Abstract
This mixed methods study examined perceived facilitators and obstacles to adopting evidence-based pain management protocols vis-a-vis documented practice changes that were measured using a chart audit tool. This analysis used data from a subgroup of four nursing homes that participated in a clinical trial. Focus group interviews with staff yielded qualitative data about perceived factors that affected their willingness and ability to use the protocols. Chart audits determined whether pain assessment and management practices changed over time in light of these reported facilitators and barriers. Reported facilitators included administrative support, staff consistency, and policy and procedure changes. Barriers were staff attitudes, regulatory issues, and provider mistrust of nurses’ judgment. Overall, staff reported improvements in pain practices. These reports were corroborated by modest but significant increases in adherence to recommended practices. Change in clinical practice is complex and requires attention to both structural and process aspects of care.
Management of persistent pain poses a challenge to health care providers, especially those who care for older adults living in nursing homes (NHs). Research indicates that as high as 80% of NH residents experience persistent pain (Gibson, 2007; Gibson & Lussier, 2012; Helme & Gibson, 2001). This finding is significant in that persistent pain negatively impacts life satisfaction and quality of life (Lapane, Quilliam, Chow, & Kim, 2012; Takai, Yamamoto-Mitani, Okamoto, Koyama, & Honda, 2010). Pain is also a risk factor for anxiety, depression, suicidal thoughts, functional disability, sleep disorders, decreased socialization and loneliness, and falls (Gibson & Lussier, 2012; Lapane et al., 2012).
Although debilitating pain is common among NH residents, it is often inadequately assessed and managed (Decker, Culp, & Cacchione, 2009; Takai et al., 2010), despite the availability of evidence-based clinical practice guidelines and resources (American Geriatrics Society Panel on Pharmacological Management of Persistent Pain in Older Persons, 2009; American Medical Directors Association, 2009; Hadjistavropoulos et al., 2007). It has been suggested that a systematic implementation of evidence-based guidelines is necessary to achieve pain relief in older adults residing in NHs (Gibson, 2007).
Successful integration of clinical guidelines into practice relies on identifying and addressing barriers to implementation, as well as using strategies and factors that are known to facilitate adoption. Rich empirical literature describing these barriers and facilitators exists. Often, barriers and facilitators are found at opposite ends of the same factor. For example, low staff turnover is a facilitator to adopting best practices, whereas high staff turnover is a barrier.
Barriers to changing clinical practice in NHs can occur at the clinician or organizational levels. Clinician-level barriers include lack of knowledge and expertise, attitudes and misconceptions, and poor communication among health care team members. (Colón-Emeric et al., 2007; Grol & Grimshaw, 2003; Jones et al., 2004; Koh, Manias, Hutchinson, Donath, & Johnston, 2008; Ploeg, Davies, Edwards, Gifford, & Miller, 2007). Efforts to change practice depend on whether staff accept or resist the trade of long-standing ways of providing care for those based on evidence. Nurses may also consider practice guidelines too prescriptive for providing individualized care, or they may disagree with guideline content. Knowledge of and experience with research and guideline development processes have also been reported to contribute positively to the extent to which practice guidelines are accepted by nurses. Changes in practice also require the collaboration of all staff involved in clinical care. Communication among members of the interdisciplinary team, who share a common goal, is seen as vital to the successful implementation and maintenance of evidence-based care (Clarke et al., 2005; Jones et al., 2004; Ploeg et al., 2007).
Organizational barriers include (a) an absence of policies and clinical procedures to ensure regular adherence to best practices; (b) minimal physician involvement in planning resident care; and (c) a lack of clinical champions to support change. Adoption of clinical guidelines is also hindered when conflicts between organizational goals and the recommended practices exist, or when administrators fail to both explicitly voice support for the changes and provide the necessary resources to effect needed practice changes (Colón-Emeric et al., 2007; Grol & Grimshaw, 2003; Tarzian & Hoffmann, 2005).
Facilitators that foster the successful implementation of evidence-based pain management guidelines include the availability of education and training, as well performance appraisals that hold staff accountable for adhering to guidelines (Koh et al., 2008; Ploeg et al., 2007). Administrative support at all levels, from directors of nursing to unit level managers, also promotes the implementation of clinical guidelines (Ploeg et al., 2007). Guidelines are more likely to be implemented in practice if they align with organizational policies and procedures and if they are accompanied by resources, such as additional staffing, necessary equipment, and release time to attend training (Ploeg et al., 2007). Access to technology, computerized forms, and automated reminders can facilitate information gathering and documentation, thereby allowing more time to learn and adopt new practices.
Investigators who test interventions to implement practice changes should consider barriers and facilitators in their design. Although it is rarely done, researchers should also monitor these factors throughout the trial (Lewin, Glenton, & Oxman, 2009). Lewin et al. (2009) urged the integration of qualitative methods into randomized controlled trials of complex interventions and asserted that qualitative approaches can be used for several purposes before, during, and after a trial. Following the trial, collection and analysis of qualitative data can (a) assist investigators in exploring reasons why an intervention succeeded or failed; (b) explain variations in the effectiveness of the intervention; (c) examine the suitability of the theory used to guide the trial; and (d) generate additional questions and hypotheses. These strategies can be used to explore specific barriers and facilitators associated with the outcomes of the intervention.
PURPOSE
The purpose of this study was to identify facilitators and barriers that affected the success of an intervention aimed at promoting the adoption of evidence-based pain management protocols into NHs. Focus group interviews were conducted with staff to determine their perceptions about factors that affected their willingness and ability to use the evidence-based protocols. Quantitative methods (e.g., a chart audit tool) were used to determine whether pain assessment and management practices changed over time in light of these facilitators and barriers.
METHODS
Data for the current investigation were collected from NH staff who previously participated in a randomized controlled study that evaluated the efficacy of evidence-based pain algorithms coupled with intense dissemination strategies (ALG) and that aimed to improve clinical pain practices and residents’ pain, depression, and mobility (Ersek et al., 2012). Only NHs randomized to the intervention arm participated in the current study because the current study’s focus was on exploring factors affecting the adoption of the best practices that were embedded in the intervention.
The intervention consisted of a program of staff education and diffusion strategies to encourage adoption of evidence-based pain management practices (Rogers, 2003). A centerpiece of the intervention was a set of algorithms that guided pain assessment and management. Algorithms present a step-by-step approach to decision making that enhance the care provider’s ability to make sound clinical decisions based on best evidence (Jablonski, Du Pen, & Ersek, 2011). The use of algorithms, as well as a multicomponent approach to change, has been shown in previous research to be successful in transforming care practices (Adli, Bauer, & Rush, 2006; Du Pen et al., 2000; Gilbody, Whitty, Grimshaw, & Thomas, 2003). Table 1 summarizes the intervention components. Additional details about the strategies appear in an earlier publication (Ersek et al., 2012).
TABLE 1.
COMPONENTS OF THE PARENT STUDYa
| Group | Intervention |
|---|---|
| Intervention (ALG) | Pain assessment and management algorithms including:
|
| Control (EDU only) | Four 1-hour classes educating staff on assessment and management of pain not using algorithms |
Note. ALG = evidence-based pain algorithms coupled with intense dissemination strategies; EDU = education control condition.
Thirteen of the 28 NHs participating in the parent study (Ersek et al., 2012) were randomized to the intervention arm. Of these NHs, a convenience sample of four (31%) were chosen to participate in the current study. These facilities were selected because they varied in size and ownership, which were characteristics that the investigators thought might result in a broader range of facilitators and barriers being identified. Table 2 details the characteristics of these selected NHs.
TABLE 2.
CHARACTERISTICS OF NURSING HOMES (NHs) THAT PARTICIPATED IN FOCUS GROUPS
| Variable | NH A | NH B | NH C | NH D |
|---|---|---|---|---|
| Type of ownership | Nonprofit church-related | Nonprofit corporation | Nonprofit corporation | State government |
| Number of certified beds | 215 | 111 | 148 | 240 |
| Overall rating (stars)a | 4 | 4 | 3 | 4 |
| Residents with moderate to severe pain (%) | 6 | 5 | 1 | 6 |
NHs are rated overall and on health inspections, NH staffing, and quality measures. More stars are better (5 possible). The Quality Measure ratings are taken from data submitted to Medicare by nursing homes between January 1, 2010 and September 30, 2010 (Centers for Medicare and Medicaid Services, 2013).
Procedures and Measures
A focus group session lasting approximately 1 hour was conducted in each facility during the day shift by research assistants (RAs). The interview occurred approximately 6 months after all outcomes data were collected for the randomized trial. All levels of caregivers were invited to take part in the focus group discussions. A convenience sample of 24 staff members across the four facilities participated, including 17 RNs, three licensed practical nurses, one advanced practice RN, and two certified nursing assistants. Staff members were employed for an average of 10 years in their current facility and 16 years in long-term care.
The RAs began each session with an introduction to the study and the focus group process. The RAs used open-ended questions to elicit staff perspectives regarding changes in pain assessment and management practices that had occurred since their participation in the randomized controlled trial. Questions were also included to obtain information about the facilitators that supported change and the barriers that undermined change (Table 3).
TABLE 3.
FOCUS GROUP QUESTIONS TO ELICIT FACILITATORS AND BARRIERS TO CHANGES IN PAIN ASSESSMENT AND MANAGEMENT PRACTICES
| What is the biggest remaining challenge to effective pain management? |
| From your perspective, what things were most helpful in adopting the algorithms and other pain management practices? |
| How useful were the classes, videorecordings, algorithm handbook, resource manual, examples of documentation forms, follow-up consultation sessions, assistance forming a pain team, and booster items in facilitating changes in your facility? |
| What things were barriers to the adoption of new pain management practices? |
| What made it difficult for your facility to adopt new pain assessment and management practices? |
| What is needed to continue improvements made in pain assessment and management practices? |
Actual changes in pain assessment and management practices in the parent study were measured using the Pain Management Chart Audit Tool (PM-CAT). Charts were audited at baseline, 1 month following the completion of the intervention, and 6 months following the completion of the entire study in each facility. For the purposes of this study, data from the baseline and 6-month audits were examined. Data were collected from a total of 92 resident charts across the four facilities participating in the focus groups.
The PM-CAT was developed by the parent study’s investigators based on evidence-based pain management guidelines available in the literature (American Geriatrics Society, 2009; American Medical Directors Association, 2012). The tool consists of 17 items—nine quality indicators of a comprehensive, multidimensional pain assessment and eight indicators that reflect current best pain management practices (Jablonski & Ersek, 2009). Most indicators are scored on a scale of 0 to 2, with 1 indicating partial adherence to best practice and 2 indicating full adherence. For example, the indicator for the frequency of chronic pain assessment is coded 2 if assessment occurs at least once per week, 1 for one to three times per month, or 0 for no pain assessment documented. Some items are scored as N/A for not applicable. For example, the item related to assessment following the initiation of a new or increased dose of an analgesic is scored N/A if no changes had been made to the analgesic regimen during the review period.
Total scores for the PM-CAT were calculated by adding the score on each of the 17 items, dividing by the total possible points, and multiplying by 100 to yield scores between zero and 100; higher scores represented greater adherence to best practices. Using similar calculations, subscale scores were also calculated for the nine-item Pain Assessment Subscale and eight-item Pain Management Subscale. Two doctorally prepared nurse investigators and one nurse practitioner collected all PM-CAT data using a detailed protocol. All three coders trained each other during a pilot phase, during which they discussed their coding, reached consensus, and refined the protocol. Interrater reliability among the three trained nurse coders was 90%.
Confidentiality of all information was assured. All study procedures were approved by the Swedish Medical Center Institutional Review Board (IRB) in Seattle, Washington. All participating facilities obtained a Federalwide Assurance from the Office for Human Research Protections, and all formally established an agreement with the Swedish Medical Center IRB.
Data Analysis
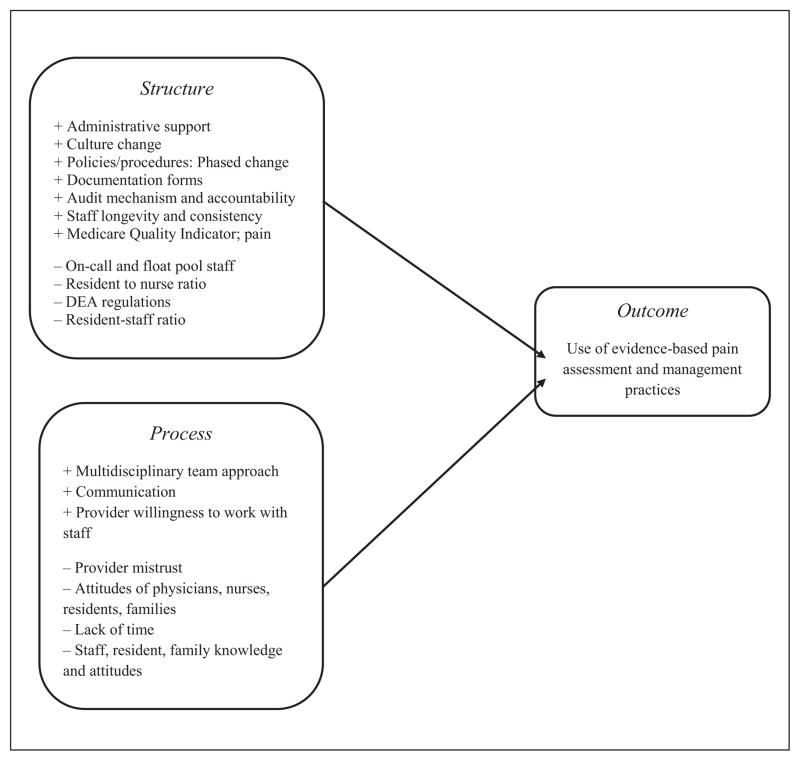
Audiorecordings of each focus group were transcribed verbatim by an RA. One of the authors (M.E.) listened to the audiorecorded interviews while reviewing the transcripts to ensure accuracy. Directed content analysis was used to identify facilitators and barriers to the adoption of evidence-based algorithms. The investigators chose this analytic approach because initial codes were derived from existing theory and research (Hsieh & Shannon, 2005). The data were coded into themes and were verified by the first author (M.E.). Themes were then organized into categories by the first author (M.E.) and validated by the second author (A.J.). Donabedian’s concepts of structure, process, and outcome were used to organize the categories (Donabedian, 1988). Structure refers to fixed characteristics of the facility (e.g., organizational structure and staffing); process denotes what is actually done by providers to deliver care (e.g., use of evidence-based algorithms to guide pain management); and outcome represents changes in practice as a result of the ALG intervention (e.g., pain assessment and management practices) (Figure). Outcomes were also evaluated using the PM-CAT.
Figure.
Facilitators (+) and barriers (−) to adoption of evidence-based pain assessment and management practices.
Note. DEA = Drug Enforcement Agency.
Quantitative data were analyzed using SPSS version 20. Means and standard deviations were calculated for the PM-CAT total scores, Pain Assessment Subscale scores, and Pain Management Subscale scores. To evaluate changes in pain practices, paired t tests were computed to compare baseline and 6-month PM-CAT total and subscale scores.
RESULTS
Qualitative Results
Structure
Focus group participants identified several structural elements that facilitated algorithm use. Active involvement by and support from administration, particularly directors of nursing, were seen as key elements in bringing about a shift in culture related to pain assessment and management. Development and implementation of new policies and procedures for ongoing pain assessment also contributed to practice improvement, especially when these new processes were accompanied by an audit mechanism and individual accountability for adherence to them. Several focus group members stated that the paced phasing in of new policies and procedures facilitated change because it was less overwhelming to staff.
Participants also indicated that the availability of needed resources supported use of the algorithms. For example, participating facilities received chart forms that served as examples for staff to use in developing forms that met their own facility’s needs. New computerized forms for documenting pain assessment and analgesic administration reminded staff to assess pain regularly. They also reported that education was an important resource that had a significant positive impact on practice change. Participants asserted that the outside experts who provided the education and follow up increased awareness throughout the facility about the need to focus on residents’ pain.
A final structural factor that participants believed exerted a significant positive impact on the adoption of evidence-based practices was consistency of staff. Salary and benefits were noted as major factors in maintaining staff and decreasing turnover. Interestingly, the major barriers to changing practice were related to staffing as well. Participants perceived that on-call and float staff assessed and treated pain less consistently than regular staff. Staff turnover and high resident-to-staff ratios were also seen as barriers.
Government regulations were viewed as both facilitators and barriers to effective pain management. In 2002, the Centers for Medicare and Medicaid Services launched the Nursing Home Quality Initiative, which includes public reporting of several quality-of-care indicators (http://www.medicare.gov/nursing-homecompare). One of the quality indicators reported was the percentage of residents who had moderate to severe pain during a 7-day assessment period. Poor performance on this indicator provided an incentive for facilities to evaluate current practice and adopt changes recommended by the ALG intervention.
Conversely, regulations that limited access to controlled substances were viewed as barriers to effective pain management. At the time the focus groups were conducted, the Drug Enforcement Administration (DEA) did not consider NH licensed nurses as agents of the physician. The law did not allow NH nurses to take verbal orders for controlled substances, except in narrowly defined situations (Center for Medicare Advocacy, Inc., 2010). This regulation led to delays in getting some pain medications to residents.
Process
In addition to structural factors, other factors related to process were viewed as either facilitators for or barriers to effective pain management. One component of the ALG intervention was the formation of a multidisciplinary pain team. Although the pain team’s activities were not always maintained over time, there continued to be multidisciplinary input into pain assessment and management. For example, participants observed that dietary, activity, physical therapy, and social services staffs approached them more often when staff thought that a resident was experiencing pain. Nursing assistants reported pain more frequently as well. The nurses believed that all staff felt empowered to report residents’ pain.
On the other hand, some participants believed that physicians’ mistrust of nurses’ judgments undermined nurses’ recommendations for pain management, thereby hindering adoption of best practices. Some staff mentioned that attitudes such as fear of addiction and over-sedation hindered nurses’ willingness to treat pain aggressively. Several emphasized that residents and their families held similar beliefs that were difficult to overcome. A final factor that hindered effective pain assessment and management was lack of time. High resident-to-nurse ratios, as well as pressures to complete other required tasks, contributed to nurses’ perceptions that there was not enough time to thoroughly assess pain.
Outcome
Participants reported that the intervention resulted in several practice changes. Two facilities stated that transitioning to electronic charting assisted the facility in making these positive changes. Comments from participants provide examples of how practice had changed in their facilities:
Upon admission we do a three-day of assessment of pain [sic] in the computer and then weekly after that until we manage the pain.
We anticipate pain on admission now.
I think that the aides and the restorative staff and the people who were charting that they [the resident] didn’t want to do it because they were pain [sic], are now feeling empowered to come forward and not feel like they are speaking out of turn.
I learned a lot of things in class, but one thing was about Tylenol®…I can’t tell you how many times I’ve used that for somebody who’s having pain and starting out with that…. So I’ve been using it and it’s been successful.
Quantitative Results
Table 4 presents the findings for the quantitative analyses. The PM-CAT Management Subscale scores were higher than PM-CAT Assessment Subscale scores both at baseline (60.4 and 35.3, respectively) and at 6 months (61.1 and 42.2, respectively). However, the PM-CAT Management Subscale scores did not change significantly from baseline to 6 months. Mean scores on both the PM-CAT Assessment Subscale and the PM-CAT Total score increased at 6 months when compared to baseline. Paired t tests showed modest, yet statistically significant, differences for the PM-CAT Assessment Sub-scale and the PM-CAT Total score at 6 months.
TABLE 4.
COMPARISON OF PAIN MANAGEMENT CHART AUDIT TOOL (PM-CAT) MEAN SCORES AT BASELINE AND 6 MONTHS
| PM-CAT Score | Baseline Mean (SD) | 6 Months Mean (SD) | t Test (2 tailed) | p Value |
|---|---|---|---|---|
| Total | 46.5 (15.5) | 50.9 (17.3) | 2.0 | 0.05 |
| Assessment Subscale | 35.3 (22.5) | 42.2 (26.0) | 2.0 | 0.04 |
| Management Subscale | 60.4 (14.9) | 61.1 (17.3) | 0.54 | 0.59 |
Note. The possible range for the PM-CAT is 0 to 100; higher scores indicate greater adherence to best practices.
DISCUSSION
Findings from this study demonstrate that known barriers and facilitators to practice change influence the adoption of best practices during and following a randomized trial. Structural barriers, such as staff turnover, poor staffing, and process variables (i.e., physicians’ negative attitudes about nurses’ skills and fear of addiction), hindered adoption of practices. In contrast, factors that were perceived as facilitating change included structural features such as the institution of comprehensive pain management policies, as well as processes such as staff education. Many of these barriers and facilitators have been identified in earlier studies (Colón-Emeric et al., 2007; Ploeg et al., 2007; Tarzian & Hoffmann, 2005).
One barrier that has not been widely mentioned in the literature was the DEA prohibition that limited the ability of NH nurses to accept phone orders for opioid agents. This was a long-standing regulation under the Controlled Substances Act, but it received greater scrutiny and enforcement in 2009 (Center for Medicare Advocacy, Inc., 2010). Although advocacy groups argued that the answer to the problem was to ensure physician availability 24 hours a day, 7 days per week (Center for Medicare Advocacy, Inc., 2010), the actual result of this in several of our study facilities was the hindrance of prompt treatment of pain. Regulatory issues are recognized barriers to pain best practices (Jones et al., 2004; Tarzian & Hoffmann, 2005), and this finding suggests that investigators, administrators, and clinicians must remain vigilant to regulatory changes that can influence guideline implementation. It also emphasizes the need for teams that conduct intervention studies and quality improvement programs that work with regulatory groups, especially surveyors, to ensure that practice changes align with both good pain management and adherence to regulatory constraints.
One facilitator that has not received much attention in the pain assessment literature is the importance of involving a broad range of staff, including nonclinical staff. Several participants voiced strong support for empowering nursing assistants, dietary staff, activities directors, and others to observe for and report residents’ pain to nurses. The role of interdisciplinary approaches in pain assessment for older adults is well documented (Hadjistavropoulos et al., 2007), including the importance of nursing assistant involvement (Ersek, 2009). Our findings suggest that all staff who interact with residents should be trained to observe for and report pain. Empowering unlicensed clinical staff and nonclinical staff to take active roles in the care team is consistent with the “culture change” model of NH care (Koren, 2010) and can enhance staff morale, reduce turnover, and improve resident outcomes (Barry, Brannon, & Mor, 2005; Bishop, Squillace, Meagher, Anderson, & Wiener, 2009; Temple, Dobbs, & Andel, 2009).
Administrative support is a well-known enabler of positive practice change (Jones et al., 2004; Ploeg et al., 2007). Our study participants emphasized the influential role that stability in and support from the Director of Nursing or Clinical Services (DNS) has on adoption of evidence-based pain practices. This finding is consistent with earlier studies that found that fewer changes in senior managers are associated with higher adherence to practice guidelines (O’Halloran et al., 2007; Specht, 2013). Hunt et al. (2012) reported that longer DNS tenures were also significantly and positively associated with RN retention.
Residents’ and families’ attitudes and beliefs about the use of pain medications were also identified as barriers to the use of evidence-based guidelines for pain management. The intervention did not focus specifically on these two groups, although resident and family barriers are well documented (Jones et al., 2004, 2005). Addressing residents’ barriers will be increasingly important as NH care moves forward in its goal to be resident-centered. Intervening appropriately to address families’ misconceptions is also important to decrease family-staff conflict, which can hinder efforts to promote residents’ comfort (Ersek, Kraybill, & Hansberry, 1999).
Quantitative analyses corroborated the findings from the focus groups. Staff described several positive outcomes in pain assessment and management, and these perceived changes in practice were supported by statistically significant, albeit modest, increases in adherence to evidence-based pain management practices. Most of the improvement in adherence to best practices occurred specifically with pain assessment. This finding is not surprising for two reasons. First, baseline scores were lower on assessment practices when compared with management practices, so there was more room for improvement in this area. Second, the algorithm intervention focused on NH staff, whose primary role is to assess pain, rather than primary care providers (PCPs), who prescribed pain medications.
Focus group participants perceived that there were several physician-related barriers that likely hindered changes in prescribing regimens. These barriers have been reported by other investigators (Jones et al., 2004; Tarzian & Hoffmann, 2005). We attempted to involve physicians and other PCPs by inviting them to watch a 30-minute, Web-based video that explained the algorithms and the study. On completion, they received $100. PCPs were also invited to join the facility-based pain team. Despite these efforts, PCPs were involved in only a few of the pain teams, and only two of 75 PCPs viewed the Webinar (Ersek et al., 2012). Future intervention studies should strongly consider team-based pain interventions that directly engage PCPs and medical directors (Nazir et al., 2013).
LIMITATIONS
The study’s findings need to be interpreted with caution because of several limitations. First, we collected data from only four facilities in one geographical region. Second, focus groups were held only on the day shift with staff members who were able to take time away from care activities, whereas nursing assistants were underrepresented. Third, practice changes came from staff reports, which may have been subject to recall bias and desire to please the investigators. Finally, pre- and post-study designs provide weak evidence, and the use of chart documentation may not reflect actual practices. However, both the focus group and the chart audit data show practice changes, thereby increasing the credibility of the findings. Moreover, our study examined barriers and facilitators vis-à-vis actual practice changes that were measured using qualitative and quantitative data. Thus, we address the recommendation made in Lewin et al. (2009) to integrate mixed methods into clinical trials of complex interventions to better understand study findings and enhance the design of future interventions.
CONCLUSION
NH residents continue to experience persistent, unrelieved pain. This problem reflects both inadequate assessment and management of pain. Using qualitative and quantitative methods, we explored structural and process-level factors that were associated with outcomes of a complex multimodal intervention to increase the use of pain best practices. Our results provide guidance in understanding the impediments and enablers to adoption of best practices in the NH setting. Research and quality improvement teams can incorporate these findings to increase the likelihood of successful adoption in future efforts.
Acknowledgments
This study was supported by Award Number R01NR009100 from the National Institute of Nursing Research (NINR).
Footnotes
The authors have disclosed no potential conflicts of interest, financial or otherwise.
The content is the sole responsibility of the authors and does not necessarily represent the official views of the NINR, National Institutes of Health, Department of Veterans Affairs or the United States Government.
Contributor Information
Dr. Mary Ersek, Investigator, Center for Health Equity Research and Promotion, Philadelphia Veterans Affairs Medical Center, and Associate Professor, University of Pennsylvania School of Nursing, Philadelphia, Pennsylvania.
Dr. Anita Jablonski, Associate Professor, Seattle University College of Nursing, Seattle, Washington.
References
- Adli M, Bauer M, Rush AJ. Algorithms and collaborative-care systems for depression: Are they effective and why? A systematic review. Biological Psychiatry. 2006;59:1029–1038. doi: 10.1016/j.biopsych.2006.05.010. [DOI] [PubMed] [Google Scholar]
- American Geriatrics Society Panel on Pharmacological Management of Persistent Pain in Older Persons. Pharmacologic management of persistent pain in older persons. Journal of the American Geriatrics Society. 2009;57:1331–1346. doi: 10.1111/j.1532-5415.2009.02376.x. [DOI] [PubMed] [Google Scholar]
- American Medical Directors Association. Pain management in the long-term care setting. Columbia, MD: Author; 2012. [Google Scholar]
- Barry TT, Brannon D, Mor V. Nurse aide empowerment strategies and staff stability: Effects on nursing home resident outcomes. The Gerontologist. 2005;45:309–317. doi: 10.1093/geront/45.3.309. [DOI] [PubMed] [Google Scholar]
- Bishop CE, Squillace MR, Meagher J, Anderson WL, Wiener JM. Nursing home work practices and nursing assistants’ job satisfaction. The Gerontologist. 2009;49:611–622. doi: 10.1093/geront/gnp040. [DOI] [PubMed] [Google Scholar]
- Center for Medicare Advocacy, Inc. Nursing home residents’ access to physicians and pain medication. 2010 Retrieved from http://www.medicareadvocacy.org/nursing-home-residents-access-to-physicians-and-pain-medication.
- Centers for Medicare and Medicaid Services. Nursing home compare. 2013 Retrieved from http://www.medicare.gov/nursing-homecompare.
- Clarke HF, Bradley C, Whytock S, Handfield S, van der Wal R, Gundry S. Pressure ulcers: Implementation of evidence-based nursing practice. Journal of Advanced Nursing. 2005;49:578–590. doi: 10.1111/j.1365-2648.2004.03333.x. [DOI] [PubMed] [Google Scholar]
- Colón-Emeric CS, Lekan D, Utley-Smith Q, Ammarell N, Bailey D, Corazzini K, Anderson RA. Barriers to and facilitators of clinical practice guideline use in nursing homes. Journal of the American Geriatrics Society. 2007;55:1404–1409. doi: 10.1111/j.1532-5415.2007.01297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker SA, Culp KR, Cacchione PZ. Evaluation of musculoskeletal pain management practices in rural nursing homes compared with evidence-based criteria. Pain Management Nursing. 2009;10:58–64. doi: 10.1016/j.pmn.2008.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donabedian A. The quality of care. How can it be assessed? Journal of the American Medical Association. 1988;260:1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- Du Pen AR, Du Pen S, Hansberry J, Miller-Kraybill B, Millen J, Everly R, Syrjala K. An educational implementation of a cancer pain algorithm for ambulatory care. Pain Management Nursing. 2000;1:116–128. doi: 10.1053/jpmn.2000.19333. [DOI] [PubMed] [Google Scholar]
- Ersek M. Introduction. In: Ersek M, editor. Core curriculum for the hospice and palliative care nursing assistant. 2. Pittsburgh, PA: Hospice and Palliative Nurses Association; 2009. pp. 1–3. [Google Scholar]
- Ersek M, Kraybill BM, Hansberry J. Investigating the educational needs of licensed nursing staff and certified nursing assistants in nursing homes regarding end-of-life care. American Journal of Hospice & Palliative Care. 1999;16:573–582. doi: 10.1177/104990919901600406. [DOI] [PubMed] [Google Scholar]
- Ersek M, Polissar N, Du Pen A, Jablonski A, Herr K, Neradilek MB. Addressing methodological challenges in implementing the nursing home pain management algorithm randomized controlled trial. Clinical Trials. 2012;9:634–644. doi: 10.1177/1740774512454243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson SJ. IASP global year against pain in older persons: Highlighting the current status and future perspectives in geriatric pain. Expert Review of Neurotherapeutics. 2007;7:627–635. doi: 10.1586/14737175.7.6.627. [DOI] [PubMed] [Google Scholar]
- Gibson SJ, Lussier D. Prevalence and relevance of pain in older persons. Pain Medicine. 2012;13(Suppl):S23–S26. doi: 10.1111/j.1526-4637.2012.01349.x. [DOI] [PubMed] [Google Scholar]
- Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interventions to improve the management of depression in primary care: A systematic review. Journal of the American Medical Association. 2003;289:3145–3151. doi: 10.1001/jama.289.23.3145. [DOI] [PubMed] [Google Scholar]
- Grol R, Grimshaw J. From best evidence to best practice: Effective implementation of change in patients’ care. The Lancet. 2003;362:1225–1230. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- Hadjistavropoulos T, Herr K, Turk DC, Fine PG, Dworkin RH, Helme R, Williams J. An interdisciplinary expert consensus statement on assessment of pain in older persons. Clinical Journal of Pain. 2007;23(Suppl 1):S1–S43. doi: 10.1097/AJP.0b013e31802be869. [DOI] [PubMed] [Google Scholar]
- Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clinics of Geriatric Medicine. 2001;17:417–431. doi: 10.1016/s0749-0690(05)70078-1. [DOI] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Hunt SR, Probst JC, Haddock KS, Moran R, Baker SL, Anderson RA, Corazzini K. Registered nurse retention strategies in nursing homes: A two-factor perspective. Health Care Management Review. 2012;37:246–256. doi: 10.1097/HMR.0b013e3182352425. [DOI] [PubMed] [Google Scholar]
- Jablonski A, Ersek M. Nursing home staff adherence to evidence-based pain management practices. Journal of Gerontological Nursing. 2009;35(7):28–34. doi: 10.3928/00989134-20090428-03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jablonski AM, Du Pen AR, Ersek M. The use of algorithms in assessing and managing persistent pain in older adults. American Journal of Nursing. 2011;111(3):34–43. doi: 10.1097/10.1097/01.NAJ.0000395239.60981.2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones KR, Fink R, Vojir C, Pepper G, Hutt E, Clark L, Mellis BK. Translation research in long-term care: Improving pain management in nursing homes. Worldviews on Evidence-Based Nursing. 2004;1(Suppl 1):S13–S20. doi: 10.1111/j.1524-475X.2004.04045.x. [DOI] [PubMed] [Google Scholar]
- Jones KR, Fink RM, Clark L, Hutt E, Vojir CP, Mellis BK. Nursing home resident barriers to effective pain management: Why nursing home residents may not seek pain medication. Journal of the American Medical Directors Association. 2005;6:10–17. doi: 10.1016/j.jamda.2004.12.010. [DOI] [PubMed] [Google Scholar]
- Koh SSL, Manias E, Hutchinson AM, Donath S, Johnston L. Nurses’ perceived barriers to the implementation of a fall prevention clinical practice guideline in Singapore hospitals. BMC Health Services Research. 2008;8:105–114. doi: 10.1186/1472-6963-8-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koren MJ. Person-centered care for nursing home residents: The culture-change movement. Health Affairs. 2010;29:312–317. doi: 10.1377/hlthaff.2009.0966. [DOI] [PubMed] [Google Scholar]
- Lapane KL, Quilliam BJ, Chow W, Kim M. The association between pain and measures of well-being among nursing home residents. Journal of the American Medical Association. 2012;13:344–349. doi: 10.1016/j.jamda.2011.01.007. [DOI] [PubMed] [Google Scholar]
- Lewin S, Glenton C, Oxman AD. Use of qualitative methods alongside randomised controlled trials of complex healthcare interventions: Methodological study. BMJ. 2009;339:b3496. doi: 10.1136/bmj.b3496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazir A, Unroe K, Tegeler M, Khan B, Azar J, Boustani M. Systematic review of interdisciplinary interventions in nursing homes. Journal of the American Medical Directors Association. 2013;14:471–478. doi: 10.1016/j.jamda.2013.02.005. [DOI] [PubMed] [Google Scholar]
- O’Halloran PD, Cran GW, Beringer TR, Kernohan G, Orr J, Murray LJ. Factors affecting adherence to use of hip protectors amongst residents of nursing homes—A correlation study. International Journal of Nursing Studies. 2007;44:672–686. doi: 10.1016/j.ijnurstu.2005.12.005. [DOI] [PubMed] [Google Scholar]
- Ploeg J, Davies B, Edwards N, Gifford W, Miller PE. Factors influencing best-practice guideline implementation: Lessons learned from administrators, nursing staff, and project leaders. Worldviews on Evidence-Based Nursing. 2007;4:210–219. doi: 10.1111/j.1741-6787.2007.00106.x. [DOI] [PubMed] [Google Scholar]
- Rogers EM. Diffusion of innovations. 5. New York, NY: Free Press; 2003. [Google Scholar]
- Specht JK. Evidence based practice in long term care settings. Journal of Korean Academy of Nursing. 2013;43:145–153. doi: 10.4040/jkan.2013.43.2.145. [DOI] [PubMed] [Google Scholar]
- Takai Y, Yamamoto-Mitani N, Okamoto Y, Koyama K, Honda A. Literature review of pain prevalence among older residents of nursing homes. Pain Management Nursing. 2010;11:209–223. doi: 10.1016/j.pmn.2010.08.006. [DOI] [PubMed] [Google Scholar]
- Tarzian AJ, Hoffmann DE. Barriers to managing pain in the nursing home: Findings from a statewide survey. Journal of the American Medical Directors Association. 2005;6(Suppl 3):S13–S19. doi: 10.1016/j.jamda.2005.03.016. [DOI] [PubMed] [Google Scholar]
- Temple A, Dobbs D, Andel R. Exploring correlates of turnover among nursing assistants in the National Nursing Home Survey. Health Care Management Review. 2009;34:182–190. doi: 10.1097/HMR.0b013e31819c8b11. [DOI] [PubMed] [Google Scholar]