Abstract
BACKGROUND:
Numerous studies have investigated the prevalence of neurologic and neurodevelopmental disorders individually, but few have examined them collectively, and there is uncertainty as to what extent they overlap.
METHODS:
The study has determined the proportions of children aged 0 to 11 years with diagnoses of autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD), epilepsy, and cerebral palsy (CP) in Norway. The data were obtained from the Norwegian Patient Register, which is nationwide and contains diagnoses assigned by Norwegian specialist health services (hospitals and outpatient clinics). The Norwegian Patient Register started collecting individual-level data in 2008, and the follow-up period for the study is years 2008 through 2010.
RESULTS:
For ASD, ADHD, and epilepsy, the proportions were highest in the oldest children. At age 11 years, the incidence was 0.7% for ASD, 2.9% for ADHD, and 0.9% for epilepsy. The cumulative incidence is likely to be higher because some cases diagnosed before 2008 were probably missed. For CP, the proportions were ∼0.3% for age ≥5 years. There was considerable overlap between diagnoses. For all disorders, boys had a significantly increased risk. In school-age children (aged 6–11 years) the male/female ratio was 4.3 for ASD, 2.9 for ADHD, 1.2 for epilepsy, and 1.3 for CP.
CONCLUSIONS:
The findings demonstrate the significant burden of disease associated with neurologic and neurodevelopmental disorders in children and that this burden is disproportionately skewed toward boys.
KEY WORDS: developmental disabilities, neurologic disorders, cumulative incidence, population register, autism spectrum disorder, attention-deficit/hyperactivity disorder, epilepsy, cerebral palsy
What’s Known On This Subject:
Prevalence estimates for neurologic and neurodevelopmental disorders in children vary widely, and there is uncertainty as to what extent the individual disorders overlap. Most previous prevalence studies have been based on survey data and not on specialist-confirmed diagnoses.
What This Study Adds:
This study used nationwide register data to determine the proportions of Norwegian children diagnosed with autism spectrum disorder, attention-deficit/hyperactivity disorder, epilepsy, and cerebral palsy and to study how the disorders overlap. All diagnoses were specialist-confirmed.
Neurologic and neurodevelopmental disorders account for a large proportion of long-term disabilities in children. Numerous studies have investigated the prevalence of such disorders individually, but only a few have examined them collectively and attempted to estimate the overall disease burden in the general population.1–4 Prevalence estimates also vary widely, which may partly be explained by the fact that most prevalence studies derive diagnoses from self-report surveys or chart abstraction, not from in-person specialist assessments.
For autism spectrum disorder (ASD), most recent prevalence estimates are ∼0.7%,5 but large studies from the United Kingdom6 and the United States7 have reported proportions as high as 1.2% and 0.9%, respectively. Attention-deficit/hyperactivity disorder (ADHD) prevalence estimates cover a wide range, but the most comprehensive review of available studies worldwide found a mean prevalence of 5.3%.8 In general, the use of the Diagnostic and Statistical Manual, Fourth Edition (DSM-IV) criteria tends to generate higher prevalence rates of ADHD than the use of International Classification of Diseases, 10th Revision (ICD-10) criteria,8,9 mainly because DSM-IV, unlike ICD-10, permits the diagnosis of ADHD on the basis of inattention alone, in the absence of hyperactivity.8 For epilepsy, the population prevalence in children is usually estimated to be between 0.5% and 1.0%.10 Recent studies from developed countries have found a decreasing prevalence, which is thought to result from better prevention of causes of epilepsy through improved perinatal care, improved immunization schedules, and reduced incidence of head trauma.10 Prevalence estimates for cerebral palsy (CP) range from 0.15% to 0.35% in most studies.11
More research is required to determine the extent of overlap between the individual neurologic and neurodevelopmental disorders. For example, it is well known that comorbid epilepsy is common in children with ASD, but the estimates vary from 5% to 46%.12 The overlap between ASD and ADHD is also debated.13 DSM-IV and ICD-10 preclude comorbid diagnoses of these disorders, but numerous studies have found extensive clinical overlap, with 20% to 50% of children with ADHD meeting criteria for ASD and 30% to 80% of ASD children meeting criteria for ADHD.13
The aim of this study was to determine the proportion of children diagnosed with ASD, ADHD, epilepsy, and CP in Norway and to investigate how the disorders overlap. The data were obtained from the Norwegian Patient Register (NPR), which collects data from all specialist health services in Norway.
Methods
Study Data
The NPR is an administrative database containing activity data from all Norwegian government-owned hospitals and outpatient clinics. Reporting of data to the NPR is mandatory and linked to the governmental reimbursement system for funding of health services. Diagnoses are reported as ICD-10 codes. The NPR was established in 1997, but the 11-digit personal identification number unique to every Norwegian citizen has only been reported since 2008, after a change in the health register act passed by the Norwegian Parliament on March 1, 2007. Consequently, individual-level research data are available from 2008 onward. The personal identification numbers are stored in encrypted form in the NPR.
Health care is free of charge for children up to age 16 years in Norway. All hospitals for children and most child outpatient clinics are government-owned. In addition, there are currently 58 pediatricians and child psychiatrists with private practices, of which 52 receive their funding through government reimbursements. Private practices receiving government reimbursements are obliged to report their data to the NPR in the same way as government-owned institutions. However, the reporting of personal identification numbers from private practices is not yet complete, and private practice data were not included in the data file used for this study. Very few cases of ASD, epilepsy, and CP are diagnosed at private clinics, so the lack of private practice data will not affect the cumulative incidence figures for those disorders. ADHD, however, is more commonly diagnosed by private specialists. We do not know the exact number of cases lost, but government figures show that the number of ADHD diagnoses reported for reimbursements by private practices account for 5% to 10% of the total number of ADHD diagnoses.
When a child has received a diagnosis of ASD, ADHD, epilepsy, or CP, follow-up is usually continued by the children’s general practitioners and/or municipal educational services working directly with schools, kindergartens, and day-care facilities. Continued specialist follow-up is provided if the child is receiving ongoing medical treatment or has medical conditions that require specialist follow-up. Therefore, we would not expect all diagnosed cases to be captured by the register every year. If children were diagnosed before 2008 and have not consulted specialist health services since then, they will not be found in the NPR. Consequently, the true cumulative incidence of the disorders will be somewhat higher than the figures calculated on the basis of current NPR data.
For this study, the NPR provided data from 2008 through 2010 for children born from 1999 through 2010 (aged 0–11 years at the end of follow-up) with diagnoses within the following ICD-10 sections:
F84 Pervasive developmental disorders (corresponding to ASD in DSM-IV)
F90 Hyperkinetic disorders (corresponding to ADHD in DSM-IV)
G40 Epilepsy
G41 Status epilepticus
G80 Cerebral palsy (CP)
The data file also included the following information: gender, year of birth, calendar year(s) in which the diagnosis was registered, type of clinic and contact (pediatric/child psychiatry; inpatient/outpatient), and number of contacts per calendar year.
In total, 136 079 inpatient and outpatient contacts with at least 1 of the relevant ICD-10 codes were identified. The personal identification number was available for 99.5% of identified cases. In cases for which the personal identification number was missing, the patient number unique to every patient within each hospital was used as a substitute. The data file did not contain any information that could be traced back to specific subjects. The use of such anonymous research files does not require regulatory ethics approval in Norway.
Statistical Analyses
Proportions for years 2008 through 2010, by gender and year of birth, were calculated by dividing the aggregate NPR numbers by the total number of residents in Norway with years of birth 1999 through 2010 at the end of follow-up on December 31, 2010. Total population numbers, broken down by gender and year of birth, were provided by Statistics Norway. Male-to-female ratios, with 95% confidence intervals (CI), were calculated by using Stata 11 (StataCorp, College Station, TX). To estimate the proportion of diagnosed cases captured by the registry, we divided the diagnoses by calendar year and calculated the proportions captured in consecutive years. On the basis of these proportions, we used the 2010 proportions to estimate the cumulative incidence of the disorders, assuming that the 2010 data would capture 60% of cases of ASD, ADHD, and epilepsy and 85% of CP cases in the study population. Estimates were made for ages 6 through 11 years combined and for 11-year-olds separately.
Validation of NPR Data
Birth years 1999 through 2010 were chosen for this study because they correspond to the recruitment period for the Norwegian Mother and Child Cohort,14 which is run by the Norwegian Institute of Public Health and includes 108 593 children and their parents. The cohort has ongoing substudies of ASD and ADHD, and studies of epilepsy and CP are under way. All these substudies are using, or will be using, NPR data for case ascertainment and will undertake independent validation of NPR diagnoses. So far, this has only been done by the ASD substudy, the Autism Birth Cohort study.15 This study validates NPR diagnoses of ASD by doing in-person clinical assessments. The assessment includes the standard diagnostic instruments for diagnosing ASD: the Autism Diagnostic Interview, Revised16 and the Autism Diagnostic Observation Schedule.17 Diagnoses are based on DSM-IV criteria for ASD. Present validation results are reported here.
Results
The study population included 731 318 children, 374 331 boys and 356 987 girls. The numbers of identified cases, distributed by gender and year of birth, are shown in Table 1. Figures 1 through 4 show the proportions of children with each diagnosis from 2008 through 2010, by year of birth, for boys and girls separately, and for all children combined. Table 2 shows male/female ratios for preschool children (aged 0–5 years) and school-age children (aged 6–11 years). Table 3 shows the overlap between the diagnoses. In Table 4, we have separated the diagnoses by calendar year and calculated the proportion of cases captured in consecutive years. Table 5 contains the proportions for 2010 and the estimates of true cumulative incidence of each disorder.
TABLE 1.
Study Population and Diagnoses
| Birth Year | Population | ASD | ADHD | Epilepsy | CP | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | |
| 1999 | 32 062 | 30 431 | 354 | 85 | 1336 | 458 | 333 | 253 | 101 | 90 |
| 2000 | 31 859 | 30 355 | 264 | 63 | 1152 | 365 | 287 | 219 | 116 | 57 |
| 2001 | 30 506 | 29 267 | 270 | 52 | 904 | 302 | 274 | 200 | 104 | 72 |
| 2002 | 29 777 | 28 759 | 252 | 49 | 649 | 202 | 232 | 195 | 94 | 67 |
| 2003 | 30 447 | 29 245 | 245 | 49 | 407 | 129 | 233 | 159 | 87 | 78 |
| 2004 | 30 703 | 29 327 | 178 | 47 | 196 | 74 | 180 | 170 | 105 | 74 |
| 2005 | 30 520 | 29 231 | 157 | 33 | 85 | 29 | 229 | 154 | 103 | 80 |
| 2006 | 31 333 | 29 848 | 100 | 33 | 31 | 12 | 189 | 153 | 93 | 65 |
| 2007 | 31 119 | 29 648 | 57 | 22 | 6 | 4 | 164 | 135 | 74 | 49 |
| 2008 | 32 055 | 30 211 | 27 | 9 | 2 | 2 | 141 | 132 | 68 | 44 |
| 2009 | 32 376 | 30 588 | 3 | 3 | 1 | 3 | 113 | 82 | 40 | 26 |
| 2010 | 31 574 | 30 077 | 0 | 0 | 2 | 1 | 31 | 40 | 2 | 7 |
| Total | 374 331 | 356 987 | 1907 | 445 | 4771 | 1581 | 2406 | 1892 | 987 | 709 |
Includes diagnoses registered in the Norwegian Patient Register (NPR) from 2008-10. ADHD diagnoses in children born in 2009 and 2010 were assumed to be registration errors and were not included in the other tables and figures.
FIGURE 1.
Proportion with autism spectrum disorder from 2008 through 2010. Includes ASD diagnoses registered in the NPR from 2008 through 2010 for children born from 1999 through 2010.
TABLE 2.
Male to Female Ratios
| Age 0–5 y | Age 6–11 y | |||||
|---|---|---|---|---|---|---|
| Boys % | Girls % | M/F Ratio | Boys % | Girls % | M/F Ratio | |
| ASD | 0.18 | 0.06 | 3.3 (2.6–4.1) | 0.84 | 0.19 | 4.3 (3.9–4.9) |
| ADHD | 0.07 | 0.03 | 2.5 (1.8–3.6) | 2.51 | 0.86 | 2.9 (2.7–3.1) |
| Epilepsy | 0.46 | 0.39 | 1.2 (1.1–1.3) | 0.83 | 0.67 | 1.2 (1.1–1.3) |
| CP | 0.20 | 0.15 | 1.3 (1.1–1.6) | 0.33 | 0.25 | 1.3 (1.2–1.5) |
Includes diagnoses registered in the NPR from 2008 through 2010 for children born 1999 through 2010. Age 0 to 5 y correspond to birth years 2005 through 2010, age 6 to 11 y to birth years 1999 through 2004.
TABLE 3.
Overlap Between Diagnoses
| Total | ASD | ADHD | Epilepsy | CP | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| ASD | 2352 | 408 | 17.3 | 263 | 11.2 | 18 | 0.8 | ||
| ADHD | 6345 | 408 | 6.4 | 335 | 5.3 | 59 | 0.9 | ||
| Epilepsy | 4298 | 263 | 6.1 | 335 | 7.8 | 552 | 12.8 | ||
| CP | 1696 | 18 | 1.1 | 59 | 3.5 | 552 | 32.5 | ||
Includes diagnoses registered in the NPR from 2008 through 2010 for children born 1999 through 2010.
TABLE 4.
Recapturing of Cases in Consecutive Years
| Registered 2008 | Recaptured 2009 | Recaptured 2010 | Registered 2009 | Recaptured 2010 | Registered 2010 | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | n | % | n | % | n | n | % | n | |
| ASD | 1000 | 719 | 72 | 621 | 62 | 1337 | 985 | 74 | 1794 |
| ADHD | 2684 | 2111 | 79 | 1580 | 59 | 3839 | 2848 | 74 | 4900 |
| Epilepsy | 2130 | 1514 | 71 | 1329 | 62 | 2623 | 1780 | 68 | 2923 |
| CP | 1151 | 1007 | 87 | 989 | 86 | 1303 | 1148 | 88 | 1452 |
Includes diagnoses registered in the NPR from 2008 through 2010 for children born 1999 through 2010.
TABLE 5.
Estimated Cumulative Incidence
| Age 6–11 y (n = 362 738) | Age 11 y (n = 62 493) | |||||
|---|---|---|---|---|---|---|
| No. Cases 2010 | Proportion 2010 | Estimated Cumulative Incidence | No. Cases 2010 | Proportion 2010 | Estimated Cumulative Incidence | |
| ASD | 1415 | 0.4% | 0.7% | 311 | 0.5% | 0.8% |
| ADHD | 4752 | 1.3% | 2.2% | 1257 | 2.0% | 3.4% |
| Epilepsy | 1904 | 0.5% | 0.9% | 401 | 0.6% | 1.1% |
| CP | 872 | 0.2% | 0.3% | 158 | 0.3% | 0.3% |
Age 6 to 11 years corresponds to birth years 1999 to 2004, age 11 years to birth year 1999. Estimates have been calculated by using NPR case numbers from 2010, assuming that within that calendar year, the NPR has captured 60% of all diagnosed cases of ASD, ADHD, and epilepsy and 85% of diagnosed cases of CP.
ASD
As shown in Fig 1, the proportions with ASD from 2008 through 2010 reached levels between 0.5% and 0.6% for children aged 7 to 10 and was 0.7% in 11-year-olds. The male/female ratio was higher in school-age children than in preschool children, 4.3 for ages 6 to 11 years (95% CI: 3.9–4.9) and 3.3 for ages 1 to 5 years (95% CI: 2.6–4.1). There was a high level of overlap between ASD and ADHD, with 17.3% of ASD cases also having diagnoses of ADHD. Comorbid epilepsy diagnoses were found in 11.2% of the ASD cases. The estimated cumulative incidence of ASD was 0.7% for ages 6 to 11 years combined and 0.8% for 11-year-olds.
Validation of ASD Diagnoses
In the ongoing validation of register ASD cases, we have now assessed 32 children invited on the basis of having ASD diagnoses registered in the NPR. Of these, 30 were found to meet the DSM-IV criteria for ASD, generating a positive predictive value of 94% (95% CI: 79%–99%). The participation rate in the validation study was 36% (32 out of 90 invited).
ADHD
ADHD diagnoses were rare in children <4 years of age. In our calculations, we have ignored the ADHD diagnoses recorded in children born in 2009 and 2010, assuming that such diagnoses in children <2 years of age are registration errors. The proportions from 2008 through 2010 were highest in the oldest children, reaching 2.9% at age 11 years (Fig 2). The male/female ratios were relatively similar in preschool and school-age children, 2.5 for ages 2 to 5 years (95% CI: 1.8–3.6) and 2.9 for ages 6 to 11 years (95% CI: 2.7–3.1). Comorbid diagnoses of ASD and epilepsy were common, with 6.4% of ADHD cases also having ASD diagnoses and 5.3% having epilepsy. The estimated cumulative incidence of ADHD was 2.2% for ages 6 to 11 years combined and 3.4% for 11-year-olds.
FIGURE 2.
Proportion with ADHD from 2008 through 2010. Includes ADHD diagnoses registered in the NPR from 2008 through 2010 for children born from 1999 through 2010.
Epilepsy
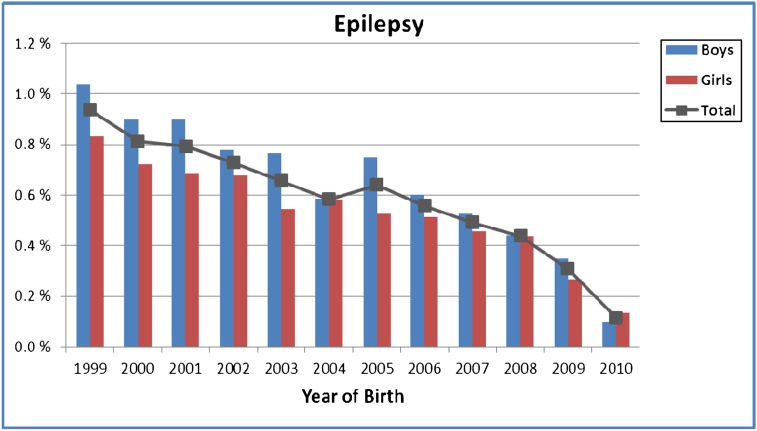
As for ASD and ADHD, the proportions with epilepsy from 2008 through 2010 were highest in the oldest children, at 0.9% overall in children aged 11 years (Fig 3). There was a significantly increased risk in boys, with a male/female ratio of 1.2 for the study population as a whole (95% CI: 1.1–1.3). Epilepsy had considerable overlap with the other diagnoses; 6.1% of registered cases had ASD, 7.8% had ADHD, and 12.8% had CP. The estimated cumulative incidence was 0.9% for ages 6 to 11 years combined and 1.1% for 11-year-olds.
FIGURE 3.
Proportion with epilepsy from 2008 through 2010. Includes epilepsy diagnoses registered in the NPR from 2008 through 2010 for children born from 1999 through 2010.
CP
As shown in Fig 4, the proportions of children with CP diagnoses from 2008 through 2010 were ∼0.3% for age ≥5 years. They were higher in boys than girls, with an overall male/female ratio of 1.3 (95% CI: 1.2–1.5). Comorbid epilepsy was found in 32.5% of children with CP. The proportions of CP cases captured in consecutive calendar years were high, and the estimated cumulative incidence (0.3% both for ages 6–11 years combined and for 11-year-olds) was similar to the proportions found for years from 2008 through 2010.
FIGURE 4.
Proportion with CP from 2008 through 2010. Includes CP diagnoses registered in the NPR from 2008 through 2010 for children born from 1999 through 2010.
Discussion
ASD
The proportion with ASD from 2008 through 2010 was 0.7% for 11-year-olds, and the estimated cumulative incidence at that age was 0.8%. The increase by age suggests that ASD is often not diagnosed until late childhood or early adolescence in Norway. If future follow-up confirms the estimate of 0.8%, it would be higher than reported in most previous studies but in line with recent findings from the United Kingdom6 and the United States.7 It is particularly worth noting that our estimate, which is based on specialist-confirmed diagnoses, is close to the latest US estimate of 0.9%,7 which was based on review of records. It is also worth noting the high levels of overlap between ASD and ADHD in our study sample, which clearly demonstrates a discrepancy between current diagnostic classification systems and clinical practice in Norway.
Validation of ASD Diagnoses
The results of the validation study indicate a high overall validity of ASD diagnoses assigned by specialist health services and confirm that the technical aspects of the NPR data collection are functioning well. The 2 children out of 32 who did not receive diagnoses of ASD at the independent validation were found to have mental retardation and specific language impairment, respectively. Those diagnoses are both closely aligned with ASD. However, the relatively low participation rate in the validation study (36%) warrants some caution in the interpretation of the findings.
ADHD
The proportion recorded with ADHD from 2008 through 2010 was 2.9% in 11-year-olds, and the estimated cumulative incidence was 3.4% at this age. The lack of data from private specialists caused a loss of some cases but no more than 10% of the total. Data from the Norwegian Prescription Database,18 which collects information on all drugs dispensed in Norway, show that 2.4% of people aged 10 to 19 years received ADHD medications in 2010. A study from the Norwegian research foundation SINTEF (Stiftelsen for industriell og teknisk forskning ved Norges tekniske høgskole) in 200419 (not available in English) found that 70% to 100% of children diagnosed with ADHD in Norway were medicated. However, the fact that the recapture of ADHD cases in consecutive years is as low as 60% to 70% in the NPR suggests that the proportion receiving medications may be lower now than it was 1 decade ago. All in all, the numbers indicate that the proportion of Norwegian children receiving a diagnosis of ADHD at some point during childhood and adolescence is between 3% and 4%, but longer follow-up is required to determine whether the ADHD prevalence in Norway is truly below the authoritative international estimate of 5.3%.8 Part of the discrepancy could simply be because the use of ICD-10 criteria, as in the Norwegian health care system, leads to fewer ADHD diagnoses than the use of DSM-IV criteria, as previously mentioned.9
Epilepsy
The finding that 0.9% of 11-year-olds had epilepsy diagnoses recorded in the period from 2008 through 2010, and the estimated cumulative incidence of 1.1% at this age are in striking contrast to recent studies in developed countries showing a prevalence closer to 0.5% than 1%.10 Our findings also differ from other epilepsy studies in that we found a significant increase in boys compared with girls. Additional research is required to find out why Norwegian figures differ from those of other comparable countries. More follow-up is also warranted to investigate why the recapture of epilepsy cases in consecutive years is as low as 60% to 70%. We had expected it to be higher in this group of patients with a presumably high proportion taking medications.
CP
Most cases of CP appeared to be diagnosed before 5 years of age, and the proportions recorded from 2008 through 2010 were relatively similar from age 5 years onward, at ∼0.3% overall. Although somewhat higher than previously reported from Norway,20 our figures are consistent with estimates of population prevalence from other Western countries.11 The high proportion of cases with comorbid epilepsy is also in accordance with previous findings.20,21 The proportions of cases recaptured in consecutive years were high, indicating that most children with CP are in contact with specialist health services every year. Consequently, the proportions of CP observed from 2008 through 2010 are likely to be close to the underlying population prevalence of the disorder.
Overall Findings
This is the first study of neurologic and neurodevelopmental disorders in Norway based on nationwide register data. The findings demonstrate the significant burden of disease associated with such disorders in children, and they clearly show how this burden is disproportionately skewed toward boys. For 11-year-olds, 4.3% of the population was registered with ≥1 of the 4 diagnoses under study, 5.9% of boys and 2.7% of girls. This is lower than recent figures from the United States,3 but the difference is largely driven by high prevalence rates of ADHD in the United States. We can safely assume that >5% of Norwegian children will have been diagnosed with ≥1 of the 4 disorders by the onset of puberty.
The main limitation of the study is the short duration of follow-up. The NPR has not been operative long enough to enable calculation of the exact cumulative incidence and population prevalence of the disorders under study. Another limitation is the lack of validation data for ADHD, epilepsy, and CP. Validation studies of these diagnoses would strengthen the research value of NPR data and will be undertaken in the years to come.
The study provides an example of the advantages of the Nordic health registers. The nationwide and mandatory data reporting prevents selection bias and loss to follow-up and provides an excellent framework for surveillance and research. It also makes it easier to study different disorders simultaneously, which is particularly beneficial for studies of neurologic and neurodevelopmental disorders because they often overlap and may share underlying genetic and environmental causes.
Acknowledgment
The population data from Statistics Norway were provided by Halvor Strømme.
Glossary
- ADHD
attention-deficit/hyperactivity disorder
- ASD
autism spectrum disorder
- CI
confidence interval
- CP
cerebral palsy
- DSM-IV
Diagnostic and Statistical Manual, Fourth Edition
- ICD-10
International Classification of Diseases, 10th Revision
- NPR
Norwegian Patient Register
Footnotes
All authors contributed as follows: (1) substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: The study was supported by grants from the Research Council of Norway, grant 189457 and 185476. The Autism Birth Cohort study, which includes the validation of autism spectrum disorder cases from the Norwegian Patient Register, is funded by the National Institute of Neurologic Disorders and Stroke, Bethesda, Maryland, grant NS47537.
References
- 1.Boyle CA, Decouflé P, Yeargin-Allsopp M. Prevalence and health impact of developmental disabilities in US children. Pediatrics. 1994;93(3):399–403 [PubMed] [Google Scholar]
- 2.Boulet SL, Boyle CA, Schieve LA. Health care use and health and functional impact of developmental disabilities among US children, 1997–2005. Arch Pediatr Adolesc Med. 2009;163(1):19–26 [DOI] [PubMed] [Google Scholar]
- 3.Boyle CA, Boulet S, Schieve LA, et al. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics. 2011;127(6):1034–1042 [DOI] [PubMed] [Google Scholar]
- 4.Atladóttir HO, Parner ET, Schendel D, Dalsgaard S, Thomsen PH, Thorsen P. Time trends in reported diagnoses of childhood neuropsychiatric disorders: a Danish cohort study. Arch Pediatr Adolesc Med. 2007;161(2):193–198 [DOI] [PubMed] [Google Scholar]
- 5.Fombonne E. Epidemiology of pervasive developmental disorders. Pediatr Res. 2009;65(6):591–598 [DOI] [PubMed] [Google Scholar]
- 6.Baird G, Simonoff E, Pickles A, et al. Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP). Lancet. 2006;368(9531):210–215 [DOI] [PubMed] [Google Scholar]
- 7.Autism and Developmental Disabilities Monitoring Network Surveillance Year 2006 Principal Investigators. Centers for Disease Control and Prevention (CDC) . Prevalence of autism spectrum disorders—Autism and Developmental Disabilities Monitoring Network, United States, 2006. MMWR Surveill Summ. 2009;58(10):1–20 [PubMed] [Google Scholar]
- 8.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942–948 [DOI] [PubMed] [Google Scholar]
- 9.Faraone SV, Sergeant J, Gillberg C, Biederman J. The worldwide prevalence of ADHD: is it an American condition? World Psychiatry. 2003;2(2):104–113 [PMC free article] [PubMed] [Google Scholar]
- 10.Shinnar S, Pellock JM. Update on the epidemiology and prognosis of pediatric epilepsy. J Child Neurol. 2002;17(Suppl 1):S4–S17 [DOI] [PubMed] [Google Scholar]
- 11.Blair E. Epidemiology of the cerebral palsies. Orthop Clin North Am. 2010;41(4):441–455 [DOI] [PubMed] [Google Scholar]
- 12.Spence SJ, Schneider MT. The role of epilepsy and epileptiform EEGs in autism spectrum disorders. Pediatr Res. 2009;65(6):599–606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rommelse NN, Franke B, Geurts HM, Hartman CA, Buitelaar JK. Shared heritability of attention-deficit/hyperactivity disorder and autism spectrum disorder. Eur Child Adolesc Psychiatry. 2010;19(3):281–295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Magnus P, Irgens LM, Haug K, Nystad W, Skjaerven R, Stoltenberg C, MoBa Study Group . Cohort profile: the Norwegian Mother and Child Cohort Study (MoBa). Int J Epidemiol. 2006;35(5):1146–1150 [DOI] [PubMed] [Google Scholar]
- 15.Stoltenberg C, Schjølberg S, Bresnahan M, et al. ABC Study Group . The Autism Birth Cohort: a paradigm for gene-environment-timing research. Mol Psychiatry. 2010;15(7):676–680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview—Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24(5):659–685 [DOI] [PubMed] [Google Scholar]
- 17.Lord C, Risi S, Lambrecht L, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30(3):205–223 [PubMed] [Google Scholar]
- 18.Norwegian Prescription Database. Available at: www.norpd.no. Accessed January 16, 2012 (data available in English)
- 19.SINTEF (Stiftelsen for industriell og teknisk forskning ved Norges tekniske høgskole). (2004). National survey of the offer comprehensive diagnosis and treatment of children and adolescents with ADHD [in Norwegian]. Report STF78 A045012.
- 20.Andersen GL, Irgens LM, Haagaas I, Skranes JS, Meberg AE, Vik T. Cerebral palsy in Norway: prevalence, subtypes and severity. Eur J Paediatr Neurol. 2008;12(1):4–13 [DOI] [PubMed] [Google Scholar]
- 21.Odding E, Roebroeck ME, Stam HJ. The epidemiology of cerebral palsy: incidence, impairments and risk factors. Disabil Rehabil. 2006;28(4):183–191 [DOI] [PubMed] [Google Scholar]