Abstract
OBJECTIVE:
To test the effect of a culturally tailored, family-centered, short-term behavioral intervention on BMI in Latino-American preschool-aged children.
METHODS:
In a randomized controlled trial, 54 parent–child dyads were allocated to the intervention and 52 dyads were allocated to an alternative school-readiness program as the control condition. Parent–child dyads were eligible if the parent self-defined Latino, was at least 18 years old, had a 2- to 6-year-old child not currently enrolled in another healthy lifestyle program, had a valid telephone number, and planned on remaining in the city for the next 6 months. The Salud Con La Familia (Health with the Family) program consisted of 12 weekly 90-minute skills-building sessions designed to improve family nutritional habits and increase physical activity. Both programs were conducted in a community recreation center serving an urban neighborhood of mostly Spanish-speaking residents.
RESULTS:
Forty-two percent of participating preschool-aged children were overweight or obese. Controlling for child age, gender, and baseline BMI, the effect of the treatment condition on postintervention absolute BMI was B = –0.59 (P < .001). The intervention effect seemed to be strongest for obese children.
CONCLUSIONS:
A skills-building, culturally tailored intervention involving parent–child dyads changed short-term early growth patterns in these Latino-American preschool-aged children. Examining long-term effects would be a prudent next step.
KEY WORDS: childhood obesity, family-centered intervention, Latino, preschool-aged children
What’s Known on This Subject:
Childhood obesity is already prevalent by preschool age, particularly among Latinos. Parents have tremendous influence on factors that contribute to childhood obesity (eg, diet, physical activity); thus, family plays a crucial role in pediatric obesity prevention.
What This Study Adds:
This randomized controlled trial examined the effect of a behavioral intervention involving Latino-American parent–preschool-aged child dyads. The intervention resulted in reductions in absolute BMI across the 3-month study period, with patterns suggesting the largest effect for obese children.
Worldwide trends indicate alarming rates of childhood overweight/obesity, even among preschool-aged children and particularly in industrialized countries.1 Increases in sedentary lifestyle and high-calorie food consumption, among other factors, contribute to epidemic levels of childhood obesity in the United States, and families of Hispanic/Latino descent are disproportionately affected.2,3 By the time children are eligible for preschool, ∼27.7% of Latino-American children are at least overweight, and 14.2% are obese compared with 17.4% and 9.1%, respectively, in non-Hispanic white populations.2 Children who are overweight during the preschool period are more likely to become overweight adolescents and obese adults.4 Food preferences and activity habits set in early childhood influence lifelong trajectories for BMI and health.5,6 Specifically, rapid BMI gain in early childhood contributes to adulthood mortality and morbidity.7,8 The longer unhealthy patterns exist, the more difficult it can be to reverse them. Therefore, healthy lifestyle interventions for preschool-aged children have the potential to improve lifelong health.
However, few pediatric obesity interventions have included preschool-age children in the prevention or early treatment of overweight and obesity. Of 7 published randomized controlled trials with this age group, most were school based.9 In their review of these studies, Monasta et al9 concluded that none of the interventions altered weight gain or BMI. Reasons suggested for the failure of these interventions included faulty study designs, inadequate parental engagement, or failure to account for macro-environments (eg, neighborhoods, community, society).
Nutrition and activity patterns are determined not only by the child but within the family10 and community.11 Thus, multilevel interventions targeting children, families, and communities are necessary to create and maintain health-promoting conditions for young children. Consequently, the Institute of Medicine12 and the Strategic Plan for NIH Obesity Research13 call for a sustainable community-engaged and family-centered approach to obesity prevention. The purpose of the current study was to examine the short-term effect of such a family-centered behavioral intervention, delivered in a community setting, on early growth patterns in Latino-American preschool-aged children.
Methods
Study Population and Design
By using a parallel-group, randomized controlled trial design, we tested the efficacy of a culturally tailored, family-centered obesity prevention intervention for Latino-American parent–preschool-aged child dyads. This trial was conducted in a public community recreation center located in a neighborhood with a relatively large Spanish-speaking population. The study was approved by the Vanderbilt University Institutional Review Board (number 080673). The full trial protocol is available from the first author on request.
Recruitment occurred between October 2008 and February 2009. A bilingual research assistant approached individuals in the waiting areas of cooperating community agencies (eg, social service agencies, pediatric clinics, community centers), briefly described the study, and screened interested parents for eligibility in the language of their choice. The study was advertised via multiple mechanisms: flyers at community organizations and businesses; Spanish-language radio; Spanish newspapers; and word-of-mouth. Parents aged >18 years met inclusion criteria if they: (1) defined themselves as Hispanic/Latino; (2) had a child aged 2 to 6 years not currently enrolled in another healthy lifestyle program; (3) had a valid telephone number; and (4) planned on remaining in the city for the next 6 months. Eligible adults underwent a 30-minute oral consent process in Spanish before providing written consent for themselves and their preschool-aged child.
Randomization and Masking
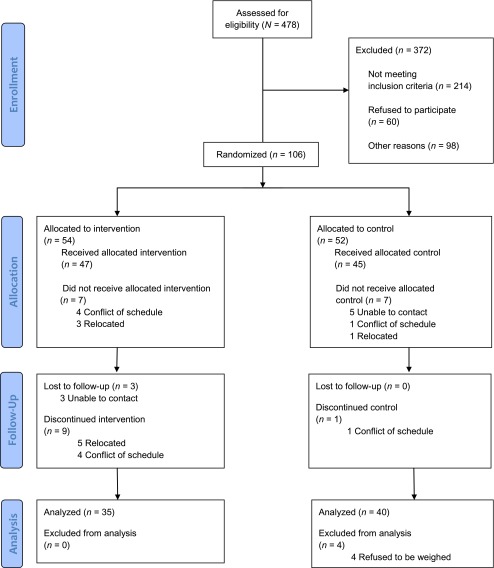
Study randomization occurred after baseline data collection. A total of 106 parent–child dyads were randomized to treatment (Fig 1). A computer-generated permuted block randomization scheme with a block size of 10 was used to ensure balanced treatment allocation once the total sample size was reached. A biostatistician generated the randomization list, and condition assignments were placed in nontransparent envelopes, which were sealed and numbered consecutively. After giving informed consent, participants opened the next numbered allocation envelope. The condition assignment and number listed on the envelope were recorded by the research assistant and the participant. Neither research staff nor participants were blinded to other participants’ condition allocation.
FIGURE 1.
Flowchart of participants.
Intervention Condition
The culturally tailored Salud Con La Familia (Health with the Family) program consisted of weekly 90-minute skills-building sessions for parents and preschool-aged children designed to improve nutritional family habits, increase weekly physical activity, and decrease media use (sedentary activity). All sessions were conducted in Spanish by the same trained facilitator. To ensure a sizeable treatment dosage,14 the intervention involved a series of 12 group sessions occurring between March and June 2009. Social cognitive theory and the transtheoretical model of change guided the intervention design.15,16 The content was based on a best-practice culturally tailored program for Latino-American families developed by the National Latino Children's Institute.17 To make this curriculum multilevel, we added a component intended to build new social groups, given the evidence that social networks can disseminate health behaviors and health outcomes throughout communities.18 Participants were randomly assigned to small social groups (6–8 parent–child dyads), and at each session they were assigned small group activities (engaging both parents and children as the focus of the intervention) and specific group roles. The Appendix provides the curricular modules.
Control Condition
A brief school readiness program was conducted as an alternative to the active intervention because there is no standard care condition for comparison. By providing some programming at the same location, we aimed to guard against differential dropout between the intervention and control groups. Participants met 3 times for 60 minutes over the 12-week study period. The control group’s program was designed to improve school readiness in preschool-aged children through increased parental verbal engagement (eg, daily reading, playing word games, how to talk to children).19 The program was based on the Dialogic Reading Model–C.A.R. (Comment and Wait, Ask Questions and Wait, and Respond by Adding More), an empirically tested curriculum that teaches parents to read picture books with their children.17 This model lends itself to all Spanish-speaking parents, importantly including those with low literacy or low English-language skills. The didactic session format did not encourage social networking. All sessions were conducted in Spanish by the same facilitator who conducted the intervention sessions.
Both transportation to and from study sessions and on-site child care services (for siblings) were provided free of charge to all study participants to overcome the most frequently cited barriers to study participation.20 Participants received small incentives after each wave of data collection (eg, cutting board, kitchen timer, gift card to local supermarket), a total value of $60 per parent–child dyad over the study period.
Treatment Fidelity
Before study initiation, a treatment fidelity plan was devised to monitor and enhance the reliability and validity of our behavioral intervention following the methodologic practices suggested by the Treatment Fidelity Workgroup of the National Institutes of Health Behavior Change Consortium.21 The plan included implementer/facilitator training and supervision; verification of essential treatment components by a supervisor; controlling for differences between interventionists by having the same 1 administer each condition; and collection of fidelity measures (eg, length, number, frequency of sessions; participation rates). A study team member observed 3 sessions of each condition and determined that 100% of the intended key messages were fully discussed, all planned activities occurred, and intervention content was never delivered during control sessions or vice versa.
Data Collection
Anthropometric measurements were collected from both preschool-aged children and participating parents collected at the community center by trained study staff who followed standardized techniques.22 The main outcome of interest was children’s absolute BMI at the 3-month follow-up. Surveys with parents were conducted by trained bilingual research staff.
Measures
Height and Weight
Body weight was measured, after voiding and while wearing light clothing but no shoes, to the nearest 0.1 kg on a calibrated digital scale (model 758C; Detecto, Webb City, MO). Body height without shoes was measured to the nearest 0.1 cm with an attached stadiometer.
BMI
Absolute BMI (weight [kg]/height [m2]) was analyzed because research suggests that it is more appropriate for analyzing change over time.23 Weight categories were also assigned to all children (underweight [<fifth percentile], normal [fifth to <85 percentile], overweight [85 to <95 percentile], or obese [≥95 percentile]), according to their BMI percentile calculated by using the Centers for Disease Control and Prevention’s calculator based on the centers’ 2000 growth charts.24
Demographic Characteristics
Parents completed a demographic survey in Spanish that included date of birth, gender, and country of origin of parent and child and highest parental education level. Acculturation was measured by using the widely used and previously validated Short Acculturation Scale for Hispanics.25 This scale asks parents what language they speak, use at home, think in, and use among friends given the following options: Spanish only, Spanish better than English, Spanish and English equally, English better than Spanish, and English only. Responses were averaged across the 4 items, with scores ranging from 1 to 5; <2 indicates a low level of acculturation.25 Internal reliability of this scale was α = .81 in our sample.
Statistical Analysis
Groups were analyzed as randomized (ie, intent-to-treat analysis), meaning we accounted for assignment to the intervention or control condition but not dosage (ie, number of sessions attended). Based on input from the community center’s staff on feasible recruitment goals, the expected sample size was 50 dyads per condition (N = 100). Given traditional26 assumptions (80% power; 2-tailed P < .05), Cohen-based software27 was used to conduct a post hoc power analysis, which indicated the final sample size (N = 92) was large enough to detect at least a medium-size effect of r = 0.31.
We used χ2 and Student’s t tests to compare the intervention and control groups on baseline characteristics. To test the effect of the intervention on children’s absolute BMI postintervention, 2 linear regression models were conducted. The first model included only the treatment group condition variable, and the second model additionally included child age at baseline, child gender, and baseline absolute BMI. The inclusion of these relevant independent variables is necessary to meet the assumptions of linear regression and to arrive at unbiased estimates of the intervention effect. Linear regression was used instead of the analysis of covariance to examine the potential size of the intervention effect and the contributions of the other predictor variables, rather than to simply determine the directionality of the effect. It should be noted that linear regression and analysis of covariance yield equivalent statistical test results.28 We also computed the average change in BMI from baseline to 3 months and described how it varied across initial weight categories.
All analyses were conducted by using Stata/IC version 12.0 for Windows (StataCorp LP, College Station, TX), and statistical significance was defined as P < .05.
Results
Sample Description
Approximately 6 weeks passed between baseline data collection and the first intervention and control sessions. In this time, 14 randomized participants withdrew from the study pool, leaving a sample of 92 dyads exposed to intervention or control conditions. As Fig 1 shows, the attrition rate from initial exposure to 3-month follow-up was lower in the control group (15%) than in the intervention group (36%). There were no significant demographic or anthropometric differences at baseline between dyads who completed the 3-month follow-up data collection (n = 75) and randomized participants who did not finish the study (n = 27) (results available on request).
Among the 75 dyads who completed the 3-month follow-up and comprised the analytic sample, 84% of the parents were born in Mexico, 11% in other Central American countries, and 5% in the United States; 91% of the children were born in the United States. As of the baseline data collection, almost two-thirds (65%) of parents neither completed high school nor obtained a certificate of General Educational Development. The average level of acculturation among parents was low. Eighty-one percent of participating parents were overweight/obese (BMI ≥25) as well as 42% of children (BMI percentile ≥85%). According to t tests and Fisher’s exact tests, the groups of dyads who completed the intervention and control conditions did not significantly differ on demographic characteristics or anthropometric measurements at baseline (Table 1).
TABLE 1.
Baseline Demographic Characteristics of Latino Parent–Child Dyads (N = 75)
| Characteristic | Control | Intervention |
|---|---|---|
| Child | ||
| Age, mean (SD) | 4.1 ± 0.9 | 4.2 ± 0.9 |
| Country of origin, n (%)a | ||
| United States | 38 (95.0) | 30 (85.7) |
| Mexico | 2 (5.0) | 4 (11.4) |
| Guatemala | 0 (0) | 1 (2.9) |
| Gender, n (%) female | 22 (55.0) | 16 (45.7) |
| Absolute BMI, mean (SD) | 17.2 ± 2.21 | 16.6 ± 2.35) |
| BMI category, n (%) | ||
| Underweight (BMI <fifth percentile) | 2 (5.0) | 1 (2.9) |
| Normal wt (BMI ≥fifth to <85th percentile) | 19 (47.5) | 21 (61.8) |
| Overweight (BMI ≥85th to <95th percentile) | 10 (25.0) | 5 (14.7) |
| Obese (BMI ≥95 percentile) | 9 (22.5) | 7 (20.6) |
| Adult | ||
| Age, mean (SD), y | 31.9 ± 5.5 | 30.7 ± 6.0 |
| Country of origin, n (%) | ||
| United States | 2 (5.0) | 2 (5.7) |
| Mexico | 35 (87.5) | 28 (80.0) |
| Guatemala | 1 (2.5) | 1 (2.9) |
| Ecuador | 1 (2.5) | 1 (2.9) |
| El Salvador | 1 (2.5) | 2 (5.7) |
| Costa Rica | 0 (0.0) | 1 (2.9) |
| Acculturation, mean (SD) | 1.4 ± 0.6 | 1.3 ± 0.5 |
| Mother of child, n (%) | 38 (95.0) | 33 (94.3) |
| Parental education, n (%) | ||
| <High school | 26 (65.0) | 23 (65.7) |
| ≥High school and <college | 11 (27.5) | 11 (31.4) |
| ≥College | 3 (7.5) | 1 (2.9) |
| BMI, mean (SD) | 30.3 ± 5.7 | 29.0 ± 5.3 |
| BMI category, n (%) | ||
| Normal (BMI ≥18.5 and <25) | 7 (17.5) | 7 (20.0) |
| Overweight (BMI ≥25 and <30) | 14 (35.0) | 16 (45.7) |
| Obese (BMI ≥30) | 19 (47.5) | 12 (34.3) |
Percentages may not sum to 100% because of rounding.
Absolute BMI Regression Results
The first linear regression model shown in Table 2 reveals a nonsignificant unadjusted effect of the treatment condition on children’s absolute BMI (B = –0.63; 95% confidence interval [CI]: –1.68 to 0.42; P = .24). When covariates were adjusted for in the second model, more precise estimates resulted in a narrower CI and statistical significance of the treatment effect. Controlling for child age, gender, and initial BMI, the effect of the treatment condition on children’s absolute BMI was B = –0.59 (95% CI: –0.94 to –0.25; P < .001).
TABLE 2.
Linear Regressions Predicting Children’s Absolute BMI After a 3-Month Intervention
| Predictor Variable | BMI at 3 Months | |||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | |||||
| B | 95% CI | P | B | 95% CI | P | |
| Treatment | −0.63 | −1.68 to 0.42 | 0.24 | −0.59 | −0.94 to –0.25 | .001 |
| Baseline BMI | — | — | 0.96 | 0.88 to 1.04 | <.001 | |
| Child age | — | — | 0.12 | −0.08 to 0.32 | .24 | |
| Child gender | — | — | 0.01 | −0.34 to 0.35 | .96 | |
| R2 | 0.01 | 0.90 | ||||
B = unstandardized coefficient. n = 75 for unadjusted models; n = 74 for adjusted models because baseline BMI information was missing for 1 child. Cells are empty if variables were not included in the model.
Variation in Absolute BMI Change Across Initial Weight Categories
To study how the effect of our intervention varied by initial weight categories, we computed change scores for each child and compared the average change in children’s absolute BMI across initial BMI weight categories for treatment and control groups. Because of the small size of the initial weight category subgroups, comparisons are discussed as trends, not as statistically significant differences. Across all weight categories, the mean ± SD change in BMI for the treatment group was –0.51 ± 0.87; for the control group, it was 0.06 ± 0.61.
The most pronounced difference in BMI change between treatment and control groups occurred among obese children. Those children who started the trial as obese and were exposed to the intervention had a mean BMI change of –0.80 ± 1.48 versus obese children in the control group who experienced a mean change of 0.08 ± 0.467. Similar differences occurred for children who were overweight at baseline: those in the intervention group had a mean BMI change of –0.63 ± 0.67 compared with those in the control group who experienced a mean change of 0.11 ± 0.76.
Those children initially categorized as normal weight who participated in the intervention decreased their BMI more than normal-weight children in the control group. To further investigate this finding, we distinguished between children who started the trial with a BMI percentile ≥5% and <45% and those that started the trial with a BMI percentile ≥45% and <85%. The children in the intervention group who were in the lower half of the normal weight category (n = 7) at baseline experienced a smaller mean change in their BMI (–0.06 ± 0.80) versus those in the control group (–0.42 ± 0.31; n = 6). In comparison, the children in the intervention group who were in the higher half of the normal-weight category at baseline (n = 14) experienced a mean change in BMI of –0.55 ± 0.55, and those in the control group (n = 13) had a mean change in BMI of 0.17 ± 0.51.
Discussion
Preschool-age is a critical period of development that affects growth patterns and associated health outcomes into adulthood.7 In the current study, a randomly assigned intervention resulted in short-term improvements (ie, decreases) in Latino-American preschool-aged children’s absolute BMI. In comparison, almost all children in the control group increased their BMI over the 3-month intervention. These findings highlight the importance of prevention at these early ages.
Latino-American preschool-aged children who participated in our intervention experienced an average reduction in absolute BMI of 0.51 over 3 months. Although this intervention is 1 of the first to demonstrate an effect in the desired direction for Latino-American preschool-aged children, 42% of whom were already overweight/obese, the reported decrease is within the range of magnitude reported for obesity treatment interventions with overweight/obese school-aged children.29–31 For example, a nonrandomized community-based intervention conducted with school-aged children in the United Kingdom resulted in a 1.0 decrease in BMI after 6 months.32
Other trials assessing children in preschool environments failed to demonstrate improvements in growth patterns.9,33 We suspect that the success of our trial was attributable to the inclusion of parent–child dyads instead of preschool-aged children alone. Similarly, a recently published small trial by Stark et al34 of 17 families with obese preschool-aged children reported reductions in BMI after an in-home family-centered intervention. Also, Epstein et al,10 in 1 of the few effective obesity treatment programs for school-aged children, demonstrated sustainable change 10 years after the program, with a strong parent involvement component to the intervention. In early childhood, the role of the parent is especially crucial because they have a great deal of influence over their child’s physical activity, sedentary lifestyle, and dietary choices.
Our data support the need for prevention efforts at early ages and the notion that a community-engaged, family-centered intervention can successfully change early short-term growth patterns. These findings are novel for 3 reasons. First, our findings suggest that future research on behavioral interventions for parent–preschool-aged child dyads can be fruitful. This type of intervention holds the promise of effectiveness in modifying a health outcome that has been resistant to change. Second, our data suggest that the preschool period offers a promising time frame in which to intervene. We consider the short-term change over 3 months to be particularly meaningful because it occurred during a critical window of development that has potential for not only preventing the onset of pediatric obesity but also for providing sustained health benefits across the life span, if these patterns are sustained.35 Third, our data fill an obvious ethnicity gap given that Latino-Americans are underrepresented in published obesity interventions, despite their increased disease burden and rising demographics.36
Despite advancing the field, there are notable limitations to our study. First, our sample size was too small to statistically test changes in weight categories over the 3 months.37,38 However, even with these small numbers, we found a statistically significant effect of the intervention on absolute BMI, and the degree of change was similar to studies39,40 with older overweight/obese children. As with most community studies, attrition occurred over the course of the intervention, and this attrition was greater in the intervention group than in the control group. This fact could have biased our findings if those who remained in the intervention were particularly motivated, but that is unlikely given that the noncompleters had initial anthropometric data similar to the completers. Recognizing this limitation, we used multiple imputation and reran the linear regression with the full randomized sample (N = 106), which resulted in similar coefficients and no change in significance. Finally, we cannot determine if these short-term gains are sustainable longitudinally. However, this is an important first step in demonstrating an effect of early intervention for Latino-American preschool-aged children, who are disproportionately at risk for obesity and all its comorbidities.
Conclusions
A skills-building, culturally tailored, family-centered intervention involving parent–child dyads changed short-term early growth patterns in Latino-American preschool-aged children. Given that this is a critical window of child development, it is a crucial time to prevent childhood obesity. Future research to test the sustainability and long-term effects of this approach would be a prudent next step.
Acknowledgments
We thank Tokesha Warner, MHA, an employee of Vanderbilt University, for research coordination, as well as Paul Widman, BS, and Stevon Neloms, MBA, of Davidson County and Nashville Metro Parks and Recreation for their voluntary collaboration during study implementation. We also thank Stephanie Mitchell and Evan Sommer for their contributions in editing the manuscript.
Glossary
- CI
confidence interval
APPENDIX
Salud Con La Familia (Health with the Family) Curricular Modules Overview
| Session | Theme | Key Messages | 90-Minute Session Activities Outline | ||
|---|---|---|---|---|---|
| 1 | Introduction, Community-building, Medical Home | 1. | Create context (what), compelling rationale (so what), and expectations (now what) for this study. | 1. | Welcome and introduction by facilitator and program team (3 minutes) |
| 2. | Icebreaker, name, place of birth, and why I am here (10 minutes) | ||||
| 3. | Assign participants to small communities (2 minutes) | ||||
| 2. | Participants are informed of study’s organization and outcome measures to be collected from them. | 4. | Themed conversation in small communities: What do I wish to get out of this program? (10 minutes) | ||
| 5. | Small communities sharing with whole group (5 minutes) | ||||
| 6. | Participants receive medical home resource information (20) | ||||
| 3. | Parents learn the importance of identifying a medical home, having 1 consistent clinic or provider group who knows the child and family to maximize health outcomes. | 7. | Parent–child kitchen activity with a healthy food item participants can prepare at home (20) | ||
| 8. | Individual goal setting (10 minutes) | ||||
| 9. | Announcements and good-byes (10 minutes) | ||||
| 2 | Parenting Skills | 1. | Parenting styles around food are often permissive and set no limits. | 1. | Facilitator welcomes participants, facilitates a fun energizer physical activity. (10) |
| 2. | Program coordinator reviews previous session’s messages. (10) | ||||
| 2. | Many Latino parents have a cultural perception of “gordito = healthy,” which deserves reconsideration for the health of Latino children in the United States. | 3. | Program coordinator makes a presentation on parenting styles around food, cultural perceptions of “gordito = healthy,” and parenting skills for setting limits with specific positive attention. (20) | ||
| 4. | Participants work in small and whole group activities practicing skills for giving specific positive attention on nutrition and physical activity: stating expectations in advance and catch your child being good. (25) | ||||
| 3. | Encouraging and monitoring the child’s and parent’s own good nutrition and daily physical activity are critical to good parenting. | 5. | Program coordinator facilitates parent–child completing an activity contract with goal setting. (10) | ||
| 4. | Positive parenting skills that are effective and sustainable can be applied for such encouragement and monitoring. | 6. | Program coordinator facilitates a kitchen activity with a healthy food item participants can prepare at home. (15) | ||
| 3 | Physical Activity Expectations | 1. | There is value in having a recreational home for Latino families, who report more inactivity than other groups. | 1. | Facilitator welcomes participants, and 1 small participant group facilitates a fun energizer physical activity. (10) |
| 2. | A community center can serve as such a home. | 2. | Facilitator reviews key messages and how participants were able to accomplish goals set in the previous session. (10) | ||
| 3. | Families receive a guided tour and hands-on orientation to the new and accessible state-of-the-art Coleman Community Center and its many uses. | 3. | Program coordinator defines the concept of energy balance, which is balancing the foods they eat and their activity levels (5) | ||
| 4. | Program coordinator and Coleman Community Center staff conduct a guided tour of the recreation center, its staff, and uses. (20) | ||||
| 4. | Free family memberships are provided for the year. | 5. | Participants work in small groups on a treasure hunt activity identifying staff, programs, materials, and uses of the Coleman Community Center for their families and applying parenting skills of stating expectations in advance and catch your child doing good. (15) | ||
| 6. | Program coordinator facilitates participants creating a parent–child activity contract with goal setting. (5) | ||||
| 7. | Program coordinator facilitates a kitchen activity with a healthy food item participants can prepare at home. (15) | ||||
| 4 | Group Physical Activity | 1. | Families can be active together if they are shown how. | 1. | Program coordinator welcomes participants, and 1 small participant group facilitates a fun energizer physical activity. (10) |
| 2. | Monitoring and encouraging physical activity is critical to good parenting. | 2. | Program coordinator reviews key messages and how participants were able to accomplish goals set in the previous session. (10) | ||
| 3. | Games, music, and dance (many from cultural traditions) provide a low-cost approach for families with children of different ages to be active together inside and outside. | 3. | Program coordinator presents on the relation between heart rate and physical activity. How do I know I am exercising enough or too much during aerobic activity? (20) | ||
| 4. | Participants work in small and whole group physical activities gauging their individual levels of physical exertion and applying parenting skills of stating expectations in advance and catch your child being good. (25) | ||||
| 5. | Program coordinator facilitates participants creating a parent–child activity contract with goal setting. (5) | ||||
| 6. | Program coordinator facilitates a kitchen activity with a healthy food item participants can prepare at home. (20) | ||||
| 5 | Reduction in Media Time | 1. | Excessive media time is harmful to children’s health. Consequences include poor school performance, attention deficit disorder, obesity, and diabetes. | 1. | Program coordinator welcomes participants, and 1 small participant group facilitates a fun energizer physical activity. (10) |
| 2. | Program coordinator reviews key messages and how participants were able to accomplish goals set in the previous session. (10) | ||||
| 2. | Setting appropriate limits is good parenting. | 3. | Program coordinator presents on the relation between media time and health outcomes. (10) | ||
| 3. | There are ways parents can evaluate the quality and age-appropriateness of media programming, self-monitor screen time, and enjoy alternatives. | 4. | Program coordinator presents on parenting skill of setting limited reasonable choices. (5) | ||
| 5. | Exercise physiologist presents on physical coordination (muscles, heart capacity, and flexibility): how to warm up and cool down, how to avoid dehydration, and how to avoid cramps. (15) | ||||
| 6. | Participants work in small and whole group physical activities building coordination (warming up, physical exertion, AND cooling down) using the parenting skills of setting limited reasonable choices on television viewing. (15) | ||||
| 7. | Program coordinator facilitates participants creating a parent–child activity contract with goal setting. (5) | ||||
| 8. | Program coordinator facilitates a kitchen activity with a healthy food item participants can prepare at home. (20) | ||||
| 6 | Family Meals | 1. | Food choices and the concept of portion size are introduced through the deeply rooted Latino tradition and memories of family gatherings. | 1. | Program coordinator welcomes participants, and 1 small participant group facilitates a fun energizer physical activity. (10) |
| 2. | Meal-planning and shopping strategies such as using a grocery list and not going hungry make possible eating healthy food on a budget. | 2. | Program coordinator reviews key messages and how participants were able to accomplish goals set in the previous session. (10) | ||
| 3. | Program coordinator presents on eating foods from each major food group daily in light of participants’ cherished memories of food choices and portion sizes at daily and special family gatherings. The influence of other family members at home on child-feeding practices is explored. Healthy meal planning and shopping on a budget is discussed along with templates for a grocery list and items to have at-hand regularly in the pantry. (25) | ||||
| 4. | Participants work in small and whole group in hands-on skills-building activities on preparing a budgeted grocery list accounting for all the food choices and portion sizes at daily family meals using the parenting skills of setting limited reasonable choices plus accounting for the influence of other family members on those choices. (20) | ||||
| 5. | Program coordinator facilitates participants creating a parent–child activity contract with goal setting. (5) | ||||
| 6. | Program coordinator facilitates a kitchen activity with a healthy food item participants can prepare at home. (20) | ||||
| 7. | The Ideal Pair | 1. | The nutritionally perfect pairing of rice and beans is discussed by remembering the age-old Latino custom of courting and meeting the perfect partner while promenading in the plaza. | 1. | Program coordinator welcomes participants, and 1 small participant group facilitates a fun energizer physical activity. (10) |
| 2. | Program coordinator reviews key messages and how participants were able to accomplish goals set in the previous session. (10) | ||||
| 3. | Program coordinator presents on eating food combinations in the Latino diet for good nutritional balance across the major food groups. (20) | ||||
| 4. | Participants work in small and whole group hands-on skills-building activities on making nutritional food pairings daily across the food groups using the parenting skills of setting limited reasonable choices. (20) | ||||
| 5. | Program coordinator facilitates participants creating a parent–child activity contract with goal setting. (5) | ||||
| 6. | Program coordinator facilitates a kitchen activity with a healthy food item participants can prepare at home. (25) | ||||
| 8 | Mid-day Snacks | 1. | The benefits of healthy snacking and activity breaks during the day to achieve energy balance are connected to the “merienda” time that is popular in many Latino homes. | 1. | Program coordinator welcomes participants, and 1 small participant group facilitates a fun energizer physical activity. (10) |
| 2. | Program coordinator reviews key messages and how participants were able to accomplish goals set in the previous session. (10) | ||||
| 2. | Portion size and drinks matter for healthy snacking: many think of la merienda as another meal and forget to include drinks in the snack choice (eg, 1 soft drink can have as many calories as a hamburger). | 3. | Program coordinator presents on taking time during the day to re-energize with food and physical activity in the midst of hectic lives and the abundance of tasty, inexpensive fast food offerings. (15) | ||
| 4. | Program coordinator presents on the parenting skill of using “when..., then...” statements. (5) | ||||
| 5. | Participants work in small and whole group hands-on skills-building activities applying the custom of “la merienda” and physical energizers they can incorporate into their daily family routines using the parenting skill of saying, “when... then...” (20) | ||||
| 3. | Fast food selection skills. For example, choosing a fast food option that offers grilled meat and fresh vegetables. | ||||
| 6. | Program coordinator facilitates participants creating a parent–child activity contract with goal setting. (5) | ||||
| 4. | Fast food selection offers an opportunity to build positive parenting skills setting appropriate limits and monitoring nutrition. | 7. | Program coordinator facilitates a kitchen activity with a healthy food item participants can prepare at home. (25) | ||
| 9 | Seeds of the Americas | 1. | Many foods such as tomatoes, corn, chocolate, and vanilla can be traced back to the ancient cultures of the Americas. | 1. | Program coordinator welcomes participants, and 1 small participant group facilitates a fun energizer physical activity. (10) |
| 2. | Program coordinator reviews key messages and how participants were able to accomplish goals set in the previous session. (10) | ||||
| 2. | Preparing food in traditional ways along with playtime physical activities can help achieve energy balance. | 3. | Program coordinator presents on foods, preparation methods, and games from a proud heritage of the Americas for energy balance. (20) | ||
| 4. | Participants work in small and whole group skills-building activities on food spices, preparation, and games from their Latin American heritage for everyday healthy food choices and activity using the parenting skill of saying, “when... then...” (20) | ||||
| 5. | Program coordinator facilitates participants creating a parent–child activity contract with goal setting. (5) | ||||
| 6. | Program coordinator facilitates a kitchen activity with a healthy food item participants can prepare at home. (25) | ||||
| 10 | The Harvest | 1. | Seasons often determine availability of certain foods and the level of physical activity possible at different times of the year. | 1. | Program coordinator welcomes participants, and 1 small participant group facilitates a fun energizer physical activity. (10) |
| 2. | Program coordinator reviews key messages and how participants were able to accomplish goals set in the previous session. (10) | ||||
| 2. | Latino culture and celebrations around harvest time and seasonal changes help convey key messages in this session. | 3. | Program coordinator presents on healthy food and activity choices and seasonal availability or conditions. Safe spaces are identified for indoor and outdoor seasonal fun. (20) | ||
| 4. | Participants work in small and whole group hands-on skills-building activities on food and activity choices appropriate for winter in the community using the parenting skill of saying, “when... then...” and identifying safe spaces for fun physical activity close to home. (20) | ||||
| 5. | Program coordinator facilitates participants creating a parent–child activity contract with goal setting. (5) | ||||
| 6. | Program coordinator facilitates a kitchen activity with a healthy food item participants can prepare at home. (25) | ||||
| 11 | Salsa and Flavor | 1. | This session introduces the use of herbs, spices, and marinades to increase flavor while cutting sodium, fat, and sugar in the preparation of food. | 1. | Program coordinator welcomes participants and 1 small participant group facilitates a fun energizer physical activity. (10) |
| 2. | Program coordinator reviews key messages and how participants were able to accomplish goals set in the previous session. (10) | ||||
| 2. | The use of salsa is an ancient practice with historical and present connections for keeping our children healthy. | 3. | Program coordinator discusses with participants their individual BMI measures, and then presents on the use of spices for creating healthier dishes. (20) | ||
| 4. | Participants work in small whole group hands-on skills-building activities on using spices to reduce sodium, fat, and sugar especially in traditional family recipes using 1 of the 4 parenting skills above. (20) | ||||
| 3. | BMI measures serve as 1 important health indicator regarding obesity. | 5. | Program coordinator facilitates participants creating a parent–child activity contract with goal setting. (5) | ||
| 6. | Program coordinator facilitates a kitchen activity with a healthy food item participants can prepare at home. (25) | ||||
| 12 | Holiday | 1. | Making healthy food choices, increasing the levels of activity, and hydration are an important and fun part of family meals and celebration that are popular with many Latinos. | 1. | Program coordinator welcomes participants, and 1 small participant group facilitates a fun energizer physical activity. (10) |
| 2. | Program coordinator reviews key messages and how participants were able to accomplish goals set in the previous session. (10) | ||||
| 2. | Healthy lifestyles and celebrations can go together. Dancing, singing, playing games, eating, and having fun at a fiesta can nourish body and spirit and make healthy lifestyles part of every family’s tradition. | 3. | Program coordinator presents on making healthy food and activity choices during family celebrations. (15) | ||
| 4. | Participants work in small and whole group hands-on skills-building activities to make family special celebrations physically active, fun and flavorful using 1 of the 4 parenting skill above. (15) | ||||
| 5. | Children present a dramatization on the food groups to their parents. (10) | ||||
| 6. | Program coordinator facilitates participants creating a parent–child activity contract with goal setting. (5) | ||||
| 7. | Program coordinator facilitates a kitchen activity with a healthy food item participants can prepare at home. (25) |
Footnotes
This trial has been registered at www.clinicaltrials.gov (identifier NCT00808431).
Dr Barkin was responsible for conceptualization and design of the study trial, analysis and interpretation of the data, drafting of the manuscript and critical revision of the manuscript for important intellectual content, obtaining funding, and supervision; Dr Gesell was responsible for conceptualization and design of the study trial, acquisition of the data, drafting of the manuscript, and critical revision of the manuscript for important intellectual content; Mr Po’e was responsible for critical revision of the manuscript for important intellectual content; Mr Escarfuller was responsible for critical revision of the manuscript for important intellectual content; and Dr Tempesti was responsible for statistical analysis, interpretation of the data, critical revision of the manuscript for important intellectual content, and technical support. Each of the authors had full access to all of the data.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by a Project Diabetes Implementation grant from the State of Tennessee (GR-09-25517-00) awarded to Dr Barkin and funds awarded to Dr Barkin from the Vanderbilt Clinical and Translational Science Award (National Center for Research Resources/National Institutes of Health) (1 UL1 RR024975). Dr Gesell was supported by the American Heart Association Clinical Research grant Program (09CRP2230246). None of the funders contributed to the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
References
- 1.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1(1):11–25 [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010;303(3):242–249 [DOI] [PubMed] [Google Scholar]
- 3.Taveras EM, Gillman MW, Kleinman K, Rich-Edwards JW, Rifas-Shiman SL. Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics. 2010;125(4):686–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9(5):474–488 [DOI] [PubMed] [Google Scholar]
- 5.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101(3 pt 2):539–549 [PubMed] [Google Scholar]
- 6.Birch LL, Fisher JO. Mothers' child-feeding practices influence daughters' eating and weight. Am J Clin Nutr. 2000;71(5):1054–1061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barker DJ, Osmond C, Forsén TJ, Kajantie E, Eriksson JG. Trajectories of growth among children who have coronary events as adults. N Engl J Med. 2005;353(17):1802–1809 [DOI] [PubMed] [Google Scholar]
- 8.Leunissen RW, Kerkhof GF, Stijnen T, Hokken-Koelega A. Timing and tempo of first-year rapid growth in relation to cardiovascular and metabolic risk profile in early adulthood. JAMA. 2009;301(21):2234–2242 [DOI] [PubMed] [Google Scholar]
- 9.Monasta L, Batty GD, Macaluso A, et al. Interventions for the prevention of overweight and obesity in preschool children: a systematic review of randomized controlled trials. Obes Rev. 2011;12(5):e107–e118 [DOI] [PubMed] [Google Scholar]
- 10.Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year follow-up of behavioral, family-based treatment for obese children. JAMA. 1990;264(19):2519–2523 [PubMed] [Google Scholar]
- 11.Huang TT, Drewnowski A, Kumanyika SK, Glass TA. A systems-oriented multilevel framework for addressing obesity in the 21st century. Prev Chronic Dis. 2009;6(3):A82 [PMC free article] [PubMed] [Google Scholar]
- 12.Institute of Medicine, Committee on Progress in Preventing Childhood Obesity. Progress in Preventing Childhood Obesity: How Do We Measure Up. Washington, DC: National Academies Press; September 2006
- 13.US Department of Health and Human Services. Strategic Plan for NIH Obesity Research. A Report of the NIH Obesity Research Task Force. Rockville, MD: National Institutes of Health; 2004
- 14.Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children Cochrane Database Syst Rev. 2005;(3):CD001871 [DOI] [PubMed] [Google Scholar]
- 15.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164 [DOI] [PubMed]
- 16.Mason HN, Crabtree V, Caudill P, Topp R. Childhood obesity: a transtheoretical case management approach. J Pediatr Nurs. 2008;23(5):337–344 [DOI] [PubMed] [Google Scholar]
- 17.National Latino Children's Institute. Healthy Lifestyles for Latino Families. Salsa, Sabor y Salud. Available at: www.nlci.org/salsa/indexSSS.htm. Accessed September 11, 2007
- 18.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379 [DOI] [PubMed] [Google Scholar]
- 19.Systems WL. Language is the key: a program for building language and literacy in early childhood. Available at: www.edgateway.net/cs/es/view/lwe/93615. Accessed October 1, 2009
- 20.Eakin EG, Bull SS, Riley K, Reeves MM, Gutierrez S, McLaughlin P. Recruitment and retention of Latinos in a primary care-based physical activity and diet trial: the Resources for Health study. Health Educ Res. 2007;22(3):361–371 [DOI] [PubMed] [Google Scholar]
- 21.Bellg AJ, Borrelli B, Resnick B, et al. Treatment Fidelity Workgroup of the NIH Behavior Change Consortium . Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443–451 [DOI] [PubMed] [Google Scholar]
- 22.Lohman TGRA, Martorell R, eds. Anthopometric Standardization Reference Manual. Champaign, IL: Human Kinetics; 1988 [Google Scholar]
- 23.Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr. 2005;59(3):419–425 [DOI] [PubMed] [Google Scholar]
- 24.The Children’s Hospital of Philadelphia. Body mass index and z-score calculation in children. Available at: http://stokes.chop.edu/web/zscore/. Accessed December 13, 2011
- 25.Barona A, Miller JA. Short acculturation scale for Hispanic youth (SASHY): a preliminary report. Hisp J Behav Sci. 1994;16:155–162 [Google Scholar]
- 26.Cohen J. A power primer. Psychol Bull. 1992;112(1):155–159 [DOI] [PubMed] [Google Scholar]
- 27.Hintze JL. PASS User's Guide: Pass 2005 Power Analysis and Sample Size for Windows. Kaysville, UT: NCSS Number Cruncher Statistical System; 2005 [Google Scholar]
- 28.Cohen J, Cohen P, West S, Aiken L. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. 3rd ed. Mahwah, NJ: Erlbaum; 2003
- 29.Chen JL, Weiss S, Heyman MB, Lustig RH. Efficacy of a child-centered and family-based program in promoting healthy weight and healthy behaviors in Chinese American children: a randomized controlled study. J Public Health (Oxf). 2010;32(2):219–229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Okely AD, Collins CE, Morgan PJ, et al. Multi-site randomized controlled trial of a child-centered physical activity program, a parent-centered dietary-modification program, or both in overweight children: the HIKCUPS study. J Pediatr. 2010;157(3):388–394, 394.e1 [DOI] [PubMed]
- 31.Magarey AM, Perry RA, Baur LA, et al. A parent-led family-focused treatment program for overweight children aged 5 to 9 years: the PEACH RCT. Pediatrics. 2011;127(2):214–222 [DOI] [PubMed] [Google Scholar]
- 32.Sacher PM, Kolotourou M, Chadwick PM, et al. Randomized controlled trial of the MEND program: a family-based community intervention for childhood obesity. Obesity (Silver Spring). 2010;18(suppl 1):S62–S68 [DOI] [PubMed] [Google Scholar]
- 33.Hesketh KD, Campbell KJ. Interventions to prevent obesity in 0-5 year olds: an updated systematic review of the literature. Obesity (Silver Spring). 2010;18(suppl 1):S27–S35 [DOI] [PubMed] [Google Scholar]
- 34.Stark LJ, Spear S, Boles R, et al. A pilot randomized controlled trial of a clinic and home-based behavioral intervention to decrease obesity in preschoolers. Obesity (Silver Spring). 2011;19(1):134–141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baker JL, Olsen LW, Sørensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357(23):2329–2337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Branscum P, Sharma M. A systematic analysis of childhood obesity prevention interventions targeting Hispanic children: lessons learned from the previous decade. Obes Rev. 2011;12(5):e151–e158 [DOI] [PubMed] [Google Scholar]
- 37.Guzmán A, Richardson IM, Gesell S, Barkin SL. Recruitment and retention of Latino children in a lifestyle intervention. Am J Health Behav. 2009;33(5):581–586 [PMC free article] [PubMed] [Google Scholar]
- 38.Olvera N, Bush JA, Sharma SV, Knox BB, Scherer RL, Butte NF. BOUNCE: a community-based mother-daughter healthy lifestyle intervention for low-income Latino families. Obesity (Silver Spring). 2010;18(suppl 1):S102–S104 [DOI] [PubMed] [Google Scholar]
- 39.Boutelle KN, Cafri G, Crow SJ. Parent Predictors of Child Weight Change in Family Based Behavioral Obesity Treatment. Obesity (Silver Spring). Feb 23 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Savoye M, Shaw M, Dziura J, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: a randomized controlled trial. JAMA. Jun 27 2007;297(24):2697–2704 [DOI] [PubMed] [Google Scholar]