Abstract
Purpose
To ascertain the patterns of uveitis at Motahari uveitis clinic, Shiraz University of Medical Sciences, a tertiary referral center in Shiraz, Southern Iran.
Methods
All new cases of uveitis referred from June 2005 to July 2011 to our center were consecutively enrolled in the study. After taking a complete history of systemic and ocular diseases, all patients underwent a complete ophthalmologic examination including determination of Snellen visual acuity, slit lamp biomicroscopy, applanation tonometry and dilated fundus examination. Patients were classified according to International Uveitis Study Group definitions.
Results
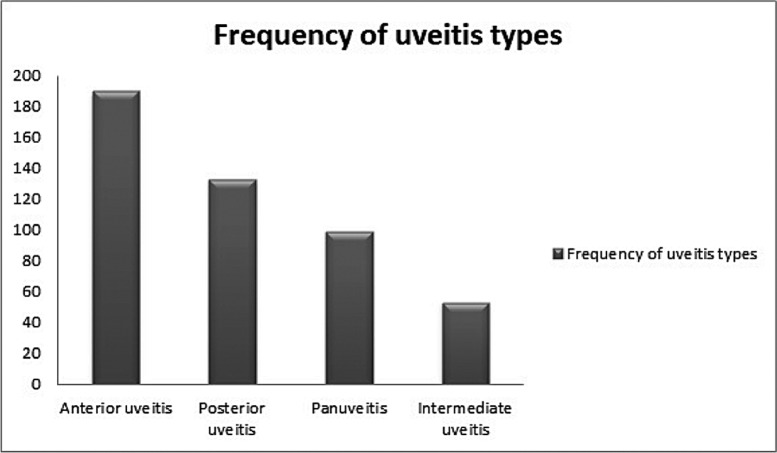
A total of 475 subjects were evaluated; mean age at the onset of uveitis was 30.5 ±15.14 years. Uveitis was unilateral in 292 (61.4%) and bilateral in 183 (38.6%) patients. Anterior uveitis was the most common type of inflammation (190 patients, 40%), followed by posterior uveitis (133 patients, 28%), panuveitis (99 patients, 20.8%) and intermediate uveitis (53 patients, 11.1%). A specific cause was found in 295 patients (61.9%). HLA-B27 negative was the most common cause of anterior uveitis (84 patients, 44.2%), Behcet's disease was the most common etiology of panuveitis (34 cases, 34.3%) and toxoplasmosis was the most common cause of posterior uveitis (56 patients, 42.1%). The great majority of intermediate uveitis cases were idiopathic (49 patients, 92.4%).
Conclusion
The most common type of uveitis in Southern Iran is anterior. The most common underlying disorders are HLA-B27 negative, toxoplasmosis and Behcet's disease.
Keywords: Uveitis, Epidemiology, Shiraz, Iran
INTRODUCTION
Uveitis is a general term describing inflammation of the uveal tract with or without involvement of adjacent structures. It may be caused by a variety of infectious or non-infectious disorders and is frequently associated with a systemic disease. It is believed that uveitis accounts for up to 10% of legal blindness in the United States.1,2
The incidence and patterns of uveitis should be defined in each population to avoid expensive and redundant screening regarding the limited resources. Multiple studies on uveitis patterns in different countries have displayed both similarities and differences; however there is limited data on uveitis in Middle Eastern countries.3-7 In this study we identify demographics and clinical features of uveitis at a referral center in Southern Iran.
METHODS
This study included all new uveitis patients who were referred from June 2005 to July 2011 to Motahari uveitis clinic which is a tertiary referral center affiliated to Shiraz University of Medical Sciences and covers a large area of Southern Iran. Patients with post-operative complications, post-surgery uveitis and trauma were excluded. A detailed standard uveitis questionnaire was filled for each case.8
A complete ophthalmologic and systemic history was obtained from all patients, followed by review of systems. Ocular examinations included determination of best corrected Snellen visual acuity, external eye examination, slit lamp biomicroscopy, applanation tonometry, Marcus-Gunn pupil testing, and dilated fundus examination with an indirect ophthalmoscope and three-mirror contact lenses. Some cases required additional work-up such as fluorescein angiography, visual field testing, electrophysiology tests or ophthalmic ultrasonography. If indicated, patients underwent a standard protocol for evaluating the etiologies of uveitis or systemic associations, including consultation with rheumatologists and infectious disease specialists.
Uveitis was classified according to the International Uveitis Study Group (IUSG) criteria based on the anatomic location of the inflammation and categorized as anterior, intermediate, posterior, or panuveitis; and also based on the group’s refinement description for clinical onset, duration and course.9
Anterior uveitis was defined when there was only irits and/or iridocyclitis. Intermediate uveitis was defined as inflammation confined to the middle portion of the eye (posterior ciliary body, pars plana). Posterior uveitis was defined as intraocular inflammation primarily involving the retina and/or choroid. Panuveitis (diffuse uveitis) was defined as inflammation in the anterior chamber, vitreous, and retina or choroid.
Based on the course of the condition, uveitis was classified as acute, with sudden onset inflammation lasting for less than 3 months; chronic uveitis, as inflammation lasting for more than 3 months; and recurrent when repeated episodes of intraocular inflammation were separated by periods of inactivity without treatment for ≥ 3 months.
Patients were classified as having non-granulomatous uveitis if there were small keratic precipitates on the corneal endothelium without iris nodules or choroidal granulomas; or granulomatous uveitis if large "mutton-fat" keratic precipitates, iris nodules and/or optic disc and choroidal granulomas were present. Whenever, despite all ocular and systemic evaluation and work-up, no specific ocular or systemic condition was revealed, the patient was classified as having idiopathic uveitis.
RESULTS
A total of 475 patients including 259 (54.5%) female and 216 (45.5%) male subjects were studied; Table 1 summarizes their general features. All patients were Caucasian and female to male ratio was 1.2:1. Mean age of the patients was 30.5±15.14 years and mean follow up duration was 41±17.25 months.
Table 1.
General features and distribution of patients based on different schemes for classification of uveitis
| Characteristic | No. (%) |
|---|---|
| Mean age (years) | 30.5; range, 5-56 |
|
| |
| Gender | |
| Male | 216 (45.5%) |
| Female | 259 (54.5%) |
|
| |
| Mean Follow-up (months) | 41; range, 10-132 |
|
| |
| Laterality | |
| Unilateral | 292 (61.4%) |
| Bilateral | 183 (38.6%) |
|
| |
| Clinical course | |
| Acute | 157 (33.1%) |
| Chronic | 318 (66.9%) |
|
| |
| Histologic type of inflammation | |
| Granulomatous | 52 (11%) |
| Non-granulomatous | 423 (89%) |
|
| |
| Infectious vs. Non-infectious | |
| Infectious | 110 (23.1%) |
| Non-infectious | 365 (76.9%) |
Uveitis was unilateral in 292 (61.4%) and bilateral in 183 (38.6%) patients. The clinical presentation was acute in 157 (33.1%) and chronic in 318 (66.9%) subjects. Uveitis was predominantly non-granulomatous (89% versus 11%) and non-infectious (76.9% versus 23.1%).
A specific etiology was found in 295 cases (61.9%) including infections in 110 patients (23.1%), systemic disease associations in 103 patients (21.6%), and a specific ocular disease in 82 patients (17.2%); the remaining 180 (38.1 %) cases were labelled as idiopathic. In the infectious uveitis group, toxoplasmosis (56 cases, 50.9%) was the most common diagnosis. Behcet's disease was the most common (59 cases, 57.2%) systemic disease and Fuch's heterochromic iridocyclitis (34 cases, 41.4%) was the most common ocular condition causing uveitis (Table 2).
Table 2.
Causes of uveitis in patients with definite diagnoses
| Number (%) | |
|---|---|
| Infectious diseases | |
| Herpetic uveitis | 15 (13.6) |
| Toxoplasmosis | 56 (50.9) |
| Toxocariasis | 6 (5.6) |
| Tuberculosis | 2 (1.8) |
| Acute retinal necrosis | 11 (10) |
| Cytomegalovirus retinitis | 5 (4.5) |
| HIV-Associated uveitis | 2 (1.8) |
| Fungal retinitis | 1 (0.9) |
| Herpes zoster uveitis | 1 (0.9) |
| Endogenous endophthalmitis | 11 (10) |
|
| |
| Total | 110 (23.1% of total cases) |
|
| |
| Collagen vascular diseases | |
| Behcet’s disease | 59 (57.2) |
| Juvenile idiopathic arthritis | 15 (14.5) |
| Seronegative spondylarthropathies | |
| Ankylosing spondylitis | 4 (3.9) |
| Nonspecific arthropathy (HLA-B27+) | 10 (9.9) |
| Inflammatory bowel disease | |
| Ulcerative colitis | 1 (0.9) |
| Sarcoidosis (confirmed/presumed) | 6 [4/2] (5.9) |
| Multiple sclerosis | 1 (0.9) |
| Systemic lupus erythematosus | 5 (4.9) |
| Masquerade Syndromes | |
| Leukemia (ALL-L2) | 2 (1.9) |
|
| |
| Total | 103 (21.6 of total cases) |
|
| |
| Ocular diseases (Non-infectious) | |
| Fuchs’ heterochromic iridocyclitis | 34 (41.4) |
| VKH disease | 25 (30.4) |
| Multifocal choroiditis and panuveitis | 3 (3.6) |
| Serpiginous choroiditis | 5 (6.3) |
| APMPPE | 3 (3.6) |
| Sympathetic ophthalmia | 3 (3.6) |
| Posner–Schlossman syndrome | 3 (3.6) |
| MEWDS | 1 (1.3) |
| Punctate inner choroidopathy | 1 (1.3) |
| Birdshot retinochoroidopathy | 1 (1.3) |
| Eales disease | 3 (3.6) |
|
| |
| Total | 82 (17.2% of total cases) |
HIV, human immunodeficiency virus; HLA, human leukocte antigen; ALL, acute lymphoblastic leukemia; VKH, Vogt-Koyanagi-Harada; APMPPE, acute placoid multifocal posterior pigment epitheliopathy; MEWDS, multiple evanescent white dot syndrome
Anterior uveitis (190 cases, 40%) was the most common type (Figure 1), of which the majority of cases were idiopathic (103 cases, 54.2%). HLA-B27 negative cases formed the majority of idiopathic anterior uveitis (84 cases, 44.2%). Fuchs' heterochromic iridocyclitis (34 cases, 17.8%) was the second most common cause of anterior uveitis (Table 3).
Figure 1.
The frequency of uveitis in different anatomical locations.
Table 3.
Etiologies of anterior uveitis
| Causes | Number (%) |
|---|---|
| Idiopathic anterior uveitis | |
| HLA-B27-negative | 84 (44.2) |
| HLA-B27-positive | 19 (10.0) |
| Fuchs’ heterochromic iridocyclitis | 34 (17.8) |
| Hepetic uveitis | 15 (7.8) |
| Ankylosing spondylitis | 4 (2.2) |
| Behcet’s disease | 4 (2.2) |
| Nonspecific arthropathy | 10 (5.2) |
| Posner-Schlossman syndrome | 3 (1.6) |
| Juvenile idiopathic arthritis | 15 (7.9) |
| Sarcoidosis | 1 (0.55) |
| Ulcerative colitis | 1 (0.55) |
|
| |
| Total | 190 (100) |
HLA, human leukocyte antigen
Posterior uveitis (133 cases, 28%) was the second common type for which toxoplasmosis (56 cases, 42.1%) was the most frequent cause followed by Behcet's disease (21 cases, 15.7%) and acute retinal necrosis syndrome (11 cases, 8.2%) (Table 4).
Table 4.
Etiologies of posterior uveitis
| Causes | Number (%) |
|---|---|
| Toxoplasmosis | 56 (42.1) |
| Behcet’s disease | 21 (15.7) |
| Serpiginous choroiditis | 5 (3.9) |
| Toxocariasis | 6 (4.7) |
| VKH disease | 8 (6) |
| APMPPE | 3 (2.2) |
| Acute retinal necrosis syndrome | 11 (8.2) |
| Cytomegalovirus retinitis | 5 (3.9) |
| Systemic lupus erythematosus | 5 (3.9) |
| MEWDS | 1 (0.7) |
| Birdshot retinochoroidopathy | 1 (0.7) |
| Eales disease | 3 (2.2) |
| Sarcoidosis | 2 (1.5) |
| Fungal retinitis | 1 (0.7) |
| Punctate inner choroidopathy | 1 (0.7) |
| HIV-associated uveitis | 1 (0.7) |
| Idiopathic | 3 (2.2) |
|
| |
| Total | 133 (100) |
VKH, Vogt-Koyanagi-Harada; APMPPE, acute placoid multifocal posterior pigment epitheliopathy; MEWDS, multiple evanescent white dot syndrome; HIV, human immunodeficiency virus
Panuveitis was next in frequency (99 cases, 20.8%,) for which Behcet's disease (34 cases, 34.3%) and idiopathic causes (25 cases, 25.2%) were the most common causes (Table 5).
Table 5.
Etiologies of panuveitis
| Cause | Number (%) |
|---|---|
| Behcet’s disease | 34 (34.3) |
| VKH disease | 17 (17.1) |
| Endogenous endophthalmitis | 11 (11.4) |
| Multifocal choroiditis and panuveitis | 3 (3) |
| Sympathetic ophthalmia | 3 (3) |
| Tuberculosis | 2 (2) |
| Leukemia (ALL- L1) | 2 (2) |
| Herpes zoster panuveitis | 1 (1) |
| HIV-Associated uveitis | 1 (1) |
| Idiopathic | 25 (25.2) |
|
| |
| Total | 99 (100) |
VKH, Vogt-Koyanagi-Harada; ALL, acute lymphoblastic leukemia; HIV, human immunodeficiency virus
Intermediate uveitis had the lowest incidence with 53 cases (11.1%); a great majority of these cases (92.4%) were idiopathic.
The overall frequency of idiopathic uveitis was 37.9% ranging from 3 cases (1.8%) in posterior uveitis to 103 cases (57.2%) in anterior uveitis (Table 6).
Table 6.
The frequency of idiopathic uveitis in different uveitis locations
| Site of inflammation | Number (%) |
|---|---|
| Anterior | 103 (57.2) |
| Intermediate | 49 (27.2) |
| Posterior | 3 (1.8) |
| Panuveitis | 25 (13.8) |
|
| |
| Total | 180 (100) |
DISCUSSION
The patterns and causes of uveitis often vary at different referral centers based on the demographics, geographical location and even referral level of the center, i.e., primary, secondary or tertiary. Having a uveitis registry in any region helps to detect its incidence and categorize more prevalent causes in that region and also to compare the results with records from other countries or other parts of the same country or region.
Causes of uveitis differ over time, such that tuberculosis and syphilis were the main causes of uveitis in the first half of the twentieth century but nowadays acquired immunodeficiency syndrome (AIDS) and cytomegalovirus (CMV) are responsible for more cases; actually they were uncommon before 1982.10
The most common presentation of uveitis in our series was blurred vision followed by eye discomfort and redness.
The proportion of male and female subjects was nearly equal in our study with a variable age at onset. Uveitis was more prevalent among male subjects in Northeast India and North India but was approximately equal in males and female subjects in North Africa.11-13
Mean patient age in our study was 30.5 (range, 5-56) years which is similar to other studies showing that uveitis frequently affects young adults.4,11,14,15
In our series anterior uveitis was the most common type of intraocular inflammation followed by posterior uveitis, panuveitis, and intermediate uveitis. This pattern is similar to the global distribution of uveitis.16 Most cases were unilateral and chronic; non-granulomatous conditions were more frequent than granulomatous ones and non-infectious etiologies were much more frequent than infectious causes. Idiopathic anterior uveitis (HLA-B27 negative) was the most common cause of anterior uveitis, which is similar to reports from the North and South of India,13,17 but different from a report from another tertiary eye center in Iran reporting that HLA-B27 associated iridocyclitis was less common and Behcet's disease, Fuchs' heterochromic iridocyclitis, Eales disease, and toxocariasis were more prevalent.4 Posterior uveitis, as compared to other studies, had a similar prevalence and was the second most common type of uveitis. We observed toxoplasmosis to be the most frequent cause of uveitis in this group.
In our study, similar to studies from North Africa and North India, panuveitis was more frequent than intermediate uveitis.11-13 Behcet's disease was the most frequent cause of panuveitis while most cases of intermediate uveitis were idiopathic.
Our patients had a specific diagnosis in 61.9% of cases. This frequency has varied from 47.1% to about 70% in different studies.11,14,18-20 The overall frequency of idiopathic uveitis has been 37.9% (range, 1.6-57.2%) which is similar to many studies on uveitis.11-16
The most common entities associated with uveitis were Behcet's disease, toxoplasmosis, Fuch's iridocylitis, and Vogt-Koyanagi-Harada (VKH) disease. The cause of uveitis displays racial and geographical differences. In the West, uveitis associated with ankylosing spondylitis, sarcoidosis, CMV retinitis, and toxoplasmosis are among the most common diagnoses.19-22
In the Middle East, toxoplasmosis, VKH,4 and acute anterior uveitis of undetermined origin7 were among the most common diagnoses. Infectious etiologies such as tuberculosis and toxoplasmosis are most common in reports from India.13,17,23,24
Two patients in our study had tuberculosis, an old man and one woman, both of whom were originally from Afghanistan temporarily residing in Iran with frequent trips to their home country.
In summary this study reports the pattern of uveitis in a large population of patients from Southern Iran, and may help complete the image of uveitis epidemiology in this region.
Acknowledgments
We would like to thank our colleagues at Poustchi Ophthalmic Research Center, Mrs. Fatemeh Ghorbani Zadeh and Mrs. Shiva Mostafavi for their assistance with the research proposal. This work was supported by a grant from Shiraz University of Medical Sciences, grant No: 88-01-01-1572.
Footnotes
Conflicts of Interest
None.
REFERENCES
- 1.Nussenblatt RB. The natural history of uveitis. Int Ophthalmol. 1990;14:303–308. doi: 10.1007/BF00163549. [DOI] [PubMed] [Google Scholar]
- 2.Rothova A, Suttorp-Van Schulten MS, Frits Treffers W, Kijlstra A. Causes and frequency of blindness in patients with intraocular inflammatory disease. Br J Ophthalmol. 1996;80:332–336. doi: 10.1136/bjo.80.4.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nashtaei EM, Soheilian M, Herbort CP, Yaseri M. Patterns of uveitis in the middle east and europe. J Ophthalmic Vis Res. 2011;6:233–240. [PMC free article] [PubMed] [Google Scholar]
- 4.Soheilian M, Heidari K, Yazdani S, Shahsavari M, Ahmadieh H, Dehghan M. Patterns of uveitis in a tertiary eye care center in Iran. Ocul Immunol Inflamm. 2004;12:297–310. doi: 10.1080/092739490500174. [DOI] [PubMed] [Google Scholar]
- 5.Al-Mezaine HS, Kangave D, Abu El-Asrar AM. Patterns of uveitis in patients admitted to a university hospital in Riyadh, Saudi Arabia. Ocul Immunol Inflamm. 2010;18:424–431. doi: 10.3109/09273948.2010.502284. [DOI] [PubMed] [Google Scholar]
- 6.Hamade IH, Elkum N, Tabbara KF. Causes of uveitis at a referral center in Saudi Arabia. Ocul Immunol Inflamm. 2009;17:11–16. doi: 10.1080/09273940802491850. [DOI] [PubMed] [Google Scholar]
- 7.Islam SM, Tabbara KF. Causes of uveitis at the eye center in Saudi Arabia: a retrospective review. Ophthalmic Epidemiol. 2002;9:239–249. doi: 10.1076/opep.9.4.239.1507. [DOI] [PubMed] [Google Scholar]
- 8.Harper SL, Chorich LJ, Foster CS. Diagnosis of uveitis. In: Foster CS, Vitale AT, editors. Diagnosis and treatment of uveitis. 1st ed. Philadelphia: W.B. Saunders; 2002. [Google Scholar]
- 9.Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–516. doi: 10.1016/j.ajo.2005.03.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oruc S, Kaplan AD, Galen M, Kaplan HJ. Uveitis referral pattern in a Midwest University Eye Center. Ocul Immunol Inflamm. 2003;11:287–298. doi: 10.1076/ocii.11.4.287.18270. [DOI] [PubMed] [Google Scholar]
- 11.Khairallah M, Yahia SB, Ladjimi A, Messaoud R, Zaouali S, Attia S, et al. Pattern of uveitis in a referral centre in Tunisia, north Africa. Eye (Lond) 2007;21:33–39. doi: 10.1038/sj.eye.6702111. [DOI] [PubMed] [Google Scholar]
- 12.Das D, Bhattacharjee H, Bhattacharyya PK, Jain L, Panicker MJ, Das K, et al. Pattern of uveitis in north east India: a tertiary eye care center study. Indian J Ophthalmol. 2009;57:144–146. doi: 10.4103/0301-4738.45506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh R, Gupta V, Gupta A. Pattern of uveitis in a referral eye clinic in north India. Indian J Ophthalmol. 2004;52:121–125. [PubMed] [Google Scholar]
- 14.Kazokoglu H, Onal S, Tugal-Tutkun I, Mirza E, Akova Y, Ozyazgan Y, et al. Demographic and clinical features of uveitis in tertiary centers in Turkey. Ophthalmic Epidemiol. 2008;15:285–293. doi: 10.1080/09286580802262821. [DOI] [PubMed] [Google Scholar]
- 15.Yang P, Zhang Z, Zhou H, Li B, Huang X, Gao Y, et al. Clinical patterns and characteristics of uveitis in a tertiary center for uveitis in China. Curr Eye Res. 2005;30:943–948. doi: 10.1080/02713680500263606. [DOI] [PubMed] [Google Scholar]
- 16.Chang JH, Wakefield D. Uveitis: a global perspective. Ocul Immunol Inflamm. 2002;10:263–279. doi: 10.1076/ocii.10.4.263.15592. [DOI] [PubMed] [Google Scholar]
- 17.Dandona L, Dandona R, John RK, McCarty CA, Rao GN. Population based assessment of uveitis in an urban population in southern India. Br J Ophthalmol. 2000;84:706–709. doi: 10.1136/bjo.84.7.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tran VT, Auer C, Guex-Crosier Y, Pittet N, Herbort CP. Epidemiological characteristics of uveitis in Switzerland. Int Ophthalmol 1994- 1995;18:293–298. doi: 10.1007/BF00917833. [DOI] [PubMed] [Google Scholar]
- 19.McCannel CA, Holland GN, Helm CJ, Cornell PJ, Winston JV, Rimmer TG. Causes of uveitis in the general practice of ophthalmology. UCLA Community-Based Uveitis Study Group. Am J Ophthalmol. 1996;121:35–46. doi: 10.1016/s0002-9394(14)70532-x. [DOI] [PubMed] [Google Scholar]
- 20.Rodriguez A, Calonge M, Pedroza-Seres M, Akova YA, Messmer EM, D’Amico DJ, et al. Referral patterns of uveitis in a tertiary eye care center. Arch Ophthalmol. 1996;114:593–599. doi: 10.1001/archopht.1996.01100130585016. [DOI] [PubMed] [Google Scholar]
- 21.Merrill PT, Kim J, Cox TA, Betor CC, McCallum RM, Jaffe GJ. Uveitis in the southeastern United States. Curr Eye Res. 1997;16:865–874. doi: 10.1076/ceyr.16.9.865.5048. [DOI] [PubMed] [Google Scholar]
- 22.Thean LH, Thompson J, Rosenthal AR. A uveitis register at the Leicester Royal Infirmary. Ophthalmic Epidemiol. 1996;3:151–158. doi: 10.3109/09286589609080121. [DOI] [PubMed] [Google Scholar]
- 23.Biswas J, Narain S, Das D, Genesh SK. Pattern of uveitis in a referral uveitis clinic in India. Int Ophthalmol 1996- 1997;20:223–228. doi: 10.1007/BF00175264. [DOI] [PubMed] [Google Scholar]
- 24.Mathur G, Biswas J. Systemic associations ofanterior uveitis in a tertiary care ophthalmic centrein south India. Int Ophthalmol. 2012;32:417–421. doi: 10.1007/s10792-012-9580-y. [DOI] [PubMed] [Google Scholar]