beyond circulation and physiology in general, competing space and terrestrial weather affect all human affairs studied thus far.
Studies can build in the steps of Vladimir Ivanovich Vernadsky's noosphere (from noös or nous, the Greek word for “mind”) (2, 64, 65), assessing it for each individual as well as for the figurative human mind as an entity encompassing the whole evolving biosphere. By the mapping of a spectrum of cycles into a time-structured chrono-noosphere (or rather briefly chronousphere), Vernadsky's temporally unstructured vision gains a time frame. In it, personalized chronouspheres (obtained by every individual's self-surveillance) contribute at least their share of magnetism to an accumulating generalized chronousphere, where thus far only relatively few individuals' contributions changed the crust of the earth. Chijevskiy already reported many signatures in the biosphere of an about 11-year sunspot cycle (6–9). To his contributions and those of Vallot, Faure, and Sardou, followed up by those of Suitbert Ertel (23–25), our era of computers, satellites, genetics, inferential statistics, and chronomics added transdisciplinary mutually validating coperiodisms.
A novel polydisciplinary spectrum recognizes Chijevskiy's “echo” (of the sun) as a partly built-into-the-biosphere autoresonance, with competing earth and space weather, where “auto” denotes the long-term persistence of a component in humans and their affairs in the absence of the environmental counterpart (20, 32, 34, 35, 37). Today, we recognize more cycles than Chijevskiy found in Vernadsky's spatially genetically (but not yet temporally chronomically) structured noosphere.
A chronousphere starts with “knowing yourself” by self-surveillance and learning about the dynamics that take place within the physiological range that can no longer be equated to random or trivial variation once the lawful variability is quantified. Equally, using a target blood pressure under which values are acceptable becomes untenable, preferably replaced by the diagnosis of VVAs (Figs. 1 and 2). In keeping with our cyber age, we here present a set of global and local displays that, for a given variable, constitute both a running history and a status quo, automatically flagging down abnormality in a number of cycles of different length, documented to relate to the cardiovascular system in clinical health and disease.
Fig. 1.
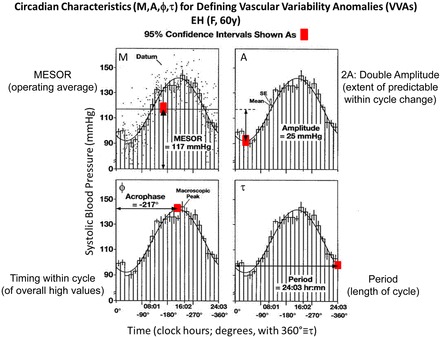
Data from a clinically healthy woman collected for 7 days are stacked over a single cycle, its period estimated as 24.03 h by nonlinear least squares. A circadian rhythm is visible to the naked eye, its characteristics illustrated with their 95% confidence intervals (CIs). The midline-estimating statistic of rhythm [MESOR (M); top left] is a rhythm-adjusted mean. The amplitude (top right) is half the predictable extent of change within a cycle. The acrophase (bottom left) is a measure of the timing of overall high values recurring in each cycle. The period (bottom right) is the duration of one cycle. VVAs, Vascular Variability Anomalies.
Fig. 2.
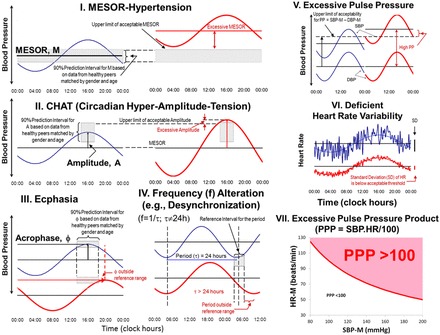
Definitions of some VVAs: MESOR-hypertension (MH; top, left, and middle) is an elevation of the blood pressure MESOR above the upper 95% prediction limits of clinically healthy peers matched by sex and age; circadian hyper-amplitude-tension (CHAT; middle left, and middle) is an elevation of the 24-h amplitude of blood pressure above the upper 95% prediction limit of clinically healthy peers matched by sex and age; ecphasia (bottom left) is a deviation of the 24-h acrophase from the 90% prediction limits of clinically healthy peers matched by sex and age; ecfrequentia (bottom middle) is a statistically significant deviation of the period from 24 h, assessed by the nonoverlap of 24 h by the 95% CI of the period assessed by nonlinear least squares; excessive pulse pressure (PP; top right) is a difference of MESORs of systolic and diastolic blood pressure [SBP (S) and DBP (D), respectively] larger than 60 mmHg (until it can be further qualified in terms of sex and age); deficient heart rate (HR) variability (middle right) is a (7 day) standard deviation of HR below 7.5 beats/min (until it can be further qualified in terms of sex and age); and excessive PP product (PPP; bottom right) is a product of the MESORs of SBP and HR (/100) larger than 100 mmHg·beats·min−1/100 (until it can be further qualified in terms of sex and age). These VVAs can occur while most, if not all data, lie within the conventional physiological range. Their presence has been associated with an increased risk of adverse cardiovascular events in several outcome studies.
Subjects and Methods
Longitudinal records of self-measurements and of around-the-clock automatically assessed blood pressure and heart rate data by ambulatory monitoring are analyzed by the extended cosinor (13, 29, 56). In both kinds of data, nonlinear least squares detect and estimate components with long periods with their uncertainties (42). When aligned with environmental periods, some shared coperiodisms are found with solar wind speed, among others. Graded local views in spectrograms, with the length of the moving interval used for analysis varied systematically, reveal the variability in both period and prominence as a function of time (Fig. 3). Gliding spectra, using a fixed interval length, visualize the extent of variability, whereas their combined global spectra identify overall cycles (11, 31). Sphygmochrons (computer summaries reporting complementary results from both curve fitting and stacking, e.g., over an idealized 24-h day) detect VVAs, that is, abnormal patterns of the circadian rhythm of blood pressure and heart rate in the light of time-specified reference values qualified by sex and age (13, 36) that await extension to extracircadian components. Alterations in the variability of blood pressure and heart rate along the circadian scale are known as VVAs or, if they persist, as vascular variability disorders (VVDs) (Fig. 2). Table 1 provides information about some of the longest data series investigated, discussed in detail elsewhere (32, 34).
Fig. 3.

SBP self-measured 5 to 6 times a day between 1967 and 2012 by a clinically healthy man (R.B.S.) is analyzed by spectrograms using a systematically varied interval length (between 4 and 24 yr). In the frequency range investigated, the circannual component is the most prominent one. Analysis by J. Czaplicki.
Table 1.
Characteristics of some of the records analyzed*
| Subject | Sex | Start | End | Length, yr | Age at Start, yr | N of Data | Variables |
|---|---|---|---|---|---|---|---|
| R.B.S. | M | May 1967 | Dec 2012 | 45.6 | 20.5 | 75,100 | BP, HR, others |
| M.I.S. | W | Feb 1984 | Nov 2003 | 19.7 | 66.7 | ∼13,000 | BP, HR |
| S.B.S. | M | Feb 1984 | Nov 2012 | 28.8 | 64.5 | ∼17,000 | BP, HR |
| Y.W. | M | Aug 1987 | Jan 2011 | 32.4 | 34.7 | 244,000 | BP, HR |
| E.H. | M | Apr 1965 | Feb 1981 | 15.8 | 38.6 | BP, HR, others | |
| J.F. | W | Jun 2009 | Mar 2011 | 1.7 | 61.3 | 10,500 | BP, HR, others |
| F.H. | M | Jul 1987 | Jan 2013 | 25.5 | 68.0 | 224,000 | BP, HR |
| O.S. | W | Jan 2005 | Sep 2005 | 0.7 | 82.6 | 8,800 | BP, HR |
| G.C. | W | Jul 1987 | Oct 2011 | 24.2 | 37.6 | 170,000 | BP, HR |
| G.S.K. | M | Mar 1998 | Jan 2013 | 14.8 | 72 | 210,700 | BP, HR |
| W.R.B. | M | May 1974 | Dec 2009 | 35.5 | 51.8 | 931 | BP, HR, other |
| J.C. | M | Feb 1990 | Mar 1993 | 3.1 | 23.3 | 26,000 | Sleep-wake |
The techniques described here form the basis of an addition to our health-care system that serves to improve individuals' physiological health as well as psychological well-being. They lead to broader findings on how systolic blood pressure can be a proxy for mental functions and their association with the Earth's or the Sun's magnetism. By odds ratios for the number of shared frequencies between psychophysiology and physics, mental functions more than match the (in physics) well-accepted association of Earth and Sun magnetism to each other (11, 31, 32, 34). As we have documented, the chronobiological viewpoint complements in time the understanding of how things work in space that we gain by mapping the genome or brain activity. Hence, in parallel with currently more popular studies, the critical importance of continuing time structural research should be realized. A dimension that yields predictably opposite effects at specifiable times, such as survival versus death as a function only of timing (22, 39), must be quantified, unless it may become a source of blunders.
Results
Decades-long surveillance (20, 32–34, 36, 37, 46: see pp. 23–31 & 228–346) opens a perspective of novel periods (Fig. 4). For practice, we recommend universal screening, to start with by the sphygmochron (13, 33, 36), now already amplified by further circadian displays, with different resolution, i.e., with different intervals analyzed as one goes. Extracircadian as well as circadian features in (preferably automatic) imaging for self-help are assessed from week to week and from year to year. Longer interval imaging of a broader spectral range (with wider ordinates) will have to explore the extracircadian range and prompt a physical examination by alterations in the weekly or longer profile. Appropriate infradian standards of reference will have to be collected to complement improved circadian reference values, a long task ahead.
Fig. 4.
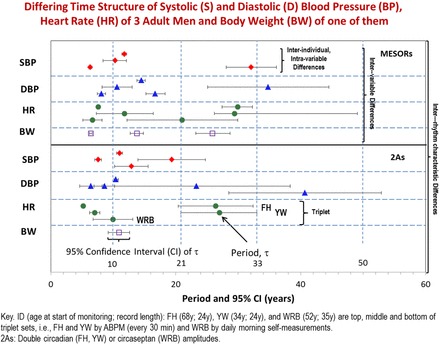
Decades-long self-measurements in the morning by an elderly man (W.R.B.) complement around-the-clock monitoring at half-hour intervals by two other men (F.H. and Y.W.). These data further open a perspective of cycles replacing or complementing trends with age and revealing a selective assortment of periods in a given variable, among variables, and among individuals. BP, blood pressure; BW, body weight.
Thomas R. Frieden, director of the CDC, briefed the media on September 5, 2012, calling uncontrolled blood pressure “public health enemy No. 2, second only to tobacco in the number of potentially preventable deaths associated with it annually” (http://www.cbsnews.com/8301–504763_162–57506364-10391704/cdc-one-third-of-u.s-adults-have-high-blood-pressure-only-half-have-it-under-control/). Frieden refers to 5.7 million Americans who were aware of their high blood pressure but were not being treated and to 14.1 million who were not aware of their hypertension (26, 66). These numbers and the estimated ∼35.8 million whose known condition is uncontrolled are all dwarfed, once we realize that high blood pressure is but one of several VVAs or VVDs, and that most of the other VVAs (or VVDs) are undiagnosed, notably when they involve variability in the normal range. One such VVA is circadian hyper-amplitude-tension (CHAT), a condition characterized by too large a circadian amplitude of blood pressure. Screening for alterations of circadian (and in the future probably other) blood pressure patterns, in the form of VVAs and VVDs, render public health enemy No. 2, the status quo dealing with blood pressure, so designated by the CDC (26, 66), into friend No. 1. Their self-detection can prompt the timely institution of intervention for prehabilitation, i.e., to prevent disease and to reduce the cost of rehabilitation. This can be achieved by an educated public and acted upon by the profession as soon as VVDs are diagnosed. Within the business plans of insurance companies, there should be incentive rewards for caregivers using C-ABPM. To deal with the problem, chronobiology shows that VVAs can often be treated, reduced in frequency and/or severity, or eliminated, so that target organ damage can be nipped in the bud (36). There is also indirect evidence suggesting that reducing the circadian amplitude of blood pressure when it is excessive is associated with fewer morbid events (60).
Environmental and physiological variability is resolved as parts of a transdisciplinary spectrum of rhythms, under the influence of extraterrestrial and terrestrial weather, with the former's effects yet to be optimized, after we learn more about them, just as we now heat or air condition to cope with extreme deviations in terrestrial temperature (32, 34, 37). Bacon reportedly compared scientific investigations to a hunt, with findings being the game. Claude Bernard added that a given game may be found “when one is looking for a different animal altogether.” The game to be looked for is former public enemy No. 2, namely VVAs (36) to be converted into friend No. 1. Eventually the surveillance of blood pressure and heart rate could start at birth to prevent now-known severe outcomes of untreated circadian VVAs and to uncover the yet-to-be-described anomalies in extracircadian cycles that are the challenge of the future. Infradians, like circadians, characterize the incidence of myocardial infarctions and sudden cardiac death. Infradians like those mapped in Figs. 3 and 4 (34) matter in the search for quantitative coherence among people (43).
Discussion
A set of global and local displays, including sphygmochrons (13, 36), constitutes a step toward enjoying cyber-aided self-help-based health in a unified time-structured art, science, and noetic well-being. Instead of focusing only on the average blood pressure and heart rate, sphygmochrons also examine the circadian patterns in these variables and compare their characteristics with those of clinically healthy peers matched by sex and age. The circadian rhythm is indeed usually prominent in these variables, as also documented in the experimental laboratory (69).
Abnormalities in the dynamics of blood pressure and heart rate, illustrated in Fig. 2, have been associated with an increased cardiovascular disease risk, even in the absence of an elevated blood pressure [midline-estimating statistic of rhythm-hypertention (MESOR-hypertension)]. Differences in the variability of blood pressure in the absence of a difference in mean value have also been reported in Wistar-Kyoto rats and their hyperactive counterpart with a larger left ventricular mass (21).
As an example, patients with noninsulin-dependent diabetes mellitus who have impaired autonomic nervous function are more likely to show circadian blood pressure ecphasia, a finding also reported in the laboratory (62), where alterations in clock gene expression have been observed (63). Decreased heart rate variability, another VVA, is also a risk factor for coronary artery disease, as also shown in rats after left coronary artery ligation (40). Heart rate variability is of particular interest herein as it has been shown to be decreased in association with magnetic storms (16).
The diagnosis of VVAs could immediately be put into widespread practice. Figure 5 shows what can happen when circadian VVAs are ignored. A set of snapshots in an ongoing self-assessment of a patient after a stroke, who tries to prevent the next one, is provided in Fig. 6.
Fig. 5.
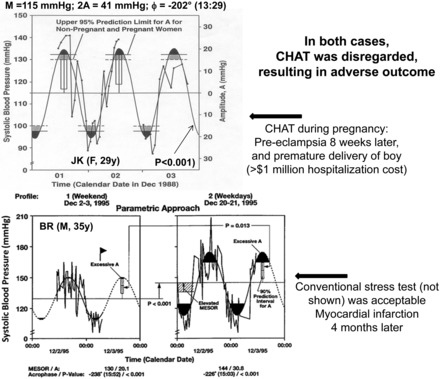
Illustrative examples of predictive value of CHAT. Top: diagnosis of CHAT in the profile of the mother (J.K.) who 8 wk later developed severe preeclampsia and delivered prematurely. The cost of hospitalization of her baby boy topped 1 million dollars during the first year alone. Even when it is associated with an acceptable BP MESOR, CHAT can be a useful warning in pregnant women and in very many others of both sexes. Bottom: weekday (left) vs. workday (right) around-the-clock profiles provide a warning of a high risk of a hard vascular event, which in the case of this 35-year-old man (B.R.) was not accompanied by an abnormal result of a conventional cardiologist's stress test.
Fig. 6.
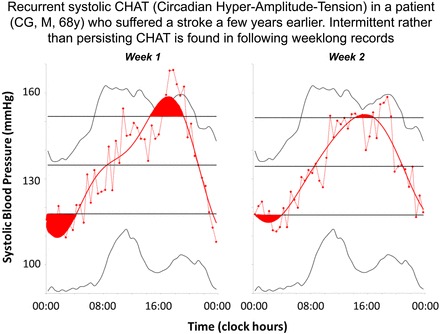
Systolic CHAT is found in 2 consecutive weeklong records of a 68-yr-old man (C.G.) who had suffered a stroke a few years earlier. All parameters were within acceptable limits during the next 3 weeklong records (not shown).
Comments from clinicians in response to results such as those in Figs. 5 and 6 show the impact of thoroughly embedded misconceptions based on insufficient evidence.
With notable exceptions (12, 13, 39, 41, 68), it is generally believed that changing the timing of administration of 24-h formulations should only have minor effects. This is far from the truth. Large clinical trials have shown that the timing of administration of certain antihypertensive drugs matters both in terms of blood pressure lowering and of actual outcomes (41). One should, however, be mindful that a preferred treatment time may, on the average, reduce the incidence of adverse outcomes in a population, but this time is not necessarily optimal for each individual patient. This has been demonstrated recently in a study of 30 patients who have been thoroughly examined after taking the same dose of the same antihypertensive drug, switched among six circadian stages in relation to awakening, each patient remaining on the same regimen for at least 1 month and contributing a 7-day C-ABPM during the last week on that schedule (68). Underlying our recommendation to individualize the optimization by timing of the daily administration of antihypertensive medication is the concept of chronotheranostics, where the timed treatment is adjusted to the chronodiagnosis (14): if a patient has CHAT, treating at a circadian stage when the circadian amplitude of blood pressure is increased even further is likely to be harmful, even if the 24-h average pressure is lowered to a larger extent. This has been demonstrated in a double-blind crossover study that accounts for the difference in actual outcomes from two large clinical trials in Asia (60).
When circadian patterns in blood pressure are discussed, concern is often expressed primarily if not exclusively for “nondippers,” that is for patients who have a day-to-night ratio less than 10%. Nondippers are encouraged to take their medication in the evening, so as to improve a nightly dip. Several outcome studies have all shown that CHAT is associated with a large increase in cardiovascular disease risk (17, 18, 44, 47, 48, 59). There is further evidence that a classification in terms of dipping can fail when a chronobiological diagnosis is predictive (10, 15, 18, 28) (Fig. 7). The fit of a (cosine) model is more powerful for risk assessment than the calculation of a day-to-night ratio, notably since the circadian amplitude and acrophase are also interpreted by cosinor in the light of reference values from clinically healthy peers specified by sex and age. Moreover, underlying the diagnosis of CHAT is the recognition that the relation of the circadian amplitude to cardiovascular disease risk is nonlinear, risk being increased only when the circadian amplitude exceeds a threshold value (for a wide range of amplitudes, there is no change in risk) (17).
Fig. 7.
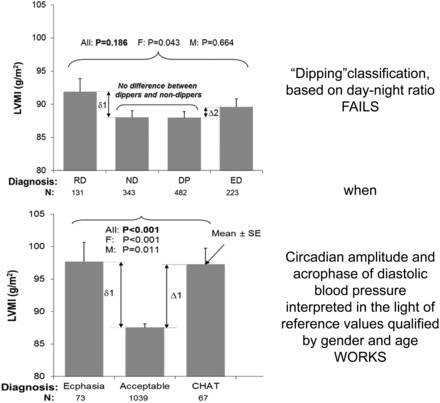
Left ventricular mass index (LVMI), used as a surrogate outcome measure, available from all 1,179 participants, is compared among patients classified in terms of circadian characteristics assessed by cosinor (bottom) or in terms of dipping gauged by the day-to-night ratio (top). Comparison among groups within each classification is done by 1-way ANOVA overall (All) and separately for women (F) and men (M). LVMI values are greatly elevated when diastolic ecphasia or CHAT is present (corresponding to abnormal circadian patterns of DBP) vs. LVMI values of patients with and acceptable circadian amplitude and acrophase pair. Such a difference in LVMI is not seen when the day-to-night ratio is used for comparison: LVMI values of patients with a negative (reverse dippers; RD), too small (nondippers; ND), or too large (extreme dippers; ED) day-to-night ratio do not differ from LVMI values of patients with an acceptable day-to-night ratio (dippers; DP). Only a small difference is found for women (P = 0.043) but not for men (P = 0.664) or overall (P = 0.186).
Patient compliance is another valid practical issue illustrating the desirability of keeping the patient engaged and motivated in his/her own health care.
Blood pressure targets are usually set only in terms of mean values, ignoring the evidence that abnormal variability patterns in blood pressure and/or heart rate are major contributors to cardiovascular disease risk. Indeed, in a 6-year prospective outcome study, uncomplicated MESOR-hypertension was associated with less than 10% occurrence of adverse events. The presence of just one additional VVA raised it to 29%, and all three patients who had three additional VVAs had a morbid event (36), Fig. 8.
Fig. 8.
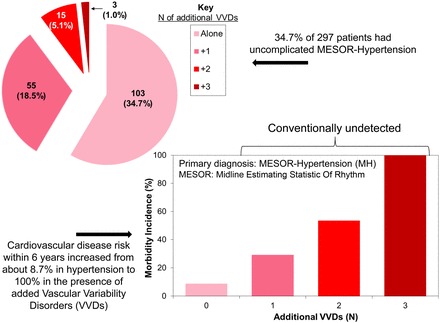
The incidence of VVAs [or, if VVAs persist, vascular variability disorders (VVDs)] was assessed in a clinic population of 297 patients. MH was diagnosed in 176 patients. Excessive PP (EPP), CHAT (a circadian BP overswing), and a deficient heart rate variability (DHRV) were identified by chronobiological and chronomic interpretation of ambulatory blood pressure monitoring (C-ABPM) at the beginning of the study. Uncomplicated MH was found in 103 patients (34.7%). MH complicated by 1, 2, or 3 additional VVAs was found in 55 (18.5%), 15 (5.1%), and 3 (1.0%) of the patients, respectively (top left). The incidence of MH, EPP, CHAT, and DHRV was related to outcomes (cerebral ischemic attack, coronary artery disease, nephropathy, and/or retinopathy), assessed for the next 6 yr. Cardiovascular disease risk associated with MH in the absence of other VVAs is much less than when it is complicated by 1, 2, or 3 additional VVAs (bottom right). Once implemented across the board rather than in selected patient populations, vascular disease could be curbed to a much larger extent at relatively low cost if the monitoring is offered directly to the public and care providers become involved only after the more reliable, but never perfect, detection of a VVA in a second survey of 7 days. A website has to be built, among other approaches, to educate and motivate the public and to provide cost-free analyses in exchange for the data, as is now provided worldwide on a small scale by the BIOCOS project (corne001@umn.edu). The data could be used to investigate the greater problem of societal disease, such as crime and terrorism, as influenced by the environment.
Cost and insufficient insurance coverage are other practical concerns. As a result, ABPM is often restricted to special cases such as patients with the “white coat syndrome.” It should be realized, however, that the only true white-coat hypertension known to us is that of a physician (Y. Watanabe) who has MESOR-hypertension when he puts on his white coat himself in his office, but not when he is not seeing patients on weekends or holidays (Tables 2 and 3) (67). Differences between work days and holidays are validated by parameter tests (5). A white-coat hypertension in the morning can be a white-coat hypotension in the afternoon (54, 55) (Fig. 9), just as a single office diagnosis can differ in conventional practice as a function of whether a patient is seen (by one physician) during mornings or (the same patient, by another physician) during afternoons (3). It seems undesirable that patients be diagnosed as hypertensive (or white-coat hypertensive) versus normotensive because they visit their caregivers at different times of day (12).
Table 2.
Comparison of 3 vascular profiles: 1 and 2 based on months of monitoring; 3 based on weekends and holidays
| Systolic Blood Pressure, mmHg | |||||
| Span | MESOR | 24 h-A | 24 h-ϕ | (A,ϕ) | |
| Jan–Aug 2008 | 142.6 | 11.76 | −246 | ||
| Aug 2008–Jan 2009 | 140.1 | 13.56 | −251 | ||
| Holiday (2008–2009) | 132.1 | 12.54 | −226 | ||
| 1 vs. 2 vs. 3 | |||||
| F | 32.174 | 0.440 | 4.598 | 2.501 | |
| P | <0.001 | 0.645 | 0.012 | 0.045 | |
| 1 vs. 2 | |||||
| F | 4.247 | 1.029 | 0.392 | 0.708 | |
| P | 0.042 | 0.313 | 0.533 | 0.495 | |
| 2 vs. 3 | |||||
| F | 29.504 | 0.246 | 7.073 | 3.886 | |
| P | <0.001 | 0.621 | 0.009 | 0.024 | |
| Diastolic Blood Pressure, mmHg | |||||
| Span | MESOR | 24 h-A | 24 h-ϕ | (A,ϕ) | |
| Jan–Aug 2008 | 87.3 | 5.94 | −236 | ||
| Aug 2008–Jan 2009 | 86.9 | 8.11 | −242 | ||
| Holiday (2008–2009) | 81.9 | 9.08 | −226 | ||
| 1 vs. 2 vs. 3 | |||||
| F | 13.248 | 1.896 | 1.129 | 1.457 | |
| P | <0.001 | 0.154 | 0.327 | 0.219 | |
| 1 vs. 2 | |||||
| F | 0.324 | 5.029 | 0.618 | 2.827 | |
| P | 0.571 | 0.027 | 0.434 | 0.065 | |
| 2 vs. 3 | |||||
| F | 13.581 | 0.254 | 1.740 | 0.949 | |
| P | 0.001 | 0.616 | 0.192 | 0.391 | |
| Heart Rate, beats/min | |||||
| Span | MESOR | 24 h-A | 24 h-ϕ | (A,ϕ) | |
| Jan–Aug 2008 | 74.9 | 4.92 | −246 | ||
| Aug 2008–Jan 2009 | 75.8 | 5.28 | −253 | ||
| Holiday (2008–2009) | 69.6 | 7.95 | −253 | ||
| 1 vs. 2 vs. 3 | |||||
| F | 21.029 | 2.543 | 0.146 | 1.355 | |
| P | <0.001 | 0.082 | 0.865 | 0.253 | |
| 1 vs. 2 | |||||
| F | 0.785 | 0.053 | 0.187 | 0.120 | |
| P | 0.378 | 0.819 | 0.667 | 0.887 | |
| 2 vs. 3 | |||||
| F | 37.279 | 3.392 | 0.001 | 1.697 | |
| P | <0.001 | 0.069 | 0.975 | 0.189 | |
A, amplitude; ϕ, acrophase, expressed in (negative) degrees, with 360° ≡ 24 h, 0° = 00:00. Results from parameter tests (5). For this time-microscopic assessment, the data during the 4 days of vacation in span 3 were removed from span 2 before analysis. MESOR, a midline-estimating statistic of rhythm.
Table 3.
Comparison of vascular end points on Sundays with weekdays reveals acceptability of BP on Sundays by contrast to weekdays in Y.W., a physician scientist
| Weekday | SBP-M | DBP-M | HR-M | SBP-2A | DBP-2A | HR-2A | S-HBI | D-HBI | TCI |
|---|---|---|---|---|---|---|---|---|---|
| Sun | 132.9 | 83.0 | 72.2 | 20.03 | 9.10 | 10.30 | 5 | 1 | 0 |
| Mon | 138.8 | 86.9 | 74.2 | 28.15 | 19.86 | 11.25 | 53 | 11 | 0 |
| Tue | 140.9 | 88.2 | 76.2 | 29.58 | 18.05 | 14.23 | 70 | 12 | 0 |
| Wed | 138.6 | 86.2 | 75.0 | 28.33 | 18.33 | 10.46 | 51 | 9 | 0 |
| Thu | 141.4 | 88.3 | 75.2 | 22.85 | 10.78 | 8.07 | 80 | 6 | 0 |
| Fri | 143.0 | 88.4 | 77.0 | 27.52 | 17.70 | 8.84 | 80 | 5 | 0 |
| Sat | 141.0 | 85.6 | 78.5 | 30.86 | 19.30 | 16.17 | 57 | 5 | 0 |
S, systolic; D, diastolic; M, MESOR; 2A, double circadian amplitude; HBI, hyperbaric index; TCI, tachycardic index. A lower value on Sundays for BP was also found for 30 series from 25 individuals, when the data of each subject were expressed as a percentage of their mean values, examined as a group by a one-way analysis of variance: the lower MESOR was statistically significant for DBP (P < 0.05) and for SBP (P < 0.10). In the same 30 series, the 2A of HR was higher on Sundays and Saturdays than on other days of the week (P < 0.05).
Fig. 9.
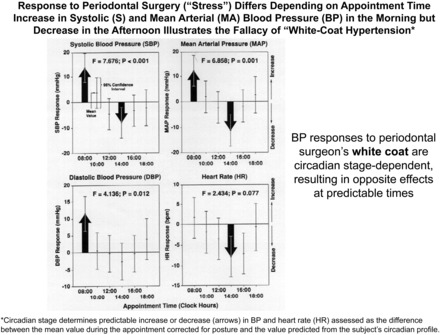
A white-coat hypertension in the morning can be a white-coat hypotension in the afternoon. MAP, mean arterial (MA) pressure.
Body rhythm assessment (C-ABPM), already aligned with chronomic monitoring (quantifying space and earth weather effects), has detected VVAs (Fig. 2), of which a high blood pressure is just one (diagnosed by C-ABPM as MESOR-hypertension), and not always the most important one (Figs. 8 and 10). In one study population, other coexisting, currently unrecognized VVAs raised the risk of a morbid event within 6 years from less than 10% to 100% (Fig. 8).
Fig. 10.
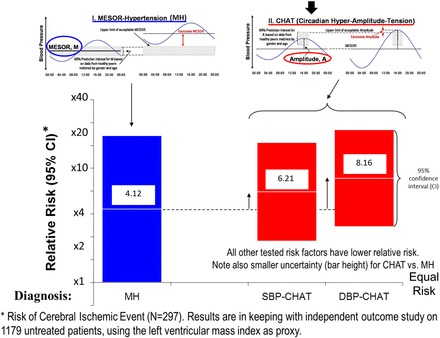
Relative risk of an adverse outcome within 6 yr of the monitoring is assessed for different risk factors as the ratio of the incidence of a cerebral ischemic event that occurred in patients with the tested risk factor by comparison with that in patients not presenting with the tested risk factor. The risk of a cerebral ischemic event for patients with MH (high BP) is less than that for patients with systolic or diastolic CHAT, a condition not currently screened for in the clinic. The risk associated with CHAT is larger than that of all other risk factors considered as well (obesity, high cholesterol, sex, alcohol consumption, family history, smoking, and age) (not shown), including an elevated BP (47, 48, cf. 17, 36). Patients with diastolic CHAT are 8.2 times more likely to suffer an adverse event than patients with an acceptable circadian amplitude of DBP, a 720% increase in risk.
Against this background, we welcome the possibility that the USA's administration is planning a decade-long scientific effort examining the workings of the human brain, to build a comprehensive map of its activity. Reducing morbid events by treating VVAs and VVDs, sometimes by no more than changing the timing of drugs we take, is in large part to save us from a stroke (60). Equally important, we have been mapping frequencies of the human brain shared with space weather and with earth weather, as the effects of the environment on the brain in time are as important as the spatial cerebral structure. In fact, in focusing on magnetism, we find that the relation of human mental functions with either earth or interplanetary magnetism more than matches (by odds ratios) the number of shared frequencies between interplanetary and earth magnetisms themselves (Fig. 11) (11, 31). We found further that human blood pressure monitoring around the clock over decades can be a proxy for mental functions while serving its primary purpose of treating or preventing brain, heart, and kidney disease, as endorsed by an international meeting on GEOCHANGE in Istanbul that we were invited to open (46).
Fig. 11.
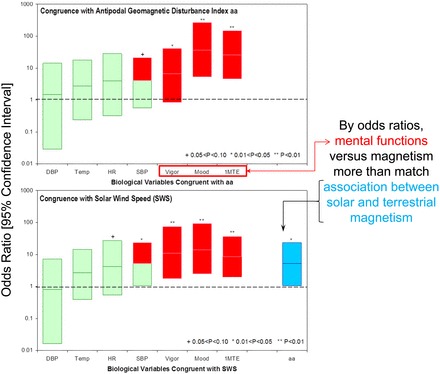
Biospheric congruence with magnetism of Earth (top) and Sun (bottom). Some inferentially statistically validated congruences of human somatic and mental functions with the environment, gauged by the antipodal geomagnetic disturbance index (aa; top) and solar wind speed (SWS; bottom) are shown. While limited to a single clinically healthy case, R.B.S., a man aging during the study from 20 to 60 yr of age, the number of congruences found for the estimation of 1 min and for mood in the spectral range investigated (from 1 cycle in 2.5 yr to 3 cycles/yr) more than equals that of the known association of helio- and geomagnetism. When congruence is assessed by means of the odds ratio based on the noncentral hypergeometric distribution, mental functions show higher congruence than somatic functions; among the latter, SBP is responsive, perhaps constituting a seemingly acceptable approximation for the mental functions. P values are based on the noncentral Fisher hypergeometric distribution, with 95% CIs computed using Fisher exact test, used since the null hypothesis was rejected in some, yet not all, cases. Temp, oral temperature; 1MTE: 1-min time estimation. SBP approximates higher congruence with environment of mental (red) (vs. somatic, green) functions that compare favorably with congruence of aa vs. SWS (blue, bottom right).
There on September 19–21, 2011, C-ABPM already revealed antecedents of the North Japan quake-tsunami in 2011 (Fig. 12). Immediate returns from including a national system of C-ABPM into the president's plans could constitute the major, already documented, focal point of priority in the study of the human brain. It could lead to a novel dimension of societal and natural disaster prevention. This could be a dividend from the same monitoring that aims to prevent personal disasters, the immediately rewarding reason for focus on noncommunicable diseases, including stroke prevention (one more reason to include chronobiology in the U.S. president's plans). C-ABPM also serves our understanding of the competing roles of space and earth weather in influencing masses of people involved in crime and terrorism, as societal and security dividends. In two terrorism databases, there are 1.33-year signatures of the solar wind, with no calendar year, and in a third, the amplitude of components with periods longer than one year more than matches that of the calendar year, suggesting that solar weather is just as (if not more) important than rain or shine on earth in influencing the behavior of populations. Pertinent evidence is documented in Fig. 13 and in our presentations in Istanbul (46; see pp. 23–31 and 228–346), yet another reason to deserve consideration by heads of state. It is good that at least one country takes the initiative to develop the technology for an international system of affordable, automatic, and unobtrusive C-ABPM (27) and that another country in Asia plans on a special department with a C-ABPM system almost certainly a priority (45, 49–51, 61). C-ABPM is feasible automatically on a small worldwide scale documented by the project on the biosphere and the cosmos (BIOCOS). It is both a humanitarian and technological challenge for international cooperation.
Fig. 12.
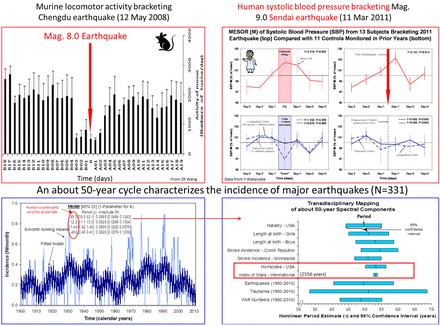
Proposed biospheric contribution to the understanding, if not prediction of earthquakes. Upper left: locomotor activity of mice telemetered around the clock was statistically significantly decreased starting 3 days before the magnitude (Mag) 8.0 earthquake in Chengdu, China, on 12 May 2008. Upper right: human SBP started increasing 2 days before the magnitude 9.0 earthquake in Sendai, Japan, on 11 March 2011, documented on the basis of weeklong records of around-the-clock ambulatory data from 13 Japanese. Similar records from longitudinal and transverse controls differ in their time course, suggesting that the trend observed before the earthquake was related to it rather than being a feature of an anticipated weekly pattern. Lower left: the monthly incidence of major earthquakes since 1900 is characterized by the presence of cycles with periods of about 49.3, 12.2, 1.44, and 0.41 yr, given with their uncertainties (in parentheses). Lower right: the most prominent about 50-year cycle is also documented in physiology, pathology, societal upheavals, and space weather. Nonlinearly estimated periods are displayed with their 95% CIs shown as the length of corresponding horizontal bars.
Fig. 13.
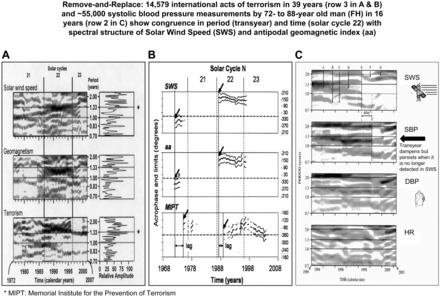
Just as removal and replacement of a gland led to endocrinology, so biological consequences of the loss of environmental spectral components are critical to chronomics, the study of chronomes (time structures) in and around us. The drifting, bi- or trifurcation, disappearance and reappearance of a component with a given frequency and, when present, the waxing and waning of its amplitude, visualized in A and C, is in keeping with external driving of an individual (C) and of a population (A and B). Note components with neighboring frequencies waxing at or near a transyear component in SWS (A, top; and C, top), geomagnetism (A, 2nd row), and in 39 yr of terrorist activity (A, bottom), an association supported by an independent method in B by the statistical significance of the fit of a 1.3-yr far-transyear to interplanetary (SWS) and terrestrial (aa) magnetism and to terrorism. Analysis in A is “glocal” insofar as it is based on the entire series in the spectral window on the right (global) and in sections of the series in the gliding windows on the left (local). Analyses only on sections of the time series are local in B (complementing the global counterpart, as seen on the right of A) and local in C. C shows time courses of the frequency structures of SWS (top) and of an elderly man's (F.H.) SBP, DBP, and HR; SBP, DBP, and HR (rows 2–4, respectively), examined by gliding spectral windows. Human SBP selectively resonates with SWS (top 2 sections). No obvious resonance, only minor coincidence of apparent change, is seen by some in DBP or HR (bottom 2 sections). Aeolian rhythms in gliding spectra of SWS and SBP change in frequency [smoothly (A) or abruptly (B–D), bifurcating (D and F), and rejoining (G); they also change in amplitude (B) up to disappearing (C and E) and reappearing]. *Memorial Institute for the Prevention of Terrorism (MIPT).
We answer in the affirmative a self-raised question about the need for a new definition of hypertension brought up by the late Thomas Pickering, a foremost exponent of the status quo. First a foe of self-measurement when it was proposed (38) and of the initially utopian-seeming ABPM and then a staunch friend of both, Pickering originally believed that circadians are simply a matter of sleep (10, 52, 53). He answered the question about the need for a new definition of hypertension by recognizing that “it should be based on improved measure of blood pressure.” An affordable, unobtrusive monitor communicating via a cell phone with a cloud system and/or a website are indeed considered by the Phoenix Study Group (composed of volunteering members of the Twin Cities chapter of the Institute of Electrical and Electronics Engineers; http://www.phoenix.tc-ieee.org) in China (27) and in a new department of chronomics at Tokyo Women's Medical University (Otsuka, personal communication). Inexpensive, unobtrusive instrumentation monitoring each and all of us is within reach. It is overdue and provides, as Pickering wanted, a new definition of risk by VVAs, so that the many currently undiagnosed patients with iatrogenic VVAs under antihypertensive medication are immediately treated, sometimes by a measure as simple as changing the timing of the drug(s) they take (Figs. 14 and 15).
Fig. 14.
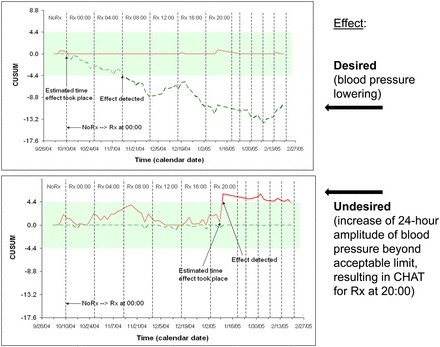
Top: changing timing of medication (ΔRx) during consecutive spans shows efficacy of treatment. An empirical approach to chronotherapy: immediately after diagnosis, one should ascertain that the treatment is effective. Optimization of treatment effects by timing can be achieved for the individual patient by systematically changing, e.g., advancing the time of treatment. Successful treatment of MH assessed by a self-starting cumulative sum (CUSUM) control chart. To optimize his hypotensive treatment (Rx), a just-diagnosed 24-yr-old individual (T.T.) switched his Rx first every 17 days by 4 h and then mostly at shorter intervals. Note statistically significant decrease in MESOR, evidenced by the breakout outside the decision interval of the negative CUSUM line. With continued Rx, the BP MESOR leaves the decision interval, indicating a statistically significant decrease in overall blood pressure. Bottom: changing timing of medication (ΔRx) during consecutive spans shows risk of iatrogenic CHAT. An empirical approach to chronotherapy: immediately after diagnosis, one should ascertain that one does not induce CHAT by inappropriate timing of antihypertensive medication. In this 24-yr-old man (T.T.) who advanced the time of treatment by 4 h every 17 days initially and at shorter intervals thereafter, treatment in the evening was associated with iatrogenic CHAT, raising the question whether the risk of MH may not have been traded for the even higher risk of stroke that CHAT represents. Iatrogenic CHAT, induced by treatment at 20:00 daily, was silent to office visits. T.T. may have traded benefit (lowering of the MESOR of BP, top) for something worse (CHAT). This danger applies to some patients with hypertension (who tend to have a large circadian amplitude of blood pressure) to whom treatment time is not specified (or is specified for bedtime) by the care provider, as was the case for T.T. A few others who took hypertensive medication at bedtime were also found to have CHAT. The figure shows the assessability of otherwise undetected harm by as-one-goes sequential analysis.
Fig. 15.
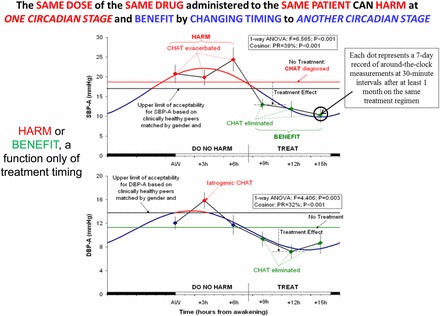
A popular drug, if prescribed without personalized surveillance, can induce a VVA, such as CHAT. A change in the time when the drug is taken can make the same dose of the same drug in the same person beneficial or vice versa. At one administration time (before noon), Hyzaar induces CHAT in DBP and exacerbates a preexisting CHAT in SBP (red). At another time of administration, Hyzaar eliminates a preexisting VVA (green). These opposite effects were found in tests at 6 medication times, each administered for about a month, with half-hourly surveillance of blood pressure during the last week of each span. These differences occur as a function of the timing of the drug's use along the scale of 24 h.
On the basic side, William Harvey jotted down in 1603 that “the movement of the blood occurs constantly in a circular manner and is the result of the beating of the heart.” With Fig. 13, we paraphrase Harvey noting that in the case of systolic blood pressure, the movement of the blood is influenced and synchronized by the rotation of the sun around its equatorial axis (P < 0.001). The same prominent periods of about 10 and 20 years characterizing sunspots are dominant in the human circulation. For practice, the diagnosis and treatment of VVAs must be individualized. Trials that focus only on the blood pressure mean do not recognize iatrogenic conditions such as CHAT (Fig. 15). Furthermore, personalization of treatment time can change harm (such as CHAT induction or enhancement) into benefit (reducing or eliminating CHAT), while also lowering the MESOR of blood pressure. Most importantly, the optimal time of gaining benefit rather than doing harm is shown to differ among patients (68). No shoe fits all.
Results herein illustrate the need for around-the-clock, preferably continuous monitoring, now technologically possible, for the multiple purposes of self-surveillance to detect VVAs and to optimize the timing of treatment administration on an individualized basis if such is needed and improving one's lifestyle by avoiding or reducing loads and learning how to better cope with them, while also gaining a tool to study broad environmental influences on our physiology and to monitor populations for a better understanding of social and natural cataclysms.
GRANTS
This study was supported by National Institute of General Medical Sciences Grant GM-13981 (to F. Halberg) and the University of Minnesota Supercomputing Institute (to G. Cornelissen and F. Halberg).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
AUTHOR CONTRIBUTIONS
F.H., D.P., K.O., and G.C. conception and design of research; F.H., K.O., Y.W., L.A.B., O.S., and G.C. performed experiments; F.H., D.P., K.O., Y.W., L.A.B., P.R., and G.C. interpreted results of experiments; F.H. drafted manuscript; F.H., D.P., O.S., and G.C. edited and revised manuscript; F.H. approved final version of manuscript; K.O., Y.W., L.A.B., J.C., D.H., and G.C. analyzed data; J.C., D.H., and G.C. prepared figures.
REFERENCES
- 1.Baecher CJ, Kottke TE. Pillars of prevention. In: Minnesota Physician. Minneapolis, MN: Minnesota Physician Publsihing, 2013, p. 20–21 [Google Scholar]
- 2.Bailes KE. Science and Russian Culture in an Age of Revolutions: V. I. Vernadsky and his Scientific School, 1863–1945. Bloomington/Indianapolis: Indiana University Press, 1990 [Google Scholar]
- 3.Bartter FC. Periodicity and medicine. In: Chronobiology, edited by Scheving LE, Halberg F, Pauly JE. Tokyo: Igaku Shoin, 1974, p. 6–13 [Google Scholar]
- 4.Beaglehole R, Bonita R, Alleyne G, Horton R, Li L, Lincoln P, Mbanya JC, McKee M, Moodie R, Nishtar S, Piot P, Reddy KS, Stuckler D. for the Lancet NCD Group. UN High-Level Meeting on Non-Communicable Diseases: addressing four questions. Lancet 378: 449–555, 2011 [DOI] [PubMed] [Google Scholar]
- 5.Bingham C, Arbogast B, Cornelissen Guillaume G, Lee JK, Halberg F. Inferential statistical methods for estimating and comparing cosinor parameters. Chronobiologia 9: 397–439, 1982 [PubMed] [Google Scholar]
- 6.Chijevskiy AL. Effect of the periodic solar activity on social phenomena. In: Traité de climatologie, biologique et médicale [in Russian] Paris, 1934, vol. 1, p. 376–385 [Google Scholar]
- 7.Chijevskiy AL. Gazette des Hôpitaux 110: 221–224, 1937 [Google Scholar]
- 8.Chijevskiy AL. (Fedynsky VV AL, Ed)The Earth in the Universe. Jerusalem: Israel Program for Scientific Translations, 1968 [Google Scholar]
- 9.Chijevskiy AL. The Terrestrial Echo of Solar Storms. Moscow: “Mysl”, 1976 [Google Scholar]
- 10.Cornelissen G, Chen CH, Halberg F. Predictive value of blood pressure variability: merits of circadian parameters versus dipping patterns. N Engl J Med 8: 850, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Cornelissen G, Grambsch P, Sothern RB, Katinas G, Otsuka K, Halberg F. Congruent biospheric and solar-terrestrial cycles. J Appl Biomed 9: 63–102, 2011 [Google Scholar]
- 12.Cornelissen G, Halberg F. Impeachment of casual blood pressure measurements and the fixed limits for their interpretation and chronobiologic recommendations. Ann NY Acad Sci 783: 24–46, 1996 [DOI] [PubMed] [Google Scholar]
- 13.Cornelissen G, Halberg Chronomedicine F. InArmitage P, Colton T. (Editors). Encyclopedia of Biostatistics (2nd ed). Chichester, UK: Wiley, 2005, p. 796–812 [Google Scholar]
- 14.Cornelissen G, Halberg F. Treatment with open eyes: markers-guided chronotheranostics. In: Chronopharmaceutics: Science and Technology for Biological Rhythm-Guided Therapy and Prevention of Diseases, edited by Yuan BC. Hoboken, NJ: Wiley; 2009, p. 257–323 [Google Scholar]
- 15.Cornelissen G, Halberg F, Beaty L, Kumagai Y, Halberg E, Halberg J, Lee J, Schwartzkopff O, Otsuka K. Cugini's syndrome in statu nascendi. Oratio contra morem prevalentem et pro chronobiologica ratione ad pressione sanguinis curandam. A plea against the prevailing custom and in favor of a chronobiological approach to treating blood pressure. Clin Ter 160: e13–e24, 2009 [PubMed] [Google Scholar]
- 16.Cornelissen G, Halberg F, Breus T, Syutkina EV, Baevsky R, Weydahl A, Watanabe Y, Otsuka K, Siegelova J, Fiser B, Bakken EE. Non-photic solar associations of heart rate variability and myocardial infarction. J Atmos Solar Terr Phys 64: 707–720, 2002 [Google Scholar]
- 17.Cornelissen G, Halberg F, Otsuka K, Singh RB. Separate cardiovascular disease risks: circadian hyper-amplitude-tension (CHAT) and an elevated pulse pressure. World Heart J 1: 223–232, 2008 [Google Scholar]
- 18.Cornelissen G, Halberg F, Otsuka K, Singh RB, Chen CH. Chronobiology predicts actual and proxy outcomes when dipping fails. Hypertension 49: 237–239, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cornelissen G, Halberg F, Rostagno C, Otsuka K. A chronomic approach to cardiac arrhythmia and sudden cardiac death. Autonomic Nervous System 44: 251–254, 2007 [Google Scholar]
- 20.Cornelissen G, Otsuka K, Halberg F. Remove and replace for a scrutiny of space weather and human affairs. Proceedings, Space Weather Effects on Humans in Space and on Earth. Moscow: Space Research Institute, 2013, vol. 2, p. 508–538 [Google Scholar]
- 21.Deschepper CF, Picard S, Thibault G, Touyz R, Rouleau JL. Characterization of myocardium, isolated cardiomyocytes, and blood pressure in WKHA and WKY rats. Am J Physiol Heart Circ Physiol 282: H149–H155, 2002 [DOI] [PubMed] [Google Scholar]
- 22.Ertel RJ, Halberg F, Ungar F. Circadian system phase-dependent toxicity and other effects of methopyrapone (SU-4885) in mice. J Pharmacol Exp Ther 146: 395–399, 1964 [PubMed] [Google Scholar]
- 23.Ertel S. Mit Sonnenflecken korreliert? Prüfmethode I: Für seltene historische Ereignisse: Testfall Grippepandemien Zeitschrift für Parapsychologie und Grenzgebiete der Psychologie 35: 178–211, 1993 [Google Scholar]
- 24.Ertel S. Influenza pandemics and sunspots—settling the controversy. Naturwissenschaften 81: 308–311, 1994 [DOI] [PubMed] [Google Scholar]
- 25.Ertel S. Space weather and revolutions. Chizhevsky's heliobiological claim scrutinized. Studia Psychologica 38: 3–22, 1996 [Google Scholar]
- 26.Frieden TR, Berwick DM. The “Million Hearts” initiative— preventing heart attacks and strokes. N Engl J Med 365: e27, 2011 [DOI] [PubMed] [Google Scholar]
- 27.Guo Y, Cornelissen G, Wu B, Beaty LA, Adams C, Nolley E, Wu J, Halberg F. Chronomic cloud system for chronorisk-interpreted ambulatory blood pressure monitoring [C-ABPM]? In: Noninvasive Methods in Cardiology, edited by Halberg F, Kenner T, Fiser B, Siegelova J. Brno, Czech Republic: Faculty of Medicine, Masaryk University, 2012, p. 165–179 [Google Scholar]
- 28.Gupta AK, Greenway FL, Cornelissen G, Pan W, Halberg F. Prediabetes is associated with abnormal circadian blood pressure variability. J Hum Hypertens 22: 627–633, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Halberg F. Chronobiology: methodological problems. Acta Med Rom 18: 399–440, 1980 [Google Scholar]
- 30.Halberg F, Breus TK, Cornelissen G, Bingham C, Hillman DC, Rigatuso J, Delmore P, Bakken E,. International Womb-to-Tomb Chronome Initiative Group: Chronobiology in Space. Minneapolis: University of Minnesota/Medtronic Chronobiology Seminar Series, 1991, no. 1, p. 1–21 [Google Scholar]
- 31.Halberg F, Cornelissen G, Grambsch P, McCraty R, Beaty L, Siegelova J, Homolka P, Hillman DC, Finley J, Thomas F, Kino T, Revilla M, Schwartzkopff O. Personalized chronobiologic cybercare; other chronomics' progress by transdisciplinary cycles' congruences: season's appreciations 2009. J Appl Biomed 9: 1–34, 2011 [Google Scholar]
- 32.Halberg F, Cornelissen G, Gumarova L, Halberg Francine Ulmer W, Hillman D, Siegelova J, Watanabe Y, Hong S, Otsuka K, Wu J, Lee JY, Schwartzkopff O, Wendt H. Integrated and as-one-goes analyzed physical, biospheric and noetic monitoring: Preventing personal disasters by self-surveillance may help understand natural cataclysms: a chronousphere (chrono-noösphere). London: SWB International, 2012 [Google Scholar]
- 33.Halberg F, Cornelissen G, Halberg E, Halberg J, Delmore P, Shinoda M, Bakken E. Chronobiology of human blood pressure. Medtronic Continuing Medical Education Seminars (4th ed). Minneapolis: Medtronic, 1988 [Google Scholar]
- 34.Halberg F, Cornelissen G, Katinas GS, Hillman D, Otsuka K, Watanabe Y, Wu J, Halberg Francine Halberg J, Sampson M, Schwartzkopff O, Halberg E. Many rhythms are control information for whatever we do: an autobiography. Folia anthropologica 12: 5–134, 2012 [Google Scholar]
- 35.Halberg F, Cornelissen G, Katinas G, Syutkina EV, Sothern RB, Zaslavskaya R, Halberg Fr Watanabe Y, Schwartzkopff O, Otsuka K, Tarquini R, Perfetto P, Siegelova J. Transdisciplinary unifying implications of circadian findings in the 1950s. J Circadian Rhythms 1: 2, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Halberg F, Cornelissen G, Otsuka K, Siegelova J, Fiser B, Dusek J, Homolka P, Sanchez de la Pena S, Singh RB, project BIOCOS. Extended consensus on need and means to detect vascular variability disorders (VVDs) and vascular variability syndromes (VVSs). World Heart J 2: 279–305, 2010 [Google Scholar]
- 37.Halberg F, Cornelissen G, Regal P, Otsuka K, Wang ZR, Katinas GS, Siegelova J, Homolka P, Prikryl P, Chibisov SM, Holley DC, Wendt RW, Bingham C, Palm SL, Sonkowsky RP, Sothern RB, Pales E, Mikulecky M, Tarquini R, Perfetto F, Salti R, Maggioni C, Jozsa R, Konradov AA, Kharlitskaya EV, Revilla M, Wan CM, Herold M, Syutkina EV, Masalov AV, Faraone P, Singh RB, Singh RK, Kumar A, Singh R, Sundaram S, Sarabandi T, Pantaleoni GC, Watanabe Y, Kumagai Y, Gubin D, Uezono K, Olah A, Borer K, Kanabrocki EA, Bathina S, Haus E, Hillman D, Schwartzkopff O, Bakken EE, Zeman M. Chronoastrobiology: proposal, nine conferences, heligeomagnetics, transyears, near-weeks, near-decades, phylogenetic and ontogenetic memories. Biomed Pharmacother 58, Suppl 1: S150–S187, 2004 [DOI] [PubMed] [Google Scholar]
- 38.Halberg F, Johnson EA, Nelson W, Runge W, Sothern R. Autorhythmometry—procedures for physiologic self-measurements and their analysis. Physiol Tchr 1: 1–11, 1972 [Google Scholar]
- 39.Halberg F, Stephens AN. Susceptibility to ouabain and physiologic circadian periodicity. Proc Minn Acad Sci 27, 139–143, 1959 [Google Scholar]
- 40.Henze M, Hart D, Samarel A, Barakat J, Eckert L, Scrogin K. Persistent alterations in heart rate variability, baroreflex sensitivity, and anxiety-like behaviors during development of heart failure in the rat. Am J Physiol Heart Circ Physiol 295: H29–H38, 2008 [DOI] [PubMed] [Google Scholar]
- 41.Hermida RC, Ayala DE, Mojon A, Fernandez JR. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int 27: 1629–1651, 2010 [DOI] [PubMed] [Google Scholar]
- 42.Marquardt DW. An algorithm for least-squares estimation of nonlinear parameters. J Soc Indust Appl Math 11: 431–441, 1963 [Google Scholar]
- 43.McCraty R, Deyhle A, Childre D. The Global Coherence Initiative: creating a coherent planetary standing wave. Global Advances in Health and Medicine 1: 64–77, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Müller-Bohn T, Cornelissen G, Halhuber M, Schwartzkopff O, Halberg F. CHAT und Schlaganfall. Deutsche Apotheker Zeitung 142: 366–370, 2002 [Google Scholar]
- 45.Murakami S, Otsuka K, Kubo Y, Shinagawa M, Yamanaka T, Ohkawa S, Kitaura Y:. Repeated ambulatory monitoring reveals a Monday morning surge in blood pressure in a community-dwelling population. Am J Hypertens 17: 1179–1183, 2004 [DOI] [PubMed] [Google Scholar]
- 46.Natural Cataclysms, and Global Problems of the Modern Civilization. Proceedings of the World Forum-International Congress (September 19–21, 2011). Istanbul, Turkey: SWB, London, 2012. http://www.2011.geocataclysm.org/ [Google Scholar]
- 47.Otsuka K, Cornelissen G, Halberg F. Predictive value of blood pressure dipping and swinging with regard to vascular disease risk. Clin Drug Investig 11: 20–31, 1996 [Google Scholar]
- 48.Otsuka K, Cornelissen G, Halberg F, Oehlert G. Excessive circadian amplitude of blood pressure increases risk of ischemic stroke and nephropathy. J Med Eng Technol 21: 23–30, 1997 [DOI] [PubMed] [Google Scholar]
- 49.Otsuka K, Cornelissen G, Norboo T, Takasugi E, Halberg F. Chronomics and “glocal” (combined global and local) assessment of human life. Progress of Theoretical Physics 173 Suppl: 134–152, 2008 [Google Scholar]
- 50.Otsuka K, Hotta N, Takasugi E, Yamanaka G, Kubo Y, Cornelissen G, Halberg F. Impaired cardiovascular function predicts mortality from respiratory disorders in the elderly. Hypertens Res 31: 589–591, 2008 [DOI] [PubMed] [Google Scholar]
- 51.Otsuka K, Izumi R, Ishioka N, Ohshima H, Mukai C. Chronomics of heart rate variability on earth and in space. Respir Physiol Neurobiol 169, Suppl 1: 69s–72s, 2009 [DOI] [PubMed] [Google Scholar]
- 52.Pickering TG. Do we really need a new definition of hypertension? J Clin Hypertens (Greenwich) 7: 702–704, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pickering TG, Shimbo D, Haas D. Ambulatory blood pressure monitoring. N Engl J Med 354: 2368–2374, 2006 [DOI] [PubMed] [Google Scholar]
- 54.Raab FJ., 2nd Automatic ambulatory monitoring of circadian blood pressure and heart rate variations associated with periodontal therapy (MS Thesis). Minneapolis: University of Minnesota, 1992 [Google Scholar]
- 55.Raab FJ, Schaffer EM, Guillaume-Cornelissen G, Halberg F. Interpreting vital sign profiles for maximizing patient safety during dental visits. J Am Dent Assoc 129: 461–469, 1998 [DOI] [PubMed] [Google Scholar]
- 56.Refinetti R, Cornelissen G, Halberg F. Procedures for numerical analysis of circadian rhythms. Biol Rhythm Res 38: 275–325, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rosch PJ. Why treating hypertension has become a dismal fiasco. Health and Stress (monthly newsletter of the American Institute of Stress), October 2003 [Google Scholar]
- 58.Rosenbaum L, Lamas D. Global health: facing a “slow-motion disaster”—the UN Meeting on Non-communicable Diseases. N Engl J Med 365: 2345–2348, 2011 [DOI] [PubMed] [Google Scholar]
- 59.Schaffer E, Cornelissen G, Rhodus N, Halhuber M, Watanabe Y, Halberg F. Blood pressure outcomes of dental patients screened chronobiologically: a seven-year follow-up. J Am Dent Assoc 132: 891–899, 2001 [DOI] [PubMed] [Google Scholar]
- 60.Shinagawa M, Kubo Y, Otsuka K, Ohkawa S, Cornelissen G, Halberg F. Impact of circadian amplitude and chronotherapy: relevance to prevention and treatment of stroke. Biomed Pharmacother 55, Suppl 1: 125s–132s, 2001 [DOI] [PubMed] [Google Scholar]
- 61.Shinagawa M, Otsuka K, Murakami S, Kubo Y, Cornelissen G, Matsubayashi K, Yano S, Mitsutake G, Yasaka K, Halberg F. Seven-day (24-h) ambulatory blood pressure monitoring, self-reported depression and quality of life scores. Blood Press Monit 7: 69–76, 2002 [DOI] [PubMed] [Google Scholar]
- 62.Su W, Guo Z, Randall DC, Cassis L, Brown DR, Gong MC. Hypertension and disrupted blood pressure circadian rhythm in type 2 diabetic db/db mice. Am J Physiol Heart Circ Physiol 295: H1634–H1641, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Su W, Xie Z, Guo Z, Duncan MJ, Lutshumba J, Gong MC. Altered clock gene expression and vascular smooth muscle diurnal contractile variations in type 2 diabetic db/db mice. Am J Physiol Heart Circ Physiol 302: H621–H633, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vernadsky VI. A few words about the noosphere. Successes of Modern Biology 18: 113–120, 1944 [Google Scholar]
- 65.Vernadsky VI. Philosophical Thought of Naturalist. Moscow: Science, 1988 [Google Scholar]
- 66.Vital signs: awareness, and treatment of uncontrolled hypertension among adults—United States, 2003–2010. Morbidity and Mortality Weekly Report 61: 703–709, 2012 [PubMed] [Google Scholar]
- 67.Watanabe Y, Cornelissen G, Halberg F, Hillman D, Fiser B, Dusek J, Homolka P, Siegelova J. Infradian modulation of the development of human true white-coat MESOR-hypertension. In: Noninvasive Methods in Cardiology, edited by Halberg F, Kenner T, Fiser B, Siegelova J. Brno, Czech Republic: Faculty of Medicine, Masaryk University, 2010, p. 104–119 [Google Scholar]
- 68.Watanabe Y, Halberg F, Otsuka K, Cornelissen G. Toward a personalized chronotherapy of high blood pressure and a circadian overswing. Clin Exp Hypertens 35: 257–266, 2013 [DOI] [PubMed] [Google Scholar]
- 69.Wauschkuhn CA, Witte K, Gorbey S, Lemmer B, Schilling L. Circadian periodicity of cerebral blood flow revealed by laser-Doppler flowmetry in awake rats: relation to blood pressure and activity. Am J Physiol Heart Circ Physiol 289: H1662–H1668, 2005 [DOI] [PubMed] [Google Scholar]


