Abstract
Purpose
To determine inter-device agreement for central corneal thickness (CCT) measurement among ultrasound pachymetry, rotating Scheimpflug imaging (Pentacam, Oculus, Wetzlar, Germany), and scanning slit corneal topography (Orbscan II, Bausch & Lomb, Rochester, NY, USA) in highly myopic eyes before and after photorefractive keratectomy (PRK).
Methods
This prospective comparative study included 61 eyes of 32 patients with high myopia who underwent PRK. Six month postoperative CCT values were compared to preoperative values in 27 patients (51 eyes) who completed the follow up period. To determine the level of agreement, Pentacam and Orbscan II readings were compared to ultrasonic pachymetry measurements as the gold standard method.
Results
Mean CCT measurements with ultrasound, Pentacam, and Orbscan II before PRK were 557µm, 556µm, and 564µm, respectively; and 451µm, 447µm, and 438µm 6 months after surgery in the same order. Preoperatively, the 95% limits of agreement (LoA) with ultrasound measurements were -20μm to 17μm for Pentacam and -21μm to 33μm for Orbscan II. Six months postoperatively, the 95% LoA were -30μm to 23μm for Pentacam and -69μm to 43μm for Orbscan II.
Conclusion
Preoperatively, CCT measurements were higher with Orbscan II as compared to ultrasound. Postoperatively, both Pentacam and Orbscan II measurements were lower than those obtained with ultrasound, but Pentacam had better agreement. The use of ultrasound, as the gold standard method, or Pentacam both appear to be preferable over Orbscan II among patients with high myopia.
Keywords: Myopia, Central Corneal Thickness, Photorefractive Keratectomy, Ultrasound Pachymetry Pentacam, Orbscan II
INTRODUCTION
A major concern in refractive surgery is accurate measurement of corneal thickness. This issue is critical in patients with high myopia because more tissue needs to be ablated to achieve emmetropia; while overestimation can be associated with the risk of postoperative keratectasia, underestimation may lead to inadvertent exclusion of patients because of concerns about insufficient corneal thickness.1,2
Ultrasonic pachymetry is currently the gold standard for measuring corneal thickness, however it suffers from limitations including the necessity for topical anesthesia, direct contact of the probe with the cornea and hence the risk of infection, the risk of incorrect probe placement, poor fixation and variations in sound wave speed due to different degrees of corneal hydration.3-5 The accuracy of ultrasonic pachymetry requires perpendicular placement of the probe onto the corneal surface, therefore examiner’s experience can affect the reliability of measurements.6
Using optical systems such as scanning slit topography (Orbscan II) and Scheimpflug photography (Pentacam), pachymetry may be performed without the need for direct contact with the corneal surface. Using ultrasonic pachymetry as the gold standard, many comparative studies have examined corneal thickness measurements of Pentacam,7-11 and Orbscan II12-16. There have also been several reports comparing these three methods.5, 17-22 To the best of our knowledge, however, there is no study comparing Orbscan II, Pentacam, and ultrasonic pachymetry in individuals with high myopia. We performed this prospective comparative study to compare central corneal thickness (CCT) measurements in highly myopic patients before photorefractive keratectomy (PRK) and six months afterwards employing the Orbscan II scanning slit topographer (Bausch & Lomb, Rochester, New York, USA), Pentacam Scheimpflug imaging system (Oculus, Wetzlar, Germany), and ultrasonic pachymeter as the gold standard (Tomey SP-3000 Pachymeter, Tomey, Nagoya, Japan).
METHODS
This prospective comparative study was conducted from May 2009 to January 2011 at two clinical sites in Tehran, Iran: Imam Hossein Medical Center and Vanak Eye Surgery Center. Approval to conduct this study was obtained from the Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran and the study followed the tenets of the Declaration of Helsinki. All highly myopic patients at these two centers who were scheduled for PRK and met the inclusion criteria were enrolled; informed consent was obtained from all subjects. Inclusion criteria were age from 19 to 52 years, myopia between 6.0 and 10.0 diopters, stable refraction for at least one year, no soft contact lens wear for two weeks, no hard contact lens wear for six weeks before baseline examinations, and predicted postoperative residual corneal thickness more than 420 microns (µm). Exclusion criteria were history of systemic diseases, especially autoimmune or collagen vascular diseases, diabetes mellitus, corneal ectasia, and any ocular diseases other than refractive error, history of eye surgery, forme fruste keratoconus, and monocular status.
Pre- and Postoperative Assessment
Pre- and six-month postoperative assessment included refraction, Snellen best-corrected visual acuity (BCVA), slit lamp examination and dilated fundus examination. To minimize the diurnal variations in CCT measurements, all examinations were performed at the same time of the day, from 9 to 10 AM; all pre- and postoperative CCT measurements were obtained by an expert optometrist using, in order, Pentacam, Orbscan II, and ultrasonic pachymetry. For Orbscan II, an acoustic equivalent correction factor of 0.94 was utilized to adjust the readings. Before ultrasonic pachymetry, tetracaine 0.5% eye drops were used for corneal anesthesia. With all three devices, a single measurement was performed, unless results appeared unreliable. The Tomey SP-3000 Pachymeter was set to calculate the average of 10 measurements with a single touch, and the standard deviation was checked to ensure accuracy.
Surgical Technique
All patients underwent conventional PRK by the same surgeon (Nader Nassiri) using the Allegretto Wave Eye-Q (software version 2.020 default treatment, Alcon Laboratories, Inc., Fort Worth, United States). After initial preparations, the epithelium was removed mechanically with a hockey knife, followed by photoablation. Mitomycin-C 0.02% (MMC, 0.2 mg/ml) was applied for 30-55 seconds depending on ablation depth. The eyes were then irrigated with 50 ml balanced salt solution and a bandage contact lens was fitted. Postoperative medications consisted of ciprofloxacin 0.3% and betamethasone 0.1% eye drops until complete corneal reepithelialization; the latter was continued four times daily for one month and tapered over the next month.
Statistical Analysis
According to previous studies, the comparison between Orbscan II and ultrasonic pachymetry needed a higher number of eyes; therefore sample size calculation was based on this comparison. Based on a pilot study on 10 patients, the highest standard deviation for CCT readings was 15µm. Considering an alpha error of 0.05 (two-sided) and statistical power of 95%, 48 eyes were required to be able to detect a difference of 10 microns. We added 25% to this number to compensate for possible dropouts, therefore 60 eyes were required for the purpose of the study.
All statistical analyses were performed using SPSS software (Version 17, SPSS Inc., Chicago, Illinois, USA). P-values less than 0.05 were considered as statistically significant. We summarized data as mean ± standard deviations, median, range, and 95% confidence intervals. To evaluate the inter-device agreement for CCT measurements, we calculated 95% limits of agreement (LoA), and used folded cumulative distribution plots of difference percentiles. To account for the correlation of CCT measurements in bilateral cases, the design effect was considered in calculating the standard deviations.
RESULTS
Of thirty-two highly myopic patients (61 eyes), 27 subjects (51 eyes) completed the trial. Five patients (10 eyes, one male and four female subjects) did not return for postoperative measurements. Table 1 depicts baseline and surgery-related data. There was no evidence of corneal ectasia or corneal haze among our patients during the follow-up period.
Table 1.
Patients’ baseline characteristics
| Variable | Summary |
|---|---|
| Age | |
| Mean ± SD | 26 ± 6.3 |
| Range | (19 to 36) years |
| Male/Female | 5/22 |
| Left /Right (%) | 27/24 (52.9) |
| Spherical equivalent | |
| Median | -6.50 |
| Range | (-6 to -9.25) Diopters |
| Cylindrical power | |
| Median | 1.25 |
| Range | (0 to 4.75) Diopters |
| BCVA | |
| Mean ±SD | 0.02 ±0.06 LogMAR |
| Ablation depth | |
| Mean ±SD | 104 ±16 microns |
| Duration of Mitomycin C | |
| Mean ±SD | 27 ± 9 seconds |
BCVA, best corrected visual acuity
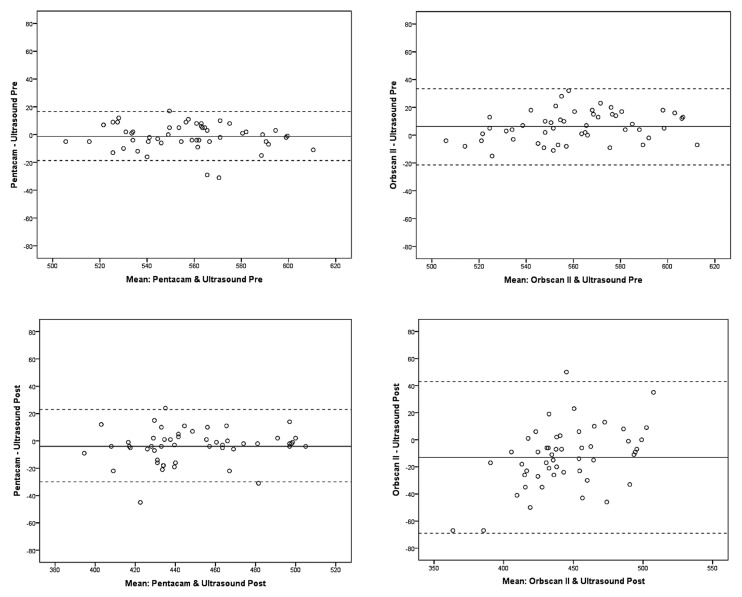
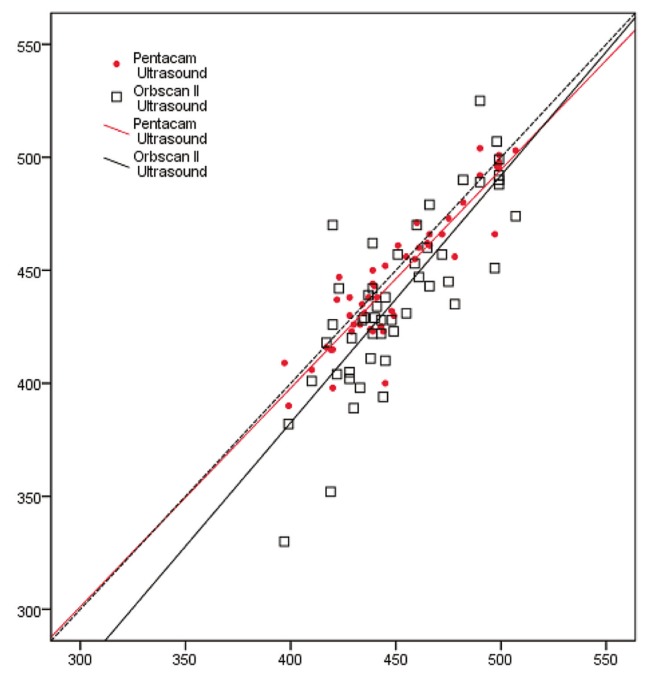
A summary of pre- and postoperative CCT readings measured with ultrasonic pachymetry, Pentacam, and Orbscan II is presented in Table 2. Table 3 summarizes differences between ultrasonic pachymetry and Orbscan II, as well as ultrasonic pachymetry and Pentacam, in terms of CCT measurements preoperatively and 6 months postoperatively. Orbscan II demonstrated greater differences and wider 95% LoA than Pentacam both before and after surgery. Inter-device agreement plots are demonstrated in figure 1. Scatter plots of pre- and postoperative CCT readings with these three devices are presented in figures 2 and 3, respectively.
Table 2.
Mean ± standard deviation (SD) and range of central corneal thickness readings measured with ultrasonic pachymetry, Pentacam and Orbscan II before and after surgery, and the resulting mean change and 95% confidence interval (CI) of the calculated mean difference
| Preoperative | Six-month postoperative | Difference | ||||
|---|---|---|---|---|---|---|
| Device | Mean ± SD | Range | Mean ± SD | Range | Mean ± SD | 95% CI of difference |
| Ultrasound | 557±34 | 508 to 616 | 451±38 | 397 to 507 | 106±26 | 99 to 114 |
| Pentacam | 556±33 | 501 to 605 | 447±41 | 390 to 504 | 109±27 | 101 to 117 |
| Orbscan II | 564±38 | 504 to 613 | 438±51 | 330 to 525 | 125±30 | 117 to 134 |
Table 3.
Comparison of central corneal thickness (CCT) in microns between paired methods. Inter-device differences are expressed in mean ± standard deviations (SD), median, range, 95% confidence interval (CI) together with the statistical significance of the difference. Inter-device agreement is demonstrated with 95% limits of agreement (LoA) and Pearson correlation coefficients (r)
| Mean difference±SD | Median | Range | 95% CI | P value | 95% LoA | r | |
|---|---|---|---|---|---|---|---|
| Preoperative | |||||||
| Pentacam/ Ultrasound | -1±9 | 0 | -31 to 37 | -4 to 1 | 0.32 | -20 to 17 | 0.927 |
| Orbscan II/Ultrasound | 6±14 | 5 | -22 to 42 | 2 to 10 | <0.001 | -21 to 33 | 0.921 |
| Postoperative | |||||||
| Pentacam/ Ultrasound | -4±13 | -3 | -45 to 24 | -8 to 0 | 0.031 | -30 to 23 | 0.914 |
| Orbscan II/ Ultrasound | -13±29 | -11 | -67 to 50 | -21 to -4 | <0.001 | -69 to 43 | 0.812 |
Figure 1.
Pre- and postoperative 95% limits of agreement for central corneal thickness; the limits of agreement are narrower between ultrasonic pachymetry and Pentacam as compared to that between ultrasonic pachymetry and Orbscan II.
Figure 2.
Scatter plot of Pentacam and Orbscan II, preoperative CCT measurement versus ultrasonic measurements. The dotted line represents the line of equivalence (CCT, central corneal thickness).
Figure 3.
Scatter plot of Pentacam and Orbscan II, postoperative CCT measurement versus ultrasonic measurements. The dotted line represents the line of equivalence (CCT, central corneal thickness).
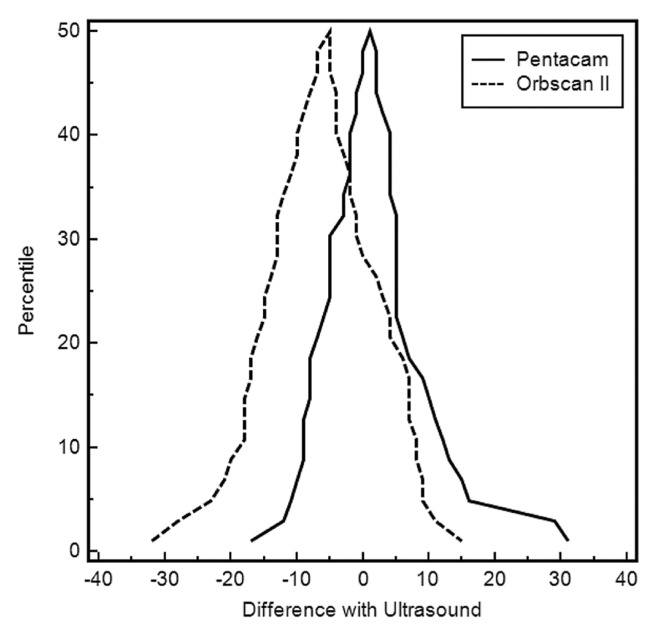
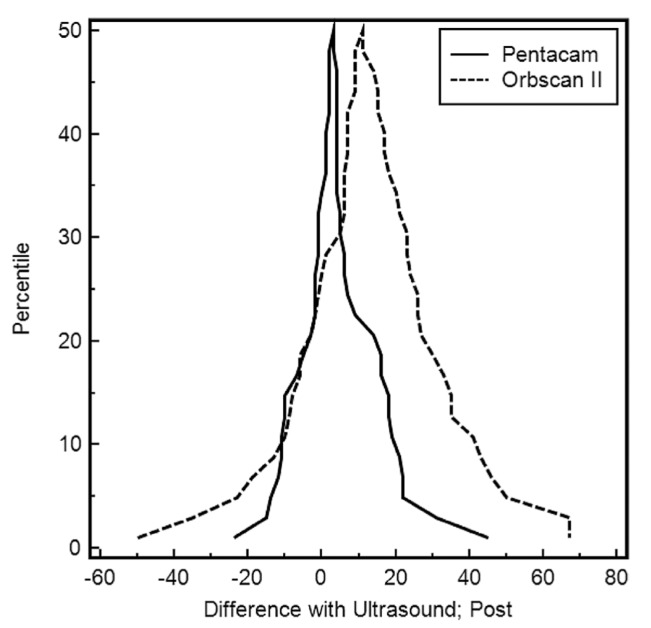
Figure 4 shows the preoperative folded cumulative distribution plot (mountain plot) of percentiles for differences between Pentacam and Orbscan II versus ultrasound measurements. The preoperative plot for Pentacam readings was closer to zero and narrower, as compared to that of Orbscan II which shows a left shift (higher readings), indicating better agreement between Pentacam and ultrasound. In the postoperative folded cumulative distribution plot shown in figure 5, the plot for Pentacam readings is again closer to zero and narrower than Orbscan II, but Orbscan II readings show a right shift, proving lower readings as compared to ultrasound.
Figure 4.
Preoperative folded cumulative distribution plot (mountain plot) of percentiles for differences of Pentacam and Orbscan II versus ultrasound measurements.
Figure 5.
Postoperative folded cumulative distribution plot (mountain plot) for pachymetry, Pentacam and Orbscan II.
DISCUSSION
In this comparative study, we measured CCT in patients with high myopia using Orbscan II, Pentacam, and compared the results with ultrasonic readings.
Comparing CCT measurements obtained with different devices such as ultrasound devices, Pentacam, and Orbscan, most studies agree that correlations are generally appropriate. Main inconsistencies found among the results are in the mean inter-device difference and their 95% LoA. In calculating the mean difference, negative and positive values would cancel each other out; statistically speaking, this test shows how far the mean difference falls from zero, and whether a particular device generally underestimates or overestimates the measured value as compared to another. However, the range of differences and standard deviations of the mean can show how widely data are distributed, thus the 95% LoA is a better indicator of device agreement and interchangeability.
Preoperatively, Orbscan showed a tendency to overestimate CCT readings as compared to ultrasound and their 95% LoA in our study was -21 to 33µm (width=54µm). Pentacam slightly underestimated CCT as compared to the ultrasonic device and their 95% LoA were -20 to 17µm (width=37µm). Results of other similar studies are not considerably different and there is general agreement that Pentacam outperforms Orbscan in measuring CCT in virgin eyes.5
Comparing measurements between Pentacam and ultrasound, reports indicate that agreement is slightly worse after refractive surgery compared to before surgery.5,11 However, comparative studies on Orbscan CCT measurements in eyes after refractive surgery show even less consistency. In the study by Kim et al, Orbscan II measurements were on average 69 microns less than ultrasound readings early in the postoperative period, and changed to a 36-micron difference when measurements were repeated 1-3 months later.18 Studying patients 6 weeks after keratorefractive surgery, Hashemi and Mehravaran5 found a 40µm underestimation with Orbscan II (x0.92) and a 90µm wide 95% LoA with ultrasonic pachymetry. This is in contrast to the report by Ho et al who observed no statistically significant difference in readings between Orbscan II and ultrasound six months after LASIK despite a 95% LoA of -35.59 to +41.67 (width=77µm).19. Faramarzi et al reported that their corrected 5-month postoperative Orbscan II readings (x0.96) were on average 9 microns higher than ultrasound readings in myopic patients who underwent PRK, and they calculated a 95% LoA of -22 to +40 (width=60µm) between postoperative Orbscan and ultrasound readings.12 In the same study, the 95% LoA between Orbscan and ultrasound readings 6 months after surgery had increased to -69 to 43 μm (width=102).
With the Orbscan II, corneal thickness is measured as the distance between the air/tear film interface as the anterior reference and the corneal endothelium as the posterior reference, but using the ultrasound method, the posterior reference is between Descemets membrane and the anterior chamber. Compared to Orbscan II, direct contact of the ultrasound probe may displace the tear film and underestimate corneal thickness. To overcome discrepancies between these two devices, the use of a correction factor has been suggested for Orbscan II readings.22 However, the discrepancy between these two devices is reversed in postoperative readings, i.e. overestimation changes to underestimation. This observation can be explained by the effect of corneal thickness itself on Orbscan measurements; Hashemi et al23 have demonstrated that Orbscan tends to underestimate CCT in thinner eyes even without surgery. This can also explain the variation observed in the results of different studies.
In terms of the agreement between Orbscan and ultrasound, the 95% LoA in operated eyes in this study almost doubled as compared to the preoperative range, which is relatively worse than results of previous studies. This can partly be attributed to the fact that we adjusted for design effect (using both eyes of the same person), therefore true variations were provided in the sample. Previous studies using both eyes of the same subject as individual cases might have overestimated inter-device agreements.
In conclusion, preoperative CCT measurements were higher with Orbscan II as compared to ultrasound. Postoperatively, both Pentacam and Orbscan II measurements were lower than ultrasound, but Pentacam had closer agreement with ultrasound as the gold standard method. The use of ultrasound and Pentacam in patients with high myopia appears to be preferable to Orbscan II, although none should be used interchangeably.
Footnotes
Conflicts of Interest
None.
REFERENCES
- 1.Iskandar NG, Peters NT, Penno EA, Gimbel HV. Postoperative complications in laser in situ keratomileusis. Curr Opin Ophthalmol. 2000;11:273–279. doi: 10.1097/00055735-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Prisant O, Calderon N, Chastang P, Gatinel D, Hoang-Xuan T. Reliability of pachymetric measurements using orbscan after excimer refractive surgery. Ophthalmology. 2003;110:511–515. doi: 10.1016/S0161-6420(02)01298-8. [DOI] [PubMed] [Google Scholar]
- 3.Miglior S, Albe E, Guareschi M, Mandelli G, Gomarasca S, Orzalesi N. Intraobserver and interobserver reproducibility in the evaluation of ultrasonic pachymetry measurements of central corneal thickness. Br J Ophthalmol. 2004;88:174–177. doi: 10.1136/bjo.2003.023416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solomon OD. Corneal indentation during ultrasonic pachometry. Cornea. 1999;18:214–215. doi: 10.1097/00003226-199903000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Hashemi H, Mehravaran S. Central corneal thickness measurement with Pentacam, Orbscan II, and ultrasound devices before and after laser refractive surgery for myopia. J Cataract Refract Surg. 2007;33:1701–1707. doi: 10.1016/j.jcrs.2007.05.040. [DOI] [PubMed] [Google Scholar]
- 6.Kawana K, Tokunaga T, Miyata K, Okamoto F, Kiuchi T, Oshika T. Comparison of corneal thickness measurements using Orbscan II, non-contact specular microscopy, and ultrasonic pachymetry in eyes after laser in situ keratomileusis. Br J Ophthalmol. 2004;88:466–468. doi: 10.1136/bjo.2003.030361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Módis L, Szalai E, Németh G, Berta A. Reliability of the corneal thickness measurements with the Pentacam HR imaging system and ultrasound pachymetry. Cornea. 2011;30:561–566. doi: 10.1097/ICO.0b013e318200096a. [DOI] [PubMed] [Google Scholar]
- 8.Huang J, Pesudovs K, Yu A, Wright T, Wen D, Li M, et al. A comprehensive comparison of central corneal thickness measurement. Optom Vis Sci . 2011;88:940–949. doi: 10.1097/OPX.0b013e31821ffe2c. [DOI] [PubMed] [Google Scholar]
- 9.Hashemi H, Jafarzadehpur E, Mehravaran S, Rezvan F, Bigdeli S. Comparison of corneal thickness measurement with the Pentacam, the PARK1 and an ultrasonic pachymeter. Clin Exp Optom . 2011;94:433–437. doi: 10.1111/j.1444-0938.2010.00572.x. [DOI] [PubMed] [Google Scholar]
- 10.Al-Mezaine HS, Al-Amro SA, Kangave D, Al-Obeidan S, Al-Jubair KM. Comparison of central corneal thickness measurements using Pentacam and ultrasonic pachymetry in post-LASIK eyes for myopia. Eur J Ophthalmol . 2010;20:852–857. doi: 10.1177/112067211002000507. [DOI] [PubMed] [Google Scholar]
- 11.Ciolino JB, Khachikian SS, Belin MW. Comparison of corneal thickness measurements by ultrasound and scheimpflug photography in eyes that have undergone laser in situ keratomileusis. Am J Ophthalmol . 2008;145:75–80. doi: 10.1016/j.ajo.2007.08.026. [DOI] [PubMed] [Google Scholar]
- 12.Faramarzi A, Karimian F, Jafarinasab MR, Jabbarpoor Bonyadi MH, Yaseri M. Central corneal thickness measurements after myopic photorefractive keratectomy using Scheimpflug imaging, scanning-slit topography, and ultrasonic pachymetry. J Cataract Refract Surg . 2010;36:1543–1549. doi: 10.1016/j.jcrs.2010.03.042. [DOI] [PubMed] [Google Scholar]
- 13.Paul T, Lim M, Starr CE, Lloyd HO, Coleman DJ, Silverman RH. Central corneal thickness measured by the Orbscan II system, contact ultrasound pachymetry, and the Artemis 2 system. J Cataract Refract Surg . 2008;34:1906–1912. doi: 10.1016/j.jcrs.2008.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng AC, Rao SK, Lau S, Leung CK, Lam DS. Central corneal thickness measurements by ultrasound, Orbscan II, and Visante OCT after LASIK for myopia. J Refract Surg . 2008;24:361–365. doi: 10.3928/1081597X-20080401-08. [DOI] [PubMed] [Google Scholar]
- 15.Li EY, Mohamed S, Leung CK, Rao SK, Cheng AC, Cheung CY. Agreement among 3 methods to measure corneal thickness: ultrasound pachymetry, Orbscan II, and Visante anterior segment optical coherence tomography. Ophthalmology . 2007;114:1842–1847. doi: 10.1016/j.ophtha.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 16.Doughty MJ, Jonuscheit S. An assessment of regional differences in corneal thickness in normal human eyes, using the Orbscan II or ultrasound pachymetry. Optometry . 2007;78:181–190. doi: 10.1016/j.optm.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 17.González-Pérez J, González-Méijome JM, Rodríguez Ares MT, Parafita MA. Central corneal thickness measured with three optical devices and ultrasound pachometry. Eye Contact Lens . 2011;37:66–70. doi: 10.1097/ICL.0b013e31820c6ffc. [DOI] [PubMed] [Google Scholar]
- 18.Kim SW, Byun YJ, Kim EK, Kim TI. Central corneal thickness measurements in unoperated eyes and eyes after PRK for myopia using Pentacam, Orbscan II, and ultrasonic pachymetry. J Refract Surg . 2007;23:888–894. doi: 10.3928/1081-597X-20071101-04. [DOI] [PubMed] [Google Scholar]
- 19.Ho T, Cheng AC, Rao SK, Lau S, Leung CK, Lam DS. Central corneal thickness measurements using Orbscan II, Visante, ultrasound, and Pentacam pachymetry after laser in situ keratomileusis for myopia. J Cataract Refract Surg . 2007;33:1177–1182. doi: 10.1016/j.jcrs.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 20.Gorgun E, Yenerel NM, Dinc UA, Oncel B, Kucumen RB, Oral D. Comparison of non-contact methods for the measurement of central corneal thickness. Ophthalmic Surg Lasers Imaging . 2011;42:400–407. doi: 10.3928/15428877-20110812-02. [DOI] [PubMed] [Google Scholar]
- 21.Sedaghat MR, Daneshvar R, Kargozar A, Derakhshan A, Daraei M. Comparison of central corneal thickness measurement using ultrasonic pachymetry, rotating Scheimpflug camera, and scanning-slit topography. Am J Ophthalmol . 2010;150:780–789. doi: 10.1016/j.ajo.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 22.Amano S, Honda N, Amano Y, Yamagami S, Miyai T, Samejima T. Comparison of central corneal thickness measurements by rotating Scheimpflug camera, ultrasonic pachymetry, and scanning-slit corneal topography. Ophthalmology . 2006;113:937–941. doi: 10.1016/j.ophtha.2006.01.063. [DOI] [PubMed] [Google Scholar]
- 23.Hashemi H, Roshani M, Mehravaran S, Parsafar H, Yazdani K. Effect of corneal thickness on the agreement between ultrasound and Orbscan II pachymetry. J Cataract Refract Surg. 2007;33:1694. doi: 10.1016/j.jcrs.2007.05.036. [DOI] [PubMed] [Google Scholar]