Abstract
OBJECTIVE:
To describe variation across selected US children’s hospitals in screening for occult fractures in children <2 years old diagnosed with physical abuse and in infants <1 year old who have injuries associated with a high likelihood of physical abuse.
METHODS:
We performed a retrospective study of children <2 years old with a diagnosis of physical abuse and infants <1 year old with non-motor vehicle crash–associated traumatic brain injuries or femur fractures admitted to 40 hospitals within the Pediatric Hospital Information System database from January 1, 1999, to December 31, 2009. We examined variation among the hospitals in the performance of screening for occult fractures as defined by receipt of skeletal survey or radionuclide bone scan. Marginal standardization implemented with logistic regression analysis was used to examine hospital variation after adjusting for patient demographic characteristics, injury severity, and year of admission.
RESULTS:
Screening for occult fractures was performed in 83% of the 10 170 children <2 years old with a diagnosis of physical abuse, 68% of the 9942 infants who had a traumatic brain injury, and 77% of the 2975 infants who had femur fractures. After adjustment for patient characteristics, injury severity, and year of admission, hospitals varied significantly in use of screening for occult fractures in all 3 groups of children.
CONCLUSIONS:
The observed variation in screening for occult fractures in young victims of physical abuse and infants who have injuries associated with a high likelihood of abuse underscores opportunities to improve the quality of care provided to this vulnerable population.
KEY WORDS: child abuse, child maltreatment, femur fracture, traumatic brain injury
What’s Known on This Subject:
Clinical guidelines for the evaluation of suspected physical abuse in young children emphasize performing radiologic imaging to screen for occult fractures. Little is known about the degree of adherence to guidelines for screening for occult fractures among pediatric hospitals.
What This Study Adds:
Adherence to guidelines related to screening for occult fractures in young children diagnosed with physical abuse varies significantly among pediatric hospitals. Use of screening in infants who have injuries associated with a high likelihood of abuse also varies among pediatric hospitals.
Young victims of physical abuse frequently have occult injuries that are not suspected on history or physical examination but are revealed on screening radiologic studies.1–10 Occult fractures, the most common type of occult injury, are identified on skeletal surveys in approximately one-third of physical abuse victims <2 years old.5,8,9,11 Although the majority of fractures discovered on skeletal surveys do not require medical intervention, they are important to the medical and legal evaluation of physical abuse.1 Identifying patterns of fractures characteristic of inflicted trauma can provide additional data needed to confirm abuse and enable child protective services to better serve the child. Dating of the fractures can provide information regarding timing of injuries and aid in identifying assailants.1
In addition to using skeletal surveys to identify fractures in children who have injuries that clearly result from abuse, clinicians use skeletal survey data to determine the level of concern for abuse in young children presenting for evaluation of injuries with unclear etiology.10 Accurately distinguishing abusive from accidental injuries in preverbal children is critical to their safety but can be challenging due to potential unreliability of caregiver histories and limitations of physical examination in this population. Failure of medical providers to recognize and diagnose abuse can result in children suffering complications from undiagnosed injuries and ongoing abuse that can lead to further injuries and death.12–17 Thus, a thorough medical evaluation should be performed in young children with injuries suspicious for abuse.2
Recognizing the importance of screening for occult fractures, the American Academy of Pediatrics recommends performing a skeletal survey in all cases of suspected physical abuse in children <2 years old.1,2 Little is known, however, about the interpretation of these guidelines. The term “suspected” is not defined and might be interpreted differently by clinicians based on medical training, experiences, perceptions of the likelihood of abuse, and relative risks and benefits of skeletal surveys.10 In addition, the availability to consult with child abuse specialists at an institution might influence screening rates in young injured children. Many children’s hospitals have developed specialized child abuse services; the structure and function of these services, however, vary across hospitals, and their impact on the care provided to victims has not been evaluated.18–21
Although previous studies have examined factors influencing the clinical decision to diagnose abuse,22–26 less is known about variation in screening practices for occult fractures. Limited data regarding the use of skeletal surveys reveal disparities in the frequency of performing screening based on race and socioeconomic status (SES).27–30 Small retrospective reviews and case series also raise concern about missed opportunities to evaluate for abuse.12–16
Given concerns about variation in screening for occult fractures and the lack of data regarding this practice, we examined patterns of use of screening radiologic studies for occult fractures in children <2 years old diagnosed with physical abuse at pediatric hospitals. Building on recent work regarding disparities in evaluation for abuse among infants,29,31 we also examined screening practices in infants <1 year old who had femur fractures or traumatic brain injury (TBI) that were not attributed to a motor vehicle crash. These serious injuries in infants have been associated with a high likelihood of abuse, but there are no clear guidelines or consensus regarding screening in this population. Finally, we examined whether the type of child abuse services available at a hospital was associated with rates of screening for occult fractures.
Methods
Data Source
We used the Pediatric Health Information System (PHIS), a database of coded diagnostic data from 43 not-for-profit, tertiary care pediatric hospitals in the United States.32 These hospitals are affiliated with Child Health Corporation of America (Shawnee Mission, KS), a business alliance of freestanding children’s hospitals. Contributing hospitals are located in 17 of the 20 major metropolitan areas and represent 85% of freestanding children’s hospitals in the United States. Hospitals submit discharge/encounter data, including demographic characteristics, diagnoses, and procedures, as well as resource utilization data, to PHIS. Through a joint effort between Child Health Corporation of America, Thomson Reuters (Ann Arbor, MI), and participating hospitals, data are subjected to reliability and validity checks before inclusion in PHIS. Various peer-reviewed publications have used PHIS to examine variation in care.33–38 We used data from 40 hospitals located in 24 states and the District of Columbia, which contributed inpatient data for at least a 3-year portion of the study period (January 1, 1999–December 31, 2009). Only inpatient cases that contained procedure and/or billing codes were included because these codes provide information about the type and timing of radiologic studies.
Information regarding the type of child abuse services at PHIS hospitals was obtained from a survey conducted by the National Association of Children’s Hospitals and Related Institutions (NACHRI) in 2008.20 Survey respondents categorized their hospital’s services as 1 of 4 levels based on NACHRI definitions: (1) no services; (2) child abuse services; (3) child abuse team; or (4) child abuse programs. Hospitals with no services refer all suspected cases to other health care institutions whereas hospitals that do have child abuse services provide clinical response to all forms of child maltreatment. To be categorized as having a child abuse team, hospitals must have a dedicated, recognizable team that provides medical, referral, and diagnostic services for child maltreatment and includes a pediatrician, administrative coordinator trained in the field of child abuse, and social work services. Hospitals with child abuse programs have an administrative unit with centralized management that provides assessment, referral and diagnostic services for all forms of maltreatment, and acts as the coordinating entity that connects community agencies involved in child protection with hospital staff and subspecialty services.20
Study Population
The 2 study populations were: (1) children <2 years old who had a diagnosis of physical abuse; and (2) infants who had serious injuries that are frequently attributed to physical abuse. The physical abuse group included children with a diagnosis of physical abuse or assault (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] 995.50, 995.54, 995.55 995.59, E960–E967, E968.0–E968.3, and E968.5–E968.9). The infant population included 2 subgroups: infants with TBI and infants with femur fractures. The TBI group included infants <1 year old with a diagnosis of TBI (ICD-9-CM 800–801, 803–804, or 851–853) in any of the 21 diagnosis fields in the PHIS database. Infants with only skull fractures or concussions (ICD-9-CM 800.0, 800.5, 801.0 801.5, 803.0, 803.5, 804.0, 804.5, 850, or 854) were excluded because the likelihood of abuse and occult fractures is lower among this group than among infants with more severe head injuries.27,39,40 The femur fracture group included infants <1 year old with a diagnosis of femur fracture (ICD-9-CM 820–821). Given our focus on potential victims of abuse, children with an E-code for transportation accidents (E800–E848) were excluded, as were infants hospitalized following birth. Infants with a diagnosis of brain or lower extremity neoplasm (ICD-9-CM 191.0–191.9 or 170.7) that might have resulted in pathologic fractures or intracranial bleeding were excluded from the infant groups. Infants with a diagnosis of both TBI and femur fracture were categorized into the TBI or femur fracture group based on which injury was imaged first. Infants in the TBI and femur groups could also be included in the physical abuse group.
Study Outcomes
The primary outcome was the performance of screening for occult fractures as determined by the presence of a procedure and/or billing code for a skeletal survey or radionuclide bone scan. In most cases, a skeletal survey is the preferred test for occult fractures but in select cases, radionuclide bone scans can serve as an alternative screening test.1
Data Analysis
For each study group (physical abuse, infant TBI, and infant femur), the unadjusted rate of screening for occult fractures was determined for each hospital. Next, we used data on patient demographic characteristics, injury severity, and year of admission to assess how much of the observed variation in screening among infants with TBI and infants with femur fractures can be attributed to differences in case-mix across hospitals and to changes over time. Patient demographic characteristics and injury severity have been associated with likelihood of skeletal survey performance in other studies.28,29 Demographic variables included age in months as a continuous variable, gender, race, and Medicaid status. Injury severity scores were calculated by using ICDMAP-90 injury diagnosis coding software (The Johns Hopkins University [Baltimore, MD] and Tri-Analytics, Inc [Ponte Vedra Beach, FL]). An ICD-9-CM–based Abbreviated Injury Score (ICD/AIS) that only considered injuries for the head region was calculated for the TBI group and a score that only considered lower extremity injuries was calculated for the femur group. Hospitals were compared by using marginal standardization methods implemented in logistic regression. This method uses the entire sample as the standard population and estimates the proportion of children who received screening for occult fractures by assuming that children were alternatively admitted to each hospital. This method for adjusted analysis has a history of use in survey research.41,42 Because American Academy of Pediatrics guidelines recommend screening for occult fractures in all children <2 years old with a diagnosis of physical abuse regardless of patient demographic and injury characteristics, no adjustment for hospital case-mix was performed for the physical abuse group.
Next, the association between the category of child abuse services available at the hospital and the rate of performance of screening for occult fractures in children diagnosed with physical abuse was analyzed by using logistic regression with variances and confidence intervals (CIs) adjusted for correlation within hospitals.43,44 A nonparametric test for trends was performed to test for changes over time in rates of screening in children diagnosed with physical abuse. Analyses were completed in Stata version 11.1 (Stata Corp, College Station, TX).
Results
Study Population
Across the 40 hospitals, 10 170 children <2 years old were diagnosed with physical abuse. Of the 12 980 infants identified with high-risk injuries for child abuse, 74% had TBI, 23% had femur fractures, and 3% had femur fractures and TBI. Of the 384 infants with both TBI and femur fractures, 359 were categorized as TBI or femur fracture based on which injury was imaged first, and 63 were excluded due to undetermined timing of imaging. The final high-risk TBI group included 9942 infants and the high-risk femur fracture group included 2975 infants.
Information regarding the type of child abuse services in 2008 was identified for 22 of the 40 hospitals; 19 hospitals had a comprehensive child abuse program with centralized administration and 3 had less formalized but dedicated child abuse teams.
Screening for Occult Fractures in Children Diagnosed With Physical Abuse
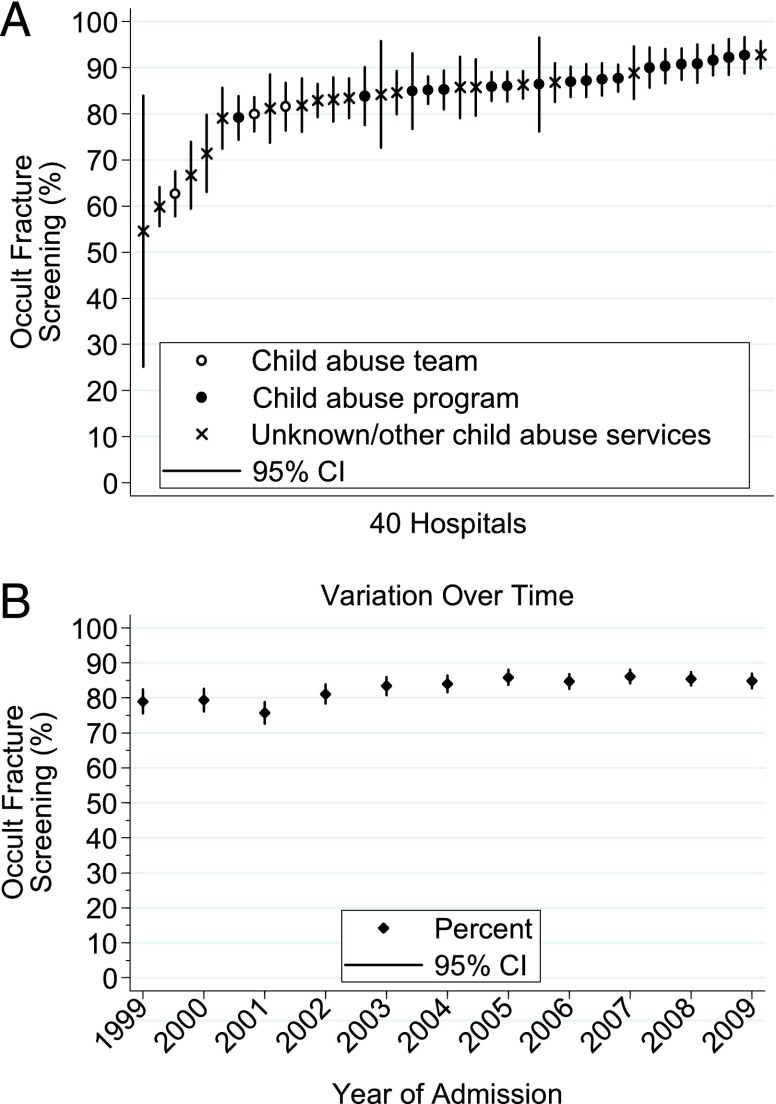
Screening was performed in 83% of children <2 years old diagnosed with physical abuse (Table 1). The rate of screening varied significantly across the 40 hospitals, from 55% (95% CI: 24–85) to 93% (95% CI: 89–97) (P < .001) and increased over time, from 79% (95% CI: 76–82) in 1999 to 85% (95% CI: 83–87) in 2009 (P < .001) (Fig 1).
TABLE 1.
Characteristics of Children Aged <2 Years Diagnosed With Physical Abuse and Infants Aged <1 Year Who Had TBI or Femur Fractures
| Characteristic | Physical Abuse (n = 10 170) | High-Risk Injury Infant Groups (n = 12 980) | ||
|---|---|---|---|---|
| TBI (n = 9942) | Femur Fracture (n = 2975) | Excludeda (n = 63) | ||
| Median age (range), mo | 4 (0–23) | 3 (0–11) | 4 (0–11) | 3 (0–10) |
| Race, % | ||||
| White | 75 | 78 | 75 | 63 |
| Black | 18 | 13 | 18 | 33 |
| Other/unknown | 7 | 9 | 7 | 3 |
| Payer, % | ||||
| Medicaid/self-pay | 72 | 60 | 62 | 57 |
| Private insurance | 11 | 21 | 19 | 16 |
| Other/unknown | 17 | 19 | 19 | 27 |
| Gender, % | ||||
| Female | 27 | 28 | 30 | 30 |
| Male | 72 | 72 | 69 | 68 |
| Unknown | <1 | <1 | 1 | 2 |
| Injury severity score, %b | ||||
| Mild | NA | 1 | 96 | NA |
| Moderate | NA | 6 | 4 | NA |
| Severe | NA | 92 | <1 | NA |
| Unknown | NA | 1 | <1 | NA |
| Screened for occult fractures, % | 83 | 68 | 77 | 84 |
| Diagnosis of physical abuse, % | 100 | 40 | 35 | 59 |
| Died, % | 6 | 5 | 1 | 5 |
Sixty-three infants with both TBI and femur fractures were excluded due to undetermined timing of imaging.
Injury severity scores were categorized as mild (1–2), moderate (3), or severe (4–6). Scores for the head region ranged from 1 to 6; scores for the lower extremities ranged from 1 to 4.
FIGURE 1.
Variation in screening for occult fractures in young children diagnosed with physical abuse (A) across hospitals and (B) over time. The type of child abuse services is based on a survey conducted by NACHRI in 2008 that categorized services available for 22 of 40 hospitals: (1) no services; (2) child abuse services; (3) child abuse team; or (4) child abuse programs.19 All remaining hospitals were included in unknown/other category.
The presence of a comprehensive child abuse program (n = 19) in 2008 versus a child abuse team (n = 3) was associated with increased screening for occult fractures (odds ratio [OR]: 2.42 [95% CI: 1.41–4.16], P = .001) during the 10-year study period. The likelihood of screening was higher at hospitals with child abuse programs than at hospitals with unknown/other types of services (OR: 1.67 [95% CI: 1.10–2.53], P = .02). Limiting analyses to 2007 to 2009 produced similar results, with higher odds of screening at hospitals with child abuse programs than at hospitals with child abuse teams (OR: 2.23 [95% CI: 1.57–3.16], P < .001) and hospitals with unknown/other types of services (OR: 1.62 [95% CI: 1.07–2.44], P = .02).
Screening for Occult Fractures in Infants With High-Risk Injuries
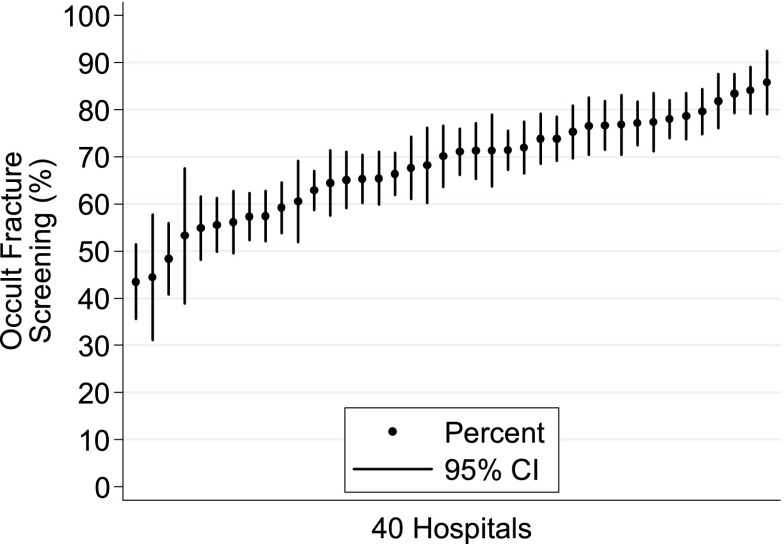
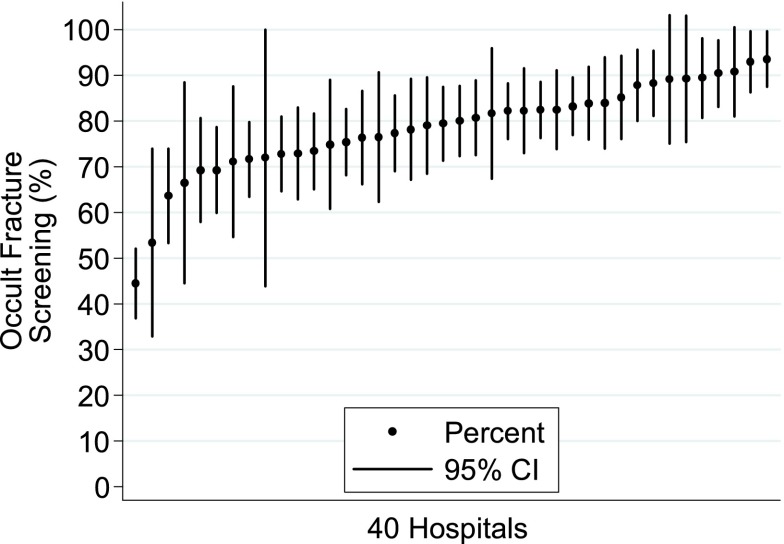
Screening was performed in 68% (95% CI: 68–69) of infants who had TBI and 77% (95% CI: 76–79) of infants with femur fractures. Variation in screening across hospitals was significant among both groups (P < .001). Unadjusted rates of screening at hospitals varied from 38% (95% CI: 30–45) to 88% (95% CI: 82–94) among infants with TBI and from 41% (95% CI: 33–48) to 94% (95% CI: 88–100) among infants with femur fractures. After adjustment for patient demographic characteristics, injury severity, and year of admission, there was still significant variation in the proportion of infants with TBI and femur fractures who had screening for occult fractures (P < .001). After adjustment, screening ranged from 44% (95% CI: 36–51) to 86% (95% CI: 79–93) for infants who had TBI and from 44% (95% CI: 37–52) to 94% (95% CI: 87– 100) for infants who had femur fractures (Figs 2 and 3).
FIGURE 2.
Variation in screening for occult fractures in infants who had TBI. Results were generated from logistic regression analysis using marginal standardization, adjusting for age, insurance, gender, year of admission, and severity of TBI based on the ICD-9-CM/AIS score for the head region.
FIGURE 3.
Variation in screening for occult fractures in infants who had femur fractures. Results were generated from logistic regression analysis by using marginal standardization, adjusting for age, insurance, gender, year of admission, and severity of the femur fracture based on the ICD-9-CM/AIS score for the lower extremities.
Diagnosis of Abuse Among Infants With TBI and Femur Fractures
A diagnosis of physical abuse was made in 40% of infants who had TBI and 35% of infants who had femur fractures. Among the subset of infants with TBI who underwent a skeletal survey, the rate of diagnosis of abuse increased to 53%. Only 12% of infants with TBI who did not undergo a skeletal survey were diagnosed as abused. A diagnosis of abuse was made in 41% of femur fracture cases that received a skeletal survey and 17% of cases without a skeletal survey.
Discussion
The results from this study highlight the finding that adherence to guidelines for screening for occult fractures in young children diagnosed with physical abuse varies substantially among pediatric institutions, with >90% of children undergoing screening at some hospitals and <70% of children receiving screening at other hospitals. The low rate of screening at some institutions underscores an opportunity to improve quality of care because imaging would be expected to reveal occult fractures in one-third of these children.4,5,8,9
Even greater variation in screening for occult fractures was noted among infants who had TBI and femur fractures, injuries associated with a high likelihood of abuse. Previous estimates of the rate of diagnosis of abuse among infants with femur factures range from 30% to 70% but might be higher if motor vehicle crash–related injuries are excluded and if cases of probable but not definite abuse are included.45–47 Similarly, the reported rate of diagnosis of abuse among infants who have TBI ranges from 33% to 95%.29,39,46,48 The high rate of diagnosed abuse among infants who have femur fractures or TBI could imply the need for universal screening for occult fractures in these populations. Another argument could be made, however, that not all infants who have these injuries require a skeletal survey and that individual case characteristics should be considered when determining if there is sufficient suspicion for abuse to warrant a skeletal survey. For instance, the likelihood that a femur fracture resulted from abuse might be lower in older infants who are beginning to ambulate than in younger infants. Also, although race and SES should not influence the clinical decision to perform an evaluation for abuse, studies have shown that black infants and infants from lower SES groups are more likely to be evaluated for abuse than white infants and infants from higher SES groups.13,22,27–29,49 Thus, for reasons that are either warranted or unwarranted, rates of skeletal survey use across hospitals might be expected to vary based on characteristics of patients presenting to those hospitals. Our results, however, demonstrated that after adjusting for differences in patient age, race, insurance status, injury severity, and year of admission, rates of screening still varied by almost twofold among infants who had TBI and by more than twofold among infants who had femur fractures.
Reasons for the observed variation in skeletal survey performance at pediatric hospitals are unknown. The decision to screen for occult fractures is likely complex and not dependent solely on patient characteristics. Studies have suggested that physician-level factors, including medical specialty, education, attitudes, and experiences, might influence the decision to consider and diagnose abuse, but such studies have not focused on screening for occult fractures.22–26 Variation in perceived risk of abuse associated with TBI and femur fractures might also contribute to the variation in rates of skeletal surveys noted in our study. Hospital-level factors including availability and accessibility of child abuse consultants, abuse-specific hospital protocols,30 and availability of technical resources might also contribute to variability in screening practices. Although the type of child abuse services was only identified for a subset of hospitals, analysis indicated that adherence to screening recommendations was higher at hospitals with comprehensive child abuse programs than at other institutions. The development and implementation of detailed clinical guidelines to aid clinicians in identifying cases that require screening for occult injuries might reduce disparities in screening. At 1 institution, racial and socioeconomic disparities in skeletal survey use in young children with TBI were eliminated after the implementation of screening guidelines in that population.30 However, it is evident from examples in other areas of medicine50–52 that simply developing guidelines is not sufficient to standardize care and improve quality. Barriers and factors that facilitate adherence to guidelines must also be examined.
Our study has limitations. First, the study relied on coded diagnostic data, which might be subject to inaccuracies in coding. Second, information regarding evaluations performed before or after hospitalization at PHIS institutions was not available. Thus, in some cases, children might have had screening performed at another hospital or in the outpatient setting that appropriately might not have been repeated. Third, additional patient-level factors including caregiver histories and other clinical details were unavailable in the PHIS database. These factors might have influenced the decision to perform a skeletal survey among injured children. Finally, although the type of child abuse services at PHIS hospitals was associated with adherence to screening recommendations, our sample only included a few hospitals without comprehensive child abuse programs. Multiple factors might affect the effectiveness and quality of child abuse services at these hospitals that are not adequately captured by using NACHRI classifications.
Conclusions
The observed variation in screening for occult fractures in young victims of physical abuse and infants who have injuries that carry a high likelihood of abuse illustrates the finding that uniform adoption of practice guidelines for screening has not occurred across major children’s hospitals. Such variation highlights an opportunity to improve the quality of care for child victims and potentially decrease the risk that abuse cases might be missed, thereby enabling protection of children at risk for ongoing harm. A clear understanding of factors that promote and prevent screening is vital for the development of effective physician-level and hospital-level interventions to enhance screening practices, improve detection and diagnosis of abuse, and decrease disparities.
Acknowledgments
We thank Nancy Hanson, Associate Director, and Karen Seaver Hill, Director of Child Advocacy, at NACHRI for their work in preparing and providing the data regarding the type of child abuse services available at the hospitals.
Glossary
- AIS
Abbreviated Injury Score
- CI
confidence interval
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- NACHRI
National Association of Children’s Hospitals and Related Institutions
- OR
odds ratio
- PHIS
Pediatric Health Information System
- SES
socioeconomic status
- TBI
traumatic brain injury
Footnotes
Dr Wood, Dr Feudtner, Mr Luan, Dr Localio, and Dr Rubin were responsible for study concept and design; Dr Wood and Mr Luan conducted the acquisition of data; Dr Wood, Dr Feudtner, Ms Medina, Dr Localio, and Dr Rubin performed the analysis and interpretation of data; and Dr Wood, Dr Feudtner, Ms Medina, Mr Luan, Dr Localio, and Dr Rubin were responsible for drafting of the manuscript, critical revisions for important intellectual content, and approval of the manuscript. Dr Wood had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors take public responsibility for the content presented in the article.
FINANCIAL DISCLOSURE: Dr Wood’s institution has received payment for expert witness court testimony that Dr Wood has provided in cases of suspected child abuse. The other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Wood has received salary funding from the National Institute of Child Health and Human Development grant (1K23HD071967-01).
References
- 1.Section on Radiology. American Academy of Pediatrics . Diagnostic imaging of child abuse. Pediatrics. 2009;123(5):1430–1435 [DOI] [PubMed] [Google Scholar]
- 2.Kellogg ND, American Academy of Pediatrics Committee on Child Abuse and Neglect . Evaluation of suspected child physical abuse. Pediatrics. 2007;119(6):1232–1241 [DOI] [PubMed] [Google Scholar]
- 3.American College of Radiology. ACR-SPR practice guideline for skeletal surveys in children. 2011 [updated 2011; cited 8/24/2012]; 1–6]. Available at: www.acr.org/∼/media/ACR/Documents/PGTS/guidelines/Skeletal_Surveys.pdf Accessed August 27, 2012 [Google Scholar]
- 4.Mandelstam SA, Cook D, Fitzgerald M, Ditchfield MR. Complementary use of radiological skeletal survey and bone scintigraphy in detection of bony injuries in suspected child abuse. Arch Dis Child. 2003;88(5):387–390, discussion 387–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Degraw M, Hicks RA, Lindberg D, Using Liver Transaminases to Recognize Abuse (ULTRA) Study Investigators . Incidence of fractures among children with burns with concern regarding abuse. Pediatrics. 2010;125(2). Available at: www.pediatrics.org/cgi/content/full/125/2/e295 [DOI] [PubMed] [Google Scholar]
- 6.Rubin DM, Christian CW, Bilaniuk LT, Zazyczny KA, Durbin DR. Occult head injury in high-risk abused children. Pediatrics. 2003;111(6 pt 1):1382–1386 [DOI] [PubMed] [Google Scholar]
- 7.Laskey AL, Holsti M, Runyan DK, Socolar RR. Occult head trauma in young suspected victims of physical abuse. J Pediatr. 2004;144(6):719–722 [DOI] [PubMed] [Google Scholar]
- 8.Belfer RA, Klein BL, Orr L. Use of the skeletal survey in the evaluation of child maltreatment. Am J Emerg Med. 2001;19(2):122–124 [DOI] [PubMed] [Google Scholar]
- 9.Hicks RA, Stolfi A. Skeletal surveys in children with burns caused by child abuse. Pediatr Emerg Care. 2007;23(5):308–313 [DOI] [PubMed] [Google Scholar]
- 10.Duffy SO, Squires J, Fromkin JB, Berger RP. Use of skeletal surveys to evaluate for physical abuse: analysis of 703 consecutive skeletal surveys. Pediatrics. 2011;127(1). Available at: www.pediatrics.org/cgi/content/full/127/1/e47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karmazyn B, Lewis ME, Jennings SG, Hibbard RA, Hicks RA. The prevalence of uncommon fractures on skeletal surveys performed to evaluate for suspected abuse in 930 children: should practice guidelines change? AJR Am J Roentgenol. 2011;197(1):W159–W163. [DOI] [PubMed] [Google Scholar]
- 12.Ravichandiran N, Schuh S, Bejuk M, et al. Delayed identification of pediatric abuse-related fractures. Pediatrics. 2010;125(1):60–66 [DOI] [PubMed] [Google Scholar]
- 13.Jenny C, Hymel KP, Ritzen A, Reinert SE, Hay TC. Analysis of missed cases of abusive head trauma. JAMA. 1999;281(7):621–626 [DOI] [PubMed] [Google Scholar]
- 14.Oral R, Blum KL, Johnson C. Fractures in young children: are physicians in the emergency department and orthopedic clinics adequately screening for possible abuse? Pediatr Emerg Care. 2003;19(3):148–153 [DOI] [PubMed] [Google Scholar]
- 15.King WK, Kiesel EL, Simon HK. Child abuse fatalities: are we missing opportunities for intervention? Pediatr Emerg Care. 2006;22(4):211–214 [DOI] [PubMed] [Google Scholar]
- 16.Thackeray JD. Frena tears and abusive head injury: a cautionary tale. Pediatr Emerg Care. 2007;23(10):735–737 [DOI] [PubMed] [Google Scholar]
- 17.Oral R, Yagmur F, Nashelsky M, Turkmen M, Kirby P. Fatal Abusive Head Trauma Cases: Consequence of Medical Staff Missing Milder Forms of Physical Abuse. Pediatric Emergency Care. 2008;24(12):816–821. [DOI] [PubMed] [Google Scholar]
- 18.National Association of Children's Hospitals and Related Institutions Defining the Children’s Hospital Role in Child Maltreatment. Alexandria, VA: NACHRI; 2006 [Google Scholar]
- 19.National Association of Children's Hospitals and Related Institutions 2005 Survey Findings: Children’s Hospitals Child Abuse Services. Alexandria, VA: NACHRI; 2006 [Google Scholar]
- 20.National Association of Children's Hospitals and Related Institutions Responding to Child Maltreatment: 2008 Survey Findings and Trends. Alexandria, VA: NACHRI; 2009 [Google Scholar]
- 21.Tien I, Bauchner H, Reece RM. What is the system of care for abused and neglected children in children’s institutions? Pediatrics. 2002;110(6):1226–1231 [DOI] [PubMed] [Google Scholar]
- 22.Lane WG, Dubowitz H. What factors affect the identification and reporting of child abuse-related fractures? Clin Orthop Relat Res. 2007;461:219–225 [DOI] [PubMed] [Google Scholar]
- 23.Flaherty EG, Sege R, Binns HJ, Mattson CL, Christoffel KK, Pediatric Practice Research Group . Health care providers’ experience reporting child abuse in the primary care setting. Arch Pediatr Adolesc Med. 2000;154(5):489–493 [DOI] [PubMed] [Google Scholar]
- 24.Flaherty EG, Sege R, Price LL, Christoffel KK, Norton DP, O’Connor KG. Pediatrician characteristics associated with child abuse identification and reporting: results from a national survey of pediatricians. Child Maltreat. 2006;11(4):361–369 [DOI] [PubMed] [Google Scholar]
- 25.Flaherty EG, Sege RD, Griffith J, et al. PROS network. NMAPedsNet . From suspicion of physical child abuse to reporting: primary care clinician decision-making. Pediatrics. 2008;122(3):611–619 [DOI] [PubMed] [Google Scholar]
- 26.Sege RD, Flaherty EG. Forty years later: inconsistencies in reporting of child abuse. Arch Dis Child. 2008;93(10):822–824 [DOI] [PubMed] [Google Scholar]
- 27.Wood JN, Christian CW, Adams CM, Rubin DM. Skeletal surveys in infants with isolated skull fractures. Pediatrics. 2009;123(2). Available at: www.pediatrics.org/cgi/content/full/123/2/e247 [DOI] [PubMed] [Google Scholar]
- 28.Lane WG, Rubin DM, Monteith R, Christian CW. Racial differences in the evaluation of pediatric fractures for physical abuse. JAMA. 2002;288(13):1603–1609 [DOI] [PubMed] [Google Scholar]
- 29.Wood JN, Hall M, Schilling S, Keren R, Mitra N, Rubin DM. Disparities in the evaluation and diagnosis of abuse among infants with traumatic brain injury. Pediatrics. 2010;126(3):408–414 [DOI] [PubMed] [Google Scholar]
- 30.Rangel EL, Cook BS, Bennett BL, Shebesta K, Ying J, Falcone RA. Eliminating disparity in evaluation for abuse in infants with head injury: use of a screening guideline. J Pediatr Surg. 2009;44(6):1229–1234, discussion 1234–1235 [DOI] [PubMed] [Google Scholar]
- 31.Trokel M, Waddimba A, Griffith J, Sege R. Variation in the diagnosis of child abuse in severely injured infants [published correction appears in Pediatrics. 2006;118(3):1324]. Pediatrics. 2006;117(3):722–728 [DOI] [PubMed] [Google Scholar]
- 32.Fisher BT, Lindenaur PK, Feudtner C. In-hospital databases. In: Strom BL, Kimmel SE, Hennessy S, eds. Pharmacoepidemiology. 5th ed. Wiley-Blackwell, Oxford, United Kingdom; 2012:244–258 [Google Scholar]
- 33.Christakis DA, Cowan CA, Garrison MM, Molteni R, Marcuse E, Zerr DM. Variation in inpatient diagnostic testing and management of bronchiolitis. Pediatrics. 2005;115(4):878–884 [DOI] [PubMed] [Google Scholar]
- 34.Tarini BA, Garrison MM, Christakis DA. Institutional variation in ordering complete blood counts for children hospitalized with bronchiolitis. J Hosp Med. 2007;2(2):69–73 [DOI] [PubMed] [Google Scholar]
- 35.Mannix R, Meehan WP, Monuteaux MC, Bachur RG. Computed tomography for minor head injury: variation and trends in major United States pediatric emergency departments. J Pediatr. 2012;160(1):136–139.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kokorowski PJ, Routh JC, Graham DA, Nelson CP. Variations in timing of surgery among boys who underwent orchidopexy for cryptorchidism. Pediatrics. 2010;126(3). Available at: www.pediatrics.org/cgi/content/full/126/3/e576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sobota A, Graham DA, Neufeld EJ, Heeney MM. Thirty-day readmission rates following hospitalization for pediatric sickle cell crisis at freestanding children’s hospitals: risk factors and hospital variation. Pediatr Blood Cancer. 2012;58(1):61–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gerber JS, Newland JG, Coffin SE, et al. Variability in antibiotic use at children’s hospitals. Pediatrics. 2010;126(6):1067–1073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Billmire ME, Myers PA. Serious head injury in infants: accident or abuse? Pediatrics. 1985;75(2):340–342 [PubMed] [Google Scholar]
- 40.Myhre MC, Grøgaard JB, Dyb GA, Sandvik L, Nordhov M. Traumatic head injury in infants and toddlers. Acta Paediatr. 2007;96(8):1159–1163 [DOI] [PubMed] [Google Scholar]
- 41.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55(2):652–659 [DOI] [PubMed] [Google Scholar]
- 42.Korn EL, Graubard BI. Analysis of Health Surveys. New York, NY: Wiley; 1999 [Google Scholar]
- 43.Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157(4):364–375 [DOI] [PubMed] [Google Scholar]
- 44.Rogers WH. Regression standard errors in clustered samples. In: Stata Technical Bulletin [computer program]. College Station, TX: Stata Press; 1993:19–23 [Google Scholar]
- 45.Schwend RM, Werth C, Johnston A. Femur shaft fractures in toddlers and young children: rarely from child abuse. J Pediatr Orthop. 2000;20(4):475–481 [PubMed] [Google Scholar]
- 46.Leventhal JM, Martin KD, Asnes AG. Fractures and traumatic brain injuries: abuse versus accidents in a US database of hospitalized children. Pediatrics. 2010;126(1). Available at: www.pediatrics.org/cgi/content/full/126/1/e104 [DOI] [PubMed] [Google Scholar]
- 47.Gross RH, Stranger M. Causative factors responsible for femoral fractures in infants and young children. J Pediatr Orthop. 1983;3(3):341–343 [DOI] [PubMed] [Google Scholar]
- 48.Reece RM, Sege R. Childhood head injuries: accidental or inflicted? Arch Pediatr Adolesc Med. 2000;154(1):11–15 [PubMed] [Google Scholar]
- 49.Hampton RL, Newberger EH. Child abuse incidence and reporting by hospitals: significance of severity, class, and race. Am J Public Health. 1985;75(1):56–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guerra CE, Schwartz JS, Armstrong K, Brown JS, Halbert CH, Shea JA. Barriers of and facilitators to physician recommendation of colorectal cancer screening. J Gen Intern Med. 2007;22(12):1681–1688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vernacchio L, Vezina RM, Mitchell AA. Management of acute otitis media by primary care physicians: Trends since the release of the 2004 American Academy of Pediatrics/American Academy of Family Physicians clinical practice guideline. Pediatrics 2007 Aug; 120:281–287 [DOI] [PubMed] [Google Scholar]
- 52.Madlon-Kay DJ. Clinician Adherence to Guideline for Phototherapy Use in Newborns. J Am Board Fam Med. 2012;25:(4)437–441 [DOI] [PubMed] [Google Scholar]