Abstract
Background
Livestock-associated MRSA (MC398) has emerged and is related to an extensive reservoir in pigs and veal calves. Individuals with direct contact with these animals and their family members are known to have high MC398 carriage rates. Until now it was assumed that MC398 does not spread to individuals in the community without pig or veal calf exposure. To test this, we identified the proportion of MC398 in MRSA positive individuals without contact with pigs/veal calves or other known risk factors (MRSA of unknown origin; MUO).
Methods
In 17 participating hospitals, we determined during two years the occurrence of MC398 in individuals without direct contact with livestock and no other known risk factor (n = 271) and tested in a post analysis the hypothesis whether hospitals in pig-dense areas have higher proportions of MC398 of all MUO.
Results
Fifty-six individuals (20.7%) without animal contact carried MC398. In hospitals with high pig-densities in the adherence area, the proportion of MC398 of all MUO was higher than this proportion in hospitals without pigs in the surroundings.
Conclusions
One fifth of the individuals carrying MUO carried MC398. So, MC398 is found in individuals without contact to pigs or veal calves. The way of transmission from the animal reservoir to these individuals is unclear, probably by human-to-human transmission or by exposure to the surroundings of the stables. Further research is needed to investigate the way of transmission.
Introduction
Since 2003, the so-called livestock-associated MRSA (LA-MRSA) has emerged in animals and humans in areas with intensive animal farming in Europe, North America, and Asia [1]. Human carriage of LA-MRSA is strongly related to direct contact with pigs, veal calves and broilers [2], [3]. The majority of these LA-MRSA strains belong to multilocus sequence type clonal complex 398 (CC398) [4]. After its emergence, the risk factor ‘direct contact with living pigs, veal calves and broilers’ was added to the Dutch national MRSA guideline and an active screening program in hospitals was implemented [5]. By the end of 2011, 39% of all newly identified MRSA strains in humans in the Netherlands belonged to this variant in the Netherlands [6].
Recent surveys showed that MRSA CC398 was 4 to 6-fold less transmissible than other MRSA strains in a hospital-setting [7]–[8]. At present, the human-to-human transmissibility of MRSA CC398 in a community setting is still unclear. Considering the extensive reservoir in animals and people who work with livestock, the occurrence of MRSA CC398 in people who are not directly involved in farming is strikingly low. So far, there are no indications that MRSA CC398 has spread extensively into the general population [9]. A cross-sectional survey in a livestock-dense region found that only 0.2% of adult individuals without livestock contact were positive for MRSA CC398 [10]. On the other hand, there are observations that proximity of farms is a potential risk factor, even in absence of direct contact between humans and animals [11]–[13]. In addition, in a recent exploratory study an association was found between consumption of poultry and MRSA carriage [14]. A spectrum of infections with MRSA CC398 have been documented, ranging from relatively minor or localized infections including abscesses [15]– and various skin and soft tissue infections (SSTI) [18]–[20], urinary tract infections [16], wound infections [16], mastitis [4], and conjunctivitis [21], as well as more serious or invasive infections, including bacteremia [21]–[24], endocarditis [24], [25], pneumonia (including necrotizing pneumonia, osteomyelitis, pyomyositis, and postoperative infections [26]. Despite the diverse array of infection types reported, it has been suggested that MRSA CC398 is less virulent than other human MRSA strains [27].
Apart from LA-MRSA and hospital-associated (HA)MRSA, MRSA rates also are rapidly increasing in community dwelling individuals without known healthcare- or livestock-associated risk factors. This third entity has been referred to as community-acquired (CA) MRSA [28] or MUO [29]. In this study, the proportion of CC398 in MUO isolates was determined. We hypothesized that people living in an area in which CC398 is common have more risk of MRSA CC398 carriage than persons living in an area in which CC398 is rare.
Methods
Ethics Statement
Ethical approval for the study was obtained by the medical ethics committee of the St. Elisabeth Hospital in Tilburg (NL 19489.008.07, protocol 0749, March 9th, 2009). Patient information was anonymized and de-identified prior to analysis.
MRSA source identification
To identify MRSA sources in the Netherlands, Infection Control Practitioners (ICP) from seventeen hospitals (three academic, seven teaching and seven general hospitals) throughout the Netherlands were asked to complete a questionnaire on a website for all consecutive patients that were found to be MRSA positive (both infection and carriage) for the first time in the microbiological laboratory of the hospital from January 2009 until December 2010. Samples were taken during a visit to the outpatient's clinic or during a stay on a ward in the hospital. Patients who had already been found MRSA-positive in the past were not included. The questionnaire on the website contained data about patient type (in- or outpatient), demographics, positive body sites, molecular typing results and probable source of MRSA. The MRSA source was identified based on the patient's history combined with molecular typing results and then classified in risk groups described in the national infection prevention guidelines [5]. When neither of these risk groups was applicable, the MRSA was classified as ‘MRSA of unknown origin (MUO)’.
Genotyping of MRSA isolates
All MRSA isolates were genotyped by multiple-locus variable number of tandem repeat analysis (MLVA) by the Dutch National Reference Center (RIVM, Bilthoven, the Netherlands) [30]. MLVA is known for its higher discriminatory power for LA-MRSA strains as compared to either multilocus sequence typing (MLST) or pulsed-field gel electrophoresis (PFGE) [30]. The MLVA profiles were clustered using a categorical clustering coefficient (unweighted-pair group method using arithmetic averages, UPGMA) and a minimum spanning tree was constructed to display the relationships between the various MLVA complexes (MC) and MRSA sources. For this study, we incorporated phiSa3 into the MLVA scheme. Furthermore, tetM was determined by use of DNA microarray (Identibac S. aureus Genotyping, Alere).
Data analysis
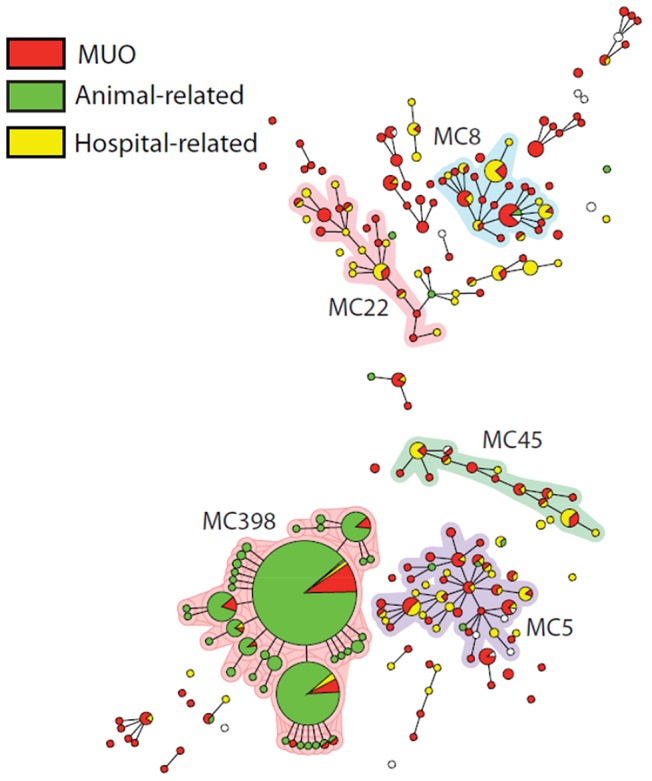
The percentage of MC398 in the group with individuals not reporting contact with pigs or veal calves was determined. We hypothesized that individuals without direct contact with pigs/veal calves living in a pig-dense area have more chance to become colonized with MC398 MUO than individuals living in areas without many pigs. Hospitals were divided into two categories: 1) Hospital with an adherence area with a high pig-density; 2) Hospital with an adherence area with a low pig-density. Municipality level data of the number of pigs were downloaded from the website of the Central Institute for Statistics (CBS) [31]. To test our hypothesis, the numbers of MC398 MUO positive individuals in these two categories were compared in a Chi-square test in a post analysis. To avoid bias by possible different screening policies of the 17 different hospitals, only MRSA infections were included in this analysis. In this way, unexpected findings in contract tracings were excluded.
Results
During 2009–2010, 1020 patients (368 inpatients and 652 outpatients) were found to be MRSA-positive in the seventeen participating hospitals. From 299 (29.3%) patients, MRSA-positive samples were obtained from body sites other than nose, throat, and perineum, mainly urine, sputum and wounds. Eight patients suffered from a bacteremia with MRSA (0.8%). In 39 patients (3.8%), MRSA was found in the perineum sample only, while other tested sites were found to be negative for MRSA.
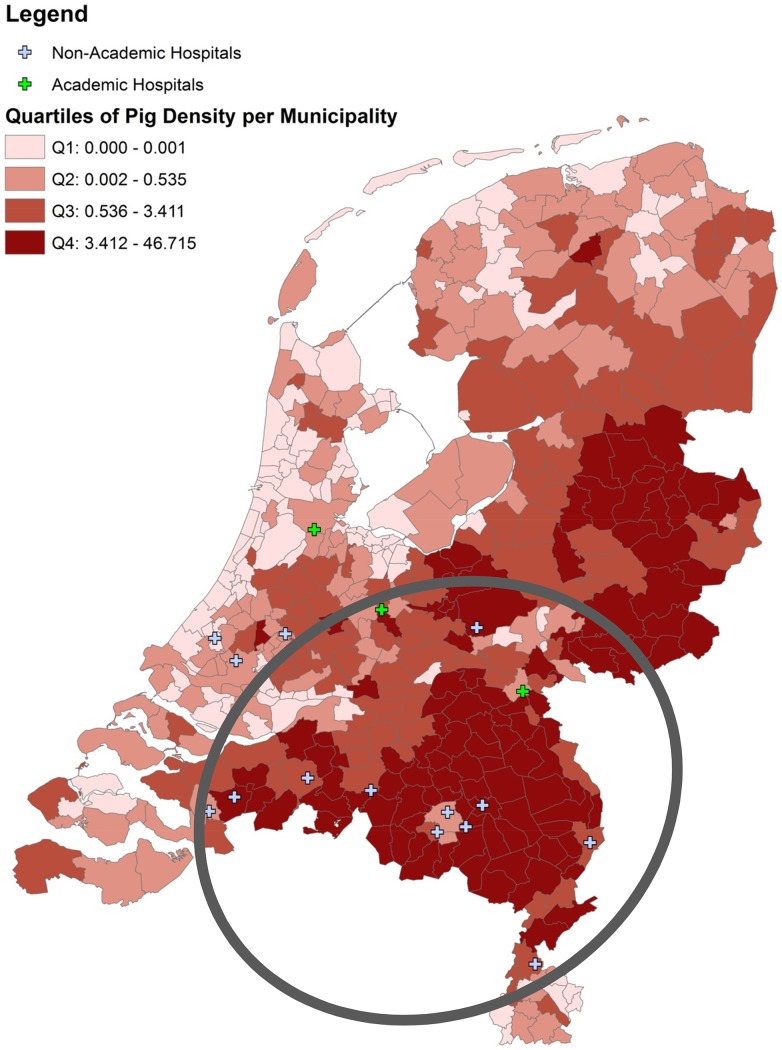
MRSA source analysis is depicted in Table 1. MLVA typing of the strains showed that 649/1020 (63.6%) strains were MC398. Two-hundred and seventy one (26.6%) of all newly identified carriers were of unknown origin, and 56 (20.7%) of them were MC398. These 56 MC398 isolates were tetM positive and lacked the prophage Sa3 (phiSa3). The mean risk to find a MC398 MUO in a participating hospital was estimated at 1 per 8 months (1 per 12 months for infections only). Thirty-five of the 56 (62.5%) individuals suffered from an infection. Figure 1 shows MUO, hospital- and animal-related MRSA and their MLVA complexes. MC398 MUO and MC398 of patients with animal contact cluster together. To test our hypothesis that individuals without animal contact have more chance to carry MC398 MRSA in pig-dense areas than in areas without many pigs, a Chi-square test was performed for hospitals with an adherence area with many pig farms compared to hospitals in an area without many pigs. Data of all participating hospitals is shown in Table 2. Pig-densities in the Netherlands are shown in Figure 2. We found an indication that, in hospitals with high pig-densities in the adherence area, the proportion of MC398 infection of all MUO infection is higher than in hospitals without pigs in the surroundings (32/148 vs. 3/59; RR 4.25 95% CI 1.35–17.21, P = 0.004).
Table 1. MRSA sources in patients in 17 Dutch hospitals, 2009–2010.
| Source | Total | MC398 | ||
| N | % of total | n | % within source | |
| Pigs/veal calves | 603 | 59.1 | 587 | 97.3 |
| Foreign hospital | 75 | 7.4 | 3 | 4.0 |
| Nosocomial transmission | 44 | 4.3 | 3 | 6.8 |
| Transmission in nursing home | 5 | 0.5 | 0 | 0.0 |
| Adoption children | 18 | 1.8 | 0 | 0.0 |
| Dialysis patients from foreign countries | 2 | 0.2 | 0 | 0.0 |
| Unknown origin (MUO) | 271 | 26.6 | 56 | 20.7 |
| No data | 2 | 0.2 | ||
| Total | 1020 | 100 | 649 | 63.6 |
Figure 1. Genotypic relatedness of 1020 MRSA isolates represented as a minimum spanning tree based on MLVA types.
Clustering of MLVA profiles was obtained using a categorical coefficient to create a minimum spanning tree in which the MLVA types are displayed as circles. The size of each circle indicates the number of isolates with this particular type. MLVA complexes (MC) are indicated in characters e.g. MC398 denotes MLVA complex 398.
Table 2. Unknown risk factor (MUO) and proportion of MC398 within this group, shown per hospital.
| Hospital | Hospital type | Newly identified MRSA (total) | Pig-density in adherence area | Unknown risk factor (MUO) | MC398 MUO | ||
| ntotal (ninfection) | % | ntotal (ninfection) | % | ||||
| 1 | teaching | 100 | High | 39 (32) | 39.0 | 7 (5) | 17.9 |
| 2 | teaching | 53 | High | 10 (7) | 18.9 | 2 (2) | 20.0 |
| 3 | general | 95 | High | 10 (7) | 10.5 | 5 (5) | 50.0 |
| 4 | general | 137 | High | 24 (18) | 17.5 | 9 (6) | 37.5 |
| 5 | general | 26 | Low | 17 (11) | 65.4 | 2 (1) | 11.8 |
| 6 | general | 19 | High | 4 (3) | 21.1 | 0 | 0 |
| 7 | teaching | 54 | High | 6 (6) | 11.1 | 1 (1) | 16.7 |
| 8 | general | 30 | High | 19 (16) | 63.3 | 1 (1) | 5.3 |
| 9 | teaching | 18 | Low | 9 (9) | 50.0 | 1 (0) | 11.1 |
| 11 | general | 40 | High | 5 (5) | 12.5 | 1 (1) | 20.0 |
| 12 | teaching | 84 | High | 15 (9) | 17.9 | 4 (0) | 26.7 |
| 13 | teaching | 25 | Low | 18 (15) | 72.0 | 1 (1) | 5.6 |
| 14 | academic | 60 | High | 23 (16) | 38.3 | 12 (9) | 52.2 |
| 15 | academic | 48 | High | 23 (14) | 47.9 | 6 (1) | 26.1 |
| 16 | academic | 52 | Low | 30 (24) | 57.7 | 1 (1) | 3.3 |
| 17 | general | 26 | High | 9 (9) | 34.6 | 2 (1) | 22.2 |
| 18 | teaching | 151 | High | 10 (6) | 6.6 | 1 (0) | 10.0 |
| Total | 1018 a | 271 (207) | 26.6 | 56 (35) | 20.7 | ||
in two individuals there were no data about the source.
Hospital 10 intended to participate, but completed no electronic forms.
Figure 2. Pig-densities in the Netherlands.
Hospitals with high pig-densities in the adherence areas are presented within the circle.
Discussion
The majority (n = 603, 59.1%) of newly identified MRSA-positive patients in 17 hospitals in 2009 and 2010 was related to exposure to livestock. A substantial proportion could not be classified to an established risk group (n = 271, 26.6%) and are therefore assumed to have acquired their MRSA in the community. One fifth (20.7%) of these MRSA strains belonged to MC398. The presence of the tetM resistance gene and the absence of the phiSa3 suggest that these isolates were animal-associated [22], [32]. We found an indication that, in hospitals with high pig-density in the surroundings, the proportion of MC398 infection of all MUO infection was higher than in hospitals with a low pig-density in the surroundings. This indicates that LA-MRSA may be spreading through other sources than direct exposure to livestock. Until now it was assumed that LA-MRSA is able to spread to the pig/veal calf farmers and others who are in close contact with the animals, but is less able to spread from the farmer to household members who do not enter the stables, and is almost unable to spread to persons in the community without pig or veal calf exposure. Thus, it is assumed that constant pressure of LA-MRSA from animals with MRSA must be present to maintain the LA-MRSA colonization in humans. However, several recent studies have shown that persistent colonization with MC398 is possible [33]–[35]. Moreover, pig-, dairy cow, and veal calf densities per municipality were also found to be independent risk factors for carriage of MRSA MC398 in two recently published case-control studies [11], [14]. Although it cannot be excluded that human-to-human transmission occurs in areas with a high MRSA MC398 pressure, environmental contamination with MRSA MC398 may play a role as well. MRSA MC398 has been shown to be present in air and soil samples collected downwind of pig and swine barns [13]. Other transmission routes can play a role as well. For example, regular consumption of poultry was recently found to be associated with CA-MRSA transmission in an exploratory hospital-based case-control study [14]. De Boer et al. demonstrated that a substantial part of the meat products obtained from retail stores in the Netherlands were colonized with MRSA, including both MC398 and non-MC398 strain types [36]. However, meat consumption cannot explain the increased prevalence in people who live in pig-dense areas. We expect the risk, associated with meat consumption, to be the same for all areas over the country. Unless, locals consume more meat from their own area.
Limitations
We performed a post hoc analysis to study whether the proportion of MC398 MUO infection is higher in hospitals in pig-dense areas than in areas with a low pig-density. Our study was originally not designed for this purpose. Therefore, we have to be careful with the conclusions. An analysis in which pig-density was determined based on postal code of the individuals would have been more reliable. These data were not available because of privacy issues. Also, the stratification of hospitals in ‘pig-dense’ and ‘pig-arm’ areas is arbitrary. Based on the CBS data, we classified the hospitals that are known to be situated in the most urbanized parts of the country as ‘pig-arm’. This resulted in four hospitals in pig-arm areas and 13 hospitals in pig-dense areas. So, more hospitals in pig-dense areas were included in the analysis. Furthermore, there may be detection bias due to differences in screening policies between hospitals. It is possible that physicians in some hospitals take more clinical samples than physicians in other hospitals. This may lead to an underestimation in the number of MUO findings. Also, classification bias may occur depending on the reliability of the history of risk factors. However, all participating hospitals screened the MRSA risk groups described in the national MRSA guideline [5]. After coincidental MRSA findings, patients were asked for these risk factors also.
In conclusion, this study shows that the majority of newly identified MRSA patients in these 17 hospitals were acquired by direct contact with pigs/veal calves. The second largest group is the group of unknown origin. One fifth of these MUO are MC398. We found a significant association between individuals living in pig-dense areas and the likelihood of MC398 MUO carriage. MC398 MUO infections were rarely detected, i.e. 1 per 12 months for every participating hospital, so, currently, this MC398 MUO seems not to cause many problems. Because of the absence of known risk factors and probable risk for transmission in the healthcare settings, it is worthwhile to monitor the number of MUO in general, and of MC398 separately, in the coming years.
Acknowledgments
CAM Study Group:
Amphia Hospital, Breda: Brigitte van Cleef, Yvonne Hendriks, Daniëlle op den Kamp, Jan Kluytmans, Marjolein Kluytmans – van den Bergh, Renée Ladestein, Rudolf Punselie, Miranda van Rijen, Erwin Verkade
Catharina Hospital, Eindhoven: Marieke Ernest, Mireille Wulf
Duke University, Durham, NC, USA: Beth Feingold
Elkerliek Hospital, Helmond: Mariëlla Brekelmans, Patricia Willemse, Mireille Wulf
Franciscus Hospital, Roosendaal: Nelleke ten Feld, Rob Wintermans
Hospital Gelderse Vallei, Ede: Bent Postma, Marja Terwee, Thuy-Nga
Groene Hart Hospital, Gouda: Truus de Ruiter, Eric van der Vorm, Antoinette Wijker
Lievensberg Hospital, Bergen op Zoom: Henk Hamers, Rob Wintermans
Maxima Medical Centre, Eindhoven/Veldhoven: Philo Das, Ellen Sanders, Kees Verduin
Orbis Medical Centre, Sittard: Dick van Dam, Jan Diederen
Regional Health Authority, Leiden: Peter ten Ham
Reinier de Graaf Hospital, Delft: Loes Nolles, Eric van der Vorm
St. Anna Hospital, Geldrop: Anouk Smeulders, Kees Verduin
St. Elisabeth Hospital, Tilburg: Anton Buiting, Helma Hörmann, Ellen Nieuwkoop
St. Franciscus Gasthuis, Rotterdam: Yvonne Muller
University Medical Centre St Radboud, Nijmegen: Diana Haverkate, Paul Verweij
University Medical Centre Utrecht, Utrecht: Marc Bonten, Marischka van der Jagt-Zwetsloot, Annet Troelstra
VieCuri Medical Centre, Venlo: Hanneke Berkhout, Liduine van den Hout
VU Medical Centre, Amsterdam: Annie Kaiser, Christina Vandenbroucke-Grauls
We want to thank Beth Feingold for creating figure 2.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All data are included in the manuscript.
Funding Statement
This work was supported by The Netherlands Organisation for Health Research and Development [grant number 125020007]. ZonMw is a non-profit organisation working for the Ministry of Health, Welfare and Sport (VWS) and the Dutch Organisation for Scientific Research (NOW). ZonMw had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. http://www.zonmw.nl/nl/
References
- 1. Smith TC, Pearson N (2011) The emergence of Staphylococcus aureus ST398. Vector Borne Zoonotic Dis 11: 327–9. [DOI] [PubMed] [Google Scholar]
- 2. van Loo I, Huijsdens X, Tiemersma E, de Neeling A, van de Sande-Bruinsma N, et al. (2007) Emergence of methicillin-resistant Staphylococcus aureus of animal origin in humans. Emerg Infect Dis 13: 1834–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mulders MN, Haenen AP, Greenen PL, Vesseur PC, Poldervaart ES, et al. (2010) Prevalence of livestock-associated MRSA in broiler flocks and risk factors for slaughterhouse personnel in The Netherlands. Epidemiol Infect 138: 743–55. [DOI] [PubMed] [Google Scholar]
- 4. Huijsdens XW, van Dijke BJ, Spalburg E, van Santen-Verheuvel MG, Heck ME, et al. (2006) Community-acquired MRSA and pig-farming. Ann Clin Microbiol Antimicrob 5: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dutch Workingparty on Infection Prevention (2007) MRSA hospital. Available at http://www.wip.nl. Accessed 1 November 2012.
- 6.Infectieziekten Bulletin (2012) Surveillance of MRSA in the Netherlands in 2011 [in Dutch]. Available at http://www.rivm.nl/Onderwerpen/I/Infectieziekten_Bulletin. Accessed 4 November 2013.
- 7. Wassenberg MW, Bootsma MC, Troelstra A, Kluytmans JA, Bonten MJ (2011) Transmissibility of livestock-associated methicillin-resistant Staphylococcus aureus (ST398) in Dutch hospitals. Clin Microbiol Infect 17 2: 316–9 10.1111/j.1469-0691.2010.03260.x [DOI] [PubMed] [Google Scholar]
- 8. Bootsma MC, Wassenberg MW, Trapman P, Bonten MJ (2011) The nosocomial transmission rate of animal-associated ST398 meticillin-resistant Staphylococcus aureus . J R Soc Interface 8 57: 578–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cuny C, Nathaus R, Layer F, Strommenger B, Altmann D (2009) Nasal colonization of humans with methicillin-resistant Staplylococcus aureus (MRSA) CC398 with and without exposure to pigs. PLoS One 4 8: e6800 10.1371/journal.pone.0006800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van Cleef BA, Verkade EJ, Wulf MW, Buiting AG, Voss A, et al. (2010) Prevalence of livestock-associated MRSA in communities with high pig-densities in The Netherlands. PLoS One 5 2: e9385 10.1371/journal.pone.0009385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Feingold BJ, Silbergeld EK, Curriero FC, van Cleef BA, Heck ME, et al. (2012) Livestock density as risk factor for livestock-associated methicillin-resistant Staphylococcus aureus, the Netherlands. Emerg Infect Dis 18: 1841–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. van Cleef BA, Monnet Dl, Voss A, Krziwanek K, Allerberger F, et al. (2011) Livestock-associated methicillin-resistant Staphylococcus aureus in humans, Europe. Emerg Infect Dis 17 3: 502–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schulz J, Friese A, Klees S, Tenhagen BA, Fetsch A, et al. (2012) Longitudinal study of the contamination of air and of soil surfaces in the vicinity of pig barns by livestock-associated methicillin-resistant Staphylococcus aureus . Appl Environ Microbiol 78: 5666–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. van Rijen MM, Kluytmans-van den Bergh MF, Verkade EJ, ten Ham PB, Feingold BJ, et al. (2013) Lifestyle-associated risk factors for community-acquired methicillin-resistant Staphylococcus aureus carriage in the Netherlands: an exploratory hospital-based case-control study. PLoS One 8 6: e65594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fanoy E, Helmhout LC, van der Vaart WL, Weijdema K, van Santen-Verheuvel MG, et al. (2009) An outbreak of non-typeable MRSA within a residential care facility. Euro Surveill 14. [PubMed] [Google Scholar]
- 16. van Belkum A, Melles DC, Peeters JK, van Leeuwen WB, van Duijkeren E, et al. (2008) Dutch Working Party on Surveillance and Research of MRSA-SOM. Methicillin-resistant and -susceptible Staphylococcus aureus sequence type 398 in pigs and humans. Emerg Infect Dis 14: 479–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pan A, Battisti A, Zoncada A, Bernieri F, Boldini M, et al. (2009) Community-acquired methicillin-resistant Staphylococcus aureus ST398 infection, Italy. Emerg Infect Dis 15: 845–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Declercq P, Petre D, Gordts B, Voss A (2007) Complicated community-acquired soft tissue infection by MRSA from porcine origin. Infection 36: 590–2. [DOI] [PubMed] [Google Scholar]
- 19. van Rijen MM, van Keulen PH, Kluytmans JA (2008) Increase in a Dutch hospital of methicillin-resistant Staphylococcus aureus related to animal farming. Clin Infect Dis 46: 261–3. [DOI] [PubMed] [Google Scholar]
- 20. Krziwanek K, Metz-Gercek S, Mittermayer H (2009) Methicillin-resistant Staphylococcus aureus ST398 from human patients, upper Austria. Emerg Infect Dis 15: 766–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Grisold AJ, Zarfel G, Hoenigl M, Krziwanek K, Feierl G, et al. (2010) Occurrence and genotyping using automated repetitive-sequence-based PCR of methicillin-resistant Staphylococcus aureus ST398 in Southeast Austria. Diagn Microbiol Infect Dis 66: 217–21. [DOI] [PubMed] [Google Scholar]
- 22. Valentin-Domelier AS, Girard M, Bertrand X, Violette J, François P, et al. (2011) Bloodstream Infection Study Group of the Réseau des Hygiénistes de Centre (RHC). Methicillin-susceptible ST398 Staphylococcus aureus responsible for bloodstream infections: an emerging human-adapted subclone? PLoS One 6: e28369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Verkade E, Bergmans AM, Budding AE, van Belkum A, Savelkoul P, et al. (2012) Recent emergence of Staphylococcus aureus clonal complex 398 in human blood cultures. PLoS One 7: e41855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ekkelenkamp MB, Sekkat M, Carpaij N, Troelstra A, Bonten MJ (2006) Endocarditis due to meticillin-resistant Staphylococcus aureus originating from pigs [in Dutch]. Ned Tijdschr Geneeskd 150: 2442–7. [PubMed] [Google Scholar]
- 25. Tristan A, Rasigade JP, Ruizendaal E, Laurent F, Bes M, et al. (2012) Rise of CC398 lineage of Staphylococcus aureus among infective endocarditis isolates revealed by two consecutive population-based studies in France. PLoS One 7 12: e51172 10.1371/journal.pone.0051172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Witte W, Strommenger B, Stanek C, Cuny C (2007) Methicillin-resistant Staphylococcus aureus ST398 in humans and animals, Central Europe. Emerg Infect Dis 13: 255–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Grundmann H, Aanensen DM, van den Wijngaard CC, Spratt BG, Harmsen D, et al. (2010) Geographic distribution of Staphylococcus aureus causing invasive infections in Europe: a molecular-epidemiological analysis. PLoS Med 7 1: e1000215 10.1371/journal.pmed.1000215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. David MZ, Daum RS (2010) Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev 23: 616–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lekkerkerk WS, van de Sande-Bruinsma N, van der Sande MA, Tjon-A-Tsien A, Groenheide A, et al. (2012) Emergence of MRSA of unknown origin in the Netherlands. Clin Microbiol Infect 18 7: 656–61. [DOI] [PubMed] [Google Scholar]
- 30. Schouls LM, Spalburg EC, van Luit M, Huijsdens XW, Pluister GN, et al. (2009) Multiple-locus variable number tandem repeat analysis of Staphylococcus aureus: comparison with pulsed-field gel elctrophoresis and spa-typing. PLoS One 4 4: e5082 10.1371/journal.pone.0005082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.CBS Central Bureau of Statistics: Statline (2009) Available: cbs.statline.nl. Accessed 2012 July.
- 32. Price LB, Stegger M, Hasman H, Aziz M, Larsen J, et al. (2013) Staphylococcus aureus CC398: host adaptation and emergence of methicillin resistance in livestock. MBio 31 1: e00305–11 10.1128/mBio.00305-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Köck R, Loth B, Köksal M, Schulte-Wülwer J, Harlizius J, et al. (2012) Does nasal colonization with livestock-associated Methicillin-resistant Staphylococcus aureus (MRSA) in pig farmers persist after holidays from pig exposure? Appl Environ Microbiol 78 11: 4046–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Slingerland BC, Tavakol M, McCarthy AJ, Lindsay JA, Snijders SV, et al. (2012) Survival of Staphylococcus aureus ST398 in the human nose after artificial inoculation. PLoS One 7 11: e48896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Verkade E, van Benthem B, Kluytmans-van den Bergh MF, van Cleef B, van Rijen M, et al. (2013) Dynamics and determinants of Staphylococcus aureus carriage in livestock veterinarians: a prospective cohort study. Clin Infect Dis 57: e11–7. [DOI] [PubMed] [Google Scholar]
- 36. de Boer E, Zwartkruis-Nahuis JT, Wit B, Huijsdens XW, de Neeling AJ, et al. (2009) Prevalence of methicillin-resistant Staphylococcus aureus in meat. Int J Food Microbiol 134: 52–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All data are included in the manuscript.