Abstract
Background
Cardiac arrhythmias are cardiac rhythm disorders that comprise an important public health problem. Few prior studies have examined the association between ambient air pollution and arrhythmias in general populations in mainland China.
Methods
We performed a time-series analysis to investigate the short-term association between air pollution (particulate matter with an aerodynamic diameter less than 10 µm [PM10], sulfur dioxide [SO2], and nitrogen dioxide [NO2]) and outpatient visits for arrhythmia in Shanghai, China. We applied the over-dispersed Poisson generalized additive model to analyze the associations after control for seasonality, day of the week, and weather conditions. We then stratified the analyses by age, gender, and season.
Results
We identified a total of 56 940 outpatient visits for cardiac arrhythmia. A 10-µg/m3 increase in the present-day concentrations of PM10, SO2, and NO2 corresponded to increases of 0.56% (95% CI 0.42%, 0.70%), 2.07% (95% CI 1.49%, 2.64%), and 2.90% (95% CI 2.53%, 3.27%), respectively, in outpatient arrhythmia visits. The associations were stronger in older people (aged ≥65 years) and in females. This study provides the first evidence that ambient air pollution is significantly associated with increased risk of cardiac arrhythmia in mainland China.
Conclusions
Our analyses provide evidence that the current air pollution levels have an adverse effect on cardiovascular health and strengthened the rationale for further limiting air pollution levels in the city.
Key words: air pollution, outpatient visits, cardiac arrhythmias, time-series
INTRODUCTION
Epidemiologic studies have demonstrated associations between short-term increases in outdoor air pollution concentrations and adverse cardiovascular effects, including increased mortality and hospital visits for ischemia heart disease, heart failure, and sudden cardiac arrest.1 The underlying mechanisms remain unclear, but the cardiac autonomic nervous system may be largely involved.2
Cardiac arrhythmias are cardiac rhythm disorders that comprise an important public health problem.3 Cardiac arrhythmias are associated with increased risk of cardiovascular complications and sudden cardiac arrest (or death), consequently leading to decreased quality of life, disability, and high mortality risk and healthcare expense.3 Dozens of recent studies have suggested that particulate matter and other air pollutants might be responsible for cardiac arrhythmias. However, most of these results were obtained from small groups of subjects treated by implantable cardioverter defibrillators (ICD) and dynamic Holter electrocardiograms.4 Few epidemiologic studies in this area have been based on more widely generalizable populations. Furthermore, research has been conducted concerning the effects of outdoor air pollution on cardiac arrhythmias in mainland China where the air pollution levels are much higher than those in developed countries.
Therefore, we conducted a time-series analysis to examine the association between ambient air pollution and outpatient visits for cardiac arrhythmia in a general population of Shanghai, China.
METHODS
Data
The daily number of outpatient visits for cardiac arrhythmia from January 1, 2010, to December 31, 2011 (730 days), was obtained from Shanghai Yangpu District Central Hospital, also known as the Yangpu Hospital of Tongji University. As a major hospital located in the Yangpu District, which covers an area of 60 km2, the hospital provides medical services for approximately 1.3 million residents in and around this district. In recent years, the hospital had approximately 1.5 million outpatient and emergency room visits per year. In the outpatient department, the physicians must enter medical record data for each patient into the computer system. The information recorded includes individual characteristics (such as gender, age, and residence) as well as any diagnoses for the current visit. The diagnosis of cardiac arrhythmias is given by clinical physicians based on electrocardiogram criteria. In this study, to ensure accuracy of cardiac arrhythmia diagnosis, a statistical physician blinded to concentrations of pollutants was responsible for summarizing each day’s confirmed outpatient visits for cardiac arrhythmia, which excluded follow-up visits. Further, we also excluded a few patients from other districts (according to their recorded residency) in order to minimize the measurement error of air pollution exposure. Data were analyzed at the aggregate level, and no individual records/information for patients were used, so the study had a waiver of informed consent. Additionally, since no participants were contacted, written informed consent was not given by participants.
Daily 24-h air pollution concentrations, including particulate matter with an aerodynamic diameter less than 10 µm (PM10), sulfur dioxide (SO2), and nitrogen dioxide (NO2), were obtained from one state-owned air quality monitoring station located in the Yangpu District almost 2 km away from this hospital. According to Chinese government rules, the location of state-owned stations should not be in the direct vicinity of traffic or industrial sources. Methods based on tapered element oscillating microbalance, ultraviolet fluorescence, and chemiluminescence were used for the measurement of PM10, SO2, and NO2, respectively. To calculate the 24-h mean concentrations of PM10, SO2, and NO2, at least 75% of the 1-h values must have been available on that particular day.
To allow for adjustment for the potential confounding effects of weather on incidence of arrhythmias, daily 24-h mean temperature and relative humidity were obtained from the database of the Shanghai Meteorological Bureau.
Statistical analysis
We adopted time-series regression models to investigate the short-term associations between air pollution and outpatient arrhythmia visits.5 Specifically, we applied a generalized additive model (GAM) to analyze the data. Because daily outpatient visits typically followed an over-dispersed Poisson distribution, we used a quasi-Poisson regression in the GAM. Consistent with previous time-series studies, we determined the model specifications empirically. We incorporated several covariates in the GAM as follows: (1) a natural cubic smooth function of calendar time with 7 degrees of freedom (df) per year to exclude unmeasured long-term and seasonal trends; (2) natural smooth functions of the mean temperature (6 df) and the relative humidity (3 df) to control for the potential nonlinear confounding effects of weather conditions; and (3) an indicator variable for “day of the week” to adjust for the day-in-week variation of the outpatient visits. We checked the autocorrelations of residuals using partial auto-correlation functions (PACF) for the above basic model. Because most previous studies suggest that the detrimental effects of air pollution on arrhythmia were limited to the first 24 h,4 we introduced air pollutant concentrations at the concurrent day into the basic model.
We also explored the age, sex, and season-specific effects of air pollution on arrhythmias. We tested the statistical significance of differences between effect estimates of the strata of a potential effect modifier (eg the difference between females and males) by calculating the 95% confidence interval (CI) as , where and are the estimates for the two categories, and and are their respective standard errors. Regardless of significance, we also considered modification of effect by a factor of two or more to be important and worthy of attention.6 For example, we considered sex to be an important modifier if the between-sex differences of effect estimates were more than doubled.
To check the stability of our results, we used alternative lag days of 1, 2, and 02 (3-day moving average) in the models. As another sensitivity analysis, we fitted two-pollutant models after controlling for other pollutants.
The statistical tests were two-sided, and effects of P < 0.05 were considered statistically significant. All models were fitted using R software version 2.15.1 (The R Foundation for Statistical Computing, Vienna, Austria) with the “mgcv” package. Results are presented as the percentage of change in the number of daily outpatient arrhythmia visits per 10-µg/m3 increase in pollutant concentrations.
RESULTS
Table 1 summarizes the basic descriptive statistics of the study population and exposures. From 2010 to 2011 (730 days), a total of 56 940 outpatient visits for cardiac arrhythmia were identified. The annual mean average pollutant concentrations were 81 µg/m3 for PM10, 29 µg/m3 for SO2, and 54 µg/m3 for NO2. The annual average temperature and humidity were 17°C and 68%, respectively, reflecting the subtropical climate in Shanghai. Generally, both the outpatient visits and the air pollution levels were highest in cool seasons (see Table 1 and eTable 1), and PM10, SO2, and NO2 had moderate positive correlation coefficients with each other and were negatively weakly correlated with temperature and humidity (see eTable 2).
Table 1. Summary of descriptive statistics.
| Mean ± SD | Minimum | P25 | Median | P75 | Maximum | |
| Outpatient visits for arrhythmia (n) | 78 ± 53 | 1 | 39 | 75 | 110 | 315 |
| Age (y) | ||||||
| 0–65 | 34 ± 30 | 0 | 12 | 26 | 50 | 236 |
| 65< | 45 ± 36 | 0 | 18 | 39 | 63 | 246 |
| Gender (n) | ||||||
| Male | 36 ± 30 | 0 | 14 | 30 | 51 | 223 |
| Female | 43 ± 36 | 0 | 16 | 36 | 60 | 225 |
| Season (n) | ||||||
| Coola | 81 ± 54 | 0 | 41 | 78 | 112 | 291 |
| Warmb | 77 ± 53 | 0 | 38 | 72 | 109 | 315 |
| Air pollutants concentrations (24-h average, µg/m3) | ||||||
| PM10 | 81 ± 63 | 10 | 44 | 64 | 98 | 600 |
| SO2 | 29 ± 18 | 7 | 16 | 24 | 37 | 130 |
| NO2 | 54 ± 23 | 11 | 37 | 51 | 67 | 182 |
| Weather conditions (24-h average) | ||||||
| Temperature (°C) | 17 ± 9 | −2 | 9 | 18 | 25 | 36 |
| Humidity (%) | 68 ± 13 | 23 | 60 | 69 | 78 | 95 |
Abbreviations: SD, standard deviation; P (25), 25th percentile; P (75), 75th percentile; PM10, particulate matter with an aerodynamic diameter less than 10 µm; SO2, Sulfur dioxide; NO2, Nitrogen dioxide.
aCool season: from November to April.
bWarm season: from May to October.
After checking the PACF plots, we did not find any apparent autocorrelations of the model residual, suggesting that the basic model may be appropriate. Table 2 shows the effect estimates using different lag days. The estimates decreased heavily from lag day 0 to lag day 2. The concurrent day concentrations generated much larger estimates than those on lag day 1 or 2. The effect of PM10 concentration was limited within the concurrent day, but the effects of SO2 and NO2 concentrations remained significant at lag day 1. A 10-µg/m3 increase in the concurrent day concentrations of PM10, SO2, and NO2 corresponded to increases in outpatient arrhythmia visits of 0.56% (95% CI 0.42%, 0.70%), 2.07% (95% CI 1.49%, 2.64%), and 2.90% (95% CI 2.53%, 3.27%), respectively. Percent increase in number of daily outpatient visits for arrhythmia associated with per interquartile range increase in pollutant concentrations using different lag days is displayed in eTable 3.
Table 2. Percent increase in number of daily outpatient visits for arrhythmia associated with a 10-µg/m3 increase in pollutant concentrations using different lag days in single-pollutant models.
| Lag | PM10 | SO2 | NO2 |
| 0 | 0.56 (0.42, 0.70) | 2.07 (1.49, 2.64) | 2.90 (2.53, 3.27) |
| 1 | −0.11 (−0.25, 0.03) | 0.53 (0.01, 1.07) | 1.10 (0.72, 1.48) |
| 2 | −0.01 (−0.15, 0.13) | 0.23 (−0.29, 0.75) | 0.14 (−0.24, 0.51) |
| 02 | 0.18 (0.01, 0.35) | 1.27 (0.59, 1.95) | 2.27 (1.80, 2.74) |
Values are reported as means and 95% confidence intervals.
Abbreviations: Lag day 02, 3 day-moving average concentrations.
Table 3 shows analysis results stratified by age, gender, and season. We observed significantly stronger associations of air pollutants and outpatient visits for arrhythmias in people aged 65 years or older. The effect of NO2 and SO2 among females was significantly stronger than males. Air pollutant effects varied by season; the effect of PM10 was three times larger in cool periods, while the effect of SO2 was almost four times larger in warm periods.
Table 3. Age, gender and season-specific percent increase in number of daily outpatient visits for arrhythmia associated with a 10-µg/m3 increase in pollutant concentrations on the concurrent day (lag 0) in single-pollutant models.
| PM10 | NO2 | SO2 | |
| Age group | |||
| ≤65 years | −0.05 (−0.27, 0.18)* | 2.00 (1.43, 2.57)* | −1.11 (−2.23, 0.01)* |
| >65 years | 0.95 (0.78, 1.13)* | 3.52 (3.03, 4.00)* | 4.15 (3.42, 4.89)* |
| Sex | |||
| Male | 0.43 (0.23, 0.64) | 1.97 (1.42, 2.53)* | 1.38 (0.52, 2.25)* |
| Female | 0.67 (0.49, 0.86) | 3.69 (3.20, 4.18)* | 2.69 (1.92, 3.46)* |
| Season | |||
| Cool | 1.03 (0.84, 1.22)* | 2.55 (2.06, 3.05)* | 1.09 (0.42, 1.75)* |
| Warm | 0.33 (0.10, 0.56)* | 3.56 (2.95, 4.16)* | 4.03 (2.68, 5.39)* |
Values are reported as means and 95% confidence intervals.
*Significant between-group difference (P < 0.05).
Table 4 compares the results of the single-pollutant and two-pollutant models. The effect of PM10 decreased only slightly after controlling for SO2 but substantially and with loss of statistical significance after controlling for NO2. The effect of SO2 appeared to decrease after adjusting for the two other pollutants. The effect of NO2 remained robust even after adjustment for PM10 and SO2.
Table 4. Percent increase in number of daily outpatient visits for arrhythmia associated with a 10-µg/m3 increase in pollutant concentrations on the concurrent day (lag 0) using single and two-pollutant models.
| Model | Mean (95% CI) | |
| PM10 | Adjusted for SO2 | 0.41 (0.25, 0.58) |
| Adjusted for NO2 | −0.05 (−0.23, 0.13) | |
| SO2 | Adjusted for NO2 | −0.94 (−2.15, 0.27) |
| Adjusted for PM10 | 1.17 (0.51, 1.83) | |
| NO2 | Adjusted for SO2 | 4.39 (3.86, 4.92) |
| Adjusted for PM10 | 2.98 (2.52, 3.44) |
Values are reported as means and 95% confidence intervals.
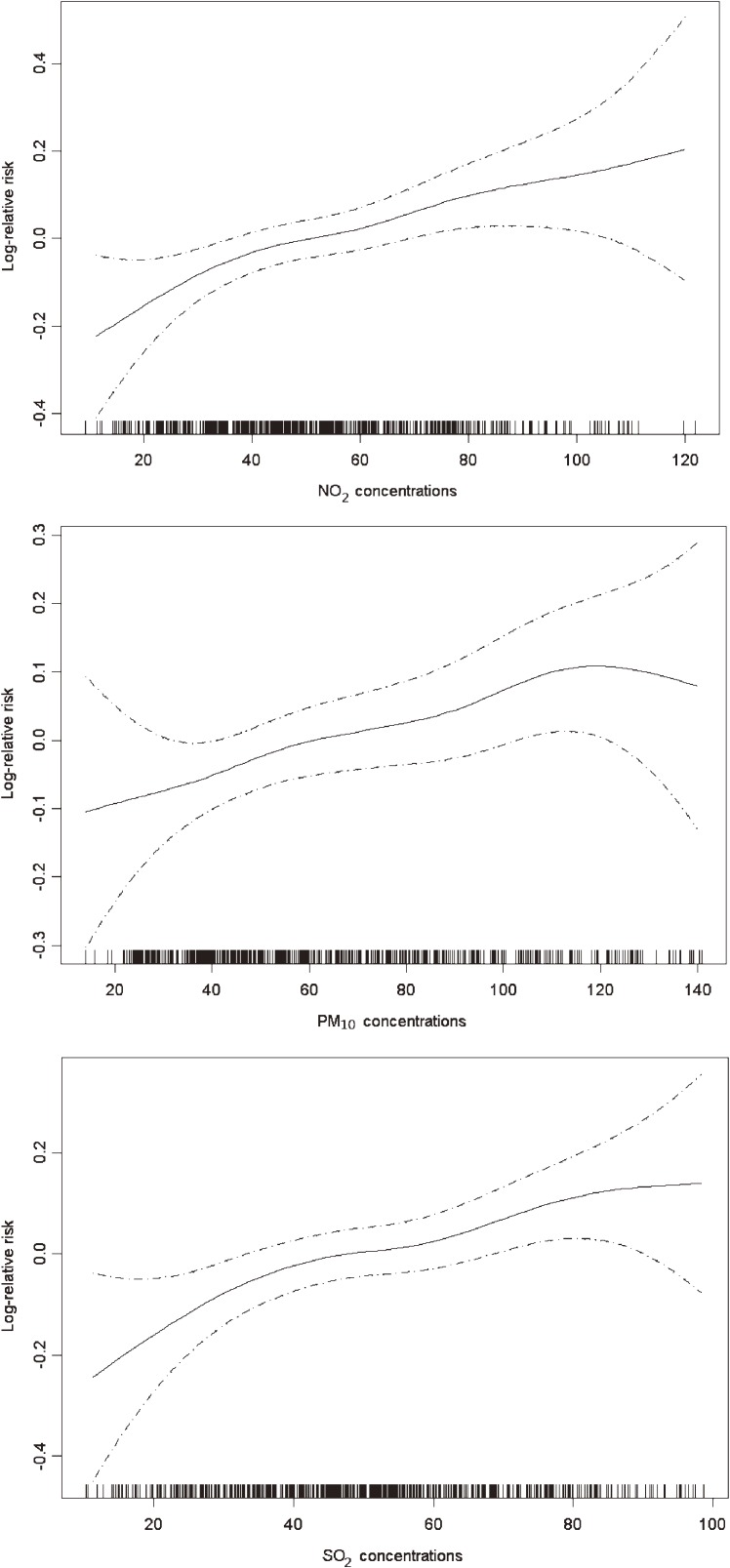
Figure depicts the unadjusted concentration-response relationships for PM10, SO2, and NO2 with outpatient visits for arrhythmia. The concentration-response relationships appeared to be linearly positive without any thresholds.
Figure. The concentration-response relationships of air pollutants and outpatient visits for arrhythmia. The X-axis is the pollutant concentrations (µg/m3) at the concurrent day. The Y-axis is the log-relative risk of outpatient visits for arrhythmia. The solid lines indicate the estimated mean change in the log-relative risk and the dotted lines represent the 95% confidence intervals of the estimates. The relative risk is expressed as the risk of outpatient visits for arrhythmia for certain concentrations of a pollutant compared to risk at its median concentration.
DISCUSSION
In the present study, we found that increased concentrations of outdoor air pollutants were associated with increased outpatient visits for cardiac arrhythmia in a general population of Shanghai, China. These effects remained significant after using alternative lag selection and controlling for co-pollutants. To our knowledge, this is one of a small number of studies worldwide that have examined the association between air pollution and cardiac arrhythmias in general populations. Our findings could arouse public health concern about the adverse impact of air pollution on heart rhythms in China.
Our results are supported by those of previous epidemiologic studies. Most previous studies linking air pollution and arrhythmia were conducted in a small group of subjects who experienced repeated measures of heart rhythm events recorded using ICDs or Holter electrocardiograms, but the results were inconsistent.4 For example, Link et al found that PM10 was associated with increased risk of atrial fibrillation onset within hours following exposure in 49 patients with ICDs.7 Rich et al also suggested an increased risk of episodes of rapid ventricular response due to paroxysmal atrial fibrillation in the hour after exposure to ambient ozone.8 In several ICD-based studies, ventricular arrhythmia was also found to be triggered by air pollution exposure within 1 or 2 days.9–11 However, despite these findings, other studies have suggested insignificant associations between arrhythmia and air pollution.12,13 The Holter-based studies somewhat consistently reported significant adverse effects of air pollution within hours of exposure on ventricular repolarization,14 premature ventricular contractions,15 parameters of heart rate variation,16 and ST segment height.17
Our findings are also consistent with previous time-series or case-crossover studies using aggregate data, although this type of evidence was scarce. A time-series study in Sao Paulo, Brazil, found that concurrent-day concentrations of PM10, NO2, and carbon monoxide (CO) significantly influenced arrhythmia emergency room visits.18 Another time-series study in Helsinki, Finland, by Halonen et al also suggested a significant association between present-day PM2.5 and hospital admissions for arrhythmia.19 Two case-crossover studies in Taiwan found that PM2.5, NO2, CO, and ozone levels on lag day 0 were associated with increased numbers of emergency room visits for cardiac arrhythmia.20,21 Gerard et al found a significant association between air pollution and daily mortality caused by arrhythmia.22
Few studies examined age, sex, and season-specific effects of air pollution on arrhythmia. We found that the association between air pollution and arrhythmia in elderly participants aged 65 years or more was stronger than in younger subjects. It is plausible that older people have higher prevalence of chronic cardiopulmonary diseases and thus are more susceptible to the harmful effects of air pollution. The reasons for the observation of a larger effect in females than in males are complex and might be attributable to females’ relatively frail physique, greater deposition of air pollutants in the lungs higher airway responsiveness, and the generally unfavorable socioeconomic status of females in China.23,24 A number of previous air pollution epidemiologic studies have shown that females were slightly more sensitive to the detrimental effects of air pollution. Season is also an important factor that can modify the health effects of air pollution because of variations in air pollution content and levels and population exposure patterns.24 We found a stronger association between NO2 and PM10 and cardiac arrhythmias in the cool season but a larger effect of SO2 in the warm season. Further studies are needed to clarify this issue.
Our analyses indicate that gaseous pollutants, especially NO2, had larger and more robust effects on outpatient visits for arrhythmia than other pollutants, suggesting that more concern should be directed toward gaseous pollutants in terms of both future health studies and pollution control. The shapes of the concentration-response relationships are crucial for public health assessment, and there has been a growing demand for accurate curves. In the present study, we found that the relationship curves were almost linearly positive. Therefore, the current air quality standards (150 µg/m3, 150 µg/m3, and 80 µg/m3 for daily average concentrations of PM10, SO2, and NO2, respectively) might not be sufficient to ensure public health protection in Shanghai, and further control of air pollution is likely to improve health benefits.
Our study has two main strengths. First, our study is the first to explore the link between air pollutants and cardiac arrhythmias in China, where air pollution levels are very high. Second, compared to most previous studies in this area that focused on a small, select population of patients, our study examined associations in a relatively large general population in Shanghai.
Nevertheless, limitations should also be addressed. As in most previous time-series studies, we utilized measurements on a fixed-site monitoring station as a proxy for the population exposure level to air pollution. This might raise a number of issues, given that the ambient monitoring results may differ from the level of personal exposure to air pollutants, as people typically spend most of their time indoors.25 However, this measurement error would generally tend to bias estimates toward the null.26 We selected a central site for air quality monitoring in the same district as the hospital so we believe this measurement error may not be very large. Second, our health data were collected from only a single hospital, which may not represent the situation in the whole city. We were not able to obtain classification data for arrhythmia, thus limiting our ability to identify subgroups susceptible to air pollution exposure. Therefore, further studies on the association between air pollution and arrhythmia are needed.
CONCLUSIONS
This time-series study found that air pollution might contribute to the increased number of outpatient visits for cardiac arrhythmia in Shanghai, China. Our results provide the first evidence that ambient air pollution is significantly associated with increased risks of cardiac arrhythmia in mainland China. Our findings might help local decision-makers establish air pollution control measures. Further large-scale studies are needed to confirm our results.
ONLINE ONLY MATERIALS
ACKNOWLEDGMENTS
The study was supported by the National Basic Research Program (973 program) of China (2011CB503802), Gong-Yi Program of China Ministry of Environmental Protection (201209008), and the National Natural Science Foundation of China (81222036).
Conflicts of interest: The authors declare that they have no competing financial interests.
REFERENCES
- 1.Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, et al. . Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–78 10.1161/CIR.0b013e3181dbece1 [DOI] [PubMed] [Google Scholar]
- 2.Tan AY, Verrier RL. The role of the autonomic nervous system in cardiac arrhythmias. Handb Clin Neurol. 2013;117:135–45 10.1016/B978-0-444-53491-0.00012-2 [DOI] [PubMed] [Google Scholar]
- 3.Murakoshi N, Aonuma K. Epidemiology of arrhythmias and sudden cardiac death in Asia. Circ J. 2013;77:2419–31 10.1253/circj.CJ-13-1129 [DOI] [PubMed] [Google Scholar]
- 4.Link MS, Dockery DW. Air pollution and the triggering of cardiac arrhythmias. Curr Opin Cardiol. 2010;25:16–22 10.1097/HCO.0b013e32833358cd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peng RD, Dominici F, Louis TA. Model choice in time series studies of air pollution and mortality. J R Stat Soc Ser A Stat Soc. 2006;169:179–203 10.1111/j.1467-985X.2006.00410.x [DOI] [Google Scholar]
- 6.Chen R, Kan H, Chen B, Huang W, Bai Z, Song G, et al. . Association of particulate air pollution with daily mortality: the China Air Pollution and Health Effects Study. Am J Epidemiol. 2012;175:1173–81 10.1093/aje/kwr425 [DOI] [PubMed] [Google Scholar]
- 7.Link MS, Luttmann-Gibson H, Schwartz J, Mittleman MA, Wessler B, Gold DR, et al. . Acute exposure to air pollution triggers atrial fibrillation. J Am Coll Cardiol. 2013;62:816–25 10.1016/j.jacc.2013.05.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rich DQ, Mittleman MA, Link MS, Schwartz J, Luttmann-Gibson H, Catalano PJ, et al. . Increased risk of paroxysmal atrial fibrillation episodes associated with acute increases in ambient air pollution. Environ Health Perspect. 2006;114:120–3 10.1289/ehp.8371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dockery DW, Luttmann-Gibson H, Rich DQ, Link MS, Mittleman MA, Gold DR, et al. . Association of air pollution with increased incidence of ventricular tachyarrhythmias recorded by implanted cardioverter defibrillators. Environ Health Perspect. 2005;113:670–4 10.1289/ehp.7767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rich DQ, Schwartz J, Mittleman MA, Link M, Luttmann-Gibson H, Catalano PJ, et al. . Association of short-term ambient air pollution concentrations and ventricular arrhythmias. Am J Epidemiol. 2005;161:1123–32 10.1093/aje/kwi143 [DOI] [PubMed] [Google Scholar]
- 11.Rich DQ, Kim MH, Turner JR, Mittleman MA, Schwartz J, Catalano PJ, et al. . Association of ventricular arrhythmias detected by implantable cardioverter defibrillator and ambient air pollutants in the St Louis, Missouri metropolitan area. Occup Environ Med. 2006;63:591–6 10.1136/oem.2005.023457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson HR, Armstrong B, Hajat S, Harrison R, Monk V, Poloniecki J, et al. . Air pollution and activation of implantable cardioverter defibrillators in London. Epidemiology. 2010;21:405–13 10.1097/EDE.0b013e3181d61600 [DOI] [PubMed] [Google Scholar]
- 13.Metzger KB, Klein M, Flanders WD, Peel JL, Mulholland JA, Langberg JJ, et al. . Ambient air pollution and cardiac arrhythmias in patients with implantable defibrillators. Epidemiology. 2007;18:585–92 10.1097/EDE.0b013e318124ff0e [DOI] [PubMed] [Google Scholar]
- 14.Liao D, Shaffer ML, Rodriguez-Colon S, He F, Li X, Wolbrette DL, et al. . Acute adverse effects of fine particulate air pollution on ventricular repolarization. Environ Health Perspect. 2010;118:1010–5 10.1289/ehp.0901648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.He F, Shaffer ML, Rodriguez-Colon S, Yanosky JD, Bixler E, Cascio WE, et al. . Acute effects of fine particulate air pollution on cardiac arrhythmia: the APACR study. Environ Health Perspect. 2011;119:927–32 10.1289/ehp.1002640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zanobetti A, Gold DR, Stone PH, Suh HH, Schwartz J, Coull BA, et al. . Reduction in heart rate variability with traffic and air pollution in patients with coronary artery disease. Environ Health Perspect. 2010;118:324–30 10.1289/ehp.0901003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chuang KJ, Coull BA, Zanobetti A, Suh H, Schwartz J, Stone PH, et al. . Particulate air pollution as a risk factor for ST-segment depression in patients with coronary artery disease. Circulation. 2008;118:1314–20 10.1161/CIRCULATIONAHA.108.765669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Santos UP, Terra-Filho M, Lin CA, Pereira LA, Vieira TC, Saldiva PH, et al. . Cardiac arrhythmia emergency room visits and environmental air pollution in Sao Paulo, Brazil. J Epidemiol Community Health. 2008;62:267–72 10.1136/jech.2006.058123 [DOI] [PubMed] [Google Scholar]
- 19.Halonen JI, Lanki T, Yli-Tuomi T, Tiittanen P, Kulmala M, Pekkanen J. Particulate air pollution and acute cardiorespiratory hospital admissions and mortality among the elderly. Epidemiology. 2009;20:143–53 10.1097/EDE.0b013e31818c7237 [DOI] [PubMed] [Google Scholar]
- 20.Tsai SS, Chiu HF, Wu TN, Yang CY. Air pollution and emergency room visits for cardiac arrhythmia in a subtropical city: Taipei, Taiwan. Inhal Toxicol. 2009;21:1113–8 10.3109/08958370902758939 [DOI] [PubMed] [Google Scholar]
- 21.Chiu HF, Tsai SS, Weng HH, Yang CY. Short-term effects of fine particulate air pollution on emergency room visits for cardiac arrhythmias: a case-crossover study in Taipei. J Toxicol Environ Health A. 2013;76:614–23 10.1080/15287394.2013.801763 [DOI] [PubMed] [Google Scholar]
- 22.Hoek G, Brunekreef B, Fischer P, van Wijnen J. The association between air pollution and heart failure, arrhythmia, embolism, thrombosis, and other cardiovascular causes of death in a time series study. Epidemiology. 2001;12:355–7 10.1097/00001648-200105000-00017 [DOI] [PubMed] [Google Scholar]
- 23.Gowd BM, Thompson PD. Effect of female sex on cardiac arrhythmias. Cardiol Rev. 2012;20:297–303 10.1097/CRD.0b013e318259294b [DOI] [PubMed] [Google Scholar]
- 24.Kan H, London SJ, Chen G, Zhang Y, Song G, Zhao N, et al. . Season, sex, age, and education as modifiers of the effects of outdoor air pollution on daily mortality in Shanghai, China: The Public Health and Air Pollution in Asia (PAPA) Study. Environ Health Perspect. 2008;116:1183–8 10.1289/ehp.10851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sarnat JA, Brown KW, Schwartz J, Coull BA, Koutrakis P. Ambient gas concentrations and personal particulate matter exposures: implications for studying the health effects of particles. Epidemiology. 2005;16:385–95 10.1097/01.ede.0000155505.04775.33 [DOI] [PubMed] [Google Scholar]
- 26.Zeger SL, Thomas D, Dominici F, Samet JM, Schwartz J, Dockery D, et al. . Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect. 2000;108:419–26 10.1289/ehp.00108419 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.