Abstract
Background
Septic arthritis of the temporomandibular (TM) joint is rare, but it is associated with high risk for significant morbidity.
Objective
We reviewed the available literature regarding the presentation, evaluation, treatment, and clinical course of TM joint septic arthritis, focusing on elements relevant to emergency medicine physicians.
Case Reports
In the first case, a healthy 6-year-old boy presented with fever and trismus; computed tomography with contrast revealed a TM joint effusion. After empiric intravenous antibiotics, intraoperative arthrocentesis of the TM joint returned one milliliter of flocculent fluid, which was cultured and grew pan-sensitive Streptococcus pyogenes. He was discharge home with amoxicillin/clavulanate and experienced complete resolution of his symptoms. In the second case, more than three weeks after extraction of her third molars, an 18-year-old woman presented with facial pain, swelling, and trismus and was found to have a loculated abscess involving the left masseteric and pterygomandibular spaces with extension to the left deep temporal region and the skull base. She experienced a complicated postoperative course and required multiple procedures and intravenous antibiotics for growth of multiple bacteria. More than a month later underwent TM joint arthrotomy for TM joint septic arthritis, and she was found to have acute osteomyelitis. She continued to require multiple treatment modalities; twenty months after her initial presentation, she underwent left total TM joint arthroplasty for fibrous ankylosis of the TM joint.
Conclusion
Septic arthritis of the TM joint may be caused by hematogenous spread of distant infection or local spread of deep masticator space infections. Patients may present with TM joint septic arthritis acutely or sub-acutely. Septic arthritis of the TM joint should be considered in the differential diagnosis of patients who present with trismus and pain or fever.
Keywords: septic arthritis, temporomandibular joint, emergency department (ED), pediatric, adult, trismus
Introduction
Septic arthritis of the temporomandibular (TM) joint is known to result in significant morbidity if diagnosis is delayed.1,2 It is most often caused by hematogenous spread of distant infection, including sexually transmitted infections and reactive arthritis3-6; it can occur in the setting of trauma, burn, or spread of local infection.7,8 While septic arthritis of the TM joint has been described in the oral maxillofacial surgery (OMFS) literature, we are not aware of prior case reports in the emergency medicine literature.
Case Reports
Case 1
A healthy 6-year-old boy presented to the emergency department (ED) with a seven-day history of fever and left ear pain associated with rhinorrhea and vomiting. The patient was seen in an urgent care clinic and diagnosed with acute otitis media. Because the child was unable to open his mouth and had significant pain when rotating his neck, he was referred to the ED for evaluation.
On evaluation, the child was alert and in moderate distress. The vital signs were as follows: temperature 39.1°C, heart rate 124 beats per minute, blood pressure 121/66 mmHg, and SaO2 97% on room air. On physical examination, the child was unable to open his mouth more than 15mm, and he refused to flex his neck due to pain. Examination of the left ear revealed mild erythema with a decreased light reflex and obscured anatomic landmarks, as well as pre-auricular swelling tenderness. The remainder of the examination was reassuring.
Laboratory findings included a white blood cell count of 19,000/uL, hemoglobin of 12.3 g/dL, and platelet count of 497,000/uL; erythrocyte sedimentation rate was 50 mm/hr, and C-reactive protein was 69.2 mg/dL. A blood culture was also obtained.
Given the patient's trismus, pain, and refusal to flex his neck, the child underwent contrasted computed tomography (CT) of the face and neck; this revealed a large effusion in the left TM joint and mildly prominent surrounding lymphadenopathy (Image 1). After evaluation by the oral maxillofacial team, the child was taken to the operating room where he underwent arthrocentesis of the left TM joint. One milliliter of flocculent fluid was successfully aspirated and sent for Gram stain and culture. Ampicillin/sulbactam was given prior to surgery, and clindamycin was administered in the operating room; ampicillin/sulbactam was continued during the hospitalization. Blood culture and culture of the joint aspirate grew pan-sensitive Streptococcus pyogenes. The patient was discharged on post-operative day two with a one-week course of amoxicillin/clavulanate and a soft mechanical diet. At the follow up clinic visit one month later his symptoms had completely resolved, he had a normal range of mandibular motion, and panoramic imaging revealed no disruption of condylar cortex.
Case 2
An 18-year-old female presented to our ED with two days of left-sided facial swelling and several weeks of pain and trismus. She smoked but was otherwise generally healthy. Three weeks prior an oral surgeon had extracted her third molars, and her postoperative course was complicated by persistent left-sided facial pain and limited oral opening. Given concern that the third molar surgery had precipitated TM joint symptoms and limited oral opening, she had been referred to a dentist for management of the suspected TM joint problems. The dentist administered several local anesthetic injections to the left face and neck, with temporary pain relief. Two days later she was seen in her community ED, where she was given IV fluid for dehydration. When the facial pain, swelling, and trismus increased, she sought medical attention in our ED.
Evaluation in our ED revealed an uncomfortable woman without dyspnea, dysphagia or odynophagia. Vitals were as follows: temperature of 36.8°C, heart rate 89 beats per minute, blood pressure 119/67 mmHg, and SaO2 99% on room air. There was significant left facial swelling extending from the temple to the neck, with mild periorbital swelling and fullness in the left posterior maxillary buccal vestibule. The patient was unable to open her mouth more than 15mm, and movement of the jaw elicited significant pain. The posterior pharynx was easily visualized, and the tonsillar pillars were symmetric. Laboratory findings included a white blood cell count of 12,500/uL, hemoglobin of 12.4 g/dL, and platelet count of 236,000/uL.
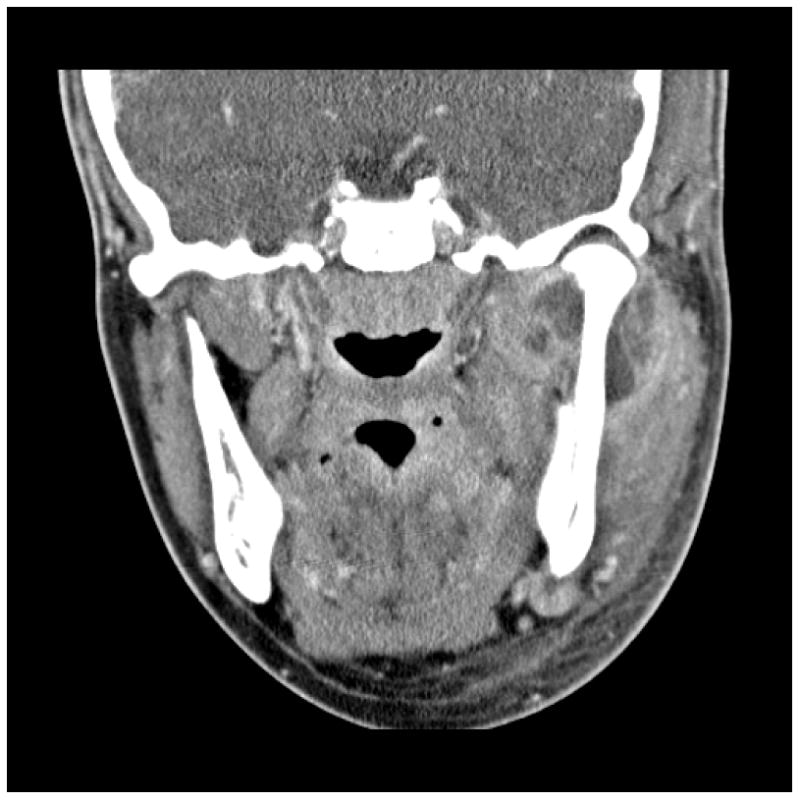
Contrasted CT revealed a loculated abscess involving the left masseteric and pterygomandibular spaces, with extension to the left deep temporal region and the skull base. The patient was evaluated by the oralmaxillofacial team and the otolaryngology team was consulted due to extension of the abscess to the skull base.
She was taken to the operating room where she underwent incision and drainage of the left deep temporal, pterygomandibular, and masseteric spaces. Purulent fluid was submitted for Gram stain and culture, and intravenous clindamycin and cefuroxime were given. Persistent pain and leukocytosis on the fourth post-operative day prompted repeat contrasted CT imaging, which demonstrated residual fluid collections involving the masticator spaces and new phlegmon formation in the left lateral pharyngeal space. On the fifth hospital day, the patient again underwent incision and drainage of the masticators space abscess, as well as incision and drainage of the lateral pharyngeal space through a submandibular approach. Because Gram stain revealed gram positive cocci and gram negative rods, antibiotic coverage was changed to vancomycin and ertapenem. Final cultures grew coagulase-negative Staphylococcus, Group C Streptococcus, and Acinetobacter baumanii. Based on susceptibility testing, the antibiotic regimen was changed to piperacillin-tazobactam monotherapy. On the ninth hospital day she was returned to the operating room for wound irrigation. She was discharged to home on hospital day 10 to complete a three-week course of piperacillin-tazobactam.
Twenty days following the first incision and drainage procedure, she returned to our ED with neck pain. Laboratory evaluation at that time revealed a white blood cell count of 7,600/uL. Contrast enhanced CT imaging of her neck showed only persistent inflammatory changes involving the masticator spaces without new or residual fluid collections. The patient underwent close follow-up, which included range of motion exercises and pain management. She continued to have intermittent non-purulent drainage from the submandibular incision and drainage site that was managed with irrigation with Dakin's solution. Two and a half months following her initial presentation, the submandibular wound had closed. However, she continued to report left masseter region pain that was believed to be due to residual inflammation, fibrosis, and range of motion exercises. Approximately three months following the initial ED presentation, she returned to clinic with new submandibular swelling; contrasted maxillofacial CT revealed a small left submandibular fluid collection, periosteal new bone formation along the medial and lateral cortices of the left mandibular ramus and condylar head, and erosion of the condylar head, consistent with osteomyelitis and a history of septic arthritis of the TM joint. The patient underwent drainage of the new submandibular abscess and left TM joint arthrotomy for debridement of a condylar sequestrum, with washout of the joint space. Surgical pathology confirmed the clinical diagnosis of acute osteomyelitis. Wound cultures grew group C Streptococcus. A 6-week course of piperacillin-tazobactam was initiated, and after one week of intermittent irrigation the pre-auricular wound healed uneventfully. However, due to continued pain and drainage from the left ramus, hyperbaric oxygen treatment was initiated; despite this, she continued to have tenderness to the left mandibular angle, so five months after her initial presentation she underwent debridement of the mandibular angle region. Pathology findings were consistent with chronic osteomyelitis. Following this final debridement the osteomyelitis resolved.
Nine months following the initial presentation infection had resolved, but the patient reported symptoms consistent with fibrous ankylosis of the TM joint, including persistent, low-grade left facial pain, an oral opening of 21mm, and no translation of the left mandibular condyle. CT imaging demonstrated progressive arthrosis of the left mandibular condyle. Twenty months after the initial presentation, she underwent left total TM joint arthroplasty. Seven months following total joint arthroplasty her interincisal opening had increased to 31 mm.
Discussion
Septic arthritis most often occurs in the hips and knees, while smaller joints are affected much less frequently.4 Septic arthritis of the TM joint most often occurs in male adults, with an average age at the time of presentation if 36 years, but it has been reported in infants and children.8-11 The most common presenting complaints are trismus and pain, although swelling, tenderness, and erythema have also been described.2,7,8
Treating clinicians evaluating patients with swelling, tenderness, or erythema to the TM joint or unilateral facial pain should include in the differential diagnosis: dental abscess or periapical dental abscess, bacterial or viral pharyngitis, retropharyngeal abscess, peritonsillar abscess, acute otitis media, mastoiditis, parotitis, submandibular sialadenitis, and lymphadenopathy. In every case, priorities include evaluation of and maintenance of the airway and close attention to any patient with a threatened airway. Signs of impending airway compromise include a hoarse voice, difficulty handling oral secretions, a sensation of dyspnea, and the patient positioning himself in the “sniffing position”; development of any of these signs or symptoms should prompt aggressive management. Patients with impending airway compromise should generally not undergo computed tomography as lying flat may precipitate airway compromise, and these patients warrant emergent consultation with oral surgery, otolaryngology, and anesthesiology, as appropriate. Pain control, hydration, initiation of antibiotics, and consideration of steroids to reduce swelling should be initiated in a timely fashion.
Staphylococcus aureus and S. saprophyticus are the most commonly cultured bacteria, although Streptococcus species, Neisseria, and Haemophilus influenza have also been reported in the literature.4,8 Infection of the TM joint is thought to occur most often due to hematogenous spread from a distant primary infection1,3; blunt trauma with resulting capsular injury may facilitate the hematogenous spread of infection into the joint space.2 While primary infections such as upper respiratory infections, acute pyelonephritis, and tonsillitis4 have been identified in the setting of septic arthritis of the TM joint, the primary source of infection often remains undetermined.1 Infection can also spread contiguously from a nearby source in the head and neck.17 In adults, spread of local infection to the TM joint has occurred in the setting of otits externa, infection of maxillary molars and sites of molar extraction, intra-articular injection, and facial burns.2 Septic arthritis of the TM joint has also been described in association with sexually transmitted infections and as part of Reiter's syndrome.5,6,12-14
Given the high risk of complications, septic arthritis of the TM joint is a medical emergency; earlier diagnosis and treatment is thought to improve clinical outcomes.4 Unfortunately, the initial symptoms of septic TM joint arthritis may be mistaken for other TM joint disorders including internal derangement, synovial chondromatosis, or rheumatoid arthritis.4 Thus, even though bony changes are often not seen during the acute phase of illness, imaging studies are indicated as part of the evaluation of TM joint disease.4 Magnetic resonance imaging is highly recommended because its sensitivity permits earlier detection of joint effusion and allows evaluation of the joint surfaces and periarticular soft tissue.4 Contrast-enhanced CT is useful in demonstrating larger joint effusions, cortical breakdown, osteomyelitis, and ankylosis of the TM joint.4 At this time, we are not aware of experience describing the use of ultrasonography for the diagnosis of TM joint effusion or for TM joint aspiration. At this time, clinical suspicion of septic arthritis of the TM join should prompt a contrasted CT scan prior to a joint aspiration. If radiographic evidence reveals bony changes, a specialist should be consulted regarding management and to perform either arthrocentesis with irrigation and lavage or an open joint procedure for more thorough debridement. Fluid for culture would be obtained at that time in conjunction with either operative procedure.
Once the diagnosis of TM joint septic arthritis has been made, joint aspiration is recommended.4 Joint aspirate should be examined grossly for color and turbidity as indicators of infection, microscopically for joint fluid analysis, and fluid should be submitted for Gram stain, culture, and sensitivity analysis.4 Labs such as white blood cell count with differential may reveal leukocytosis or neutrophilia. C-reactive protein levels may be elevated during the acute stage of illness.4 When fever is present, blood cultures may also be a useful diagnostic test.4
Complications of septic arthritis of the TM joint include a high incidence of local spread of infection, recurrence of infection, destruction of joint articular surfaces, and fibrous or bony ankylosis of the temporomandibular joint.1,8 Thus, therapy should include early use of broad spectrum antibiotics, joint arthrotomy or aspiration with lavage, and reduction in joint loading.2,4,7,15 In the acute setting, septic arthritis may be treated by aspiration alone and may be as effective as arthrotomy and washout for pediatric patients.2 Arthroscopic lysis of adhesions and capsular stretch early in the course of disease may also be helpful.15 Aggressive range of motion exercises should be initiated following improvement of the acute infectious process to minimize the risk of long-term restricted oral opening. Because ankylosis is thought to impair mandibular growth, children with septic arthritis of the TM joint should undergo early and aggressive range of motion exercises to restore full mobility.
Our cases illustrate two contrasting presentations of septic arthritis of the TM joint. The first case is noteworthy for the complete response early diagnosis, surgical drainage, and antibiotics. The second case underscores the potential complications of TM joint septic arthritis, with a prolonged clinical, with multiple operative interventions, and development of ankylosis that was treated by total joint arthroplasty.
Conclusion
Septic arthritis of the TM joint may be caused by hematogenous spread of distant infection or local spread of deep masticator space infections. Patients may present with TM joint septic arthritis acutely or sub-acutely. Septic arthritis of the TM joint should be considered in the differential diagnosis of patients who present with trismus and pain or fever.
Figure 1.
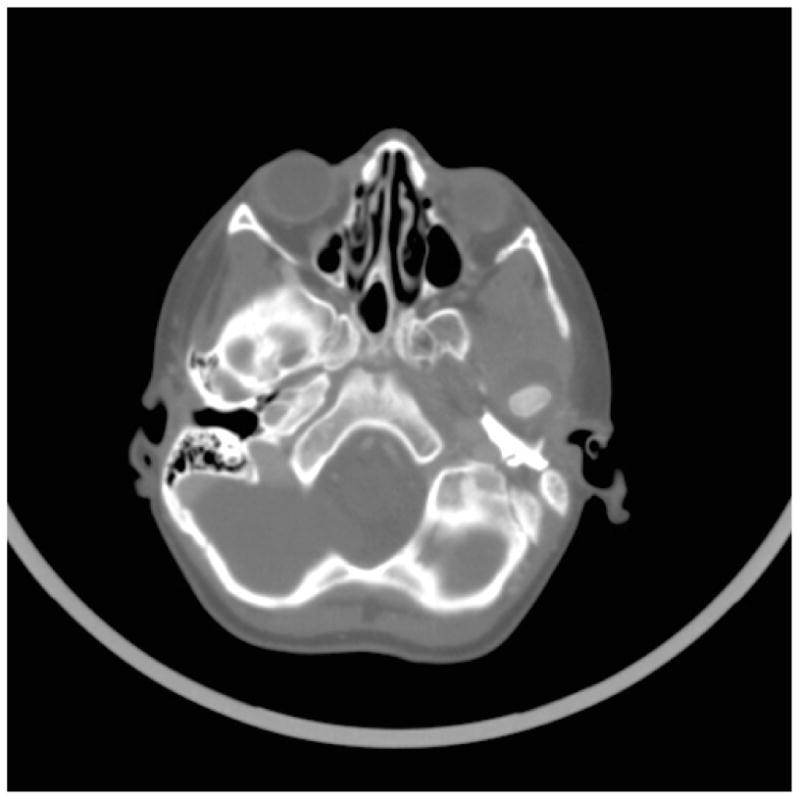
Large effusion in the left temporomandibular joint in a 6-year-old boy with trismus and fever.
Figure 2. 18-year-old female with loculated abscess of the left masseteric and pterygomandibular spaces, with extension to the left deep temporal region and skull base.
Acknowledgments
This work was supported by the Office of Academic Affiliations, Department of Veterans Affairs, VA National Quality Scholars Program with resources and the use of facilities at VA Tennessee Valley Healthcare System, Nashville, TN (CDM) and by the Vanderbilt CTSA grant UL1 RR024975-01 from NCRR/NIH (CDM).
Footnotes
Reprints: Reprints are not available from the authors
References
- 1.Leighty SM, Spach DH, Myall RW, Burns JL. Septic arthritis of the temporomandibular joint: review of the literature and report of two cases in children. Int J Oral Maxillofac Surg. 1993;22:292–7. doi: 10.1016/s0901-5027(05)80519-3. [DOI] [PubMed] [Google Scholar]
- 2.Bounds GA, Hopkins R, Sugar A. Septic arthritis of the temporo-mandibular joint--a problematic diagnosis. Br J Oral Maxillofac Surg. 1987;25:61–7. doi: 10.1016/0266-4356(87)90158-6. [DOI] [PubMed] [Google Scholar]
- 3.Goldschmidt MJ, Butterfield KJ, Goracy ES, Goldberg MH. Streptococcal infection of the temporomandibular joint of hematogenous origin: a case report and contemporary therapy. J Oral Maxillofac Surg. 2002;60:1347–53. doi: 10.1053/joms.2002.35736. [DOI] [PubMed] [Google Scholar]
- 4.Trimble LD, Schoenaers JA, Stoelinga PJ. Acute suppurative arthritis of the temporomandibular joint in a patient with rheumatoid arthritis. J Maxillofac Surg. 1983;11:92–5. doi: 10.1016/s0301-0503(83)80022-8. [DOI] [PubMed] [Google Scholar]
- 5.Bomalaski JS, Jimenez SA. Erosive arthritis of the temporomandibular joint in Reiter's syndrome. J Rheumatol. 1984;11:400–2. [PubMed] [Google Scholar]
- 6.Alexander WN, Nagy WW. Gonococcal arthritis of the temporomandibular joint. Report of a case. Oral Surg Oral Med Oral Pathol. 1973;36:809–13. doi: 10.1016/0030-4220(73)90331-9. [DOI] [PubMed] [Google Scholar]
- 7.Cai XY, Yang C, Chen MJ, Zhang SY, Yun B. Arthroscopic management of septic arthritis of temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:24–30. doi: 10.1016/j.tripleo.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 8.Cai XY, Yang C, Zhang ZY, Qiu WL, Chen MJ, Zhang SY. Septic arthritis of the temporomandibular joint: a retrospective review of 40 cases. J Oral Maxillofac Surg. 2010;68:731–8. doi: 10.1016/j.joms.2009.07.060. [DOI] [PubMed] [Google Scholar]
- 9.Parmar J. Case Report: septic arthritis of the temporomandibular joint in a neonate. Br J Oral Maxillofac Surg. 2008;46:505–6. doi: 10.1016/j.bjoms.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 10.Amos MJ, Patterson AR, Worrall SF. Septic arthritis of the temporomandibular joint in a 6-year-old child. Br J Oral Maxillofac Surg. 2008;46:242–3. doi: 10.1016/j.bjoms.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 11.Viraraghavan R, Kelly L, Podstreleny S, Obeid G. Fever and jaw pain in a five-year-old. TMJ septic arthritis. Pediatr Infect Dis J. 2000;19:1113, 5–6. [PubMed] [Google Scholar]
- 12.Henry CH, Hudson AP, Gerard HC, Franco PF, Wolford LM. Identification of Chlamydia trachomatis in the human temporomandibular joint. J Oral Maxillofac Surg. 1999;57:683–8. doi: 10.1016/s0278-2391(99)90432-9. discussion 9. [DOI] [PubMed] [Google Scholar]
- 13.Henry CH, Hughes CV, Gerard HC, Hudson AP, Wolford LM. Reactive arthritis: preliminary microbiologic analysis of the human temporomandibular joint. J Oral Maxillofac Surg. 2000;58:1137–42. doi: 10.1053/joms.2000.9575. discussion 43-4. [DOI] [PubMed] [Google Scholar]
- 14.Henry CH, Whittum-Hudson JA, Tull GT, Wolford LM. Reactive arthritis and internal derangement of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e22–6. doi: 10.1016/j.tripleo.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Sembronio S, Albiero AM, Robiony M, Costa F, Toro C, Politi M. Septic arthritis of the temporomandibular joint successfully treated with arthroscopic lysis and lavage: case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e1–6. doi: 10.1016/j.tripleo.2006.08.028. [DOI] [PubMed] [Google Scholar]


