In 2011, an estimated 677,000 children were victims of abuse or neglect (U.S. Department of Health and Human Services, 2012). Nearly 18% of these victims were physically abused, with 81% of the perpetrators being the child’s parents (U.S. Department of Health and Human Services, 2012). Because only a small fraction of child maltreatment cases are ever reported to child protective services, general population estimates are much higher. According to the most recent National Incidence of Child Abuse and Neglect Study (NIS-4), an estimated 1.25 million children in the United Stated experienced maltreatment; over 25% of those children were physically abused (Sedlak et al., 2010). Yet much of the published literature has focused on children involved with the child welfare system, limiting our ability to understand factors that might lead to better prevention efforts. A growing body of research has contributed to understanding ways to reduce or prevent child maltreatment by identifying protective and risk factors. In particular, the relationship between child maltreatment and social connections (i.e., social networks and social support) has been examined. Social networks are considered an individual’s broad collection of social ties including family members, friends, coworkers, neighbors and other people in the community whereas social support refers specifically to the supportive resources (i.e. tangible support, emotional support, and social companionship) available through social networks (Barrera, 1986).
Conceptual Model
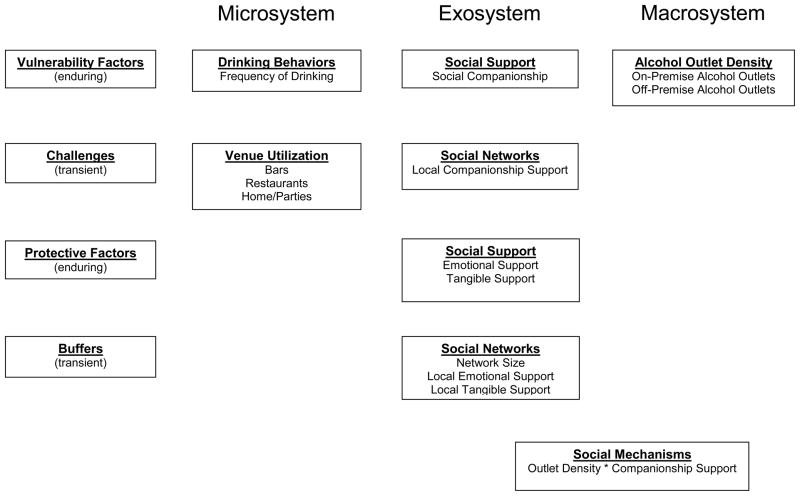
This study is situated in the ecological-transactional framework of child maltreatment (Cichetti & Lynch, 1993; Cichetti, Toth, & Mauchan, 2000). This model suggests that child maltreatment occurs as a result of a wide range of interactions that an individual has with neighbors, friends, family, and community institutions and vulnerability factors that include low income and substance misuse (Cichetti, Toth, & Mauchan, 2000). The ecological-transactional model specifies four systems levels with various vulnerability and protective factors associated with each of these systems. These factors are further delineated by the length of time they occur: transient or enduring. The systems of the ecological-transactional model are distinguished by their proximity to the individual being abused and include the octogenic system (individual developmental tasks that may contribute to further behaviors and psychological problems), microsystem (family environment), exosystem (formal and informal structures within the immediate environment for the family), and macrosystem (cultural values, beliefs, and institutions of larger communities). More specifically, this study tests a specific social mechanism described in a conceptual model by Freisthler and Holmes (2012) that details how alcohol outlet density, alcohol use, and social support may interact resulting in maltreatment. The piece of this model being tested can be found in Figure 1, along with the corresponding system levels from the ecological-transactional model. The particular aspects being studied primarily fall within the micro-, exo-, and macrosystems and are described in more detail below.
Figure 1.
Conceptual Model Showing Key Study Variables in the Ecological-Transactional Systems
Social Support, Support Networks, and Child Abuse
Limited access to supportive resources is a risk factor for child maltreatment (Coohey, 1995; Giovannoni & Billingsley, 1970; Oats, Davis, Ryan, & Stewart, 1979; Wolock & Magura, 1996). Parents who have fewer contacts with their social network members are more likely to maltreat their children (Coohey, 1995; Giovannoni & Billingsley, 1970; Polansky, Ammons, & Gaudin; 1985; Oats et al., 1979; Wolock & Magura, 1996). Child maltreatment is also more likely to occur when a parent lives further away from his or her social network members (Coohey, 2007; Giovannoni & Billingsley, 1970; Polansky et al., 1985) and perceives his or her network members to be less supportive (Coohey, 1996, 2000, 2007; Daniel, Hampton, & Newberger; 1983; Newberger, Hampton, Mark, & White; 1986; Ortega, 2002; Polansky et al., 1985; Turner & Avison, 1985). Social support and use of social networks fall within the exosystem of the ecological-transactional framework.
Studies have found that social support, primarily measured as tangible resources such as money or babysitting, can reduce child maltreatment (Coohey, 1995, 1996, 2000, DePanfilis, 1996; Ortega, 2002; Polansky et al., 1985; Thompson. 1985). However, parents may receive many different types of support not captured in previous research. One of these types of support, social companionship, also called belonging (Uchino, 2004), includes spending time with friends or family members doing leisure activities such as going to lunch or the movies (Cohen & Hoberman, 1983; DePanfilis, 1996). Although limited evidence suggests that lower levels of companionship are related to use of physical abuse (DePanfilis, 1996; Williamson, Borduin, & Howe, 1991), few studies have investigated this relationship among parents in relation to child maltreatment. When leisurely activities include consuming alcohol, social companionship support may actually prove detrimental for parents at risk for committing physical abuse.
Although the majority of the literature strongly emphasizes the positive influence of social support on the risk of child maltreatment, possible less desirable consequences of social support exist. For example, negative consequences of social support may be group conformity (Portes, 1998), where individuals feel pressured to adapt similar behavioral norms as their social network. Similarly, social support can produce positive and negative outcomes depending on the context of the interactions (Woolcock & Narayan, 2000). In the case of substance abuse, this may mean increased opportunities for binge drinking in a high risk group of drinkers.
Little is known about how negative social interactions impact parenting behaviors; however, the effect of social networks members engaging in risky behaviors among adolescents is informative. Adolescents whose peers engage in risky behavior are more likely to also engage in such behavior (Beal, Ausiello, & Perrin, 2001; Hawkins, Catalano, & Miller, 1992; He, Kramer, Houser, Chomitz, & Hacker, 2004; Kandel, 1973, 1978; Livaudais, Napoles-Springer, Stewart, & Kaplan, 2007; Romer & Hennessy, 2007). Thus, parents who receive social support resources in the form of social companionship (i.e., spending time with family or friends doing leisure activities) may also be engaging in risky behavior (e.g., heavy drinking) that result in problematic parenting.
Here social support is viewed as both an enduring vulnerability factor (e.g., social companionship) and an enduring protective factor (e.g., emotional and tangible) dependent on the type of support being provided. In addition, the effects of social networks are conceptualized to vary by characteristics such as the size and percentage of local social companionship support. For example, the percentage of local social companionship support could be a transient vulnerability factor as it increases the risk for child physical abuse, while the total size of a social network and percentage of emotional or tangible support could be transient buffers against this vulnerability. These are transient (vs. enduring) as support is dependent on individuals accessing support and having supportive individuals living in the neighborhood.
Parent Drinking, Drinking Venue Utilization, Alcohol Outlets, and Child Physical Abuse
Alcohol abuse and dependence have long been cited as vulnerability factors for child maltreatment, particularly physical abuse (Berger, 2005; Dube et al., 2001). Research has suggested that parents who are heavy drinkers or who abuse alcohol are more likely to physically assault their child than parents who were moderate drinkers or abstainers (Famularo, Kinscherff, & Fenton, 1992; Kelleher, Chaffin, Hollenberg, & Fischer, 1994; Murphy, Jellinek, Quinn, & Smith, 1991). However, much of the research relating alcohol use to child maltreatment has been conducted on groups that cannot be generalized to the larger population (Testa & Smith, 2009). Specifically, these studies include parents already involved with the child welfare system or in treatment for substance abuse, both specialized groups of people that represent only a portion of the total populations (Testa & Smith, 2009). The current study assesses drinking behaviors in a general population sample of parents to reduce problems associated with previous studies of non-representative populations.
More recently, the role of where parents drink and its effect on parenting behaviors has been identified as one risk factor related to the use of physical abuse (Freisthler, 2011; Freisthler & Gruenewald, 2013). Freisthler and Gruenewald (2013) found that parents who had drink more frequently at bars and at home or parties used physical abuse significantly more often. Given that social companionship support takes into account the support for spending time on recreational activities, this study goes beyond categorizing drinking behavior as simply a single variable (quantity*frequency) and includes measures of frequency of drinking at several venues (bars, restaurants, homes/parties) and the continued volume (i.e., quantity) of drinking at those locations. Both constructs fall within the microsystem with frequency of drinking as a vulnerability factor and dose-response as a challenge.
Alcohol availability, as measured by alcohol outlet density in the macrosystem, has also been related to rates of child maltreatment. Areas with greater density of bars have higher substantiated reports of child maltreatment (Freisthler, 2004; Freisthler, Midanik, & Gruenewald, 2004) and increases in foster care entries over time (Freisthler, Gruenewald, Remer, Lery, & Needell, 2007). Yet, all of these studies were at the ecological level and did not include individual-level covariates. Thus, although they could make gross generalizations about the relationship between outlets and child maltreatment, they could not identify the specific mechanisms by which outlets may be affecting maltreating behaviors. In a study of parents, Freisthler and Gruenewald (2013) found that having more bars in the immediate vicinity (within a half mile) was related to more frequent use of physical abuse among drinkers, controlling for a variety of individual and psychosocial characteristics including drinking locations.
Relationship between Alcohol Outlets, Parent Drinking, and Social Support
The proximity of social network members (i.e., live within the respondent’s neighborhood) may affect participation in leisure activities, drinking behaviors and ultimately child physical abuse. Warde, Tampubolon, and Savage (2005) found that having more people in your social network increased the likelihood of participating in various recreational activities, such as going out for a meal or drink with another individual. Thus, if drinking occurs during these activities, parenting decisions and behaviors may be affected through the disinhibiting qualities of alcohol (Pihl, Lau, & Assaad, 1997; Pihl, Peterson, & Lau, 1993). In this context, interactions with social network members may not act as a protective factor against child maltreatment. Instead, having opportunities to socialize with friends and families outside of the home in environments that may promote risky drinking may ultimately affect the judgment of the parent when he or she returns home (Freisthler & Holmes, 2012). These socialization opportunities may in fact increase use of physical abuse if other members of those social networks indicate that use of these similar types of physical punishment or do not sanction the offending parent when he or she remarks about using it (Emery, Nguyen, & Kim, 2013).
These relationships may be exacerbated in neighborhood areas that provide more opportunities for parents to socialize, such as in bars and/or restaurants that sell alcohol. Bar density has also been related to higher rates of violence, both cross-sectionally (Gruenewald Freisthler, Remer, LaScala, & Treno, 2006; Lipton and Gruenewald, 2002) and over time (Gruenewald & Remer, 2006). At the individual level, drinking at bars is related to higher levels of alcohol-related aggression (Treno, Gruenewald, Remer, Johnson, & LaScala, 2008). These contexts provide opportunities for parents to spend recreational time with other adults in places where children are generally not allowed. At the city-level, having greater densities of on-premise alcohol outlets (i.e., establishments where alcohol is sold and consumed at that location) may be indicative of having a more active “night life” and provide more opportunities for parents to socialize in these contexts. Having a higher percentage of support network members who live in a neighborhood with a higher density of alcohol outlets may further heighten aggressive parenting.
Research Question and Hypotheses
Several limitations have been identified in the literature presented, including the general lack of inclusion of social companionship support in studying physical abuse, use of biased samples to study alcohol use behaviors, and the ecological nature of most alcohol outlet density studies. In order to address limitations in previous research, the current study examines whether parental drinking behavior, drinking locations, alcohol outlet density, and types of social support are related to the risk of child physical abuse in a general population sample. Thus, we combine the macrosystem, exosystem, and microsystem variables in one study. It is hypothesized that parents who consume alcohol frequently will be more likely to physically abuse their children than parents who consume alcohol infrequently or abstain from alcohol use. This study also examines whether the percentage of perceived social companionship that lives locally (within the respondent’s neighborhood) is related to the risk of physical abuse while controlling for parental drinking behavior, and whether this relationship is moderated by alcohol outlet density. It is hypothesized that perceived social companionship support, percentage of social network that is local, and the interaction between percent local social companionship support and on-premise alcohol outlet density will be positively related to the risk of child physical abuse net parental drinking behavior.
Method
Study Design and Sample Characteristics
Data from 3,023 respondents were obtained through a telephone survey. Approximately 60 respondents per city (with a low of 47 respondents and a high of 74 respondents) from 50 mid-sized cities in California were sampled using stratified random sampling procedures from listed samples. Potential respondents were identified via listed samples of telephone numbers obtained from a third party vendor who has access to these data from sources that include credit bureaus, credit card companies, and other companies that maintain lists. These lists are supplemented with any samples identified as households with a child under the age of twelve. These listed samples were then de-duplicated against each other before being loaded into a computer assisted telephone interview (CATI) system, which then randomized the order in which they were called. Listed sampling allows for a more target sampling effort within geographic areas, such as are needed here, than traditional random digit dialing (RDD) techniques (Gruenewald, Remer, & LaScala, 2014). Listed samples are relatively unbiased when compared to RDD (Brick, Waksber, Kulp, & Starer, 1995; Kempf & Remington, 2007; Tucker, Lepkowski, & Piekarski, 2002).
Individuals on these lists were sent a preannouncement letter with information about the study. Respondents had to be a parent or guardian of a child 12 years of age or younger living with them at least 50% of the time. The survey took approximately 30 minutes to complete and was given using CATI procedures. The use of telephone survey methodology allowed for the identification and recruitment of a general population sample, minimizing biases introduced when using a sample of individuals already involved with the child welfare system or those in treatment for substance abuse problems (Testa & Smith, 2009).
Interviewers obtained verbal informed consent for each of the participants due to the nature of the survey administration (i.e., conducted over the telephone) and to maintain anonymity of survey participants. Participants were mailed a $25 check for participation to an address they specified. The 50 cities were chosen to maximize ecological validity from all 138 cities in California with population sizes between 50,000 and 500,000 (Thompson, 1992). The original list of 138 cities was randomized. The first city in the list (the “seed” city) was included in the sample. The next city on the list in random number order was then selected if it was at least two cities and greater than one mile away from the seed city. This procedure was followed until the sample of 50 cities was achieved. Thus no city included in the study is geographically next to any other city in the sample. This procedure assured us geographic coverage across the state, important for the overall study aims (Lipperman-Kreda, Grube, & Friend, 2012).
To reduce non-response bias, each phone number received 10 call attempts at different days and times if a live person was not reached (e.g., busy signal or voice mail). Two refusal conversion attempts were made with enumerated households (i.e., households identified with a child 12 year or younger in the household) to improve response rates. Poststratification survey weights based on race/ethnicity, gender, and household type (single- vs. two-parent households) were constructed to increase generalizability to all 138 cities of this size in California. The response rate was calculated using standard definitions from the American Association for Public Opinion Research (AAPOR). AAPOR response rates divide the number of completed interviews by the sum of the number of completed interviews, the number of refusals, the number of non-contacts, and a proportion of cases with unknown eligibility. Unknown eligibility was assessed as the ratio of the number of completed and eligible non-interviews to the number of completed and eligible non-interviews plus the number of known non-eligible respondents (AAPOR, 2002). Potential respondents who did not speak English or Spanish were counted as not eligible, as the sampling frame included all English or Spanish speaking parents of children 0 to 12 years. Using this methodology, the response rate for this survey was 47.4%.
Dependent Variable
Child physical abuse was measured using the severe physical assault items from the Conflict Tactics Scale, Parent-Child Version (CTSPC; Straus, Hamby, Finkelhor, Moore, & Runyan, 1998). This scale consists of four items for children over 2 years of age and five items for children under 2 years and includes questions about severe physical abuse (e.g., slapping the child on the face, head, or ears, and throwing or knocking the child down). An additional item for shaking a child is included for children under 2 years. Respondents answered via categories about number of times these behaviors occurred in the past year (ranging from Never to More than 10 times). The internal consistency for this scale is similar to other general population studies (α = .51) and has shown both construct and discriminant validity by Straus and colleagues (1998). Respondents were instructed to answer the question about parenting behaviors for the child who had the most recent birthday, called the “focal child”.
As these items were sensitive in nature and could reflect a parent’s willingness to report abusive behavior, several strategies were employed to minimize socially desirable responses. Items related to child physical abuse were asked via interactive voice response technology (IVR) and encrypted in the data corresponding to the participant. IVR is a survey administration methodology that allows a survey participant to respond to a question from a computerized voice menu in order to increase disclosure of sensitive subjects (Midanik & Greenfield, 2006). The survey interviewers and the survey programmer had no direct access to information on abuse or neglectful behaviors and the research personnel did not have identifying information on who committed abusive and neglectful acts. This provided respondents with a greater level of security with regards to answering sensitive questions, and exempted survey and research staff from having to report respondents to Child Protective Services. Items from the CTSPC were interspersed in the order recommended by Straus et al. (1998) such that an abusive behavior was followed by a non-violent strategy. The scale was made up of multiple items, allowing for a more complete measure of child physical abuse. The scale was scored using the midpoint of the response category for each item and then summed. Table 1 provides descriptive statistics.
Table 1.
Descriptive Statistics for Full Sample (n = 3023) and Drinkers Only (n = 2152)
| Variable Name | Full Sample | Drinkers Only | ||
|---|---|---|---|---|
| Weighted % or x̄ (sd) | Sample n | Weighted % or x̄ (sd) | Sample n | |
| Average Frequency of Physical Abuse | 0.33 (1.98) | 2770 | 0.34 (2.02) | 2003 |
| Alcohol Use Categories | ||||
| Lifetime Abstainer | 9.3 | 292 | -- | -- |
| Ex-Drinker | 19.2 | 564 | -- | -- |
| Light Drinker | 41.9 | 1357 | -- | -- |
| Moderate Drinker | 18.4 | 517 | -- | -- |
| Infrequent Heavy Drinker | 4.0 | 101 | -- | -- |
| Occasional Heavy Drinker | 4.4 | 106 | -- | -- |
| Frequent Heavy Drinker | 2.7 | 71 | -- | -- |
| Frequency of drinking context utilization | ||||
| Home/Parties | -- | -- | 3.71 (6.0) | 2147 |
| Bar | -- | -- | 0.21 (0.9) | 2150 |
| Restaurants | -- | -- | 0.51 (1.5) | 2147 |
| Dose-Response for drinking contexts | ||||
| Home/Parties | -- | -- | 3.81 (14.5) | 2135 |
| Bar | -- | -- | 0.40 (3.7) | 2144 |
| Restaurants | -- | -- | 0.44 (1.9) | 2140 |
| Gender (Focal Child) | ||||
| Male | 50.4 | 1495 | 52.3 | 1101 |
| Female | 49.6 | 1414 | 47.7 | 991 |
| Age, in years (Focal Child) | 6.68 (3.6) | 2914 | 6.75 (3.6) | 2085 |
| Age, in years | 39.43 (8.4) | 3023 | 39.97 (8.2) | 2152 |
| Gender (n = 3023) | ||||
| Female | 52.1 | 1973 | 49.5 | 1354 |
| Male | 47.9 | 1050 | 50.5 | 798 |
| Number of children | 2.19 (0.9) | 3023 | 2.16 (0.9) | 2152 |
| Marital Status | ||||
| Single, Divorced, Widowed | 23.3 | 350 | 23.0 | 249 |
| Married or Cohabiting | 76.7 | 2673 | 77.0 | 1914 |
| Race/Ethnicity (n = 3009) | ||||
| Non-Hispanic White | 50.5 | 1753 | 54.8 | 1386 |
| Non-Hispanic Black | 5.0 | 111 | 4.6 | 67 |
| Hispanic | 29.4 | 733 | 26.4 | 439 |
| Asian | 10.0 | 236 | 9.1 | 139 |
| Multi-Racial | 2.5 | 92 | 2.7 | 72 |
| Other | 2.6 | 84 | 2.4 | 54 |
| Income | ||||
| ≤ $20,000 | 10.9 | 258 | 6.8 | 123 |
| $20,001 – $40,000 | 15.0 | 358 | 13.4 | 211 |
| $40,001 – $60,000 | 14.2 | 373 | 14.3 | 262 |
| $60,001 – $80,000 | 14.3 | 450 | 14.3 | 316 |
| $80,001 – $100,000 | 12.9 | 412 | 13.4 | 309 |
| $100,001 – $150,000 | 19.4 | 648 | 22.3 | 532 |
| $150,001 + | 13.3 | 409 | 15.5 | 344 |
| Parenting Stress | 3.93 (1.3) | 2984 | 4.01 (1.3) | 2128 |
| Impulsivity Level | 0.78 (1.3) | 2975 | 0.72 (1.3) | 2128 |
| Symptoms of Depression | ||||
| Yes | 19.1 | 504 | 18.0 | 334 |
| No | 80.9 | 2480 | 82.0 | 1808 |
| Symptoms of Anxiety | ||||
| Yes | 47.4 | 1401 | 47.0 | 995 |
| No | 52.6 | 1605 | 53.0 | 1156 |
| Social Support | ||||
| Tangible | 14.41 (2.1) | 2995 | 14.48 (2.0) | 2138 |
| Emotional | 14.73 (2.0) | 2995 | 14.85 (1.9) | 2136 |
| Social Companionship | 14.07 (2.1) | 2995 | 14.13 (2.1) | 2140 |
| Average Size of Social Network | 10.82 (10.5) | 2971 | 10.71 (9.5) | 2136 |
| Proportion of Local Social Support | ||||
| Tangible | 0.33 (0.3) | 2945 | 0.31 (0.3) | 2122 |
| Emotional | 0.29 (0.3) | 2961 | 0.27 (0.3) | 2128 |
| Social Companionship | 0.38 (0.4) | 2884 | 0.36 (0.4) | 2080 |
| City-Level Alcohol Environment | ||||
| Density of Off-premise outlets (per area) | 4.05 (3.1) | 50 | 4.05 (3.1) | 50 |
| Density of On-premise outlets(per area) | 6.41 (4.4) | 50 | 6.41 (4.4) | 50 |
Independent Variables
Alcohol drinking
Respondents were asked about how often they drank alcohol and given twelve response categories ranging from every day to never had a drink of alcohol in my life. In a separate set of questions, they were also asked the frequencies with which they had 1 or more, 2 or more, 3 or more, 6 or more, and 9 or more drinks in the past four weeks. For those who report not drinking in the past four weeks, they are asked the same questions over the past year (allowing the method to be extended to low frequency drinking). Respondents were also asked the maximum number of drinks they consumed on any occasion during the same time frame, monthly or yearly, on which their self-reports were based. A “drink” was defined for the respondents as a 12-ounce can of beer, a 5-ounce glass of wine, or a 1-ounce shot of liquor. Use of specific drinking contexts was measured in terms of the frequency during the prior 28 or 365 days when respondents reported attending these places where drinking occurred. Respondents self-reported the number of times they drank a) at home, b) in bars, c) in restaurants, and d) at parties outside of the home. The 365 day measures were scaled to a 28-day metric. The answers to these series of questions allow us to create two different drinking typologies: categories of alcohol use, including abstaining; and context-specific dose-response models to determine if drinking in higher quantities results in more use of physical abuse towards the focal child.
Alcohol Use Categories
Responses from the questions above were recoded into seven categories : a) lifetime abstainers (never drank alcohol), b) ex-drinkers (did not drink alcohol in past year, but drank alcohol during his/her lifetime), c) light drinkers (drank either in the past month or past year but never more than 1–2 drinks per occasion), d) moderate drinkers (drank 3–4 drinks at least once during past month but never drank more than 4 drinks), e) infrequent heavy drinkers (drank 5 or more drinks once a month or less), f) occasional heavy drinkers (drank 5 or more drinks 2–3 days a month or 1–2 days per week), and g) frequent heavy drinkers (drank 5 or more drinks 3–5 days per week or daily). These categories have been used in previous work examining intimate partner violence and depression (Kaufman, Kantor, & Straus, 1987; Lipton, 1994; Paschall, Freisthler, & Lipton, 2005). About 41% of respondents report engaging in light drinking behaviors while about 29% report drinking moderately or heavily on at least one occasion.
Context-Specific Dose Response Drinking Models
Drinking patterns were measured using a graduated frequency approach derived from the above questions that provides model-based estimates of dimensions of drinking patterns using a mathematical model described in Freisthler and Gruenewald (2013), with a brief description below. Model based estimates represent average levels of risk associated with drinking at specific contexts and are independent of effects related to drinking quantities. In other words, drinking context variables provide information about the risk of using child physical abuse based on the number of times a respondent had at least one drink at a specific location. Using minimal data, model based estimates also provide effects related to variations in drinking quantities at each of those locations. Thus, the second set of variables in these context-specific dose-response models shows how use of child physical abuse is related to each additional drink (more than one) of alcohol.
Alcohol Outlet Density
Data on alcohol outlets was obtained from the California Department of Alcoholic Beverage Control for 2009. Outlet locations were geocoded to the street address of the establishment. Numbers of active alcohol outlets by city were calculated for off-premise alcohol establishments (license type 20 Off-Sale Beer & Wine or 21 Off-Sale General) and on-premise alcohol outlets (license type 23 Small Beer Manufacturing, 40 On-sale beer, 42 Beer/Wine Public Premise, 48 General Public Premise, 61 Beer public premises, 75 General Brew-Pub, 41 Beer/Wine Eating Place, or 47 General Eating Place). Geocoding rates of these data exceeded 99%. Density measures were created by summing the number of each type of outlet and dividing by the number of square miles for the city.
Social Support
Three types of social support were measured using the Interpersonal Support Evaluation List (ISEL) short form (Cohen, Mermelstein, Kamarck, & Hoberman, 1985) which asks four questions for each: emotional support, tangible support, and belongingness (or social companionship support). Responses included Definitely False, Probably False, Probably True, and True on items such as “If I were sick, I could easily find someone to help with my daily chores” and “I don’t often get invited to do things with others.” Items were reverse coded when necessary and summed. Reliability was assessed using Cronbach’s alpha for each subscale: social companionship support α = .67, emotional support α = .68, and tangible support α = .63.
Attributes of Social Networks
For each social support subscale, respondents were asked to provide the number of members in their social network who provided that type of support. Given that respondents were not asked for unique network members, the number of network members for all three types of support was averaged to get the relative size of social networks. This question was then followed by the number of those individuals who lived within the same neighborhood as the respondent. A percentage of local support was calculated for each subtype of social support (e.g., percentage of emotional support givers who are local). Thus the average size of respondent’s social networks provides information on how many people can provide social support while the percentage of local support represents how many network members who provide each of the three types of social support live locally.
Psychosocial risk factors
Individual level risk factors such as depressive symptoms (Chaffin, Kelleher, & Hollenberg, 1996), anxiety (Lahey, Conger, Atkeson, &Treiber, 1984; Whipple & Webster-Stratton, 1991; Freisthler & Gruenewald, 2013), impulsivity (Rohrbeck & Twentyman, 1986; Freisthler & Gruenewald, 2013), and parenting stress (Chan, 1994; Whipple & Webster-Stratton, 1991) have been related to child physical abuse and were included in study models.
Depression and Anxiety
Past month depression and anxiety were measured using the Primary Care Evaluation of Mental Disorders (PRIME-MD) tool (Kroenke Spitzer, & Williams, 2003; Kroenke Spitzer, Williams, Monahan, & Lowe 2007). Two items assessed depression: a) having been bothered a lot by little interest or pleasure in doing things and b) having been bothered a lot by feeling down, depressed, or hopeless. A positive response to either item was recoded as having symptoms for depression. Anxiety was measured with three items: a) having been bothered a lot by “nerves,” or feeling anxious or on edge, b) having been bothered a lot by worrying about a lot of different things, or c) having had an anxiety attack (suddenly feeling fear or panic). As with depression, a positive response for any item was coded as having symptoms for anxiety. Internal consistency was .65 for depression and .61 for anxiety.
Impulsivity
Impulsivity was measured using a modified version of Dickman’s Dysfunctional Impulsivity Scales (Dickman, 1990). Dysfunctional impulsivity refers to acting rapidly and inaccurately (e.g., I often get into trouble because I don’t think before I act) and was measured by 7 items. Yes/no responses were summed with higher values on the scale indicating higher levels of impulsivity. Internal consistency for this version of the scale was .73.
Parenting Stress
Two items measured parenting stress: a) I got very angry when this child misbehaved, and b) I felt stressed out by this child’s misbehavior from the Dimensions of Discipline Inventory (Straus & Fauchier, 2007). Responses were never, sometimes, often, and always. Items were summed and internal consistency measured using Cronbach’s alpha (α = 0.65).
Sociodemographic Controls
The age and gender of the focal child were included as control variables. Control variables also included the age, gender, race/ethnicity, and marital status, income and number of children for the respondents. In the models, marital status is coded as married or cohabiting (compared to single, divorced, or widowed); race/ethnicity includes Asian, African American, Hispanic/Latino, Multi-racial and Other race/ethnicities, with Caucasian as the comparison group; and income had seven categories (see Table 1).
Data Analysis
Data were analyzed using multilevel Poisson models as respondents (Level 1) were nested within cities (Level 2) due to the design of the study. This nesting implies non-independence among respondents within cities, that is, respondents from the same city are expected to be more similar to each other than they are to respondents from other cities. At the highest level of analysis (Level 2, city level), measures of community-level variables (i.e., outlet density variables) were included as city-level random effects. At the lowest level of analysis (Level 1, individual), the dependent measures were predicted from background characteristics of respondents (sociodemographics), psychosocial characteristics (impulsivity) and drinking levels (abstainer, moderate drinker). The general form of the multilevel model used was:
Level 1:
| (1) |
In Equation 1, Y was the outcome measure of interest (e.g., frequency of child physical abuse), measured at the person level, b0 is the city-specific intercept, b1-p are regression coefficients expressing the associations (slopes) between p person-level predictors (X1-p; e.g., age) and the outcome, and e is the individual-specific residual or error.
Level 2:
| (2) |
Equation 2 g00 shows the overall sample intercept for the equation predicting city-specific intercepts and u0 is the random city-specific residual component. In multilevel regression, the b0 can be thought of as representing adjusted city-level means on the outcome variable. Because the outcome variables used in these models was discrete (counts; e.g., frequency of physical abuse), non-linear multilevel (Poisson) regression techniques under the HGLM module of the HLM Version 7 software (Raudenbush, Bryk, Cheong, & Congdon, 2006) was used. Results for the population average model are presented.
Missing data
Missing data on most variables was negligible at less than four percent. Due to the sensitive nature of the physical abuse items and the likely concerns about reporting, about nine percent of cases had missing data on this variable. In order to assess the effects of the missing data on the final analysis, a two-stage procedure that tested and corrected for effects related to biases associated with sample selection was completed (Greene, 1993, 2002; Heckman, 1979). Respondents who had missing data for the items asking about physically abusive behaviors were significantly more likely to be Hispanic (b = 0.27, p < .001), Asian (b = 0.26, p = .026), and have more children (b = 0.08, p = .024) and less likely to be married (b = −0.20, p = 0.014). In the second stage of this procedure, the Inverse Mill’s ratio (IMR) was created from the results of the probit model and used as a covariate in the full model assessing the relationship of alcohol use to child physical abuse. The IMR was not statistically significantly related to child physical abuse in the final model (b = 3.18, p = .481), thus selection bias was not a problem in the final model presented here. Cases with missing data were dropped from the analyses.
Results
Bivariate t-tests between drinkers and non-drinkers were conducted for the social support and social network variables. Drinkers reported significantly higher levels of tangible support, t(2995) = 3.05, p = .002), emotional support, t(2990) = 4.81, p < .001), and social companionship support, t(2996) = 2.31, p = .021) when compared to non-drinkers. Drinkers reported significantly lower percentages of local network members providing tangible support, t(2943) = −4.40, p < .001), emotional support, t(2959) = −4.89, p < .001), and social companionship support t(2871) = −4.91, p < .001) than non-drinkers. There was no difference between drinkers and non-drinkers on average size of social network, t(2968) = −.98, p < .33).
Results for the multilevel model of the full sample using drinking categories (including abstainers) can be found in Table 2 and for the context-specific dose-response models for drinkers only can be found in Table 3. In each table, the results for two different models are provided. Model 1 contains direct effects for both outlet density variables (at Level 2) and the whole complement of individual level variables (at Level 1). The second model in each table includes cross-level interactions for the relationship of social companionship with both outlet density variables.
Table 2.
Multilevel Poisson Model for Alcohol Use, Types of Social Support, and Frequency of Physical Abuse (n = 2371)
| Variable Name | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | |
| Intercept | −1.821 | 0.627 | ** | −1.922 | 0.622 | ** |
| Level 2: City-level Alcohol Environment | ||||||
| Off-premise per square mile | −0.192 | 0.066 | ** | −0.121 | 0.073 | |
| On-premise per square mile | 0.108 | 0.040 | ** | 0.029 | 0.042 | |
| Level 1: Individual Characteristics | ||||||
| Male (Focal Child) | 0.264 | 0.094 | ** | 0.173 | 0.094 | ** |
| Age, in years (Focal Child) | 0.067 | 0.016 | *** | 0.069 | 0.015 | *** |
| Male | 0.328 | 0.104 | ** | 0.337 | 0.105 | ** |
| Age, in years | −0.008 | 0.008 | −0.009 | 0.008 | ||
| Number of Children | 0.082 | 0.049 | 0.105 | 0.048 | * | |
| Married or Cohabitating | −0.312 | 0.136 | * | −0.232 | 0.137 | |
| Race/Ethnicity (reference: white) | ||||||
| Asian American | 0.837 | 0.171 | *** | 0.858 | 0.173 | *** |
| African American | 0.714 | 0.198 | *** | 0.769 | 0.196 | *** |
| Hispanic | 0.007 | 0.127 | 0.023 | 0.125 | ||
| Multi-racial | −0.447 | 0.310 | −0.368 | 0.310 | ||
| Other race | 0.493 | 0.243 | * | 0.678 | 0.238 | ** |
| Income | −0.104 | 0.031 | ** | −0.121 | 0.031 | *** |
| Depressive Symptoms | 0.367 | 0.126 | ** | 0.430 | 0.124 | ** |
| Anxiety Symptoms | −0.308 | 0.103 | ** | −0.295 | 0.102 | ** |
| Impulsivity | 0.156 | 0.027 | *** | 0.139 | 0.027 | *** |
| Parenting Stress | 0.268 | 0.033 | *** | 0.287 | 0.033 | *** |
| Alcohol Use Levels (reference: lifetime abstainer) | ||||||
| Ex-Drinker | 0.774 | 0.348 | * | 0.840 | 0.344 | * |
| Light Drinker | 1.116 | 0.334 | ** | 1.113 | 0.331 | ** |
| Moderate Drinker | 1.085 | 0.357 | ** | 1.119 | 0.352 | ** |
| Infrequent Heavy Drinker | 0.793 | 0.420 | 0.795 | 0.411 | ||
| Occasional Heavy Drinker | 0.913 | 0.402 | * | 0.954 | 0.396 | * |
| Frequent Heavy Drinker | 0.996 | 0.412 | * | 0.946 | 0.411 | * |
| Types of Social Support | ||||||
| Tangible | −0.106 | 0.026 | *** | −0.107 | 0.026 | *** |
| Emotional | −0.086 | 0.029 | ** | −0.104 | 0.029 | *** |
| Social Companionship | 0.077 | 0.030 | ** | 0.096 | 0.216 | ** |
| Average Network Size | 0.006 | 0.004 | 0.005 | 0.004 | ||
| Percentage of Local Support by Type | ||||||
| Tangible | −0.029 | 0.214 | 0.106 | 0.216 | ||
| Emotional | −0.331 | 0.204 | −0.482 | 0.208 | * | |
| Social Companionship | 0.415 | 0.153 | ** | 0.186 | 0.167 | |
| Companionship * Off-premise | −0.198 | 0.099 | * | |||
| Companionship * On-premise | 0.187 | 0.035 | *** | |||
| Variance Component (τ) | 0.785 | 0.179 | *** | 0.781 | 0.178 | *** |
p < .001,
p < .01,
p < .05
Table 3.
Multilevel Poisson Model of Dose-Response Drinking, Types of Social Support, and Child Physical Abuse (n = 1764)
| Variable Name | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | |
| Intercept | −1.141 | 0.625 | −1.054 | 0.605 | ||
| Level 2: City-level Alcohol Environment | ||||||
| Off-premise per square mile | −0.115 | 0.082 | 0.033 | 0.088 | ||
| On-premise per square mile | 0.074 | 0.048 | −0.087 | 0.052 | ||
| Level 1: Individual Characteristics | ||||||
| Male (Focal Child) | 0.512 | 0.108 | *** | 0.662 | 0.109 | *** |
| Age, in years (Focal Child) | 0.105 | 0.018 | *** | 0.112 | 0.018 | *** |
| Male | 0.566 | 0.109 | *** | 0.606 | 0.109 | *** |
| Age, in years | 0.0002 | 0.009 | −0.002 | 0.008 | ||
| Number of Children | −0.070 | 0.060 | −0.044 | 0.059 | ||
| Married or Cohabitating | −0.363 | 0.147 | * | −0.177 | 0.149 | |
| Race/Ethnicity (reference: white) | ||||||
| Asian American | 1.059 | 0.201 | *** | 1.036 | 0.207 | *** |
| African American | 0.734 | 0.246 | ** | 0.768 | 0.250 | ** |
| Hispanic | 0.118 | 0.140 | 0.100 | 0.139 | ||
| Multi-racial | −0.639 | 0.365 | −0.383 | 0.348 | ||
| Other race | 0.467 | 0.316 | 0.616 | 0.302 | * | |
| Income | −0.138 | 0.036 | *** | −0.151 | 0.035 | *** |
| Depressive Symptoms | 0.186 | 0.150 | 0.254 | 0.146 | ||
| Anxiety Symptoms | −0.329 | 0.118 | ** | −0.300 | 0.114 | ** |
| Impulsivity | 0.249 | 0.031 | *** | 0.209 | 0.032 | *** |
| Parenting Stress | 0.264 | 0.037 | *** | 0.303 | 0.037 | *** |
| Frequency of Context Utilization | ||||||
| Bars | 0.410 | 0.057 | *** | 0.578 | 0.068 | *** |
| Restaurants | 0.070 | 0.031 | * | 0.084 | 0.028 | ** |
| Home and parties | 0.041 | 0.008 | *** | 0.042 | 0.008 | *** |
| Dose-response for Drinking Contexts | ||||||
| Bars | −0.097 | 0.027 | *** | −0.135 | 0.037 | *** |
| Restaurants | −0.037 | 0.032 | −0.046 | 0.031 | ||
| Home and Parties | 0.002 | 0.004 | 0.002 | 0.004 | ||
| Types of Social Support | ||||||
| Tangible | −0.177 | 0.029 | *** | −0.197 | 0.028 | *** |
| Emotional | −0.084 | 0.035 | * | −0.124 | 0.034 | *** |
| Social Companionship | 0.125 | 0.035 | *** | 0.156 | 0.035 | *** |
| Average Network Size | 0.001 | 0.006 | −0.004 | 0.006 | ||
| Percentage of Local Support by Type | ||||||
| Tangible | −0.161 | 0.246 | 0.087 | 0.251 | ||
| Emotional | −0.070 | 0.234 | −0.230 | 0.246 | ||
| Social Companionship | 0.191 | 0.175 | −0.300 | 0.196 | ||
| Companionship * Off-premise | −0.328 | 0.129 | * | |||
| Companionship * On-premise | 0.316 | 0.045 | *** | |||
| Variance Component (τ) | 1.147 | 0.262 | *** | 1.161 | 0.265 | *** |
p < .001,
p < .01,
p < .05
Models for Drinking Categories
Table 2 presents the results for the analysis of drinking categories, social support, social network attributes, and alcohol outlet density on child physical abuse. Compared to lifetime abstainers, all levels of alcohol use (except infrequent heavy drinkers) used physical abuse significantly more often. Respondents with more tangible and emotional support used physical abuse less often, while those with higher levels of social companionship support used physical abuse more often. Having a higher percentage of local network members who provided social companionship was positively related to frequent use of physical abuse. Alcohol outlet density was directly related to child physical abuse in Model 1, but in Model 2, on-premise outlet density was indirectly positively related through social companionship while off-premise outlet density was indirectly negatively related through social companionship. The percentages of local tangible and emotional support were not related to use of child physical abuse.
Parents reporting depressive symptoms, higher levels of impulsivity, and parenting stress used physical abuse significantly more often. Respondents who were male, Asian, African American, of “Other” race/ethnicity with more children used physical abuse more often, while having a younger focal child, reporting fewer symptoms of anxiety and having higher income was negatively related to use of physical abuse.
Models for Context-Specific Dose-Response Models
The results for the context-specific dose-response models for drinkers can be found in Table 3. Parents who drink more frequently at bars, restaurants and homes/parties used physical abuse more often. Each additional drink at bars is related to less use of physical abuse, indicating that a dose-response relationship is not present. Additional drinks (above the first drink) were not related to physical abuse when drinking at restaurants or homes/parties. Similar to the results from all respondents, tangible and emotional support were negatively related to number of times using physical abuse while social companionship had a positive relationship. No direct relationship between alcohol outlet densities and child physical abuse was found, but density of both on-premise and off-premise outlets were moderated by percentage of local social companionship support.
Physical abuse was higher for older male focal children and male, African American, Asian, and Other race/ethnicity respondents. Impulsive parents with high levels of parenting stress, and who report depressive symptoms use physical abuse more often. Respondents who were report fewer symptoms of anxiety and had higher incomes report using less physically abusive parenting practices.
Discussion
This study is one of the first to examine how type of social support, percentage of local social network members, drinking behaviors, and alcohol outlet density may place children at greater risk for physical abuse. Consistent with the ecological-transactional framework, our major findings suggest that macrosystem (alcohol outlet density), exosystem (social support and social networks) and microsystem (drinking behaviors and venue utilization) factors directly or indirectly play a role in the physical abuse of children. In addition, the interaction of factors across levels (alcohol outlet density and the percentage of local social companionship) can accentuate vulnerability for physical abuse. We present the discussion of these findings within the ecological-transactional framework.
Alcohol Outlet Density (Macrosystem)
Our study found direct relationships between alcohol outlet density and frequency of child physical abuse in the full sample without the cross-level interactions. Previous research has found a positive relationship between alcohol outlet densities and child maltreatment (Freisthler, 2004, Freisthler et al., 2007) and specifically density of off-premise outlets and rates of child physical abuse (Freisthler et al., 2004). This study differ in that on-premise density was related to more frequent use of physical abuse and off-premise was related to less use of physical abuse.
Our study takes a major step forward by explicitly testing one previously suggested theoretical mechanism for the relationship between alcohol outlets and child maltreatment (Freisthler & Holmes, 2012). We found that having a higher percentage of local social companionship support was related to more frequent use of physical abuse, and that this effect was moderated by alcohol outlet density. Parents involved with local social networks that favor frequent drinking away from home may be susceptible to influences that heighten aggressive parenting. Neighborhoods with high densities of on-premise alcohol outlets may house more negative social networks and provide more opportunities to drink outside the home, further enhancing the effect of local companionship support on frequency of child physical abuse. Parents may also choose to bring their children to these locations (e.g., restaurants), increasing stress if they expect a different behavior from their children including less whining, following directions the first time, or sitting quietly. If these behaviors do not occur, parents may use physical abuse to discipline the children after leaving the venue. These findings continue to build evidence that child maltreatment is influenced by the interaction between individual and ecological factors (Freisthler & Gruenewald, 2013).
Social Networks and Types of Social Support (Exosystem)
Similar to past research examining the relationship between perceived social support resources and child physical abuse (DePanfiles, 1996; Ortega, 2002; Polansky et al., 1985), emotional and tangible support were related to decreased frequency of physical abuse. In contrast, our results suggest that a rarely examined form of social support, social companionship, may actually put the child at greater risk of physical abuse. Further, this study found that when a parent reported having a higher percentage of his or her social companionship support network living within his or her neighborhood, more frequent physical abuse occurred in the full sample. Thus, the presence of negative social influences could lead to downward leveling of social norms, and ultimately affect parenting decisions and behaviors (Portes, 1998; Woolcock & Narayan, 2000). In other words, parents who have a lot of friends who live in their neighborhood with whom they regularly socialize may share discipline strategies with others, including use of physical discipline. Positive or non-reactions of friends and families providing social companionship support may create a norm where use of physical abuse is informally sanctioned (Emery et al., 2013).
Taken together, these findings indicate that differentiating between types of social support could help establish more nuanced relationships with both drinking behaviors and child physical abuse. It should be noted that these findings occurred when examining both the level of alcohol use and the dose-response relationship for drinkers.
Drinking Behaviors and Venue Utilization (Microsystem)
With regards to drinking behaviors, our first set of analyses that examines all types of drinking behaviors (from ex-drinkers to frequent heavy drinkers) found that all drinking categories (except for infrequent heavy drinkers) used physically abusive parenting practices more often than lifetime abstainers (Table 2). The dose-response models show that each additional drinking event at a bar, restaurant or home/party was related to more frequent use of physical abuse. Taken together, these findings suggest that any drinking behavior places a child at risk for physical abuse. As a parent drinks more, however, there may be a time when he or she is too intoxicated to perpetrate physical abuse. Previously, heavy drinking or alcohol abuse or dependence has been shown to be a risk factor for child physical abuse (Berger, 2005; Dube et al., 2001). This is supported here in the overall sample, but not for the drinkers only analysis; we also show that drinking location may play an important role in child physical abuse (Freisthler & Gruenewald, 2013).
Several microsystem vulnerability factors, including depressive symptoms, impulsivity, and parenting stress were related to higher frequency of child physical abuse, consistent with child maltreatment literature. Additionally, demographic characteristics of both the focal child (older age and male gender) and the parent (male gender, Asian American, African American, or other race, and lower income) were associated with higher frequency of physical abuse. These findings are consistent with child maltreatment literature (Black, Heyman, & Smith Slep, 2001; Sedlak et al., 2010). Unexpectedly, having fewer symptoms of anxiety was related to increased use of physical abuse. This could be a result of our anxiety measure, which include only two items. Alternatively, anxious parents could be more concerned about the social consequences of physically abusive behaviors than those with less anxiety.
Practice and Policy Implications
Practitioners working with parents who abuse their children should be aware that not all social support is necessarily beneficial. Workers could screen for more information about members of their social networks, including risky behavior. Doing this may lead to the identification of those at increased risk for child physical abuse. Social services providing treatment for neglectful and abusive parents might examine how family and friends may contribute to abusive behaviors. Interventions that assist parents in establishing more emotionally or tangibly supportive relationships with friends, families, and neighbors could provide at-risk parents with additional resources and reduce maltreatment.
Restricting alcohol outlets could reduce rates of child physical abuse (Sen, 2006), especially in areas where local social networks practice risky behaviors. In addition, community-based interventions could form babysitting cooperatives and welcoming committees in order to strengthen emotional and tangible support networks in high-risk neighborhoods (Freisthler & Holmes, 2012). These interventions could be used to help boost positive neighborhood influences, while diminishing the influence of risky social networks.
Limitations and Implications for Future Research
This study advances the literature on better understanding the specific mechanisms relating alcohol outlet densities to child physical abuse. In this case, that mechanism is through the percentage of local companionship support. Despite this, the study has several limitations. First, as a telephone survey with a low to moderate response rate, the survey cannot be generalized to all populations of parents. Telephone response rates have been declining in recent years and the response rate in the current study is similar to or better than response rates for other major telephone surveys (see, e.g., Curtin, Presser, & Singer, 2005; Kohut, Keeter, Doherty, Dimock, & Christian, 2012). Post-stratification survey weights were constructed to partially address this issue. This does not fully address issues related to non-response bias, particularly given that low income, young, and non-White populations traditionally do not have landlines (Kempf & Remington, 2007). Further, the sample in this study tends to be of higher income than those in the state of California at large. Given that we find rates of physical abuse are higher among low income parents, this study may underestimate the prevalence of physical abuse. Importantly, however, the populations studied here are often not included in studies of children involved in the child welfare system. Thus, it may provide important avenues for prevention or information about physical abuse rates among population not known to the child welfare system. Unfortunately, no individual-level data are available to examine differences between those that responded and those that did not in order to assess and control for this non-response bias above the use of post-stratification weights.
Next, the reliability estimates of some of the scales used in this study are slightly below acceptable levels. The small number of items that comprise each scale (four or fewer) may partially explain the low Cronbach’s alpha values (Tavakol & Dennick, 2011). This may be due, in part, to the use of the brief scales for the ISEL and PRIME-MD inventories. Use of the full scales with more items may result in higher reliability estimates of the measures. Factor analyses of the scale items were conducted to determine whether or not scales measured one or multiple constructs. For all scales, only one construct was being measured. Finally assessments of whether or not reliability would be improved by dropping an item found that, as developed, the scales had the strongest reliability estimates. Thus, full versions of the scales or similar scales with better reliability estimates are needed to replicate these findings.
As relationships between alcohol use, social support, and child physical abuse are still only correlational (using respondents’ assessments of past year behaviors), we cannot infer causality. We do control for a wide variety of individual and psychosocial covariates; however, we are unable to link any given physical abuse event to the use of alcohol. The social desirability bias among parents reporting physically abusive parenting behaviors could continue to be a problem despite the measures taken here to reduce it. Finally, the dose-response measures of drinking were estimated for each drinking context but are not able to take into account differential drinking behaviors across context types (e.g., some people have more drinks at bars than at home). Future research needs to account for how much parents drink at each context.
Although not conclusive, this study has supported the importance of examining the characteristics of social network members to understand the influence they may have on parenting behaviors, particularly pertaining to child maltreatment. Future research should further examine the role of alcohol use among parental social network members on child maltreatment. More specific information on the timing of drinking events in relation to physical abuse is warranted as is a longitudinal follow up with parents. Do parents drink as a response to stress after the abuse has occurred? Rather than lessening stress and anxiety, does socializing with friends intensify feelings of frustration or inadequacy around parenting, resulting in maladaptive parenting behaviors? Does drinking, even at low levels, increase disinhibition, allowing parents to use physical force more readily than when not drinking? How does alcohol outlet density further support the use of physical abuse? Is it through the facilitation of social activities for parents? Or, is it through a process of social selection where individuals more prone to violence use bars more often, escalating their violent tendencies? Additional work should also focus on what aspects of social companionship may facilitate abusive parenting. Under what circumstance do social networks condone or at least ignore physically abusive parenting practices? Answers to these questions will allow researchers to better tease apart the different mechanisms relating types of support, alcohol use, and alcohol outlets to child physical abuse. More importantly, a better understanding of these mechanisms will allow for a better, more nuanced approach to developing interventions to reduce physical abuse of children.
Acknowledgments
This project was supported by grant number P60-AA-006282 from the National Institute on Alcohol Abuse and Alcoholism. The content is solely the responsibility of the authors and does not necessarily represent the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Bridget Freisthler, Luskin School of Public Affairs, University of California, Los Angeles.
Megan R. Holmes, Mandel School of Applied Social Sciences, Case Western Reserve University
Jennifer Price Wolf, Prevention Research Center, Pacific Institute for Research and Evaluation.
References
- Barrera M. Distinctions between social support concepts, measures, and models. American Journal of Community Psychology. 1986;14:413–445. [Google Scholar]
- Beal AC, Ausiello J, Perrin JM. Social influences on health-risk behaviors among minority middle school students. Journal of Adolescent Health. 2001;28:474–480. doi: 10.1016/s1054-139x(01)00194-x. [DOI] [PubMed] [Google Scholar]
- Berger LM. Income, family characteristics, & physical violence toward children. Child Abuse & Neglect. 2005;29:107–133. doi: 10.1016/j.chiabu.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Black DA, Heyman RE, Smith Slep AM. Risk factors for child physical abuse. Aggression and Violent Behavior. 2001;6:121–188. [Google Scholar]
- Brick JM, Waksberg J, Kulp D, Starer A. Bias in list-assisted telephone samples. Public Opinion Quarterly. 1995;59:218–235. [Google Scholar]
- Chaffin M, Kelleher K, Hollenberg J. Onset of physical abuse and neglect: Psychiatric, substance abuse, and social risk factors from prospective community data. Child Abuse & Neglect. 1996;20:191–203. doi: 10.1016/s0145-2134(95)00144-1. [DOI] [PubMed] [Google Scholar]
- Chan YC. Parenting stress and social support of mothers who physically abuse their children in Hong Kong. Child Abuse and Neglect. 1994;18:261–269. doi: 10.1016/0145-2134(94)90110-4. [DOI] [PubMed] [Google Scholar]
- Cohen S, Hoberman H. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983;13:99–125. [Google Scholar]
- Cohen S, Mermelstein R, Kamarack T, Hoberman H. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social support: Theory, research, and application. Dordrecht, Netherlands: Martinus Nijhoff; 1985. pp. 73–94. [Google Scholar]
- Coohey C. Neglectful mothers, their mothers, and partners: The significance of mutual aid. Child Abuse & Neglect. 1995;19:885–889. doi: 10.1016/0145-2134(95)00051-9. [DOI] [PubMed] [Google Scholar]
- Coohey C. Child maltreatment: Testing the social isolation hypothesis. Child Abuse & Neglect. 1996;20:241–254. doi: 10.1016/s0145-2134(95)00143-3. [DOI] [PubMed] [Google Scholar]
- Coohey C. The role of friends, in-laws, and other kin in father-perpetrated child physical abuse. Child Welfare. 2000;79(4):373–402. [PubMed] [Google Scholar]
- Coohey C. Social networks, informal child care, and inadequate supervision by mothers. Child Welfare. 2007;68(6):53–66. [PubMed] [Google Scholar]
- Curtin R, Presser S, Singer E. Changes in telephone survey nonresponse over the past quarter century. Public Opinion Quarterly. 2005;69:87–98. [Google Scholar]
- Daniel JH, Hampton RR, Newberger EH. Child abuse and accidents in black families: A controlled comparative study. American Journal of Orthopsychiatry. 1983;53:645–653. doi: 10.1111/j.1939-0025.1983.tb03408.x. [DOI] [PubMed] [Google Scholar]
- DePanfilis D. Social isolation of neglectful families: A review of social support assessment and intervention models. Child Maltreatment. 1996;1:37–52. [Google Scholar]
- Dickman SJ. Functional & dysfunctional impulsivity: Personality & cognitive correlates. Journal of Personality & Social Psychology. 1990;58:95–102. doi: 10.1037//0022-3514.58.1.95. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Croft JB, Edwards VJ, Giles WH. Growing up with parental alcohol abuse: Exposure to childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect. 2001;25:1627–1640. doi: 10.1016/s0145-2134(01)00293-9. [DOI] [PubMed] [Google Scholar]
- Emery C, Nguyen H, Kim J. Understanding child maltreatment in Hanoi: Intimate partner violence, low self-control, and social and child care support. Journal of Interpersonal Violence. 2013 doi: 10.1177/0886260513506276. [DOI] [PubMed] [Google Scholar]
- Famularo R, Kinscherff R, Fenton T. Parental substance abuse and the nature of child maltreatment. Child Abuse & Neglect. 1992;16:475–483. doi: 10.1016/0145-2134(92)90064-x. [DOI] [PubMed] [Google Scholar]
- Freisthler B. A spatial analysis of social disorganization, alcohol access, and rates of child maltreatment in neighborhoods. Children and Youth Services Review. 2004;26:803–819. [Google Scholar]
- Freisthler B. Alcohol use, drinking venue utilization, and child physical abuse: Results from a pilot study. Journal of Family Violence. 2011;26:185– 193. doi: 10.1007/s10896-010-9352-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freisthler B, Midanik LT, Gruenewald PJ. Alcohol outlets and child physical abuse and neglect: Applying routine activities theory to the study of child maltreatment. Journal of Studies on Alcohol. 2004;65:586–592. doi: 10.15288/jsa.2004.65.586. [DOI] [PubMed] [Google Scholar]
- Freisthler B, Gruenewald PJ, Remer LG, Lery B, Needell B. Exploring the spatial dynamics of alcohol outlets and Child Protective Services referrals, substantiations, and foster care entries. Child Maltreatment. 2007;12:114–124. doi: 10.1177/1077559507300107. [DOI] [PubMed] [Google Scholar]
- Freisthler B, Holmes MR. Explicating the social mechanisms linking the ecology of alcohol use behaviors to child maltreatment. Journal of Sociology and Social Welfare. 2012;39:25–48. [PMC free article] [PubMed] [Google Scholar]
- Freisthler B, Gruenewald P. Where the individual meets the ecological: A study of parent drinking patterns, alcohol outlets, and child physical abuse. Alcoholism: Clinical and Experimental Research. 2013;37:993–1000. doi: 10.1111/acer.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovannoni JM, Billingsley A. Child neglect among the poor: A study of parental adequacy in family of three ethnic groups. Child Welfare. 1970;49:196–204. [Google Scholar]
- Greene WH. Econometric analysis. New York, NY: Macmillan; 1993. [Google Scholar]
- Greene WH. LimDep (Version 8.0) Plainview, NY: Econometric Software; 2002. [Google Scholar]
- Gruenewald PJ, Freisthler B, Remer L, LaScala EA, Treno A. Ecological models of alcohol outlets and violent assaults: Crime potentials and geospatial analysis. Addiction. 2006;101:666–677. doi: 10.1111/j.1360-0443.2006.01405.x. [DOI] [PubMed] [Google Scholar]
- Gruenewald PJ, Remer L. Changes in outlet densities affect violence rates. Alcoholism: Clinical & Experimental Research. 2006;30:1184–1193. doi: 10.1111/j.1530-0277.2006.00141.x. [DOI] [PubMed] [Google Scholar]
- Gruenewald PJ, Remer L, LaScala EA. Testing a social ecological model of alcohol use: The California 50-city study. Addiction. 2014 doi: 10.1111/add.12438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood - implications for substance-abuse prevention. Psychological Bulletin. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- He K, Kramer E, Houser RF, Chomitz VR, Hacker KA. Defining and understanding healthy lifestyles choices for adolescents. Journal of Adolescent Health. 2004;35:26–33. doi: 10.1016/j.jadohealth.2003.09.004. [DOI] [PubMed] [Google Scholar]
- Heckman J. Sample selection bias as a specification error. Econometrica. 1979;47:153–161. [Google Scholar]
- Kandel DB. Adolescent marijuana use: Role of parents and peers. Science. 1973;181:1067–1070. doi: 10.1126/science.181.4104.1067. [DOI] [PubMed] [Google Scholar]
- Kandel DB. Homophily, selection, and socialization in adolescent friendships. The American Journal of Sociology. 1978;84:427–436. [Google Scholar]
- Kaufman Kantor G, Straus M. The “drunken bum” theory of wife beating. Social Problems. 1987;34:214–231. [Google Scholar]
- Kelleher K, Chaffin M, Hollenberg J, Fischer E. Alcohol and drug disorders among physically abusive and neglectful parents in a community-based sample. American Journal of Public Health. 1994;84:1586–1590. doi: 10.2105/ajph.84.10.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempf AM, Remington PL. New challenges for telephone survey research in the Twenty-First century. Annual Review of Public Health. 2007;28:113–126. doi: 10.1146/annurev.publhealth.28.021406.144059. [DOI] [PubMed] [Google Scholar]
- Kohut A, Keeter S, Doherty C, Dimock M, Christian L. Assessing the representativeness of public opinion surveys. Washington, DC: Pew Research Center for the People & the Press; 2012. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Annuals of Internal Medicine. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Conger RD, Atkeson BM, Treiber FA. Parenting behavior and emotional status of physically abusive mothers. Journal of Consulting and Clinical Psychology. 1984;52:1062–1071. doi: 10.1037//0022-006x.52.6.1062. [DOI] [PubMed] [Google Scholar]
- Leenders R. Longitudinal behavior of network structure and actor attributes: Modeling interdependence of contagion and selection. In: Doreian P, Stokman FN, editors. Evolution of social networks. Amsterdam, The Netherlands: Gordon & Breach; 1997. pp. 165–184. [Google Scholar]
- Lipperman-Kreda S, Grube JW, Friend KB. Local tobacco policy and tobacco outlet density: Associations with youth smoking. Journal of Adolescent Health. 2012;50:547–552. doi: 10.1016/j.jadohealth.2011.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipton RI. The effects of moderate alcohol use on the relationship between stress and depression. American Journal of Public Health. 1994;84:1913–1917. doi: 10.2105/ajph.84.12.1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipton R, Gruenewald P. The spatial dynamics of violence and alcohol outlets. Journal of Studies on Alcohol. 2002;63:187–195. doi: 10.15288/jsa.2002.63.187. [DOI] [PubMed] [Google Scholar]
- Livaudais JC, Napoles-Springer A, Stewart S, Kaplan CP. Understanding Latino adolescent risk behaviors: Parental and peer influences. Ethnicity and Disease. 2007;17:298–304. [PubMed] [Google Scholar]
- Midanik LT, Greenfield T. Using interactive voice response technology for sensitive questions in national surveys: The 2005 National Alcohol Survey. Paper presented that the American Association of Public Health Annual Meeting; Boston, MA. 2006. [Google Scholar]
- Murphy JM, Jellinek MS, Quinn D, Smith G. Substance abuse and serious child mistreatment: Prevalence, risk, and outcome in a court sample. Child Abuse & Neglect. 1991;15:197–211. doi: 10.1016/0145-2134(91)90065-l. [DOI] [PubMed] [Google Scholar]
- Newberger EH, Hampton RR, Marx TJ, White KM. Child abuse and pediatric social illness: An epidemiological analysis and ecological reformulation. American Journal of Orthopsychiatry. 1986;56:589–601. doi: 10.1111/j.1939-0025.1986.tb03492.x. [DOI] [PubMed] [Google Scholar]
- Oats RK, Davis AA, Ryan MG, Stewart LF. Risk factors associated with child abuse. Child Abuse & Neglect. 1979;3:547–553. [Google Scholar]
- Ortega DM. How much support is too much? Parenting efficacy and social support. Children and Youth Services Review. 2002;24:853–876. [Google Scholar]
- Paschall MJ, Freisthler B, Lipton RI. Moderate alcohol use and depression in young adulthood: Findings from a National Longitudinal Study. American Journal of Public Health. 2005;95:453–457. doi: 10.2105/AJPH.2003.030700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pihl RO, Lau ML, Assaad JM. Aggressive disposition, alcohol, & aggression. Aggressive Behavior. 1997;23:11–18. [Google Scholar]
- Pihl RO, Peterson JB, Lau MA. A biological model of the alcohol-aggression relationship. Journal of Studies on Alcohol. 1993;11:128–139. doi: 10.15288/jsas.1993.s11.128. [DOI] [PubMed] [Google Scholar]
- Polansky NA, Ammons PW, Gaudin JM. Loneliness and isolation in child neglect. Social Casework: The Journal of Contemporary Social Work. 1985;6:38–47. [Google Scholar]
- Portes A. Social capital: Its origins and applications in modern sociology. Annual Review of Sociology. 1998;24:1–24. [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YF, Congdon R. HLM6: Hierarchical linear & nonlinear modeling. Lincolnwood, IL: Scientific Software International; 2006. [Google Scholar]
- Rohrbeck CA, Twentyman CT. Multimodal assessment of impulsiveness in abusing, neglecting, and nonmaltreating mothers and their preschool children. Journal of Consulting and Clinical Psychology. 1986;54:231–236. doi: 10.1037//0022-006x.54.2.231. [DOI] [PubMed] [Google Scholar]
- Romer D, Hennessy M. A biosocial-affect model of adolescent sensation seeking: The role of affect evaluation and peer-group influence in adolescent drug use. Prevention Science. 2007;8(2):89–101. doi: 10.1007/s11121-007-0064-7. [DOI] [PubMed] [Google Scholar]
- Sedlak AJ, Mettenburg J, Basena M, Petta I, McPherson K, Greene A, Li S. Fourth National Incidence Study of Child Abuse and Neglect (NIS–4): Report to Congress. Washington, DC: U.S. Department of Health and Human Services, Administration for Children and Families; 2010. [Google Scholar]
- Sen B. The relationship between beer taxes, other alcohol policies, and child homicide deaths. Topics in Economic Analysis & Policy. 2006;6:1–17. [Google Scholar]
- Straus MA, Fauchier A. Manual for the Dimensions of Discipline Inventory (DDI) Durham, NH: University of New Hampshire, Family Research Laboratory; 2007. [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the parent-child conflict tactics scales: Development and psychometric data for a national sample of American parents. Child Abuse & Neglect. 1998;22:249–270. doi: 10.1016/s0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- Tavakol M, Dennick R. Making sense of Cronbach’s alpha. International Journal of Medical Education. 2011;2:53–33. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa M, Smith B. Prevention and drug treatment. The Future of Children. 2009;19:147–168. doi: 10.1353/foc.0.0033. [DOI] [PubMed] [Google Scholar]
- Thompson RA. Preventing child maltreatment through social support. Thousand Oaks, CA: Sage; 1985. [Google Scholar]
- Thompson SK. Sampling. New York, NY: Wiley; 1992. [Google Scholar]
- Treno AJ, Gruenewald PJ, Remer LG, Johnson F, LaScala EA. Examining multi-level relationships between bars, hostility, and aggression: Social selection and social influence. Addiction. 2008;103:66–77. doi: 10.1111/j.1360-0443.2007.02039.x. [DOI] [PubMed] [Google Scholar]
- Tucker C, Lepkowski JM, Piekarski L. The current efficiency of list-assisted telephone sampling designs. Public Opinion Quarterly. 2002;66:321–338. [Google Scholar]
- Turner RJ, Avison WR. Assessing risk factors for problem parenting. Journal of Marriage and the Family. 1985;43:881–892. [Google Scholar]
- Uchino B. Social Support and physical health: Understanding the health consequences of relationships. New Haven, CT: Yale University Press; 2004. [Google Scholar]
- U.S. Department of Health and Human Services, Administration on Children, Youth and Families. Child maltreatment 2011. Washington, DC: Author; 2012. [Google Scholar]
- Warde A, Tampubolon G, Savage M. Recreation, informal social networks and social capital. Journal of Leisure Research. 2005;37:402–25. [Google Scholar]
- Whipple EE, Webster-Stratton C. The role of parental stress in physically abusive families. Child Abuse and Neglect. 1991;15:279–291. doi: 10.1016/0145-2134(91)90072-l. [DOI] [PubMed] [Google Scholar]
- Williamson JM, Borduin CM, Howe BA. The ecology of adolescent maltreatment: A multilevel examination of adolescent physical abuse, sexual abuse, and neglect. Journal of Consulting and Clinical Psychology. 1991;59:449–457. doi: 10.1037//0022-006x.59.3.449. [DOI] [PubMed] [Google Scholar]
- Wolock I, Magura S. Parental substance abuse as a predictor of child maltreatment re-reports. Child Abuse & Neglect. 1996;20:1183–1193. doi: 10.1016/s0145-2134(96)00114-7. [DOI] [PubMed] [Google Scholar]
- Woolcock M, Narayan D. Social capital: Implications for development theory, research and policy. The World Bank Research Observer. 2000;15:225–24. [Google Scholar]