Abstract
Worldwide, more than three million children are infected with HIV, 90% of whom live in sub-Saharan Africa. As the HIV epidemic matures and antiretroviral treatment is scaled up, children with HIV are reaching adolescence in large numbers. The growing population of adolescents with perinatally acquired HIV infection living within this region presents not only unprecedented challenges but also opportunities to learn about the pathogenesis of HIV infection. In this Review, we discuss the changing epidemiology of paediatric HIV and the particular features of HIV infection in adolescents in sub-Saharan Africa. Longstanding HIV infection acquired when the immune system is not developed results in distinctive chronic clinical complications that cause severe morbidity. As well as dealing with chronic illness, HIV-infected adolescents have to confront psychosocial issues, maintain adherence to drugs, and learn to negotiate sexual relationships, while undergoing rapid physical and psychological development. Context-specific strategies for early identification of HIV infection in children and prompt linkage to care need to be developed. Clinical HIV care should integrate age-appropriate sexual and reproductive health and psychological, educational, and social services. Health-care workers will need to be trained to recognise and manage the needs of these young people so that the increasing numbers of children surviving to adolescence can access quality care beyond specialist services at low-level health-care facilities.
Introduction
HIV infection has been established for more than 30 years, with sub-Saharan Africa continuing to have the highest incidence of HIV of any region.1 The global epidemiology of paediatric HIV mirrors that of adults. Of more than three million children infected with HIV, 90% live in sub-Saharan Africa.1 The advent of the HIV epidemic resulted in a reversal of the improvements recorded in child health outcomes in the 1970s and 1980s, with global child mortality rates a third to two-thirds higher than they would have been in the absence of HIV/AIDS.2
However, since 2004, access to paediatric antiretroviral treatment has expanded globally, resulting in a substantial decline in mortality rates in HIV-infected children.3 In view of this increased survival, HIV is now evolving into a chronic illness among adolescents.4 Young adults who have grown up with HIV present an important challenge to HIV care programmes. Longstanding HIV infection acquired when the immune system was not developed results in distinctive chronic clinical complications that cause severe morbidity. In addition to dealing with chronic illness, HIV-infected adolescents have to confront psychosocial issues, maintain adherence to drugs, and learn to negotiate sexual relationships while undergoing rapid physical and psychological changes.5
In this Review, we discuss the evolving epidemiology of paediatric HIV infection and the shift of the infection burden onto adolescents. We also consider some of the unique features that characterise HIV infection in survivors of perinatally acquired HIV infection.
The ageing paediatric HIV epidemic
Unlike the rapid widespread implementation of highly effective HIV interventions in industrialised countries that began in the mid 1990s, antiretroviral treatment for prevention of mother-to-child HIV transmission only became available in much of Africa around 2004. Although in sub-Saharan Africa the number of infant infections has dropped by 24% from 2009 to 2011, treatment coverage remains suboptimum, with only 59% of HIV-infected pregnant women receiving antiretroviral treatment to prevent mother-to-child transmission in the 21 high-burden countries, and about 1000 infants were infected daily in 2011.1
Before antiretroviral treatment was available, HIV-infected infants in Africa had a 50% probability of dying by age 2 years.6 The increasing availability of antiretroviral drugs has resulted in a substantial rise in the life expectancy of children living with HIV in low-income countries, so that escalating numbers of children are surviving to adolescence and beyond.7,8 For example, more than 40% of the 25 000 children in HIV care in Zimbabwe in 2009 were age 10 years or older.9 However, the large numbers of adolescents in HIV programmes in sub-Saharan Africa are not accounted for fully by raised survival related to antiretroviral treatment. Over the past decade, substantial numbers of children in sub-Saharan Africa with perinatally acquired HIV have been presenting to health-care services for the first time during adolescence.10,11 By extrapolation of high early mortality rates associated with untreated HIV in the early days of the HIV epidemic, the widely held perception was that survival to older childhood without treatment in sub-Saharan Africa would be exceptional. However, epidemiological data indicate that at least a third of HIV-infected infants have slow-progressing infection, with a median survival of 16 years without treatment.12 In recent years, survival estimates in sub-Saharan Africa for untreated infants infected perinatally have been revised upwards, with about a 20–30% probability of overall survival in untreated HIV-infected infants to at least age 10 years.12,13
In industrialised countries, two distinct prognostic groups were recognised in the era before antiretroviral treatment—people with fast-progressing infection and those with slow progression of disease. However, exact survival probabilities for HIV-infected infants in Africa were ill-defined because cohorts were not followed up beyond age 5 years.14,15 In population-based HIV prevalence surveys in southern Africa, HIV prevalence of 2–6% was reported consistently among adolescents, before antiretroviral treatment became available.16–18 Up to age 14 years, no difference in HIV prevalence by sex is evident, inferring a non-sexual route of HIV acquisition.19 However, in children older than 14 years, prevalence of HIV is disproportionately higher in girls than in boys, reflecting the well-recognised increased risk of HIV infection through sexual transmission in young women compared with young men.19
As the HIV epidemic matures, as strategies are developed to prevent mother-to-child transmission, and as paediatric antiretroviral drugs become more widely available, the number of HIV-infected infants will decline, whereas the number of children with HIV infection surviving to older ages will increase for some time. Falling prevalence of HIV in adults will compound this trend by reducing the number of infant infections. Such regional trends have been masked by the standard reporting of HIV data in just three age categories: 0–4 years, 5–14 years, and 15–49 years. The number of adolescents infected perinatally accumulated slowly after the onset of the adult epidemic because of the time needed for infants to reach an older age (figure 1). Even with universal access to interventions for prevention of mother-to-child transmission and with scale-up of antiretroviral treatment, a time lag of two decades will be present before the numbers of adolescents infected with HIV perinatally begins to decrease.12
Figure 1.
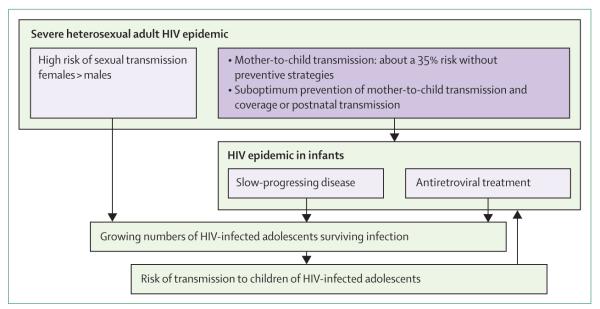
Evolution of the paediatric HIV epidemic in sub-Saharan Africa
Clinical complications of HIV infection
HIV infection in infancy and early childhood is associated with rapid disease progression and typically presents as failure to thrive, severe bacterial and viral infections and AIDS-defining illnesses, including pneumocystis pneumonia, HIV encephalopathy, and refractory candidosis.20 By contrast, older children in sub-Saharan Africa with HIV infection are either asymptomatic or typically have a history of multiple, non-specific complaints, including recurrent upper-respiratory-tract infections, diarrhoea, minor skin infections, and suboptimum growth.21,22 These illnesses are also common in their HIV-uninfected peers and are not recognised as an indication of underlying HIV infection. Health-care workers are only prompted to undertake HIV testing after an individual develops advanced immunosuppression and presents with typical AIDS-indicator illnesses.21 Therefore, health-care providers must have a low threshold for HIV testing in areas of high prevalence, even for children with no apparent risk factors for HIV infection.
Infections and malignant disease
In general, the range of opportunistic infections among HIV-infected adolescents more closely resembles that noted in adults with HIV infection than that in HIV-infected infants and young children.23,24 Cryptococcosis—less commonly seen in younger paediatric patients—is a frequent infectious pathogen in hospitalised HIV-infected young adults in sub-Saharan Africa; further, the incidence of tuberculosis rises in adolescence.25,26 Social contact widens during a child’s teenage years, putting immunosuppressed young people at especially high risk of tuberculosis infection and disease.26,27 However, tuberculosis is difficult to diagnose and treatment is commonly given on the basis of chronic respiratory symptoms without a definitive microbiological diagnosis.28 Therefore, the burden of tuberculosis might be over estimated, because HIV-infected adolescents report high rates of longstanding chronic respiratory symptoms.29
HIV-infected adolescents are susceptible to vaccine-preventable illnesses, which typically have the greatest effect on young children. A lower response rate to early childhood immunisations, and waning immunity after early vaccination, are likely causes; in outbreak situations, HIV-infected adolescents can be especially vulnerable.30–33 Of 195 HIV-infected children identified with measles in an outbreak in Botswana in 2009–10, the median age was 13 years (IQR 10–15).34 The most severely affected patients were HIV-infected adolescents, most of whom had been immunised against measles during early childhood. Further, in a study of young people age 8–17 years in Rwanda who received hepatitis B vaccinations, amounts of HIV RNA and CD4 counts were both independent predictors of hepatitis B antibody response.35 Revaccination could restore immunity, although currently no robust evidence is available to support this. Also, as adolescent girls become sexually active, cervical cancer is of concern. Human papillomavirus (HPV) is associated strongly with cervical cancer, and HPV infection rates in Africa are high. Cervical dysplasia happens frequently and at a young age in girls infected with HIV, but few screening services are available.36 Findings of a study in Tanzania showed that 65% of adolescent girls acquired HPV within 1 year of sexual debut.37 The HPV vaccine has proven safe, immunogenic, and acceptable to adolescents and their guardians.38 However, policies about HPV vaccination are still being developed for most countries in sub-Saharan Africa.39
The range of cancers in HIV-infected children is age-dependent. HIV is associated with a significantly increased risk of Burkitt’s lymphoma and Kaposi’s sarcoma, with Kaposi’s sarcoma being more common in adolescents than in infants and young children.40–42 Unlike young children, who are more likely to have raised CD4+ T-cell counts at presentation and have lymphatic Kaposi’s sarcoma, adolescents present in a similar way to adults, with lower CD4+ T-cell counts and cutaneous lesions.43 In children, the absolute CD4 T-cell count alone is insufficient to ascertain the risk of malignant disease; duration of immunosuppression is a relevant risk factor, which has important implications for the risk of malignant disease in adolescents.44 Longstanding HIV infection might predispose to premature malignant diseases in young adults.45 B-cell and T-cell lymphoproliferative disorders, which are present frequently in HIV-infected children and often at remarkably preserved CD4 counts, potentially represent a preneoplastic state.44 The risk of these disorders developing into overt malignant diseases in adolescence and beyond is not yet known. Cases of atypical and rare malignant diseases in HIV-infected adolescents have been reported.44,46,47
Chronic disease
One of the striking features of HIV infection in adolescence is the high prevalence of chronic complications. These disorders can lead to severe disability (figure 2).
Figure 2. Clinical manifestations of HIV infection in adolescents infected by perinatal transmission.
(A) Severe stunting in a 14-year-old boy (height-for-age Z score −3·5). (B) Diffuse planar warts in a 13-year-old boy. (C, D) Deforming, non-infectious, seronegative arthritis in a 16-year-old boy. All patients and their guardians have provided their consent for pictures to be reproduced.
Chronic lung disease
As children get older, they are at increased risk of developing HIV-associated chronic lung disease. This disorder is well-described in HIV-infected younger children, and lymphocytic interstitial pneumonitis was the predominant cause before use of antiretroviral treatment became widespread.48,49 Lymphocytic interstitial pneumonitis responds well to antiretroviral treatment, but delayed initiation of antiretroviral drugs can lead to long-term sequelae such as bronchiectasis and cor pulmonale in adolescence.50 The range of chronic lung disease seems to differ in adolescents compared with younger children.51 In a study from Zimbabwe of 116 adolescents with HIV infection acquired perinatally, more than 30% of children had severe and disabling chronic respiratory symptoms; these findings were confirmed by those of a study from Malawi in 160 older children.52 Unexpectedly, in the Zimbabwe study, high-resolution CT scanning showed predominantly small-airways disease consistent with constrictive obliterative bronchiolitis, with lymphocytic interstitial pneumonitis being an exceptional finding. Unlike lymphocytic interstitial pneumonitis, obliterative bronchiolitis seemed to have little reversibility with antiretroviral treatment once established; 7% of children had coexisting pulmonary hypertension.29 Obliterative bronchiolitis, which occurs with graft-versus-host disease and after viral infections and exposure to chemical fumes, is a progressive life-threatening condition, and little is known about its natural history and pathogenesis in people with HIV infection or how it should be managed.51,53 Chest radiographic findings are non-specific, and high-resolution CT—the gold standard diagnostic method—is not typically available in resource-limited settings.53 Obliterative bronchiolitis has not been described before in US and European cohorts of HIV-infected adolescents. The availability of antiretroviral treatment during early childhood might be preventive for this disorder, and geographical variability or genetic predisposition could have a role.54
Cardiac disease
Cardiac disease is well-described in HIV-infected infants and young children, and risk increases with age.55–57 Abnormalities include dilated cardiomyopathy, pericardial effusion, left-ventricular diastolic dysfunction, increased left-ventricular wall thickness or mass, and decreased left-ventricular fractional shortening. Subclinical abnormalities can develop into symptomatic cardiac disease with increasing age, but few data are available on the burden of cardiac pathology in adolescents from Africa with HIV infection.58 In a cohort of hospitalised HIV-infected adolescents in Zimbabwe, cardiac disease—including cardiomyopathy—was the reason for admission in 12% of cases.24 An assessment was done of 110 perinatally infected adolescents in HIV care in Harare.59 67% had left-ventricular hypertrophy and 24% had impaired left-ventricular relaxation or restrictive physiology. Moreover, 31% had right-ventricular dilatation and 4% met echocardiographic criteria for pulmonary hypertension, which were both probably secondary to chronic lung disease. Also, exertional dyspnoea was noted in 43% and chest pain in 39%; finally, 37% had a New York Heart Association score of greater than 2, indicating substantial limitation of activity.59 The effect of antiretroviral treatment on the natural history of cardiac abnormalities is not clear. Prolonged exposure to certain classes of antiretroviral drug—such as protease inhibitors—causes lipid abnormalities and could itself increase the risk of premature cardiovascular disease.60
Growth failure
Growth failure, including stunting and pubertal delay, is one of the hallmarks of paediatric HIV infection and generally distinguishes adolescents with perinatally acquired HIV infection from their uninfected peers and from those infected sexually.21,24,61–64 Growth failure can become especially obvious in adolescence as untreated HIV-infected adolescents lag behind peers who are going through periods of rapid growth and pubertal development. Stunting—a reflection of poor linear growth—happens over a long period and might be the only manifestation of chronic HIV infection in an otherwise seemingly healthy adolescent. Wasting occurs mainly with development of advanced disease and reflects acute illness.65 The extent of stunting is more profound among HIV-infected children in Africa compared with those in resource-rich settings, possibly reflecting higher background rates of malnutrition and an increased burden of infection.66 Although catch-up growth can be achieved after initiation of antiretroviral treatment, children who begin treatment in later childhood are typically unable to regain their height potential.67,68 The dissociation between physical development and cognitive and chronological age can cause considerable psychological morbidity among HIV-infected adolescents; stunting and pubertal delay are visible manifestations of HIV infection and lead to stigmatisation and discrimination of those affected.
Neurocognitive disease
Progressive encephalopathy—characterised by a stepwise or continuous deterioration in brain function—is well recognised in HIV-infected infants and young children. Overall neurocognitive function seems to be within the normal range for older survivors of perinatally acquired HIV infection, although studies vary greatly with respect to methods and generally do not contain a control group, making comparison of findings difficult.69,70 Seemingly asymptomatic HIV-infected adolescents do have deficits that are difficult to identify by routine testing. These include shortfalls in cognitive function, fine motor function, memory, perceptual performance, quantitative abilities, and mental processing and language abilities.70 Data for the effect of antiretroviral treatment on neurocognitive outcomes are conflicting and suggest that children who receive antiretroviral drugs in infancy or before the onset of symptoms are likely to have better outcomes than are those who access treatment at an older age.71–73 Despite treatment with antiretroviral drugs, subtle defects persist and have important implications for adolescents, particularly with respect to adherence to medication, education and career planning, risk behaviours, and overall quality of life.73,74
Skin disease
Skin disease is one of the most common manifestations of HIV infection, and adolescents are affected disproportionately. In a series of 301 young adults admitted to hospital in Harare, those with dermatological abnormalities were 37 times more likely to have HIV infection; furthermore, 70% of HIV-infected adolescents had two or more skin manifestations, a higher proportion than that reported in studies of HIV-infected younger children and adults.75 HIV-infected adolescents typically report a history of non-specific recurrent rashes occurring throughout childhood. Common manifestations include papular pruritic eruption, angular cheilitis, molluscum contagiosum, herpes zoster, and common warts (verruca vulgaris). Moreover, diffuse planar warts—prominent on the face and in other sun-exposed areas of the body—are noted frequently in young people with HIV infection and are typically extensive and stigmatising. Histology and HPV types accord with epidermodysplasia verruciformis, a potentially premalignant condition, and little improvement takes place with antiretroviral treatment, despite immune reconstitution.76 Use of topical glycolic acid can speed resolution.77 Other skin manifestations improve with antiretroviral treatment, although transient worsening or initial presentation might be associated with immune reconstitution.78,79 Similar to growth failure, skin disease is a visible manifestation of HIV infection and—in areas with a high prevalence of HIV—is associated widely with having the infection, resulting in affected children being severely stigmatised (figure 2).
Renal and bone disease
HIV-associated nephropathy is thought to be due to direct infection of renal epithelial cells.80 Similar to other chronic complications, risk of HIV-associated nephropathy increases with age; moreover, African people might be at particularly high risk because of the augmented frequency of APOL1 gene variants in this population, which have been associated with HIV-associated nephropathy in African cohorts.81 HIV infection is also associated with decreased bone-mineral content and density.82,83 Factors contributing to low bone density in HIV-infected adolescents include advanced HIV disease, renal disease, vitamin D deficiency, malabsorption, longstanding chronic HIV-mediated inflammation, stunted growth, low body mass, and delayed puberty. Adolescence is an important period for bone-mineral acquisition, and compromised bone mass can increase the risk of premature osteoporosis.84 Although antiretroviral treatment significantly reduces the risk of kidney disease and is beneficial to bone growth, tenofovir—recommended in first-line regimens for HIV treatment—can cause proximal renal tubular toxic effects and decreased bone-mineral density. The toxic effects of tenofovir are relatively uncommon in adults. However, the risk of adverse effects of tenofovir may be higher in children and adolescents because of their immature physiology and ongoing bone growth.
Limitations of existing studies
Few data have been published on the range, epidemiology, and pathogenesis of chronic disorders associated with HIV infection in adolescents. Studies to date are limited by their cross-sectional nature, small sample sizes, and absence of controls. Much research has been undertaken in high-income settings, in the era before antiretroviral treatment was introduced. Studies include a mix of patients—eg, those who have not received antiretroviral drugs before and individuals who have experience of these regimens—and were not disaggregated by age, therefore limiting the generalisability of the findings to HIV-infected adolescents in Africa. Complex clinical issues place heavy demands on already overstretched health-care systems, and optimum screening and management strategies are not well defined
Antiretroviral treatment in adolescence
In their 2013 guidelines for treatment of HIV, WHO recommend earlier initiation of antiretroviral treatment compared with previous guidelines.85 Antiretroviral treatment is recommended up to 5 years of age, regardless of clinical or immunological stage of disease; however, in older children, adolescents, and adults, antiretroviral treatment is deferred until the patient develops WHO stage 3 or 4 HIV disease or the CD4 count drops below 500 cells per μL. Unlike adults, children are infected at a period when the immune system is immature. Compared with adult patients, HIV-driven chronic immune activation in children can lead to premature ageing of the immune system and cause more adverse outcomes on immune health. Delayed treatment also increases the risk of development and progression of end-organ complications in addition to compromising growth potential.67,72
Although earlier access to HIV treatment might help to prevent these complications, antiretroviral treatment itself can lead to side-effects, such as lipodystrophy, hyperlipidaemia, and insulin resistance.67,71,86,87 Use of tenofovir is likely to rise now it is available as a fixed-drug combination for once-daily dosing. The potential risk of tenofovir-related renal and bone toxic effects have been highlighted as a concern by WHO, and recommendations for monitoring of children and prepubertal adolescents receiving tenofovir have been developed.85,88
In the 2013 WHO HIV guidelines, the antiretroviral regimens and dosing schedules recommended for adults are also recommended for adolescents heavier than 35 kg. Although this guideline harmonises treatment across age groups, data for the pharmacokinetics of drugs in adolescents are sparse. Pubertal changes and growth delay can affect drug metabolism, and the optimum period when the change from weight-based to age-based dosing should occur is not clear, with a potential risk of under-dosing or over-dosing.89
Psychosocial issues and mental health
Over and above HIV-related issues that are common to any age group, HIV-infected adolescents are likely to face recurrent and cumulative psychological stressors, such as illness and the death of their parents and siblings, responsibility for welfare of younger siblings or other ill family members, stigma and discrimination, the fear of being viewed as abnormal, and confrontation of mortality and an uncertain future.90,91 HIV/AIDS in the family affects the health and wealth of households, thus aggravating pre-existing poverty.92 The orphanhood epidemic has matured alongside the HIV epidemic. Thus, more than 50% of AIDS orphans are adolescents.93,94 Many adverse outcomes of being orphaned have been reported, including loss of effective guidance and supervision, inconsistent care, psychological distress and poor mental health, loss of educational opportunities, impoverishment, increased sexual vulnerability, and high rates of risk taking.95–99 Issues with schooling are also prevalent, such as absenteeism because of illness or clinic appointments, disclosure of HIV status to school officials, and stigmatisation from classmates and teachers.100,101
The emotional effects of coping with HIV infection can be severe, and the frequency of psychiatric admissions among HIV-infected adolescents is significantly higher compared with that in the general paediatric population in high-income countries.102,103 This increase is possibly attributable to a combination of the neuropathological effects of HIV infection and environmental factors.104 In Africa, HIV occurs in the context of social factors such as being orphaned, poverty, and inconsistent guardianship, which results in augmented risk of behavioural problems and psychiatric disorders among adolescents, including post-traumatic stress disorder, depression, and severe anxiety.105–107 Mental health needs typically receive little attention as families struggle to address immediate medical concerns and the social and economic outcomes of HIV.92 These factors ultimately affect an adolescent’s access to HIV care and treatment adherence, undermining the success of antiretroviral regimens.108,109
Adherence to antiretroviral treatment
Many key life events happen during adolescence, including completion of school, initiation of sexual activity, and becoming economically productive. Furthermore, adolescence is typically a period of experimentation and engagement in high-risk behaviours. Unsurprisingly, adolescents with chronic disease show a poorer adherence to treatment than do adults and young children.110–112 Likewise, when compared with younger children and adults, HIV-infected adolescents and young adults consistently have disproportionately higher rates of poor drug adherence and virological failure.113–117 In a study of 154 adolescents and 7622 adults, the rate of optimum treatment adherence declined over time, from 21% at 6 months for adolescents (compared with 41% for adults) to 7% at 24 months (compared with 21%); furthermore, adolescents had a shorter time to viral rebound and were less likely to achieve long-term immunological recovery than were adult patients.113
Correlates of poor treatment adherence in adolescence include being orphaned, lack of knowledge, mental health problems, changes of guardianship, attending school, and absence of parental and social support.109,116,118,119 Delayed disclosure of HIV status to the adolescent, and a resultant lack of autonomy, substantially affect adherence.118 In Uganda, children whose primary caregiver was the only one who knew the child’s HIV status were three times more likely to be non-adherent to antiretroviral treatment.120 By contrast, good adherence to an antiretroviral regimen was associated with an adolescent’s knowledge of their HIV status, valuable social support, and having a strong relationship with parents.121,122 However, even for adolescents with these apparent advantages, structural barriers of stigma and poverty still affect adherence.119 The desire for conformity with peers during adolescence, and a fear of stigmatisation, greatly affects treatment adherence. Antiretroviral treatment is a daily reminder of being HIV-positive, and drug fatigue can result in adolescents stopping the regimen.121 Transition of adolescents from paediatric to adult HIV care services might further disrupt adherence, because the time available for counselling is diminished and health-care providers have little experience of addressing adolescent-specific concerns.123
Outcomes of poor treatment adherence include clinical progression of disease, emergence of drug resistance, and the risk of spreading drug-resistant HIV strains when adolescents become sexually active.124 The importance of addressing adherence in this age group cannot be overemphasised. The high risk of developing drug resistance during this period of life, combined with the fact that patients who began antiretroviral treatment as children will be taking these drugs for a much longer period than will those who were diagnosed as adults, is of grave concern in view of the limited availability of alternative regimens in resource-constrained settings. Additionally, the risk of onward transmission of HIV to a sexual partner is high during adolescence.117 Thus, maintaining adherence during adolescence is crucial not only to ensure sustainability of treatment success but also to prevent HIV transmission.124 An evidence base for effective interventions to support adherence among adolescents in low-income settings is absent. Furthermore, no one intervention to maintain sustained adherence is feasible because the process is dynamic and individual.
Sexual and reproductive health
Adolescents and young adults have been the focus of primary HIV prevention programmes for many years. With growing numbers of HIV-infected children surviving to adolescence and becoming sexually active,125,126 the need for secondary prevention programmes is increasing. Sexual identity-building in adolescence is complex and culturally specific, and sexual behaviours are shaped partly by societal norms.127 Many interventions to reduce sexual risk behaviours have been developed in high-income settings, but these might have scant applicability to African young people.
Some factors put adolescents at especially high risk of transmitting HIV infection, including early sexual debut, having multiple sex partners, being at high risk of sexual violence, and adolescent girls engaging in transactional sex with older men.98,128 Findings of a study at 20 sites in Uganda, of adolescents infected with HIV perinatally, showed low levels of condom use, with 63% of the young people aware of the need to use condoms to prevent HIV infection of their partner or prevention of sexually transmitted infections, but only 30% reporting use.129 Barriers to use of condoms included fear of rejection, peer pressure, poverty, alcohol use, poor negotiation skills, possible disclosure of HIV status through insistence on condom use, ambivalence about becoming a parent, and impulsivity that is characteristic of adolescence.130 Oral and anal sexual intercourse is also reported frequently, as a means to avoid pregnancy and to preserve virginity.131,132
The desire to have children remains strong, independent of HIV status, and a romantic relationship is typically not regarded as legitimate unless it produces a baby.133 The cultural value placed on having children means that adolescents living with HIV engage in early relationships to fulfil their obligation to have children before they die.133 In Uganda, the rate of pregnancy among adolescents living with HIV was similar to that recorded in the general population.133 Of 1238 adolescents in care at the Paediatric Infectious Disease Clinic in Kampala, Uganda, by the end of 2012, 123 girls had become pregnant since 2008 and at least 12 male adolescents had fathered children (unpublished data; S Bakeera-Kitaka, Makerere University College of Health Sciences, Kampala, Uganda). Management of HIV-infected pregnant adolescents poses specific challenges in terms of ensuring that mother-to-child transmission does not occur, decreasing the risk of complications in pregnancy in girls who have comorbidities, lessening the stigma associated with HIV infection, and handling the low levels of disclosure to sexual partners.130,134 Only a few sexually active adolescents report disclosing their HIV status to their current partner (29% in young people age 15–17 years and 42% in adults age 18–19 years).129 Many adolescent pregnancies are unwanted, and termination of pregnancy is sought from unskilled providers.128,135
Awareness of and knowledge about reproductive health, HIV transmission, and contraceptive methods is poor among HIV-infected adolescents.130 Discrepancy between the information given by health-care providers and the actual needs of HIV-infected adolescents is common, with the concerns of young people sometimes not taken into account.136 Health-care providers need to recognise that young people perinatally infected with HIV are sexually active or anticipate being so in the future. HIV care programmes should provide age-appropriate information on prevention of HIV transmission and family-planning and give support about disclosure of HIV status to partners and contraceptive services. Without consistent use, condoms are an ineffective contraceptive, and hormonal contraceptives should, therefore, be considered. Use of hormonal contraceptives does not accelerate disease progression but, as with antiretroviral treatment, adolescents adhere poorly to both condoms and hormonal contraceptives.137,138 Long-acting contraception such as progestogen implants and depots might, therefore, be a pragmatic option for adolescents.138 However, this option must be accompanied by counselling on the use of condoms to prevent onward HIV transmission and acquisition of sexually transmitted infections.
Disclosure of HIV status
Although often deferred in early childhood,139,140 disclosure of HIV status becomes crucial as children approach cognitive maturity and puberty. Young adults have to make decisions about sexual relationships and plan for the future, and these decisions can only be made with an accurate understanding of the nature of their illness.141 Although the benefits of disclosure are considerable, informing a child of his or her own HIV status is often delayed. Furthermore, deferring disclosure can adversely affect treatment adherence and psychological well-being and might affect family functioning and the adolescent’s social and academic life.120,121,142–145 Delays to the initiation of the process of disclosure increase the difficulty of the eventual revelation. In a study from Kinshasa, Democratic Republic of the Congo, the median age at disclosure of HIV status was 15 years.146 A child who discovers their HIV status will have many questions about the implications of being HIV-positive and of having HIV in the family, which unfold over time. Adolescents actively desire direct communication with their caregivers about their HIV status, but most adults are ill-equipped to handle this process positively and, thus, prefer to manage HIV infection in silence.146,147
Study findings highlight the contextual challenges faced by caregivers in disclosing the HIV status to a child. Reluctance of parents to reveal HIV status is typically attributable to a desire to protect their child from psychological distress, to prevent disclosure of the mother’s HIV status, and to avoid not only having to address their own feelings of guilt at having infected their child but also possible blame from their child.148–150 Other barriers include the fear of discrimination and stigma toward both the adolescent and the family as a whole.150,151
The process of disclosure to children poses several difficulties. Sometimes confusion arises about whether the health-care provider or the caregiver should disclose the information to the child.149,151,152 Despite recommendations for a developmentally appropriate and incremental process of disclosure, with ongoing support to address questions that arise, caregivers and health-care workers typically think of disclosure as a discrete event.153 Adolescents report that disclosure is usually a one-point event and that they are not given opportunities to ask questions.154 Health-care workers sometimes do not have the skills necessary to help caregivers and families deal with the complex issues associated with revealing HIV status to an infected child. With many children receiving antiretroviral treatment through busy clinics, practical approaches to supporting disclosure with limited time and staffing are needed.
Recommendations for policy and research
Service provision has been affected adversely by an underappreciation of the burden of surviving adolescents living with HIV in Africa and the morbidity associated with HIV in this age group. Strategies to enable earlier identification of HIV infection of children with slow-progressing disease need to be implemented urgently. Specific issues should be taken into account by policy makers: informed consent, confidentiality, and autonomy in a group with evolving capacities; training of health-care providers; and provision of quality care beyond centres of excellence to accessible low-level health-care settings. A global effort, led by WHO and UNICEF, has been initiated to respond to the needs of this previously neglected group of young adults, and guidelines on HIV testing and care have been developed.155,156 Panel 1 outlines suggestions for interventions and research priorities aimed at addressing issues pertinent to the emerging adolescent HIV epidemic. Many concerns—such as disclosure, adherence, stigma, and transitioning—can be extrapolated to other chronic illnesses in adolescence, and development of policies to address these issues is an opportunity to address the broader agenda of chronic illness in adolescence.
In Africa, dedicated health-care services for young people are the exception rather than the rule, and little or no provision has been made for the special needs of this age group. Without appropriately tailored services, adolescents are likely to fall through the cracks of paediatric-based or adult-orientated HIV care. There is an urgent need to develop and rapidly implement policies and programmes aimed at early diagnosis and improvement of care provided to the expanding numbers of adolescents who are growing up with HIV. A model that integrates HIV clinical care with sexual and reproductive health and psychological, educational, and social services (panel 2) will help to prepare young adults for an independent and productive future and reduce the effect of this devastating epidemic at community and societal level.155 As these children take an important step towards adulthood, they deserve our support, encouragement, and investment to live their life to its full potential.
Panel 1: Suggested interventions and research priorities.
Population-based epidemiology
Epidemiology of HIV infection in adolescents
Modelling the effect of strategies to prevent mother-to-child transmission and antiretroviral treatment on the paediatric HIV epidemic
Identification of competing causes of childhood mortality: malaria, poor sanitation, and unclean drinking water are potential disproportionate hazards for the survival of HIV-infected children
Surveillance of HIV infection: inclusion of children and adolescents in demographic health surveys (currently include individuals older than 15 years) and population-based surveys
Reporting of HIV epidemiological data in finer age-bands—eg, 0–5 years, 6–10 years, 11–15 years, 16–19 years
Earlier identification of HIV-infected individuals with slow-progressing disease
Screening algorithms to define at-risk adolescents157
Community-based HIV-testing approaches, including school-based testing, testing at community outlets (eg, churches), home-based testing, self-testing, and voluntary counselling and testing sites85,155
Ethics of HIV-testing—eg, age of consent, testing for adolescents without caregivers
Context-specific strategies to improve links to HIV care
HIV care
How can virological outcomes after antiretroviral treatment be improved?
Promotion of retention in care and adherence—eg, integration of HIV testing and care services, peer-led support, adherence clubs, economic enablers, community-based provision of antiretroviral treatment, once-daily dosing, mobile phone technologies, managed problem-solving, point-of-care CD4 count112,158–160
Pharmacokinetic studies in adolescents, to define optimum dosing in relation to stunting and pubertal delay
Strategies for preservation of long-term treatment options—eg, holding regimens, structured treatment interruption
Chronic complications of HIV infection
Earlier initiation of antiretroviral treatment to prevent complications
Interventions for lung and heart disease: corticosteroids, inhaled or oral antibiotics, preventive treatment for tuberculosis, phosphodiesterase inhibitors
Investigation of neurocognitive deficits
Screening and management strategies for chronic complications and long-term toxic effects appropriate for low-income settings88
Implementation of human papillomavirus vaccination
Reproductive and sexual health
Mother and child outcomes in individuals who have children: potential for high maternal mortality and risk of HIV to child
Effectiveness of antiretroviral treatment for prevention of second-generation perinatal HIV transmission in view of the potential for transmission of HIV that is resistant to one or more classes of antiretroviral drug
Strategies to reduce risky behaviour
Strategies to prevent onward transmission—eg, male circumcision, health education, pre-exposure prophylaxis
Psychosocial and mental health
Strategies directed at health providers, families, teachers and HIV-infected adolescents to manage stigma
Providing life-skills and vocational support
Optimum disclosure strategies161
Age-appropriate and culturally valid screening and management of mental health problems
Biomedical research
Host and viral attributes
Genetic and immunological correlates of slow progression of HIV infection
Pathogenesis of chronic complications
Panel 2: Components of a comprehensive care package for HIV-infected adolescents.
Early identification of HIV infection and linkage to care
Strengthened facility-based testing: opt-out testing in inpatient and outpatient departments, and testing within sexual and reproductive health-care and primary-care services
Family-based testing: testing all children whose parents and natural siblings are infected with HIV
Integrated testing and care services—eg, tuberculosis care, sexual and reproductive health care, decentralised HIV care
Prevention and management of chronic complications
Timely institution of antiretroviral treatment
Monitoring for chronic clinical complications: growth assessment, lung and cardiac function, learning disabilities, renal disease, dyslipidaemia
Referral to clinical specialties for investigation and management of systemic complications
Liaison with disability rehabilitation services
Human papillomavirus vaccination and cervical screening after sexual debut
Psychosocial and mental health
Regular assessment of psychosocial status: schooling, guardianship, bereavement
Screening and treatment for depression
Counselling for caregivers of HIV-infected children
Training for teachers about management of confidentiality and discrimination, and communication with caregivers
Training for health-care workers about adolescent development and adolescent-centred counselling
Attention to autonomy and confidentiality by health-care workers
Linkage to community-based psychosocial support services
Services to address sexual abuse and economic exploitation
Adherence support
Simplified antiretroviral treatment regimens: once-daily dosing, fixed-drug combinations
Education about antiretroviral treatment using age-appropriate methods
Counselling that uses a problem-solving approach and addresses psychosocial context
Use of peer or paraprofessional treatment supporters
Use of reminder devices and communication technologies with an interactive component
Sexual and reproductive health
Screening for sexually transmitted infections after sexual debut
Training on condom use, and provision of condoms and contraception
Age-appropriate counselling on family-planning and prospects of having children
Disclosure of HIV status
Timely and developmentally appropriate disclosure of HIV status
Ongoing post-disclosure support
Joint involvement of health-care workers and caregivers in disclosure process
Transition from paediatric to adult care services
Liaison between paediatric and adult clinical staff before transition
Search strategy and selection criteria.
We searched PubMed for articles published from January, 1990, to September, 2013, with MeSH terms for HIV, Africa, and “adolescents”, and with MeSH and related terms for specific topic areas (eg, “disclosure”, “lung disease”). We also looked for relevant publications among our personal files and searched Google scholar and abstracts from meetings of the International AIDS Society and the Conference on Retroviruses and Opportunistic Infections. Articles resulting from these searches and relevant references cited in those articles were reviewed. We did not set any language limits.
Acknowledgments
We thank Bruce Dick and Robert Miller for helpful comments on the manuscript. RAF is funded by the Wellcome Trust through an intermediate fellowship (095878/Z/11/Z). EL is funded by an NIMH K23 career development award (MH095669); her research is also supported by a CDC/PEPFAR public health effectiveness research grant. The funders had no role in the writing of this Review or in the decision to submit for publication.
Footnotes
Contributors SB-K wrote the section on sexual health. TM wrote the psychosocial issues section. EDL wrote clinical, adherence, and disclosure sections. RAF had the idea for the Review, wrote the policy, epidemiology, and clinical sections, and provided the clinical pictures. JC and KG did the literature search.
Conflicts of interest We declare that we have no conflicts of interest.
References
- 1.Joint United Nations Programme on HIV/AIDS (UNAIDS) [accessed Nov 28, 2013];UNAIDS report on the global AIDS epidemic 2013. 2013 Nov; http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf.
- 2.Dabis F, Ekpini ER. HIV-1/AIDS and maternal and child health in Africa. Lancet. 2002;359:2097–104. doi: 10.1016/S0140-6736(02)08909-2. [DOI] [PubMed] [Google Scholar]
- 3.WHO. UNAIDS. UNICEF [accessed Nov 28, 2013];Towards universal access: scaling up priority HIV/AIDS interventions in the health sector—progress report 2010. 2010 Sep 28; http://whqlibdoc.who.int/publications/2010/9789241500395_eng.pdf. [Google Scholar]
- 4.Hazra R, Siberry GK, Mofenson LM. Growing up with HIV: children, adolescents, and young adults with perinatally acquired HIV infection. Annu Rev Med. 2010;61:169–85. doi: 10.1146/annurev.med.050108.151127. [DOI] [PubMed] [Google Scholar]
- 5.Sohn AH, Hazra R. The changing epidemiology of the global paediatric HIV epidemic: keeping track of perinatally HIV-infected adolescents. J Int AIDS Soc. 2013;16:18555. doi: 10.7448/IAS.16.1.18555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newell M-L, Coovadia H, Cortina-Borja M, Rollins N, Gaillard P, Dabis F, for the Ghent International AIDS Society (IAS) working group on HIV infection in women and children Mortality of infected and uninfected infants born to HIV-infected mothers in Africa: a pooled analysis. Lancet. 2004;364:1236–43. doi: 10.1016/S0140-6736(04)17140-7. [DOI] [PubMed] [Google Scholar]
- 7.Fatti G, Bock P, Eley B, Mothibi E, Grimwood A. Temporal trends in baseline characteristics and treatment outcomes of children starting antiretroviral treatment: an analysis in four provinces in South Africa, 2004–2009. J Acquir Immune Defic Syndr. 2011;58:e60–67. doi: 10.1097/QAI.0b013e3182303c7e. [DOI] [PubMed] [Google Scholar]
- 8.van Dijk JH, Sutcliffe CG, Munsanje B, et al. HIV-infected children in rural Zambia achieve good immunologic and virologic outcomes two years after initiating antiretroviral therapy. PLoS One. 2011;6:e19006. doi: 10.1371/journal.pone.0019006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferrand R, Lowe S, Whande B, et al. Survey of children accessing HIV services in a high prevalence setting: time for adolescents to count? Bull World Health Organ. 2010;88:428–34. doi: 10.2471/BLT.09.066126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferrand RA, Luethy R, Bwakura F, Mujuru H, Miller RF, Corbett EL. HIV infection presenting in older children and adolescents: a case series from Harare, Zimbabwe. Clin Infect Dis. 2007;44:874–78. doi: 10.1086/511873. [DOI] [PubMed] [Google Scholar]
- 11.Walker AS, Mulenga V, Sinyinza F, et al. the CHAP trial team Determinants of survival without antiretroviral therapy after infancy in HIV-1-infected Zambian children in the CHAP trial. J Acquir Immune Defic Syndr. 2006;42:637–45. doi: 10.1097/01.qai.0000226334.34717.dc. [DOI] [PubMed] [Google Scholar]
- 12.Ferrand RA, Corbett EL, Wood R, et al. AIDS among older children and adolescents in southern Africa: projecting the time course and magnitude of the epidemic. AIDS. 2009;23:2039–46. doi: 10.1097/QAD.0b013e32833016ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marston M, Becquet R, Zaba B, et al. Net survival of perinatally and postnatally HIV-infected children: a pooled analysis of individual data from sub-Saharan Africa. Int J Epidemiol. 2011;40:385–96. doi: 10.1093/ije/dyq255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gray L, Newell ML, Thorne C, Peckham C, Levy J, the European Collaborative Study Fluctuations in symptoms in human immunodeficiency virus-infected children: the first 10 years of life. Pediatrics. 2001;108:116–22. doi: 10.1542/peds.108.1.116. [DOI] [PubMed] [Google Scholar]
- 15.Commenges D, Alioum A, Lepage P, Van de Perre P, Msellati P, Dabis F. Estimating the incubation period of paediatric AIDS in Rwanda. AIDS. 1992;6:1515–20. doi: 10.1097/00002030-199212000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Brookes H, Shisana O, Richter L. The national household HIV prevalence and risk survey of South African children. Human Social Research Council; Cape Town: 2004. [Google Scholar]
- 17.National AIDS Coordinating Agency . Second Botswana AIDS Impact Survey (BAIS II) Government of Botswana; Botswana: 2005. [Google Scholar]
- 18.Gomo E, Rusakaniko S, Mashange W, Mutswanga J, Chandiwana B, Munyati S. Household survey of HIV-prevalence and behaviour in Chimanimani District, Zimbabwe. Human Social Research Council; Cape Town: 2005. [Google Scholar]
- 19.Gregson S, Nyamukapa CA, Garnett GP, et al. Sexual mixing patterns and sex-differentials in teenage exposure to HIV infection in rural Zimbabwe. Lancet. 2002;359:1896–903. doi: 10.1016/S0140-6736(02)08780-9. [DOI] [PubMed] [Google Scholar]
- 20.Blokzijl ML. Human immunodeficiency virus infection in childhood. Ann Trop Paediatr. 1988;8:1–17. doi: 10.1080/02724936.1988.11748530. [DOI] [PubMed] [Google Scholar]
- 21.Ferrand RA, Munaiwa L, Matsekete J, et al. Undiagnosed HIV infection among adolescents seeking primary health care in Zimbabwe. Clin Infect Dis. 2010;51:844–51. doi: 10.1086/656361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harrison A, Pierre RB, Palmer P, et al. Clinical manifestations of adolescents with HIV/AIDS in Jamaica. West Indian Med J. 2008;57:257–64. [PubMed] [Google Scholar]
- 23.Marais BJ, Gie RP, Hesseling AH, Beyers N. Adult-type pulmonary tuberculosis in children 10–14 years of age. Pediatr Infect Dis J. 2005;24:743–44. doi: 10.1097/01.inf.0000173305.04212.09. [DOI] [PubMed] [Google Scholar]
- 24.Ferrand RA, Bandason T, Musvaire P, et al. Causes of acute hospitalization in adolescence: burden and spectrum of HIV-related morbidity in a country with an early-onset and severe HIV epidemic: a prospective survey. PLoS Med. 2010;7:e1000178. doi: 10.1371/journal.pmed.1000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meiring ST, Quan VC, Cohen C, et al. the Group for Enteric. Respiratory and Meningeal disease Surveillance in South Africa (GERMS-SA) A comparison of cases of paediatric-onset and adult-onset cryptococcosis detected through population-based surveillance, 2005–2007. AIDS. 2012;26:2307–14. doi: 10.1097/QAD.0b013e3283570567. [DOI] [PubMed] [Google Scholar]
- 26.Marais BJ, Gie RP, Schaaf HS, et al. The clinical epidemiology of childhood pulmonary tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis. 2004;8:278–85. [PubMed] [Google Scholar]
- 27.Wood R, Racow K, Bekker LG, et al. Indoor social networks in a South African township: potential contribution of location to tuberculosis transmission. PLoS One. 2012;7:e39246. doi: 10.1371/journal.pone.0039246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perez-Velez CM, Marais BJ. Tuberculosis in children. N Engl J Med. 2012;367:348–61. doi: 10.1056/NEJMra1008049. [DOI] [PubMed] [Google Scholar]
- 29.Ferrand RA, Desai SR, Hopkins C, et al. Chronic lung disease in adolescents with delayed diagnosis of vertically acquired HIV infection. Clin Infect Dis. 2012;55:145–52. doi: 10.1093/cid/cis271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morris L, Posada R, Hickman C, et al. Susceptibility to measles among perinatally HIV-infected adolescents and young adults. Presented at AIDS 2012, the XIX International AIDS Conference; Washington, DC, USA. July 22–27, 2012; [accessed Nov 28, 2013]. http://pag.aids2012.org/EPosterHandler.axd?aid=14088. [Google Scholar]
- 31.Moss WJ, Scott S, Mugala N, et al. Immunogenicity of standard-titer measles vaccine in HIV-1-infected and uninfected Zambian children: an observational study. J Infect Dis. 2007;196:347–55. doi: 10.1086/519169. [DOI] [PubMed] [Google Scholar]
- 32.Aurpibul L, Puthanakit T, Sirisanthana T, Sirisanthana V. Response to measles, mumps, and rubella revaccination in HIV-infected children with immune recovery after highly active antiretroviral therapy. Clin Infect Dis. 2007;45:637–42. doi: 10.1086/520651. [DOI] [PubMed] [Google Scholar]
- 33.L’Huillier AG, Ferry T, Courvoisier DS, et al. the Pediatric Infectious Diseases Group of Switzerland. the Group of Switzerland (PIGS) the Swiss HIV Cohort Study (SHCS) the Swiss Mother & Child HIV Cohort Study (MoCHiV) Impaired antibody memory to varicella zoster virus in HIV-infected children: low antibody levels and avidity. HIV Med. 2012;13:54–61. doi: 10.1111/j.1468-1293.2011.00936.x. [DOI] [PubMed] [Google Scholar]
- 34.Wolf ER, Wirth KE, Ho-Foster A, et al. The effect of measles on disease markers in HIV + children and adolescents living in Botswana. Presented at AIDS 2012, the XIX International AIS Conference; Washington, DC, USA. July 22–27, 2012; [accessed Nov 28, 2013]. http://pag.aids2012.org/EPosterHandler.axd?aid=14589. [Google Scholar]
- 35.Mutwa PR, Boer KR, Rusine JB, et al. Hepatitis B virus prevalence and vaccine response in HIV-infected children and adolescents on combination antiretroviral therapy in Kigali, Rwanda. Pediatr Infect Dis J. 2013;32:246–51. doi: 10.1097/INF.0b013e318271b93d. [DOI] [PubMed] [Google Scholar]
- 36.van Bogaert LJ. Age at diagnosis of preinvasive and invasive cervical neoplasia in South Africa: HIV-positive versus HIV-negative women. Int J Gynecol Cancer. 2011;21:363–66. doi: 10.1097/IGC.0b013e3182094d78. [DOI] [PubMed] [Google Scholar]
- 37.Watson-Jones D, Baisley K, Brown J, et al. High prevalence and incidence of human papillomavirus in a cohort of healthy young African female subjects. Sex Transm Infect. 2013;89:358–65. doi: 10.1136/sextrans-2012-050685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Katz IT, Nkala B, Dietrich J, et al. A qualitative analysis of factors influencing HPV vaccine uptake in Soweto, South Africa among adolescents and their caregivers. PLoS One. 2013;8:e72094. doi: 10.1371/journal.pone.0072094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Firnhaber C, Wilkin T. Human papillomavirus vaccines: where do they fit in HIV-infected individuals? Curr HIV/AIDS Rep. 2012;9:278–86. doi: 10.1007/s11904-012-0128-6. [DOI] [PubMed] [Google Scholar]
- 40.Serraino D, Franceschi S. Kaposi’s sarcoma and non-Hodgkin’s lymphomas in children and adolescents with AIDS. AIDS. 1996;10:643–47. doi: 10.1097/00002030-199606000-00010. [DOI] [PubMed] [Google Scholar]
- 41.Athale UH, Patil PS, Chintu C, Elem B. Influence of HIV epidemic on the incidence of Kaposi’s sarcoma in Zambian children. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;8:96–100. [PubMed] [Google Scholar]
- 42.Tukei VJ, Kekitiinwa A, Beasley RP. Prevalence and outcome of HIV-associated malignancies among children. AIDS. 2011;25:1789–93. doi: 10.1097/QAD.0b013e3283498115. [DOI] [PubMed] [Google Scholar]
- 43.Gantt S, Kakuru A, Wald A, et al. Clinical presentation and outcome of epidemic Kaposi sarcoma in Ugandan children. Pediatr Blood Cancer. 2010;54:670–74. doi: 10.1002/pbc.22369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mueller BU. Cancers in children infected with the human immunodeficiency virus. Oncologist. 1999;4:309–17. [PubMed] [Google Scholar]
- 45.Moore SW, Davidson A, Hadley GP, et al. Malignant liver tumors in South African children: a national audit. World J Surg. 2008;32:1389–95. doi: 10.1007/s00268-008-9526-8. [DOI] [PubMed] [Google Scholar]
- 46.Ramdial PK, Sing Y, Deonarain J, Hadley GP, Singh B. Dermal Epstein Barr virus-associated leiomyosarcoma: tocsin of acquired immunodeficiency syndrome in two children. Am J Dermatopathol. 2011;33:392–96. doi: 10.1097/DAD.0b013e3181e5d16a. [DOI] [PubMed] [Google Scholar]
- 47.Mangeya N, Mafukidze AT, Pascoe M, et al. Cholangiocarcinoma presenting in an adolescent with vertically acquired HIV infection. Int J STD AIDS. 2008;19:717–18. doi: 10.1258/ijsa.2008.008078. [DOI] [PubMed] [Google Scholar]
- 48.Jeena PM, Coovadia HM, Thula SA, Blythe D, Buckels NJ, Chetty R. Persistent and chronic lung disease in HIV-1 infected and uninfected African children. AIDS. 1998;12:1185–93. doi: 10.1097/00002030-199810000-00011. [DOI] [PubMed] [Google Scholar]
- 49.Zar HJ. Chronic lung disease in human immunodeficiency virus (HIV) infected children. Pediatr Pulmonol. 2008;43:1–10. doi: 10.1002/ppul.20676. [DOI] [PubMed] [Google Scholar]
- 50.Sharland M, Gibb DM, Holland F. Respiratory morbidity from lymphocytic interstitial pneumonitis (LIP) in vertically acquired HIV infection. Arch Dis Child. 1997;76:334–36. doi: 10.1136/adc.76.4.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Weber HC, Gie RP, Cotton MF. The challenge of chronic lung disease in HIV-infected children and adolescents. J Int AIDS Soc. 2013;16:18633. doi: 10.7448/IAS.16.1.18633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rylance J, Mwalukomo T, Rylance S, et al. Lung function and bronchodilator response in perinatally HIV-infected Malawian adolescents. Presented at the 19th Conference on Retroviruses and Opportunistic Infections; Seattle, WA, USA. March 5–8, 2012. [Google Scholar]
- 53.Lynch JP, III, Weigt SS, DerHovanessian A, Fishbein MC, Gutierrez A, Belperio JA. Obliterative (constrictive) bronchiolitis. Semin Respir Crit Care Med. 2012;33:509–32. doi: 10.1055/s-0032-1325161. [DOI] [PubMed] [Google Scholar]
- 54.Colom AJ, Teper AM, Vollmer WM, Diette GB. Risk factors for the development of bronchiolitis obliterans in children with bronchiolitis. Thorax. 2006;61:503–06. doi: 10.1136/thx.2005.044909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lubega S, Zirembuzi GW, Lwabi P. Heart disease among children with HIV/AIDS attending the paediatric infectious disease clinic at Mulago Hospital. Afr Health Sci. 2005;5:219–26. doi: 10.5555/afhs.2005.5.3.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Okoromah CA, Ojo OO, Ogunkunle OO. Cardiovascular dysfunction in HIV-infected children in a sub-Saharan African country: comparative cross-sectional observational study. J Trop Pediatr. 2012;58:3–11. doi: 10.1093/tropej/fmr009. [DOI] [PubMed] [Google Scholar]
- 57.Brown SC, Schoeman CJ, Bester CJ. Cardiac findings in children admitted to a hospital general ward in South Africa: a comparison of HIV-infected and uninfected children. Cardiovasc J S Afr. 2005;16:206–10. [PubMed] [Google Scholar]
- 58.Lipshultz SE, Miller TL, Wilkinson JD, et al. Cardiac effects in perinatally HIV-infected and HIV-exposed but uninfected children and adolescents: a view from the United States of America. J Int AIDS Soc. 2013;16:18597. doi: 10.7448/IAS.16.1.18597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Miller RF, Kaski JP, Hakim J, et al. Cardiac disease in adolescents with delayed diagnosis of vertically-acquired HIV infection. Clin Infect Dis. 2013;56:576–82. doi: 10.1093/cid/cis911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Barlow-Mosha L, Eckard AR, McComsey GA, Musoke PM. Metabolic complications and treatment of perinatally HIV-infected children and adolescents. J Int AIDS Soc. 2013;16:18600. doi: 10.7448/IAS.16.1.18600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Buchacz K, Rogol AD, Lindsey JC, et al. the Pediatric AIDS Clinical Trials Group 219 Study Team Delayed onset of pubertal development in children and adolescents with perinatally acquired HIV infection. J Acquir Immune Defic Syndr. 2003;33:56–65. doi: 10.1097/00126334-200305010-00009. [DOI] [PubMed] [Google Scholar]
- 62.de Martino M, Tovo PA, Galli L, et al. the Italian Register for HIV infection in Children Puberty in perinatal HIV-1 infection: a multicentre longitudinal study of 212 children. AIDS. 2001;15:1527–34. doi: 10.1097/00002030-200108170-00010. [DOI] [PubMed] [Google Scholar]
- 63.Majaliwa ES, Mohn A, Chiarelli F. Growth and puberty in children with HIV infection. J Endocrinol Invest. 2009;32:85–90. doi: 10.1007/BF03345686. [DOI] [PubMed] [Google Scholar]
- 64.Williams PL, Abzug MJ, Jacobson DL, et al. the International Maternal Pediatric and Adolescent AIDS Clinical Trials P219219C Study and the Pediatric HIVAIDS Cohort Study Pubertal onset in children with perinatal HIV infection in the era of combination antiretroviral treatment. AIDS. 2013;27:1959–70. doi: 10.1097/QAD.0b013e328361195b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Arpadi SM. Growth failure in children with HIV infection. J Acquir Immune Defic Syndr. 2000;25(suppl 1):S37–42. doi: 10.1097/00042560-200010001-00006. [DOI] [PubMed] [Google Scholar]
- 66.Kekitiinwa A, Lee KJ, Walker AS, et al. the Collaborative HIV Paediatric Study (CHIPS) Steering Committe. the Mulago Cohort Team Differences in factors associated with initial growth, CD4, and viral load responses to ART in HIV-infected children in Kampala, Uganda, and the United Kingdom/Ireland. J Acquir Immune Defic Syndr. 2008;49:384–92. doi: 10.1097/QAI.0b013e31818cdef5. [DOI] [PubMed] [Google Scholar]
- 67.Gsponer T, Weigel R, Davies MA, et al. the IeDEA Southern Africa Variability of growth in children starting antiretroviral treatment in southern Africa. Pediatrics. 2012;130:e966–77. doi: 10.1542/peds.2011-3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bakeera-Kitaka S, McKellar M, Snider C, et al. [accessed Nov 28, 2013];Antiretroviral therapy for HIV-1 infected adolescents in Uganda: assessing the impact on growth and sexual maturation. J Pediatr Infect Dis. 2008 3:97–104. http://iospress.metapress.com/content/j668135704616802/ [Google Scholar]
- 69.Bagenda D, Nassali A, Kalyesubula I, et al. Health, neurologic, and cognitive status of HIV-infected, long-surviving, and antiretroviral-naive Ugandan children. Pediatrics. 2006;117:729–40. doi: 10.1542/peds.2004-2699. [DOI] [PubMed] [Google Scholar]
- 70.Laughton B, Cornell M, Boivin M, Van Rie A. Neurodevelopment in perinatally HIV-infected children: a concern for adolescence. J Int AIDS Soc. 2013;16:18603. doi: 10.7448/IAS.16.1.18603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Laughton B, Cornell M, Grove D, et al. Early antiretroviral therapy improves neurodevelopmental outcomes in infants. AIDS. 2012;26:1685–90. doi: 10.1097/QAD.0b013e328355d0ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Puthanakit T, Ananworanich J, Vonthanak S, et al. the PREDICT Study Group Cognitive function and neurodevelopmental outcomes in HIV-infected children older than 1 year of age randomized to early versus deferred antiretroviral therapy: the PREDICT neurodevelopmental study. Pediatr Infect Dis J. 2013;32:501–08. doi: 10.1097/INF.0b013e31827fb19d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Le Doaré K, Bland R, Newell ML. Neurodevelopment in children born to HIV-infected mothers by infection and treatment status. Pediatrics. 2012;130:e1326–44. doi: 10.1542/peds.2012-0405. [DOI] [PubMed] [Google Scholar]
- 74.Puthanakit T, Aurpibul L, Louthrenoo O, et al. Poor cognitive functioning of school-aged children in thailand with perinatally acquired HIV infection taking antiretroviral therapy. AIDS Patient Care STDS. 2010;24:141–46. doi: 10.1089/apc.2009.0314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lowe S, Ferrand RA, Morris-Jones R, et al. Skin disease among human immunodeficiency virus-infected adolescents in Zimbabwe: a strong indicator of underlying HIV infection. Pediatr Infect Dis J. 2010;29:346–51. doi: 10.1097/INF.0b013e3181c15da4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lowe SM, Katsidzira L, Meys R, et al. Acquired epidermodysplasia verruciformis due to multiple and unusual HPV infection among vertically-infected, HIV-positive adolescents in Zimbabwe. Clin Infect Dis. 2012;54:e119–23. doi: 10.1093/cid/cis118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Moore RL, de Schaetzen V, Joseph M, et al. Acquired epidermodysplasia verruciformis syndrome in HIV-infected pediatric patients: prospective treatment trial with topical glycolic acid and human papillomavirus genotype characterization. Arch Dermatol. 2012;148:128–30. doi: 10.1001/archdermatol.2011.268. [DOI] [PubMed] [Google Scholar]
- 78.Seoane Reula E, Bellon JM, Gurbindo D, Muñoz-Fernandez MA. Role of antiretroviral therapies in mucocutaneous manifestations in HIV-infected children over a period of two decades. Br J Dermatol. 2005;153:382–89. doi: 10.1111/j.1365-2133.2005.06758.x. [DOI] [PubMed] [Google Scholar]
- 79.Amerson EH, Maurer TA. Immune reconstitution inflammatory syndrome and tropical dermatoses. Dermatol Clin. 2011;29:39–43. doi: 10.1016/j.det.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 80.Bhimma R, Purswani MU, Kala U. Kidney disease in children and adolescents with perinatal HIV-1 infection. J Int AIDS Soc. 2013;16:18596. doi: 10.7448/IAS.16.1.18596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Genovese G, Friedman DJ, Ross MD, et al. Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science. 2010;329:841–45. doi: 10.1126/science.1193032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Arpadi SM, Horlick M, Thornton J, Cuff PA, Wang J, Kotler DP. Bone mineral content is lower in prepubertal HIV-infected children. J Acquir Immune Defic Syndr. 2002;29:450–54. doi: 10.1097/00126334-200204150-00004. [DOI] [PubMed] [Google Scholar]
- 83.O’Brien KO, Razavi M, Henderson RA, Caballero B, Ellis KJ. Bone mineral content in girls perinatally infected with HIV. Am J Clin Nutr. 2001;73:821–26. doi: 10.1093/ajcn/73.4.821. [DOI] [PubMed] [Google Scholar]
- 84.Puthanakit T, Siberry GK. Bone health in children and adolescents with perinatal HIV infection. J Int AIDS Soc. 2013;16:18575. doi: 10.7448/IAS.16.1.18575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.WHO [accessed Nov 28, 2013];Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. 2013 Jun; http://apps.who.int/iris/bitstream/10665/85321/1/9789241505727_eng.pdf. [PubMed]
- 86.Innes S, Cotton MF, Haubrich R, et al. High prevalence of lipoatrophy in pre-pubertal South African children on antiretroviral therapy: a cross-sectional study. BMC Pediatr. 2012;12:183. doi: 10.1186/1471-2431-12-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lipshultz SE, Williams PL, Wilkinson JD, et al. the Pediatric HIV/AIDS Cohort Study (PHACS) Cardiac status of children infected with human immunodeficiency virus who are receiving long-term combination antiretroviral therapy: results from the Adolescent Master Protocol of the Multicenter Pediatric HIV/AIDS Cohort Study. JAMA Pediatr. 2013;167:520–27. doi: 10.1001/jamapediatrics.2013.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.WHO. HIV/AIDS Programme [accessed Nov 28, 2013];Technical update on treatment optimization: use of tenofovir in HIV-infected children and adolescents—a public health perspective. 2012 Jun; http://apps.who.int/iris/bitstream/10665/70944/1/9789241503822_eng.pdf.
- 89.Rakhmanina NY, van den Anker JN, Soldin SJ, van Schaik RH, Mordwinkin N, Neely MN. Can therapeutic drug monitoring improve pharmacotherapy of HIV infection in adolescents? Ther Drug Monit. 2010;32:273–81. doi: 10.1097/FTD.0b013e3181dca14b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nyamukapa CA, Gregson S, Lopman B, et al. HIV-associated orphanhood and children’s psychosocial distress: theoretical framework tested with data from Zimbabwe. Am J Public Health. 2008;98:133–41. doi: 10.2105/AJPH.2007.116038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Petersen I, Bhana A, Myeza N, et al. Psychosocial challenges and protective influences for socio-emotional coping of HIV+ adolescents in South Africa: a qualitative investigation. AIDS Care. 2010;22:970–78. doi: 10.1080/09540121003623693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bachmann MO, Booysen FL. Health and economic impact of HIV/AIDS on South African households: a cohort study. BMC Public Health. 2003;3:14. doi: 10.1186/1471-2458-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.UNAIDS. UNICEF. USAID [accessed Nov 28, 2013];Children on the brink 2004: a joint report of new orphan estimates and a framework for action. 2004 Jul; http://www.unicef.org/publications/cob_layout6-013.pdf.
- 94.Monasch R, Boerma JT. Orphanhood and childcare patterns in sub-Saharan Africa: an analysis of national surveys from 40 countries. AIDS. 2004;18(suppl 2):S55–65. doi: 10.1097/00002030-200406002-00007. [DOI] [PubMed] [Google Scholar]
- 95.Gregson S, Nyamukapa CA, Garnett GP, et al. HIV infection and reproductive health in teenage women orphaned and made vulnerable by AIDS in Zimbabwe. AIDS Care. 2005;17:785–94. doi: 10.1080/09540120500258029. [DOI] [PubMed] [Google Scholar]
- 96.Nyamukapa CA, Gregson S, Wambe M, et al. Causes and consequences of psychological distress among orphans in eastern Zimbabwe. AIDS Care. 2010;22:988–96. doi: 10.1080/09540121003615061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Nyamukapa C, Gregson S. Extended family’s and women’s roles in safeguarding orphans’ education in AIDS-afflicted rural Zimbabwe. Soc Sci Med. 2005;60:2155–67. doi: 10.1016/j.socscimed.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 98.Cluver L, Orkin M, Boyes M, Gardner F, Meinck F. Transactional sex amongst AIDS-orphaned and AIDS-affected adolescents predicted by abuse and extreme poverty. J Acquir Immune Defic Syndr. 2011;58:336–43. doi: 10.1097/QAI.0b013e31822f0d82. [DOI] [PubMed] [Google Scholar]
- 99.Cluver LD, Orkin M, Gardner F, Boyes ME. Persisting mental health problems among AIDS-orphaned children in South Africa. J Child Psychol Psychiatry. 2012;53:363–70. doi: 10.1111/j.1469-7610.2011.02459.x. [DOI] [PubMed] [Google Scholar]
- 100.Cohen J, Reddington C, Jacobs D, et al. School-related issues among HIV-infected children. Pediatrics. 1997;100:E8. doi: 10.1542/peds.100.1.e8. [DOI] [PubMed] [Google Scholar]
- 101.Cluver L, Bowes L, Gardner F. Risk and protective factors for bullying victimization among AIDS-affected and vulnerable children in South Africa. Child Abuse Negl. 2010;34:793–803. doi: 10.1016/j.chiabu.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 102.Gaughan DM, Hughes MD, Oleske JM, Malee K, Gore CA, Nachman S, the Pediatric AIDS Clinical Trials Group 219C Team Psychiatric hospitalizations among children and youths with human immunodeficiency virus infection. Pediatrics. 2004;113:e544–51. doi: 10.1542/peds.113.6.e544. [DOI] [PubMed] [Google Scholar]
- 103.Mellins CA, Brackis-Cott E, Dolezal C, Abrams EJ. Psychiatric disorders in youth with perinatally acquired human immunodeficiency virus infection. Pediatr Infect Dis J. 2006;25:432–37. doi: 10.1097/01.inf.0000217372.10385.2a. [DOI] [PubMed] [Google Scholar]
- 104.Mellins CA, Malee KM. Understanding the mental health of youth living with perinatal HIV infection: lessons learned and current challenges. J Int AIDS Soc. 2013;16:18593. doi: 10.7448/IAS.16.1.18593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Betancourt TS, Rubin-Smith JE, Beardslee WR, Stulac SN, Fayida I, Safren S. Understanding locally, culturally, and contextually relevant mental health problems among Rwandan children and adolescents affected by HIV/AIDS. AIDS Care. 2011;23:401–12. doi: 10.1080/09540121.2010.516333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Langhaug LF, Pascoe SJ, Mavhu W, et al. High prevalence of affective disorders among adolescents living in rural Zimbabwe. J Community Health. 2010;35:355–64. doi: 10.1007/s10900-010-9261-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Cluver L, Gardner F, Operario D. Poverty and psychological health among AIDS-orphaned children in Cape Town, South Africa. AIDS Care. 2009;21:732–41. doi: 10.1080/09540120802511885. [DOI] [PubMed] [Google Scholar]
- 108.Mellins CA, Brackis-Cott E, Dolezal C, Abrams EJ. The role of psychosocial and family factors in adherence to antiretroviral treatment in human immunodeficiency virus-infected children. Pediatr Infect Dis J. 2004;23:1035–41. doi: 10.1097/01.inf.0000143646.15240.ac. [DOI] [PubMed] [Google Scholar]
- 109.Nyandiko WM, Ayaya S, Nabakwe E, et al. Outcomes of HIV-infected orphaned and non-orphaned children on antiretroviral therapy in western Kenya. J Acquir Immune Defic Syndr. 2006;43:418–25. doi: 10.1097/01.qai.0000243122.52282.89. [DOI] [PubMed] [Google Scholar]
- 110.Borus JS, Laffel L. Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr. 2010;22:405–11. doi: 10.1097/MOP.0b013e32833a46a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Desai M, Oppenheimer JJ. Medication adherence in the asthmatic child and adolescent. Curr Allergy Asthma Rep. 2011;11:454–64. doi: 10.1007/s11882-011-0227-2. [DOI] [PubMed] [Google Scholar]
- 112.Shroufi A, Gunguwo H, Dixon M, et al. HIV-infected adolescents in southern Africa can achieve good treatment outcomes: results from a retrospective cohort study. AIDS. 2013;27:1971–78. doi: 10.1097/QAD.0b013e32836149ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Nachega JB, Hislop M, Nguyen H, et al. Antiretroviral therapy adherence, virologic and immunologic outcomes in adolescents compared with adults in southern Africa. J Acquir Immune Defic Syndr. 2009;51:65–71. doi: 10.1097/QAI.0b013e318199072e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bygrave H, Mtangirwa J, Ncube K, Ford N, Kranzer K, Munyaradzi D. Antiretroviral therapy outcomes among adolescents and youth in rural Zimbabwe. PLoS One. 2012;7:e52856. doi: 10.1371/journal.pone.0052856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Evans D, Menezes C, Mahomed K, et al. Treatment outcomes of HIV-infected adolescents attending public-sector HIV clinics across Gauteng and Mpumalanga, South Africa. AIDS Res Hum Retroviruses. 2013;29:892–900. doi: 10.1089/aid.2012.0215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bakanda C, Birungi J, Mwesigwa R, et al. Survival of HIV-infected adolescents on antiretroviral therapy in Uganda: findings from a nationally representative cohort in Uganda. PLoS One. 2011;6:e19261. doi: 10.1371/journal.pone.0019261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Charles M, Noel F, Leger P, et al. Survival, plasma HIV-1 RNA concentrations and drug resistance in HIV-1-infected Haitian adolescents and young adults on antiretrovirals. Bull World Health Organ. 2008;86:970–77. doi: 10.2471/BLT.07.050120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Haberer JE, Cook A, Walker AS, et al. Excellent adherence to antiretrovirals in HIV+ Zambian children is compromised by disrupted routine, HIV nondisclosure, and paradoxical income effects. PLoS One. 2011;6:e18505. doi: 10.1371/journal.pone.0018505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Biadgilign S, Deribew A, Amberbir A, Deribe K. Barriers and facilitators to antiretroviral medication adherence among HIV-infected paediatric patients in Ethiopia: a qualitative study. SAHARA J. 2009;6:148–54. doi: 10.1080/17290376.2009.9724943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Nabukeera-Barungi N, Kalyesubula I, Kekitiinwa A, Byakika-Tusiime J, Musoke P. Adherence to antiretroviral therapy in children attending Mulago Hospital, Kampala. Ann Trop Paediatr. 2007;27:123–31. doi: 10.1179/146532807X192499. [DOI] [PubMed] [Google Scholar]
- 121.Bikaako-Kajura W, Luyirika E, Purcell DW, et al. Disclosure of HIV status and adherence to daily drug regimens among HIV-infected children in Uganda. AIDS Behav. 2006;10(suppl):S85–93. doi: 10.1007/s10461-006-9141-3. [DOI] [PubMed] [Google Scholar]
- 122.Hodgson I, Ross J, Haamujompa C, Gitau-Mburu D. Living as an adolescent with HIV in Zambia: lived experiences, sexual health and reproductive needs. AIDS Care. 2012;24:1204–10. doi: 10.1080/09540121.2012.658755. [DOI] [PubMed] [Google Scholar]
- 123.Vijayan T, Benin AL, Wagner K, Romano S, Andiman WA. We never thought this would happen: transitioning care of adolescents with perinatally acquired HIV infection from pediatrics to internal medicine. AIDS Care. 2009;21:1222–29. doi: 10.1080/09540120902730054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Attia S, Egger M, Müller M, Zwahlen M, Low N. Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS. 2009;23:1397–404. doi: 10.1097/QAD.0b013e32832b7dca. [DOI] [PubMed] [Google Scholar]
- 125.Levine AB, Aaron E, Foster J. Pregnancy in perinatally HIV-infected adolescents. J Adolesc Health. 2006;38:765–68. doi: 10.1016/j.jadohealth.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 126.Rice E, Batterham P, Rotheram-Borus MJ. Unprotected sex among youth living with HIV before and after the advent of highly active antiretroviral therapy. Perspect Sex Reprod Health. 2006;38:162–67. doi: 10.1363/psrh.38.162.06. [DOI] [PubMed] [Google Scholar]
- 127.Bearinger LH, Sieving RE, Ferguson J, Sharma V. Global perspectives on the sexual and reproductive health of adolescents: patterns, prevention, and potential. Lancet. 2007;369:1220–31. doi: 10.1016/S0140-6736(07)60367-5. [DOI] [PubMed] [Google Scholar]
- 128.Fatusi A, Blum RW. Adolescent health in an international context: the challenge of sexual and reproductive health in sub-Saharan Africa. Adolesc Med State Art Rev. 2009;20:874–86. [PubMed] [Google Scholar]
- 129.Birungi H, Mugisha J, Nyombi J, Obare F, Evelia H, Nyinkavu H. [accessed Nov 28, 2013];Sexual and reproductive health needs of adolescents perinatally infected with HIV in Uganda. 2008 Jul; http://www.popcouncil.org/pdfs/frontiers/FR_FinalReports/Uganda_HIV.pdf. [Google Scholar]
- 130.Bakeera-Kitaka S, Nabukeera-Barungi N, Nöstlinger C, Addy K, Colebunders R. Sexual risk reduction needs of adolescents living with HIV in a clinical care setting. AIDS Care. 2008;20:426–33. doi: 10.1080/09540120701867099. [DOI] [PubMed] [Google Scholar]
- 131.Cherie A, Berhane Y. Oral and anal sex practices among high school youth in Addis Ababa, Ethiopia. BMC Public Health. 2012;12:5. doi: 10.1186/1471-2458-12-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kazaura MR, Masatu MC. Sexual practices among unmarried adolescents in Tanzania. BMC Public Health. 2009;9:373. doi: 10.1186/1471-2458-9-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Birungi H, Mugisha JF, Obare F, Nyombi JK. Sexual behavior and desires among adolescents perinatally infected with human immunodeficiency virus in Uganda: implications for programming. J Adolesc Health. 2009;44:184–87. doi: 10.1016/j.jadohealth.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 134.Siu GE, Bakeera-Kitaka S, Kennedy CE, Dhabangi A, Kambugu A. HIV serostatus disclosure and lived experiences of adolescents at the Transition Clinic of the Infectious Diseases Clinic in Kampala, Uganda: a qualitative study. AIDS Care. 2012;24:606–11. doi: 10.1080/09540121.2011.630346. [DOI] [PubMed] [Google Scholar]
- 135.Obare F, van der Kwaak A, Birungi H. Factors associated with unintended pregnancy, poor birth outcomes and post-partum contraceptive use among HIV-positive female adolescents in Kenya. BMC Womens Health. 2012;12:34. doi: 10.1186/1472-6874-12-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Birungi H, Obare F, Mugisha JF, Evelia H, Nyombi J. Preventive service needs of young people perinatally infected with HIV in Uganda. AIDS Care. 2009;21:725–31. doi: 10.1080/09540120802511901. [DOI] [PubMed] [Google Scholar]
- 137.Phillips SJ, Curtis KM, Polis CB. Effect of hormonal contraceptive methods on HIV disease progression: a systematic review. AIDS. 2013;27:787–94. doi: 10.1097/QAD.0b013e32835bb672. [DOI] [PubMed] [Google Scholar]
- 138.Belzer M, Rogers AS, Camarca M, et al. the Adolescent Medicine HIV/AIDS Research Network Contraceptive choices in HIV infected and HIV at-risk adolescent females. J Adolesc Health. 2001;29(suppl):93–100. doi: 10.1016/s1054-139x(01)00282-8. [DOI] [PubMed] [Google Scholar]
- 139.Biadgilign S, Deribew A, Amberbir A, Escudero HR, Deribe K. Factors associated with HIV/AIDS diagnostic disclosure to HIV infected children receiving HAART: a multi-center study in Addis Ababa, Ethiopia. PLoS One. 2011;6:e17572. doi: 10.1371/journal.pone.0017572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kallem S, Renner L, Ghebremichael M, Paintsil E. Prevalence and pattern of disclosure of HIV status in HIV-infected children in Ghana. AIDS Behav. 2011;15:1121–27. doi: 10.1007/s10461-010-9741-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Domek GJ. Social consequences of antiretroviral therapy: preparing for the unexpected futures of HIV-positive children. Lancet. 2006;367:1367–69. doi: 10.1016/S0140-6736(06)68584-X. [DOI] [PubMed] [Google Scholar]
- 142.Ferris M, Burau K, Schweitzer AM, et al. The influence of disclosure of HIV diagnosis on time to disease progression in a cohort of Romanian children and teens. AIDS Care. 2007;19:1088–94. doi: 10.1080/09540120701367124. [DOI] [PubMed] [Google Scholar]
- 143.Lee MB, Rotheram-Borus MJ. Parents’ disclosure of HIV to their children. AIDS. 2002;16:2201–07. doi: 10.1097/00002030-200211080-00013. [DOI] [PubMed] [Google Scholar]
- 144.Williams PL, Storm D, Montepiedra G, et al. Predictors of adherence to antiretroviral medications in children and adolescents with HIV infection. Pediatrics. 2006;118:e1745–57. doi: 10.1542/peds.2006-0493. [DOI] [PubMed] [Google Scholar]
- 145.Menon A, Glazebrook C, Campain N, Ngoma M. Mental health and disclosure of HIV status in Zambian adolescents with HIV infection: implications for peer-support programs. J Acquir Immune Defic Syndr. 2007;46:349–54. doi: 10.1097/QAI.0b013e3181565df0. [DOI] [PubMed] [Google Scholar]
- 146.Vaz L, Corneli A, Dulyx J, et al. The process of HIV status disclosure to HIV-positive youth in Kinshasa, Democratic Republic of the Congo. AIDS Care. 2008;20:842–52. doi: 10.1080/09540120701742276. [DOI] [PubMed] [Google Scholar]
- 147.Wood K, Chase E, Aggleton P. ‘Telling the truth is the best thing’: teenage orphans’ experiences of parental AIDS-related illness and bereavement in Zimbabwe. Soc Sci Med. 2006;63:1923–33. doi: 10.1016/j.socscimed.2006.04.027. [DOI] [PubMed] [Google Scholar]
- 148.Kouyoumdjian FG, Meyers T, Mtshizana S. Barriers to disclosure to children with HIV. J Trop Pediatr. 2005;51:285–87. doi: 10.1093/tropej/fmi014. [DOI] [PubMed] [Google Scholar]
- 149.Moodley K, Myer L, Michaels D, Cotton M. Paediatric HIV disclosure in South Africa: caregivers’ perspectives on discussing HIV with infected children. S Afr Med J. 2006;96:201–04. [PubMed] [Google Scholar]
- 150.Vreeman RC, Nyandiko WM, Ayaya SO, Walumbe EG, Marrero DG, Inui TS. The perceived impact of disclosure of pediatric HIV status on pediatric antiretroviral therapy adherence, child well-being, and social relationships in a resource-limited setting. AIDS Patient Care STDS. 2010;24:639–49. doi: 10.1089/apc.2010.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Brown BJ, Oladokun RE, Osinusi K, Ochigbo S, Adewole IF, Kanki P. Disclosure of HIV status to infected children in a Nigerian HIV Care Programme. AIDS Care. 2011;23:1053–58. doi: 10.1080/09540121.2011.554523. [DOI] [PubMed] [Google Scholar]
- 152.Myer L, Moodley K, Hendricks F, Cotton M. Healthcare providers’ perspectives on discussing HIV status with infected children. J Trop Pediatr. 2006;52:293–95. doi: 10.1093/tropej/fml004. [DOI] [PubMed] [Google Scholar]
- 153.WHO [accessed Nov 28, 2013];Guideline on HIV disclosure counselling for children up to 12 years of age. 2011 Dec; http://whqlibdoc.who.int/publications/2011/9789241502863_eng.pdf. [PubMed]
- 154.Vaz LM, Eng E, Maman S, Tshikandu T, Behets F. Telling children they have HIV: lessons learned from findings of a qualitative study in sub-Saharan Africa. AIDS Patient Care STDS. 2010;24:247–56. doi: 10.1089/apc.2009.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ferguson J, Baggaley R, Pazvakavambwa B, Ncube B, Desta Woldehanna T, Hirnschall G, the WHO Adolescent HIV Guidelines Development Group WHO guidelines on HIV testing and counselling for adolescents and care for adolescents living with HIV. Presented at the 7th International AIDS Society Conference; Kuala Lumpur, Malaysia. June 30–July 3, 2013; [accessed Nov 28, 2013]. http://www.who.int/hiv/events/2013/IAS_poster_01_htc.pdf.pdf. [Google Scholar]
- 156.WHO . HIV and adolescents: guidance for HIV testing and counselling and care for adolescents living with HIV—recommendations for a public health approach and considerations for policy-makers and managers. World Health Organization; Geneva: 2013. Annex 14: strengthening health services and outcomes for adolescents living with HIV. [PubMed] [Google Scholar]
- 157.Ferrand RA, Weiss HA, Nathoo K, et al. A primary care level algorithm for identifying HIV-infected adolescents in populations at high risk through mother-to-child transmission. Trop Med Int Health. 2011;16:349–55. doi: 10.1111/j.1365-3156.2010.02708.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Patten GE, Wilkinson L, Conradie K, et al. Impact on ART initiation of point-of-care CD4 testing at HIV diagnosis among HIV-positive youth in Khayelitsha, South Africa. J Int AIDS Soc. 2013;16:18518. doi: 10.7448/IAS.16.1.18518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Dowshen N, Kuhns LM, Johnson A, Holoyda BJ, Garofalo R. Improving adherence to antiretroviral therapy for youth living with HIV/AIDS: a pilot study using personalized, interactive, daily text message reminders. J Med Internet Res. 2012;14:e51. doi: 10.2196/jmir.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Gross R, Bellamy SL, Chapman J, et al. Managed problem solving for antiretroviral therapy adherence: a randomized trial. JAMA Intern Med. 2013;173:300–06. doi: 10.1001/jamainternmed.2013.2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Boon-Yasidhi V, Chokephaibulkit K, McConnell MS, et al. Development of a diagnosis disclosure model for perinatally HIV-infected children in Thailand. AIDS Care. 2013;25:756–62. doi: 10.1080/09540121.2012.749331. [DOI] [PubMed] [Google Scholar]



